Chapter 16
NOISE
Robert A. Dobie
About five to nine million Americans had potentially hazardous noise exposures in the workplace in the 1980s;1,2 massive job reductions in manufacturing in the United States since then have surely reduced the number at risk. Noise can be annoying and distracting. It interferes with spoken communication and masks the warning signals necessary for safety and productivity. As one of several generalized stressors, noise may contribute to cardiovascular disorders. However, the most important and best-characterized effect of excessive noise exposure is hearing loss. It is widely believed that reducing noise to a level low enough to prevent hearing loss will also prevent its other harmful effects (some important exceptions to this rule will be noted later). Therefore, this chapter will primarily deal with noise-induced hearing loss (NIHL), with special emphasis on risk assessment and prevention.
OCCUPATIONAL SETTING
Excessive noise is produced by an almost infinite variety of processes—anything that cuts, grinds, collides, explodes, or just moves (itself, another object, or a gas or liquid) will make noise. The industries listed in Table 16.1 are responsible for much of the hazardous occupational noise exposures in the United States. In some industry groups such as fishing, forestry, construction, transportation, trade, and services, fewer than half of workers receive hazardous exposures. According to surveys, >50% of workers in such industries as textiles, lumber and wood, and mining receive hazardous exposures.1
TABLE 16.1 Some industries with risks of hazardous noise exposure.3
| Construction |
| Manufacturing |
| Ship building |
| Mining |
| Agriculture |
| Textiles |
| Utilities |
| Paper |
| Machining |
| Forestry |
| Landscaping |
| Paper mills |
| Transportation |
| Stone cutting |
| Furniture |
| Oil and gas |
| Airports |
Although these survey results are interesting, they are of limited use to the occupational physician. No industrial sector is completely free of hazardous noise exposures. Only assessment of individual workplaces—or, even better, individual workers’ exposures—can accurately identify persons at risk for NIHL.
MEASUREMENT ISSUES
Fortunately, risk to hearing (unlike annoyance, sleep deprivation, and some other effects of noise) is relatively well predicted by three measurable physical properties of sound: frequency, intensity, and time. In general, more hazardous sounds are louder, longer, and more concentrated in the frequency range where we hear best.
Frequency
A vibrating object moves air molecules back and forth, creating a sound wave that propagates outward. The number of complete cycles or oscillations per second is the frequency of the sound, measured in hertz (Hz) or kilohertz (1 kHz = 1000 Hz). Normal young people can hear sounds ranging in frequency from about 20 Hz to 20 kHz, but our best hearing is in the 1–5-kHz region.
Only artificial objects like tuning forks and electronic oscillators put out pure tones, that is, sounds having energy at only one frequency. Natural sounds like speech contain many frequencies simultaneously; indeed, it is the relative intensities of these different frequencies, or harmonics, that permit us to recognize speech sounds or to distinguish one musical instrument from another.
Intensity
Sound intensity (energy flow per unit area per unit time) is difficult to measure directly but is directly proportional to the square of sound pressure, which is easily measured and thus much more commonly reported, in units of pascals (Pa) or micropascals (1 Pa = 106 μPa). The ratio between the softest audible sound pressure (20 μPa) and the loudest tolerable sound pressure (20 Pa) is a million to one. To avoid having to either switch units or use too many zeroes, this pressure range is compressed by using logarithms, just as when converting hydrogen ion concentration to pH.
Specifically, the decibel (dB) is defined as

For general-purpose sound level measurements, P0 is set at 20 μPa, a barely audible level for the best-heard frequencies (inaudible for higher and lower frequencies). Decibels measured with P0 = 20 μPa are identified as “sound pressure level” (SPL). Thus, a sound pressure (P) of 20 μPa would be 0-dB SPL.
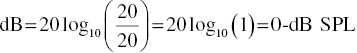
Sounds less intense than 20 μPa would represent negative values in dB SPL. In other words, 0 dB does not represent the absence of sound but a sound whose pressure equals the reference pressure level. A very intense sound of 20 Pa (barely tolerable) would have a sound pressure level of 120-dB SPL:
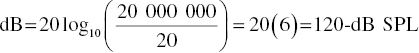
Since decibels are logarithmic, they combine in ways that may seem surprising. For example, if two sound sources which individually produce 80-dB SPL are turned on simultaneously, the result is only a 3-dB increase, to 83-dB SPL, rather than a doubling, as might be expected. Since doubling the distance from a sound source reduces the acoustic energy flow per unit area by a factor of 4 (area is proportional to distance2), sound pressure level decreases by 6 dB under ideal circumstances. However, this only holds true outdoors; because of reverberation, sound levels change much less in most indoor workplaces as one moves away from a sound source.
