Chapter 4
Finding Out How Exercise Works
IN THIS CHAPTER
![]() Recognizing how your body’s hormones regulate blood glucose during exercise
Recognizing how your body’s hormones regulate blood glucose during exercise
![]() Finding out how your body makes energy to fuel your workouts
Finding out how your body makes energy to fuel your workouts
![]() Adjusting your activities to stay in blood glucose balance
Adjusting your activities to stay in blood glucose balance
![]() Discovering how glucose responses to intense exercise differ
Discovering how glucose responses to intense exercise differ
What exactly happens to your body when you exercise? Your metabolism gets revved up, and you’re off and running (maybe not literally). Have you ever wondered how your body fuels itself during these physical endeavors?
Clearly, your body uses a lot of calories that come from somewhere that isn’t always obvious, particularly if you’re active first thing in the morning before you eat anything. Your body can run like a well-tuned car or like one that needs a tune-up. You want to aim for the former.
In this chapter, I explain how hormones in your body keep your blood glucose from dropping too much when you’re active. You also find out why activities don’t always affect your blood glucose the way you expect or want them to, and what to do if that happens. You can keep your blood glucose levels in check when you’re active, but doing so often takes a bit of planning.
Knowing How Hormones React
Hormones in your body act like traffic lights when managing your blood glucose. When one turns green, another one with an opposite action turns red, and traffic flows one way. Then the lights reverse, and traffic flows in the opposite direction. It’s usually a tightly regulated process because of how critical glucose is to the function of your brain and nerves.
Directing the flow of glucose in blood
In the case of your body, the traffic lights are controlled by insulin and a bunch of glucose-raising hormones that work in concert (see Table 4-1). Insulin has a lowering effect on blood glucose, and the rest have the ability to raise it.
TABLE 4-1 Actions of Glucose-Raising Hormones
Hormone |
Where It Comes From |
Effects During Exercise |
Glucagon |
Pancreas (alpha cells) |
Stimulates liver glycogen to break down and new glucose to be formed to raise glucose; affected by balance with insulin in liver circulation |
Epinephrine (adrenaline) |
Adrenal medulla |
Stimulates muscle and some liver glycogen to break down; releases fat into the bloodstream |
Norepinephrine |
Adrenal medulla, sympathetic nerve endings |
Stimulates liver to produce new glucose; greater release during intense exercise raises blood glucose more |
Growth hormone |
Anterior pituitary |
Directly stimulates fat release in blood; suppresses glucose use; stimulates protein storage in muscles |
Cortisol |
Adrenal cortex |
Mobilizes amino acids and glycerol to use to make glucose; releases fat for muscle use rather than blood glucose |
At rest, you need insulin to keep your blood glucose from going too high after meals. But when you’re fasting overnight or exercising, your liver needs to release more glucose into the blood, and that requires the opposing hormones.
The most common response is that your blood glucose goes down when you exercise moderately. This happens because contracting muscles take up blood glucose directly without insulin, although insulin can add to the drop. Exercise responses aren’t always predictable, though, and many things can affect how your blood glucose reacts. Sometimes it goes up rather than down when you’re active. (See the following section for more on this effect.)
Understanding why your glucose sometimes goes up with exercise
When you do high-intensity or vigorous exercise like sprinting, intervals, heavy resistance training, and competitions, you often experience an immediate rise in your blood glucose, primarily due to the hormones epinephrine and glucagon. Intense exercise causes your body to release more of the hormones that boost how much glucose your liver releases into your blood, all while keeping your muscles from taking up as much by temporarily raising their insulin resistance. Even when you don’t have diabetes, insulin increases after (and sometimes during) intense workouts.
Glucose-raising hormones work so well that they can easily exceed your body’s immediate need for glucose, especially because you can’t sustain working out at high intensity for long. In such cases, you don’t have to worry about getting low during exercise because your blood glucose goes up during and for a brief time after these activities.
