Ahsan A.N, Habib M.A, Khoda B. Resource based process planning for additive manufacturing. Computer-Aided Design. 2015;69:112–125.
Arcaute K, Mann B, Wicker R. Stereolithography of spatially controlled multi-material bioactive poly (ethylene glycol) scaffolds. Acta Biomaterialia. 2010;6(3):1047–1054.
Arcaute K, Mann B.K, Wicker R.B. Stereolithography of three-dimensional bioactive poly (ethylene glycol) constructs with encapsulated cells. Annals of Biomedical Engineering. 2006;34(9):1429–1441.
Ashkin A, Dziedzic J.M. Optical trapping and manipulation of viruses and bacteria. Science. 1987;235(4795):1517–1520.
Bajaj P, Schweller R.M, Khademhosseini A, West J.L, Bashir R. 3D biofabrication strategies for tissue engineering and regenerative medicine. Annual Review of Biomedical Engineering. 2014;16:247–276.
Barron J.A, Young H.D, Dlott D.D, Darfler M.M, Krizman D.B, Ringeisen B.R. Printing of protein microarrays via a capillary-free fluid jetting mechanism. Proteomics. 2005;5(16):4138–4144.
Barron J.A, Krizman D.B, Ringeisen B.R. Laser printing of single cells: statistical analysis, cell viability, and stress. Annals of Biomedical Engineering. 2005;33(2):121–130.
Barron J.A, Spargo B.J, Ringeisen B.R. Biological laser printing of three dimensional cellular structures. Applied Physics A. 2004;79(4–6):1027–1030.
Bergeron V, Bonn D, Martin J.Y, Vovelle L. Controlling droplet deposition with polymer additives. Nature. 2000;405(6788):772–775.
Bertsch A, Bernhard P, Vogt C, Renaud P. Rapid prototyping of small size objects. Rapid Prototyping Journal. 2000;6(4):259–266.
Billiet T, Vandenhaute M, Schelfhout J, Van Vlierberghe S, Dubruel P. A review of trends and limitations in hydrogel-rapid prototyping for tissue engineering. Biomaterials. 2012;33(26):6020–6041.
Bryant S.J, Nuttelman C.R, Anseth K.S. Cytocompatibility of UV and visible light photoinitiating systems on cultured NIH/3T3 fibroblasts in vitro. Journal of Biomaterials Science, Polymer Edition. 2000;11(5):439–457. .
Burks H.E, Phamduy T.B, Azimi M.S, Saksena J, Burow M.E, Collins-Burow B.M, Chrisey D.B, Murfee W.L. Laser direct-write onto live tissues: a novel model for studying cancer cell migration. Journal of Cellular Physiology. 2016;231(11):2333–2338.
Catros S, Guillemot F, Nandakumar A, Ziane S, Moroni L, Habibovic P, van Blitterswijk C, Rousseau B, Chassande O, Amédée J, Fricain J.C. Layer-by-layer tissue microfabrication supports cell proliferation in vitro and in vivo. Tissue Engineering Part C: Methods. 2011;18(1):62–70.
Choi J.W, Kim H.C, Wicker R. Multi-material stereolithography. Journal of Materials Processing Technology. 2011;211(3):318–328.
Chrisey D.B, Pique A, McGill R.A, Horwitz J.S, Ringeisen B.R, Bubb D.M, Wu P.K. Laser deposition of polymer and biomaterial films. Chemical Reviews. 2003;103(2):553–576.
Cumpston B.H, Ananthavel S.P, Barlow S, Dyer D.L, Ehrlich J.E, Erskine L.L, Heikal A.A, Kuebler S.M, Lee I.Y.S, McCord-Maughon D, Qin J. Two-photon polymerization initiators for three-dimensional optical data storage and microfabrication. Nature. 1999;398(6722):51–54.
Dababneh A.B, Ozbolat I.T. Bioprinting technology: a current state-of-the-Art review. Journal of Manufacturing Science and Engineering. 2014;136(6):061016.
Devillard R, Correa M.M, Kériquel V, Rémy M, Kalisky J, Ali M, Guillotin B, Guillemot F. Cell patterning by laser-assisted bioprinting. Methods in Cell Biology. 2013;119:159–174.