Sound pressure level is not enough to specify hazard to hearing: 120-dB SPL would be extremely loud (and hazardous) at a well-heard frequency such as 2 kHz, but it would be inaudible (and harmless) at 50 kHz. One could measure the sound pressure in each of several audible octave bands (an octave comprises a 2 : 1 frequency ratio, e.g., 500–1000 Hz), but this would be too cumbersome. Instead, hearing conservation professionals universally use decibels on the A-scale to combine frequency and intensity for a single-number measurement of potential hazard. A sound level meter operating in the A-scale mode uses electronic filters to cut out inaudible frequencies altogether, to partially remove poorly heard frequencies, and to give full weight to the best-heard frequencies (1–5 kHz). Thus, two sounds with identical sound pressure levels could have different A-scale readings; the one with most energy in the 1–5-kHz range would be higher, more accurately reflecting the risk of NIHL (Table 16.2).
TABLE 16.2 Sound pressure level versus A-scale.
| Source | dB SPL | dBA |
| Jet | 90 | 92 |
| Diesel | 90 | 85 |
Sound level meters can be deceptively easy to use. However, microphone care, selection, calibration, and placement, timing of measurements, and proper interpretation of data are just a few of the variables that can affect the reliability and validity of sound level measurements. Use of these instruments is normally best delegated to acoustic engineers, industrial hygienists, audiologists, or others who have been trained in their use.
Time
Even an A-scale reading is not enough; 5 minutes/day at 100 dBA is much less hazardous than 8 hours/day at 90 dBA. Using the logarithmic decibel scale, a 3-dB change is equivalent to a doubling (or halving) of sound energy per unit time. If the hazard were proportional to the total sound energy received by the ear, factoring in time would be simple; a twofold increase in exposure time would be equivalent to a 3-dB increase in sound pressure level (dBA). Indeed, many experts support the use of a 3-dB exchange rate to relate time and level to overall hazard. However, there is considerable evidence that intermittent exposures are less hazardous than continuous exposures at the same level and total duration.4 Since high-level exposures are often interrupted, the Occupational Safety and Health Administration3(OSHA) has adopted a 5-dB exchange rate in an attempt to incorporate the protective effects of intermittency. Under OSHA regulations, for example, a 90-dBA exposure for 8 hours is considered as hazardous as a 95-dBA exposure for 4 hours (Table 16.3).
TABLE 16.3 Time–intensity trading.
Source: Adapted from OSHA General Industry Standard 29 CFR 1910.95, Table G-16.
| Level (dBA) | Duration (hours) |
| 90 | 8 |
| 95 | 4 |
| 100 | 2 |
| 102 | 1.5 |
| 105 | 1 |
| 110 | 0.5 |
| 115 | 0.25 or less |
Time-weighted average (TWA) is a useful single number characterizing a day’s exposure in terms of frequency, intensity, and time. This is the level (in dBA) that, if present for 8 hours, would present a hazard equal to that of the exposure in question. Both of the previously mentioned exposures (90 dBA/8 hours and 95 dBA/4 hours) would be described as 90-dBA TWA.
Calculating TWA for varying exposure times (e.g., 6 hours, 37 minutes) and combinations of exposures at different levels and durations is mathematically straightforward but cumbersome. Fortunately, most acoustic hazard assessment now uses noise dosimeters, wearable devices that use built-in microprocessors to automatically calculate TWA for a day’s exposure.
EXPOSURE GUIDELINES
The Occupational Safety and Health Act,5 modified by the OSHA Hearing Conservation Amendment,3 established extensive regulations for industries in the United States. The mining and railroad industries are subject to separate federal regulation by the Mine Safety and Health Administration and the Federal Railroad Administration, respectively.6
OSHA defines the permissible exposure limit (PEL) as 90-dBA TWA. Higher exposures must be reduced by engineering or administrative controls or by the use of hearing protection devices (HPDs). OSHA also recognizes a borderline or low-risk range of exposures at 85–90-dBA TWA. Workers with daily exposures >85-dBA TWA must be covered by hearing conservation programs (HCPs), which will be discussed later.