Your body needs some insulin in your system to keep a check and balance on this exaggerated release of glucose-raising hormones during intense exercise, but not so much that your blood glucose drops excessively. If you make your own insulin, your body releases less (but still some) during exercise, and then it releases more as blood glucose rises to lower it back to normal after you stop.
Staying elevated too long after a workout
Due to the residual effects of these glucose-raising hormones, you may experience some insulin resistance immediately after intense exercise, which can last for a few hours. For instance, after doing near-maximal cycling — like cycling up a hill or working against a hard resistance in a spin class — to exhaustion, adults with type 1 diabetes on insulin pumps have elevated blood glucose levels for two hours afterward. If you take insulin, you’ll likely need some extra insulin to bring your blood glucose levels back to normal.
Similarly, in type 2 diabetes, blood glucose can rise in response to a maximal hard cycling workout and stay that way afterward for an hour or two. Eventually, your blood glucose comes down because many people with type 2 diabetes are still making some of their own insulin. Even if you don’t make insulin anymore, it usually comes down over time since your body is more sensitive to the effects of any insulin in your body after a workout. Doing an easier cool-down before you stop entirely may bring your glucose down faster.
Engaging Your Exercise Energy Systems
The way your muscles make and use energy depends on how fast you move, how much force your muscles produce, and how long the activity lasts. Your body has three distinct energy systems (Figure 4-1) to supply your muscles with adenosine triphosphate (ATP), a high-energy compound found in all cells that directly fuels muscle contractions. The three systems act on a continuum, meaning that the first one, followed by the second and finally the third, make ATP as your exercise continues longer than two minutes.
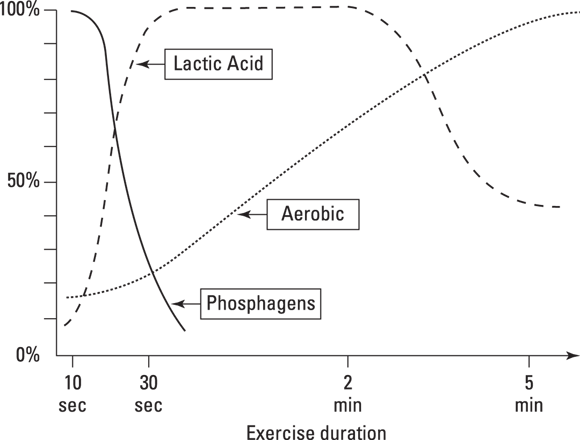
© John Wiley & Sons, Inc. (Adapted from Colberg, S. Diabetic Athlete’s Handbook, Human Kinetics, 2009.)
FIGURE 4-1: Exercise energy systems.
Muscle cells contain only small quantities of ATP ready for use when you start — enough to fuel any activity for about a second, at best. If you want to keep going longer, your muscles need to get ATP from another source right away. Although all the systems can make ATP, the rate at which they supply it varies. The fuels used to make the ATP and the amount of time needed to produce it also differ by system.
Phosphagens system (short and powerful)
For short activities or power moves, your phosphagens system (also called ATP–CP or glycolytic system) supplies almost all the energy you need. It’s called an anaerobic system because it doesn’t need oxygen to operate. It consists of ATP that is already stored in muscle and creatine phosphate (CP) that can be used to rapidly replenish that ATP supply.
The compound CP can’t fuel an activity directly, but it can make more ATP that can after you’ve used up your muscles’ initial one-second supply. The energy released from the rapid breakdown of CP then replenishes ATP to fuel your muscles for another five to nine seconds of activity.
Any activity that lasts less than 10 seconds is fueled mainly by phosphagens. Some examples include a power lift, a 40-meter sprint, a pole vault, a long jump, a baseball pitch, or a basketball dunk.
Generally, these types of activities don’t lower your blood glucose because glucose isn’t used to produce the energy. On the contrary, they can raise your glucose levels because, being short and intense, they can cause your body to release an excess of glucose-raising hormones, and then they end. The extra glucose released stays in your bloodstream.