Dhariwala B, Hunt E, Boland T. Rapid prototyping of tissue-engineering constructs, using photopolymerizable hydrogels and stereolithography. Tissue Engineering. 2004;10(9–10):1316–1322.
Doraiswamy A, Narayan R.J, Lippert T, Urech L, Wokaun A, Nagel M, Hopp B, Dinescu M, Modi R, Auyeung R.C.Y, Chrisey D.B. Excimer laser forward transfer of mammalian cells using a novel triazene absorbing layer. Applied Surface Science. 2006;252(13):4743–4747.
Doraiswamy A, Narayan R.J, Harris M.L, Qadri S.B, Modi R, Chrisey D.B. Laser microfabrication of hydroxyapatite-osteoblast-like cell composites. Journal of Biomedical Materials Research Part A. 2007;80(3):635–643.
Emons M, et al. Two-photon polymerization technique with sub-50 nm resolution by sub-10 fs laser pulses. Optical Materials Express. 2012;2(7):942–947.
Fedorovich N.E, Oudshoorn M.H, van Geemen D, Hennink W.E, Alblas J, Dhert W.J. The effect of photopolymerization on stem cells embedded in hydrogels. Biomaterials. 2009;30(3):344–353.
Fitz-Gerald J.M, Wu H.D, Pique A, Horwitz J.S, Auyeung R.C.Y, Chang W, Kim W.J, Chrisey D.B. Maple direct write: a new approach to fabricate ferroelectric thin film devices in air at room temperature. Integrated Ferroelectrics. 2000;28(1–4):13–28.
Gaebel R, Ma N, Liu J, Guan J, Koch L, Klopsch C, Gruene M, Toelk A, Wang W, Mark P, Wang F. Patterning human stem cells and endothelial cells with laser printing for cardiac regeneration. Biomaterials. 2011;32(35):9218–9230.
Gaetani R, Doevendans P.A, Metz C.H, Alblas J, Messina E, Giacomello A, Sluijter J.P. Cardiac tissue engineering using tissue printing technology and human cardiac progenitor cells. Biomaterials. 2012;33(6):1782–1790.
Gauvin R, Chen Y.C, Lee J.W, Soman P, Zorlutuna P, Nichol J.W, Bae H, Chen S, Khademhosseini A. Microfabrication of complex porous tissue engineering scaffolds using 3D projection stereolithography. Biomaterials. 2012;33(15):3824–3834.
Gittard S.D, Narayan R.J. Laser direct writing of micro- and nano-scale medical devices. Expert Review of Medical Devices. 2010;7(3):343–356.
Gruene M, Pflaum M, Deiwick A, Koch L, Schlie S, Unger C, Wilhelmi M, Haverich A, Chichkov B.N. Adipogenic differentiation of laser-printed 3D tissue grafts consisting of human adipose-derived stem cells. Biofabrication. 2011;3(1):015005. .
Gruene M, Pflaum M, Hess C, Diamantouros S, Schlie S, Deiwick A, Koch L, Wilhelmi M, Jockenhoevel S, Haverich A, Chichkov B. Laser printing of three-dimensional multicellular arrays for studies of cell–cell and cell–environment interactions. Tissue Engineering Part C: Methods. 2011;17(10):973–982.
Gudapati H, Yan J, Huang Y, Chrisey D.B. Alginate gelation-induced cell death during laser-assisted cell printing. Biofabrication. 2014;6(3):035022.
Gudapati H, Dey M, Ozbolat I. A comprehensive review on droplet-based bioprinting: past, present and future. Biomaterials. 2016;102:20–42.
Guillemot F, Souquet A, Catros S, Guillotin B, Lopez J, Faucon M, Pippenger B, Bareille R, Rémy M, Bellance S, Chabassier P. High-throughput laser printing of cells and biomaterials for tissue engineering. Acta Biomaterialia. 2010;6(7):2494–2500.
Hadjizadeh A, Doillon C.J. Directional migration of endothelial cells towards angiogenesis using polymer fibres in a 3D co-culture system. Journal of Tissue Engineering and Regenerative Medicine. 2010;4(7):524–531.
Hahn M.S, Miller J.S, West J.L. Three-dimensional biochemical and biomechanical patterning of hydrogels for guiding cell behavior. Advanced Materials. 2006;18(20):2679–2684.