Exposures are sometimes described in terms of noise dose, where the PEL (90-dBA TWA) is equivalent to a noise dose of 1.0 (or 100%). Exposures of 85-dBA TWA and 95-dBA TWA would be described as noise doses of 0.5 (50%) and 2.0 (200%), respectively. TWA and noise dose are interchangeable descriptions of noise exposure hazard, and most dosimeters will read out whichever the user prefers. OSHA requires that dosimeters incorporate all continuous, intermittent, and impulsive sounds between 80 and 130 dBA into their calculations.
These guidelines are intended to protect almost all covered workers from substantial occupationally related NIHL. However, a few highly susceptible workers may incur mild NIHL at exposure levels below the PEL. Some workers are not covered by OSHA regulations; others may increase their risk by moonlighting at a second noisy job. Nonoccupational exposures, especially hunting and target shooting, are often more hazardous to hearing than workplace exposures.
Observance of OSHA noise exposure guidelines will not always protect against safety hazards other than NIHL. For example, a brief period of intense noise (1 hour per day at 95 dBA) would neither exceed the PEL nor require an HCP. However, during that period, speech communication would be severely disrupted, and warning signals could become inaudible.
Speech interference can be a useful clue to a potentially hazardous noise environment. People raise their voices to be heard over loud background noises. Most will need to shout to converse at arm’s length at sound levels >85 dBA; this is also the level at which OSHA requires hearing conservation programs for workers with 8-hour exposures.
NORMAL PHYSIOLOGY
The outer ear includes the pinna or auricle (the visible part) and the ear canal, a skin-lined tube leading to the eardrum; together, these structures provide resonances that enhance transmission of certain frequencies (around 3 kHz) and impair others. These effects are rather small; traumatic or surgical alterations of outer-ear structures produce only minimal hearing changes. Complete blockage of the ear canal with earwax or a foreign body will cause mild to moderate hearing loss.
The middle ear is separated from the ear canal by the eardrum, a thin membrane connected to a chain of three tiny bones, or ossicles: the malleus, incus, and stapes. The footplate of the stapes, which transmits the vibrations of the eardrum and ossicular chain into the inner ear, is much smaller in area than the eardrum. Thus, the pressure exerted on the inner-ear fluids is increased or amplified, much as the difference in cross sections amplifies the force in a hydraulic system. Without this ingenious mechanical arrangement, most of the sound energy reaching the inner ear would be reflected back into the air. Two small muscles attach to the malleus and stapes and contract in response to loud sounds. This acoustic reflex stiffens the ossicular chain, impairing transmission of low-frequency sounds and slightly enhancing transmission of sounds above 2 kHz; the reflex offers some protection against NIHL, at least for low frequencies (1 kHz and lower). The middle ear is an air-containing space that receives a regular air supply via the Eustachian tube. Disruptions of the middle-ear mechanism (perforated eardrum, fixed or disconnected ossicles, and fluid-filled middle-ear space) can cause mild to moderately severe hearing loss.
Hearing loss caused by outer-ear or middle-ear disorders is called conductive, because it interferes with normal air conduction of sound to the inner ear. Sounds presented by an oscillator held directly against the skull reach the inner ear by bone conduction and are heard normally by people with conductive hearing loss.
The inner ear contains organs of both hearing and balance; the latter will not be discussed here. The hearing organ, or cochlea, includes a spiral basilar membrane encased in a snail-shaped cavity in the temporal bone; on that membrane are spirally arranged hair cells, which change mechanical fluid vibrations into nerve impulses traveling to the brain. The hair cells of the base of the cochlear spiral respond best to high frequencies, whereas those at the apex respond only to low frequencies. At any given point along the spiral, there are three rows of outer hair cells, essential for hearing soft sounds, and one row of inner hair cells, which connect to almost all the nerves carrying sound to the brain.
Inner-ear hearing losses are usually lumped together as sensorineural, although the vast majority affect the hair cells (sensory) and very few directly affect the nerve cells (neural). Outer hair cells are more vulnerable than inner hair cells to most diseases and injuries causing sensorineural hearing loss, including age-related hearing loss, NIHL, and ototoxic drugs.