Lactic acid system (fast, furious, and painful)
You’ve probably heard of lactic acid already because it gets a bad rap. People blame it for making their muscles stiff and sore after exercise, as well as for the pain they feel in their active muscles. Only the second part is true, though, because lactic acid stays in the muscles for only a few minutes after it’s formed, and it certainly isn’t what makes you sore later. (That’s caused by muscle damage and increased blood flow — swelling — in those areas to fix them.)
Lactic acid is also the name for your body’s second energy system, the lactic acid (or rapid glycolysis) system. It supplies the extra fuel for activities that last longer than 10 seconds, but only up to about 2 minutes. This system is also anaerobic because it makes ATP by breaking down glucose stored in muscle as glycogen.
Activities that get most of their fuel from this energy system are less than two minutes in duration at a higher intensity. They include 800-meter runs; 200-meter swimming events; and stop-and-start activities with short, intense activity like basketball, lacrosse, field hockey, and ice hockey.
Aerobic system (lasts longer)
The other end of the spectrum from the first two energy systems is the aerobic energy system used for endurance activities or ultra-endurance exercise. Sometimes called cardio workouts (short for cardiovascular, or involving the heart and the blood vessels), aerobic activities mainly depend on production of energy using oxygen.
Your muscles require a steady supply of ATP during sustained activities like walking, running, swimming, cycling, rowing, and cross-country skiing, which you usually do for a longer period. Extreme examples of prolonged aerobic activities include running a marathon, doing a triathlon, or participating in successive full days of long-distance cycling or backpacking. This system uses a mix of carbohydrate and fat to make ATP — more fat during rest and greater carbohydrate use during exercise. Your muscles can use some protein as fuel, but it usually contributes less than 5 percent of the total energy. Your body may use slightly more protein (up to 15 percent) during extremely prolonged endurance activities like running a marathon.
At rest, your diet and how recently you last exercised affect the mix of fuels your body uses, but most people use about 60 percent fat and 40 percent carbohydrate. If you’re exercising with hyperglycemia, your body may use more blood glucose than normal, regardless of your type of diabetes.
Circulating hormones like adrenaline get the fat out of your fat cells (called adipocytes), and those fats go to your working muscles as fatty acids the muscles can use for fuel during less-intense or longer-duration activities. Your body can use more fat during mild and moderate activities, along with some carbohydrate. The fats stored in the muscles themselves (intramuscular triglycerides) are more important to fuel helping you recover from exercise or during very prolonged workouts (lasting more than two to three hours).
Using Carbohydrate and Fat as Fuels
Glucose, the body’s main form of energy during exercise, is in the blood, muscles, and liver. All carbohydrate can be converted into glucose. Some of it gets used right away, but more is usually stored in your liver and muscles as glycogen after you eat.
During the first few minutes of exercise, your muscles utilize the glucose stored there almost exclusively, releasing lactic acid as a byproduct. As you continue to exercise, your body releases stress hormones, adrenaline, and other hormones that signal to your liver that your body needs more glucose, and your liver releases the glucose you need.
After 20 minutes or so of doing any activity, your body begins to use slightly more stored fat for energy. How much depends on things like how hard you’re working (more intense exercise uses more carbohydrates), how long you exercise (longer workouts increase fat use), how frequently you exercise (because fully restoring extra carbohydrates in your body takes a while), and your usual diet.
Carbohydrate: A high-octane fuel
Doing moderate or vigorous exercise always requires that you have some carbohydrates available, or you’ll be too fatigued to do anything but walk or stop to rest. The body prefers to use carbohydrate because it’s more fuel efficient. It’s like using a high-octane gas and getting more mileage for the same amount of gas — only in the case of the body, carbohydrates release more energy with less oxygen needed compared to fat.
Forget the “fat-burning range”
You’re always burning calories during exercise, and whether they come from glucose or fat doesn’t matter in terms of expending a certain number of calories or losing weight, despite your cardio training machine or cardio tracking app telling you that you’re in a “fat-burning range” or a “cardio-training range.” (You use more carbohydrate than anything in either range.)