Hopp B, Smausz T, Kresz N, Barna N, Bor Z, Kolozsvári L, Chrisey D.B, Szabó A, Nógrádi A. Survival and proliferative ability of various living cell types after laser-induced forward transfer. Tissue Engineering. 2005;11(11–12):1817–1823.
Hribar K.C, Soman P, Warner J, Chung P, Chen S. Light-assisted direct-write of 3D functional biomaterials. Lab on a Chip. 2014;14(2):268–275.
Huang T.Q, Qu X, Liu J, Chen S. 3D printing of biomimetic microstructures for cancer cell migration. Biomedical Microdevices. 2014;16(1):127–132.
Itoga K, Yamato M, Kobayashi J, Kikuchi A, Okano T. Cell micropatterning using photopolymerization with a liquid crystal device commercial projector. Biomaterials. 2004;25(11):2047–2053.
Keriquel V, Guillemot F, Arnault I, Guillotin B, Miraux S, Amédée J, Fricain J.C, Catros S. In vivo bioprinting for computer-and robotic-assisted medical intervention: preliminary study in mice. Biofabrication. 2010;2(1):014101.
Klein F, Richter B, Striebel T, Franz C.M, Freymann G.V, Wegener M, Bastmeyer M. Two-component polymer scaffolds for controlled three-dimensional cell culture. Advanced Materials. 2011;23(11):1341–1345.
Koch L, Deiwick A, Schlie S, Michael S, Gruene M, Coger V, Zychlinski D, Schambach A, Reimers K, Vogt P.M, Chichkov B. Skin tissue generation by laser cell printing. Biotechnology and Bioengineering. 2012;109(7):1855–1863.
Lin Y, Huang G, Huang Y, Jeremy Tzeng T.R, Chrisey D. Effect of laser fluence in laser-assisted direct writing of human colon cancer cell. Rapid Prototyping Journal. 2010;16(3):202–208.
Lin Y, Huang Y, Wang G, Tzeng T.R.J, Chrisey D.B. Effect of laser fluence on yeast cell viability in laser-assisted cell transfer. Journal of Applied Physics. 2009;106(4):043106.
Lin Y, Huang Y, Chrisey D.B. Droplet formation in matrix-assisted pulsed-laser evaporation direct writing of glycerol-water solution. Journal of Applied Physics. 2009;105(9):093111.
Lu Y, Chen S. Projection printing of 3-dimensional tissue scaffolds. In: Liebschner A.K.M, ed. Computer-Aided Tissue Engineering. New York, NY: Humana Press; 2012:289–302.
Ma X, Qu X, Zhu W, Li Y.S, Yuan S, Zhang H, Liu J, Wang P, Lai C.S.E, Zanella F, Feng G.S. Deterministically patterned biomimetic human iPSC-derived hepatic model via rapid 3D bioprinting. Proceedings of the National Academy of Sciences of the United States of America. 2016;113(8):2206–2211. .
Melchels F.P, Feijen J, Grijpma D.W. A review on stereolithography and its applications in biomedical engineering. Biomaterials. 2010;31(24):6121–6130.
Nahmias Y, Schwartz R.E, Verfaillie C.M, Odde D.J. Laser-guided direct writing for three-dimensional tissue engineering. Biotechnology and Bioengineering. 2005;92(2):129–136.
Narayan R, ed. Rapid Prototyping of Biomaterials: Principles and Applications. Woodhead Publishing; 2014.
Odde D.J, Renn M.J. Laser-guided direct writing for applications in biotechnology. Trends in Biotechnology. 1999;17(10):385–389.
Odde D.J, Renn M.J. Laser-guided direct writing of living cells. Biotechnology and Bioengineering. 2000;67(3):312–318.
Ovsianikov A, Chichkov B, Mente P, Monteiro-Riviere N.A, Doraiswamy A, Narayan R.J. Two photon polymerization of polymer–ceramic hybrid materials for transdermal drug delivery. International Journal of Applied Ceramic Technology. 2007;4(1):22–29.