The more calories you burn (from either source), the more weight you can potentially lose. The so-called training range you’re in matters only to your duration — you’ll be able to do easier exercise for longer — and to its effect on your blood glucose levels, which lower more with easier activities.
Predicting Your Usual Glucose Response
Doing any physical movement increases your body’s use of blood glucose, which can cause you to develop hypoglycemia more readily during or after your workout while you’re working out. Most of the changes in your blood glucose depend on how much insulin is in your bloodstream when you’re active, along with how well that insulin is working when you’re resting. For example, if your insulin levels are high during an activity, your muscles take up more blood glucose, and you may end up with low blood glucose. You can even end up low for up to 48 hours after you exercise.
On the other hand, exercising when your blood glucose is too high — especially with ketones from having too little insulin in your body — can cause your blood glucose to go even higher. Exercising under those conditions can put you into a serious state of ketoacidosis (DKA, or diabetic ketoacidosis) caused by the combination of too much blood glucose and not enough insulin. Certain types of exercise, such as intense resistance workouts, can also raise your blood glucose, regardless of whether you have diabetes.
Many other factors can impact your usual responses to physical activity. After you learn to anticipate their effects and manage as many as you can, a somewhat predictable pattern emerges over time to help you better predict your blood glucose responses to similar exercise. The type of activity you do can also affect your blood glucose responses, along with how hard, how long, and how often you’re active.
Factoring in Exercise Variables
A number of different factors impact how your blood glucose responds to any activity you do. In this section, you find out more about what those are and the response you can expect.
Type (which exercises)
What type of activity you do is your choice because almost any movement can benefit your health, including cardio training, resistance work, intervals, and cross-training. In adults with type 2 diabetes, a single bout of cardio or resistance training has similar glycemic benefits.
Choosing activities that help you gain or maintain your muscle mass to better manage your diabetes and your overall health as you age is always a good idea. Muscles are the main place you can store the extra carbohydrates you eat and, the bigger your muscle tank, the more carbohydrates you can store there (which helps keep blood glucose levels down). Plus, regular exercise keeps the tank at least partway empty most of the time.
Picking an activity (any activity)
Not surprisingly, people like to do a lot of different types of activities; one type certainly doesn’t fit all. In the Big Blue Test (BBT) conducted online a few years back, almost half of people with diabetes walked, while others engaged in running or jogging (12 percent), cycling (9 percent), using conditioning machines (6 percent), dancing (6 percent), or other activities (19 percent). Choosing between doing cardio training or resistance workouts may be less important than simply choosing to do anything.
Managing your blood glucose, regardless
No matter what you do, be aware of your blood glucose numbers and be cautious. If your blood glucose is too high or low, or you’re not feeling well, you shouldn’t exercise. Also, if your blood glucose goes up, don’t take a correction dose of insulin (if you use it) unless your blood glucose is still high one to two hours later. In that case, consider taking a third to a half dose of your usual correction dose so you don’t get low later.
Intensity (how hard)
How hard you work out should reflect your training and fitness goals, such as whether you want to get fitter, perform better, or just burn some calories
Considering factors that determine your desired intensity
The biggest impact on blood glucose is likely the intensity of your activity. For example, 75 percent of exercisers have their glucose levels drop when they’re active, about 9 percent stay the same, and 15 percent have an increase rather than a decrease.
In general, doing exercise at a low intensity (less than 40 percent heart rate reserve, or HRR) has a lesser glucose-lowering effect than moderate-intensity exercise — unless you do the exercise long enough. How much glucose you use during moderate workouts depends on both how long you work out and how hard you do it. For vigorous exercise (60 percent HRR and higher), you may end up with temporary increases in your blood glucose. (Check out the later section “Heart rate reserve” for details on this measurement.)
Doing any higher-intensity exercise (like interval training) may raise your blood glucose, at least temporarily. In this case, your blood glucose is likely to drop over the next few hours — even more so than if you’d done a similar amount of an easier exercise.
Doing easy activities can help lower blood glucose over the course of the day for most people. If you’re active longer, even just doing an easy activity like walking or standing, your body uses more blood glucose, and your blood levels can decrease over time. How much glucose you use depends on how fit you are doing that activity. Being fitter increases fat use (over glucose) in most cases.
Monitoring your exercise intensity
You have options on how to follow how hard you’re working out, if you choose to do that. They’re as easy as seeing how well you can talk to thinking about how hard it feels to actually measuring something that reflects your intensity.
TALK TEST
A good way to determine whether to speed up or slow down is by using the talk test. Exercising moderately — meaning that you can still carry on a conversation during your activity — is optimal. You’re working hard enough, but not so hard that you have to stop early.
RATING OF PERCEIVED EXERTION
Another measure of intensity is perceived exertion, which is how hard you feel you’re working. You should base it on your own perception of your heartbeats, breathing rate, sweating, and feelings of fatigue. Although it’s a subjective measure, your exertion rating is a reasonable estimate of your actual heart rate (pulse) during activities.
HEART RATE RESERVE
A third method to monitor exercise intensity uses a target heart rate during your workouts. Having a target allows you to use the latest apps or monitoring devices to get the most out of your activities, especially if your find that having a target is motivating.
What’s your heart rate reserve? Basically, your reserve is just the total amount you can raise your pulse, or the difference between your heart rate at rest and how high it can go.
Figuring out your target heart rate by using this method is better than using a percentage of your maximal heart rate, and it isn’t as complicated as it seems at first. To use this method, you need to know what your maximum heart rate (MHR) is. It’s best if you have that measured during a maximal exercise test, but you can also estimate it quite easily. You also need to know your true resting heart rate (RHR). This measurement is your pulse rate right after you wake up and before you’ve gotten out of bed in the morning.
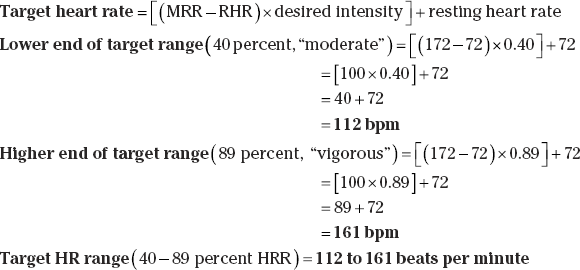
Here are the relevant equations to figure out your exercise intensity target:
- Heart rate reserve (HRR) = Maximum heart rate – resting heart rate
- Percent HRR = HRR × desired intensity (percentage as decimal)
- Target heart rate = [HRR × target intensity] + resting HR
- Estimated maximum heart rate = 220 – Age, or = 208 – (0.7 × Age)
Following is a sample calculation of 40-89 percent of heart rate reserve for a 48-year-old woman.
- Resting HR (RHR): 72 beats per minute (bpm)
- Maximum HR (MHR): 172 bpm (estimated as 220 – age)
Duration (how long)
To burn an equivalent number of calories and to manage your blood glucose, you have to do lower-intensity exercise for longer than you would one at a higher intensity. The standard recommendation is 30 minutes of moderate-intensity work most days of the week, but doing most activities for longer lowers your blood glucose more. The effect is more similar if, and only if, you use up about the same number of calories doing an activity at any intensity.
Here are some key points about your blood glucose and how long you exercise:
- When you work out longer, you usually have larger drops in blood glucose during mild and moderate exercise.
- Doing any exercise for longer tends to drop blood glucose more, but really long activities have effects that can last a day or two.
- Your glucose responses also depend on whether you’re already trained for a specific activity (and use more fat as fuel).
- Blood glucose responses to vigorous activity are more variable, but it depends on how long you do such activity.
- Your responses may also vary if you haven’t eaten for a while or exercise first thing in the morning, regardless of how long or hard your exercise is.
- How long each of your workouts lasts may not be as critical as the total duration in a day when it comes to managing blood glucose.