Ovsianikov A, Schlie S, Ngezahayo A, Haverich A, Chichkov B.N. Two-photon polymerization technique for microfabrication of CAD-designed 3D scaffolds from commercially available photosensitive materials. Journal of Tissue Engineering and Regenerative Medicine. 2007;1(6):443–449.
Ovsianikov A, Chichkov B.N. Three-dimensional microfabrication by two-photon polymerization technique. In: Liebschner A.K.M, ed. Computer-Aided Tissue Engineering. New York, NY: Humana Press; 2012:311–325.
Ovsianikov A, et al. Laser photofabrication of cell-containing hydrogel constructs. Langmuir. 2014;30(13):3787–3794.
Ozbolat I.T. Bioprinting scale-up tissue and organ constructs for transplantation. Trends in Biotechnology. 2015;33(7):395–400.
Ozbolat I.T, Hospodiuk M. Current advances and future perspectives in extrusion-based bioprinting. Biomaterials. 2016;76:321–343.
Ozbolat I.T, Yu Y. Bioprinting toward organ fabrication: challenges and future trends. IEEE Transactions on Bio-Medical Engineering. 2013;60(3):691–699.
Patz T.M, Doraiswamy A, Narayan R.J, He W, Zhong Y, Bellamkonda R, Modi R, Chrisey D.B. Three-dimensional direct writing of B35 neuronal cells. Journal of Biomedical Materials Research Part B: Applied Biomaterials. 2006;78(1):124–130.
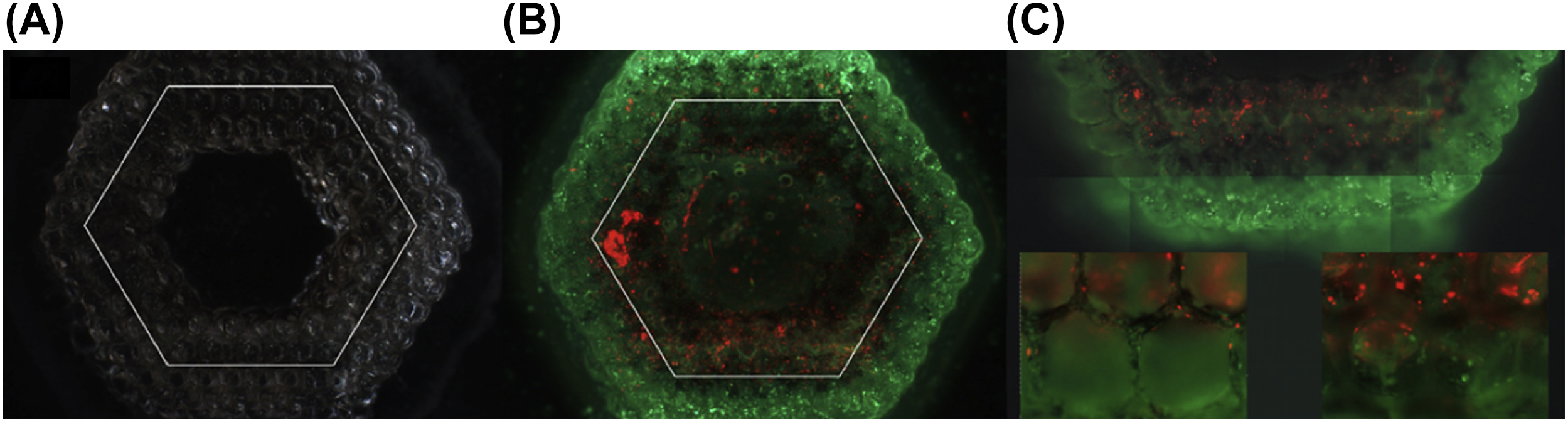
Phamduy T.B, Sweat R.S, Azimi M.S, Burow M.E, Murfee W.L, Chrisey D.B. Printing cancer cells into intact microvascular networks: a model for investigating cancer cell dynamics during angiogenesis. Integrative Biology. 2015;7(9):1068–1078.
Piqué A. The matrix-assisted pulsed laser evaporation (MAPLE) process: origins and future directions. Applied Physics A. 2011;105(3):517–528.
Renn M.J, Pastel R, Lewandowski H.J. Laser guidance and trapping of mesoscale particles in hollow-core optical fibers. Physical Review Letters. 1999;82(7):1574–1577.
Riggs B.C, Dias A.D, Schiele N.R, Cristescu R, Huang Y, Corr D.T, Chrisey D.B. Matrix-assisted pulsed laser methods for biofabrication. MRS Bulletin. 2011;36(12):1043–1050.
Ringeisen B.R, Kim H, Barron J.A, Krizman D.B, Chrisey D.B, Jackman S, Auyeung R.Y.C, Spargo B.J. Laser printing of pluripotent embryonal carcinoma cells. Tissue Engineering. 2004;10(3–4):483–491.
Ringeisen B.R, Wu P.K, Kim H, Pique A, Auyeung R.Y.C, Young H.D, Chrisey D.B, Krizman D.B. Picoliter-scale protein microarrays by laser direct write. Biotechnology Progress. 2002;18(5):1126–1129. .
Roisman I.V, Rioboo R, Tropea C. Normal impact of a liquid drop on a dry surface: model for spreading and receding. Proceedings of the Royal Society of London A: Mathematical, Physical and Engineering Sciences. 2002;458(2022):1411–1430.
Roots Analysis Private Ltd. 3D Bioprinting Market 2014–2030. 2014.
Salonitis K. 10.03 – stereolithography. In: Hashmi S, et al., ed. Comprehensive Materials Processing. Oxford: Elsevier; 2014:19–67.
Schiele N.R, Koppes R.A, Corr D.T, Ellison K.S, Thompson D.M, Ligon L.A, Lippert T.K, Chrisey D.B. Laser direct writing of combinatorial libraries of idealized cellular constructs: biomedical applications. Applied Surface Science. 2009;255(10):5444–5447.
Schiele N.R, Chrisey D.B, Corr D.T. Gelatin-based laser direct-write technique for the precise spatial patterning of cells. Tissue Engineering Part C: Methods. 2010;17(3):289–298.
Sellinger A.T, Martin A.H, Fitz-Gerald J.M. Effect of substrate temperature on poly (methyl methacrylate) nanocomposite thin films deposited by matrix assisted pulsed laser evaporation. Thin Solid Films. 2008;516(18):6033–6040.
Serbin J, Ovsianikov A, Chichkov B. Fabrication of woodpile structures by two-photon polymerization and investigation of their optical properties. Optics Express. 2004;12(21):5221–5228.
Unger C, Gruene M, Koch L, Koch J, Chichkov B.N. Time-resolved imaging of hydrogel printing via laser-induced forward transfer. Applied Physics A. 2011;103(2):271–277.
Williams C.G, Malik A.N, Kim T.K, Manson P.N, Elisseeff J.H. Variable cytocompatibility of six cell lines with photoinitiators used for polymerizing hydrogels and cell encapsulation. Biomaterials. 2005;26(11):1211–1218.
Xiong R, Zhang Z, Chai W, Huang Y, Chrisey D.B. Freeform drop-on-demand laser printing of 3D alginate and cellular constructs. Biofabrication. 2015;7(4):045011.
Xiong R, Zhang Z, Huang Y. Identification of optimal printing conditions for laser printing of alginate tubular constructs. Journal of Manufacturing Processes. 2015;20:450–455.
Xu J, Grant S.A, Pastel R.L. Laser-guided direct writing: a novel method to deposit biomolecules for biosensors arrays. IEEE Transactions on Biomedical Engineering. 2003;50(1):126–128.
Zhang Z, Xiong R, Corr D.T, Huang Y. Study of impingement types and printing quality during laser printing of viscoelastic alginate solutions. Langmuir. 2016;32(12):3004–3014.
Zhang Z, Xiong R, Mei R, Huang Y, Chrisey D.B. Time-resolved imaging study of jetting dynamics during laser printing of viscoelastic alginate solutions. Langmuir. 2015;31(23):6447–6456.
Zhou C, Chen Y, Yang Z, Khoshnevis B. Digital material fabrication using mask-image-projection-based stereolithography. Rapid Prototyping Journal. 2013;19(3):153–165.
Zipfel W.R, Williams R.M, Webb W.W. Nonlinear magic: multiphoton microscopy in the biosciences. Nature Biotechnology. 2003;21(11):1369–1377.







![]() (6.1)
(6.1)