Frequency (how often)
Being active every day is generally better for your blood glucose. The effects of aerobic exercise last 2 to 72 hours, but usually on the shorter end of that range. That means your insulin action usually starts to go down when you go more than two days without being active, and your blood glucose can creep up. Being active daily is best for improving insulin action and more than once during each day can also be helpful.
As long as you do the same total amount of activity, whatever you’re doing likely has the same blood glucose benefits whether you do it daily or every other day, at least if you have type 2 diabetes. That’s like doing either 30 minutes a day or a full hour every other day. Not surprisingly, doing more total exercise overall (through various combinations of exercise duration, intensity, and frequency) can improve your blood glucose and insulin action even more. Exercising with type 1 diabetes can result in more variable blood glucose levels unless you balance out your food and insulin doses.
Timing (when you work out)
The time of day you exercise also affects how your blood glucose responds. Your body is temporarily more insulin resistant first thing in the morning when you have higher levels of cortisol and other hormones that help your liver keep your blood glucose stable overnight. Exercising before breakfast may not have the glucose-lowering effect that you expect.
For instance, in men treated with oral type 2 diabetes medications, doing one hour of moderate cycling barely changed their blood glucose when they exercised before breakfast. But it dropped dramatically (down to normal) when they waited two hours after breakfast to exercise.
On the other hand, if you tend to drop too low during activities, exercising in the early morning may work to prevent low blood glucose. Moderate walking and similar exercises after dinner also help prevent spikes in blood glucose then, more so than doing the same exercise before dinner.
The largest drops in blood glucose often occur when you exercise longer (at least 30 minutes) and begin working out within one to two hours after eating, which is when insulin levels are at their highest. Knowing when your injected or pumped insulin (or even the insulin your own pancreas releases) is peaking and taking your doses into account can help you predict such changes.
If your doses are too high, insulin may make your blood glucose go too low during exercise. If you exercise shortly after eating breakfast and taking insulin, your insulin dose will affect your levels of circulating insulin. At least in one study, exercisers with type 1 diabetes who did 60 minutes of moderate cycling starting 90 minutes after taking their regular dose with an insulin pump and eating breakfast had to lower their rapid-acting insulin meal boluses by 50 percent and reduce basal insulin to nothing during the activity. If they did the same exercise in the afternoon, they needed to reduce their meal bolus insulin by even more. Any changes you may need to make to your insulin need to be unique to you, though, and could be more or less than the ones from that study.
If you exercise for long enough in the morning before eating, you can develop hypoglycemia. Doing longer early morning exercise without eating anything beforehand isn’t a good idea for that reason. In many people with diabetes, their carbohydrate stores in their liver are lower than normal, leading them to rely more on making new glucose to keep blood glucose constant, which doesn’t always work well during activities that last a long time.
If you exercise in the evening, one benefit is that when you wake up, your fasting blood glucose may be lower because of the residual insulin sensitivity that came from exercising before bedtime. Evening exercise can also lead to a higher risk of hypoglycemia while you’re asleep, though, and you may need to adjust your food intake or insulin doses to compensate for that decrease.
Training effects (how fit you are)
After you train doing the same activity for several weeks, your blood glucose doesn’t drop as much as it did when you first started because training increases your body’s ability to use fat. Using more fat decreases how much muscle glycogen and blood glucose you use doing the same exercise after your muscles have adapted. This training effect is evident when you have diabetes because you find need to take in fewer carbohydrates for the same activity after several weeks or to lower your insulin less (if you take any).
This change in fuel use explains why you may need more carbohydrate to keep your blood glucose stable when you first start an activity but less after doing it for several weeks. But if you work out harder to reach the same relative intensity (for example, if reaching 65 percent of HRR after training requires you to do a harder workload than at the start), your blood glucose use during the activity will likely be nearly as high as before.
These training effects are sport-specific, which means that if you’ve been walking and then decide to try a new activity like swimming, your blood glucose will probably drop more during swimming until you’re trained at that.
Accounting for Other Factors
Just when thought you had it all figured out, you need to take some other possible factors into account. Here are the other things that can change your blood glucose responses that you need to consider.
Environment
Whether it’s hot, humid, or cold outside when you exercise or you’re on top of a mountain (at high altitude), environmental extremes can affect how your blood glucose responds. Usually any environmental extreme causes your body to use more carbohydrates (and blood glucose), although being at very high altitude (over 15,000 feet) can make you insulin resistant, particularly if you develop acute mountain sickness.
Insulin regimen changes
A normal response to being active is that insulin levels in the body decrease during the activity. If you have to inject or pump insulin, lowering the level of insulin in your blood during exercise isn’t as easy.
Because muscle contractions allow your muscles to take up glucose without insulin, too much insulin along with the effects of muscle activity can equal a rapid decrease in blood glucose levels. The effects of the two are additive.
Of course, any changes you need are dependent on your starting blood glucose and how hard and how long you choose to work out at any given time. Starting out at higher intensity requires fewer changes, as do shorter activities.
Bodily concerns
Many other factors can influence your blood glucose responses to any given workout. If you’re sick or have an infection, your blood glucose may go up. If you’re mentally stressed out or upset, dehydrated, or in the second half of your menstrual cycle (women only), it may also go up.
If you’re in the first half of your menstrual cycle, have been following a low-carbohydrate diet, or have worked out recently, it may go down instead. Trying to anticipate the effects of each of these factors at any given time can be overwhelming.
Hypoglycemia-associated autonomic failure (HAAF)
People with type 1 diabetes have a higher risk of getting low during exercise when they have hypoglycemia-associated autonomic failure (HAAF), a poorly understood phenomenon. In a series of studies over the years, researchers have found that when individuals who use insulin do exercise, their bodies don’t release as many of their glucose-raising hormones as usual the next time that they exercise or develop hypoglycemia (the same day or even the next day). The same thing happens when you’ve had a bad low blood glucose (that is, one that is below 65 mg/dL, lasts a long time, or someone else has to help you treat) in the prior 24 hours and you exercise.
What experiencing HAAF means is that when you’re doing successive days of exercise, you may need to lower insulin further or eat more to prevent hypoglycemia. And the same applies if you ever have a bad bout of hypoglycemia within a day or two before you work out. Thankfully, mild hypoglycemia doesn’t have the same lasting effects and usually doesn’t cause HAAF to occur.
 The glucose-raising hormones the body releases during exercise (and fasting) include epinephrine (more commonly known as adrenaline), norepinephrine, and glucagon. Specifically, the hormone release comes from the sympathetic arm of your nervous system — that’s the one that helps your body to respond to physical or mental stressors with an increased heart rate (pulse). It’s the fight-or-flight system that gets you moving quickly. Other hormones that factor in more during longer workouts include growth hormone and cortisol.
The glucose-raising hormones the body releases during exercise (and fasting) include epinephrine (more commonly known as adrenaline), norepinephrine, and glucagon. Specifically, the hormone release comes from the sympathetic arm of your nervous system — that’s the one that helps your body to respond to physical or mental stressors with an increased heart rate (pulse). It’s the fight-or-flight system that gets you moving quickly. Other hormones that factor in more during longer workouts include growth hormone and cortisol. Insulin is the only hormone that lowers blood glucose, while all the others raise it either directly or indirectly.
Insulin is the only hormone that lowers blood glucose, while all the others raise it either directly or indirectly. Working out can be an effective way to lower your blood glucose when it gets higher than you want it to be.
Working out can be an effective way to lower your blood glucose when it gets higher than you want it to be. After these hormones wane, your blood glucose can easily drop later while your body is restoring the muscle glycogen that you used during your workout. Beware of later-onset lows after intense exercise if you take insulin.
After these hormones wane, your blood glucose can easily drop later while your body is restoring the muscle glycogen that you used during your workout. Beware of later-onset lows after intense exercise if you take insulin.