PATHOPHYSIOLOGY OF NOISE-INDUCED HEARING LOSS
Most hazardous noise exposures cause reversible inner-ear injury at first. Hair cells may lose their normal ability to respond to sound, accompanied by a temporary elevation of threshold (the softest sound that can be heard), or temporary threshold shift (TTS), lasting hours to days. Individuals often experience this as a muffling of sound, together with tinnitus (i.e., ringing in the ears) and fullness. After repeated TTS-inducing exposures, permanent hair cell loss and noise-induced permanent threshold shift (NIPTS) occur. At least in some animals, exposures that cause very large TTSs can cause immediate and permanent loss of auditory nerve cell function without measurable threshold shifts.7 Some very brief but intense exposures, especially involving impulsive sounds such as gunfire, can cause immediate permanent threshold shift (PTS) without intervening TTS; this is called acoustic trauma, as distinct from ordinary NIHL.
We might expect NIHL to affect hearing for the same frequencies contained in the offending sound, and this is true, up to a point. However, most occupational and recreational noises contain a broad spectrum of frequencies; thus, the frequency pattern of NIHL is determined more by the sensitivity of the ear than by the frequency content of the noise. Other factors, such as the acoustic reflex, probably also play a role; the result is that for almost all cases of NIHL and acoustic trauma, the first and most severe effects are seen in the 3–6-kHz region.
Hearing loss is usually represented using an audiogram, a graph of hearing sensitivity (the softest sounds a patient can hear) as a function of frequency. The vertical axis plots thresholds in dB hearing level (HL). Recall that dB SPL implies a reference level of 20 μPa and that dBA represents a weighted sum across the audible range of frequencies, suitable for noise hazard assessment. In contrast, dB HL implies a reference level of normal human (young adult) hearing; for each audiometric frequency, 0-dB HL is average normal hearing, whereas thresholds above 15-dB HL are abnormal for young adults (although not necessarily handicapping or even noticeable).
Figure 16.1 shows median audiograms for a group of retired jute mill workers with noise exposure above 100 dB and an age- and gender-matched control group.8 The well-known 4-kHz dip is evident in the noise-exposed audiogram. NIPTS is simply the decibel difference between audiometric thresholds for noise-exposed and non-noise-exposed populations.
FIGURE 16.1 Median audiograms for noise-exposed and control subjects.
For repeated exposures to occupational noise, NIPTS grows gradually. After about 10 years, the growth decelerates markedly, and NIPTS approaches a plateau. The International Organization for Standardization has published tables and formulas (ISO 19999) that describe the growth of NIPTS over time for different frequencies and exposure levels. Some selected curves from ISO 1999 are reproduced in Figure 16.2. Note that all three curves show (i) the plateau effect, (ii) that the predicted NIPTS is much greater for 4 kHz than for 1 kHz, and (iii) that 40 years of exposure at 85 dBA produces only slight changes at 4 kHz (and none at 1 kHz). These curves represent median NIPTS; that is, half of exposed persons would be expected to show greater losses, and half would show lesser losses.
FIGURE 16.2 Noise-induced permanent threshold shift as a function of time for different frequencies and exposure levels.
With prolonged exposure (or immediately in cases of acoustic trauma), frequencies below 3 kHz may demonstrate substantial losses. The AMA and most workers’ compensation programs consider the speech frequencies to be 0.5, 1, 2, and 3 kHz, because losses for these frequencies interfere with everyday speech communication, in quiet or noisy backgrounds.10 Most of the acoustic energy in normal speech is concentrated below 1 kHz, especially in vowel sounds. However, most of the information content is above 1 kHz, where the consonants have their peak energies. Thus, people with NIHL (or any other high-frequency sensorineural hearing loss) will often complain that they can hear speech but cannot understand it. This can lead to social isolation and depression.
NIPTS, as plotted in Figures 16.1 and 16.2, has not been directly measured in human epidemiologic studies. Rather, the hearing levels of a group of noise-exposed workers (known intensity and duration) are compared to hearing levels for non-noise-exposed workers with similar age, gender, and other characteristics. The differences between these two groups are reported as NIPTS. Implicit in this approach is the fact that people lose hearing as they age (high frequency > low frequency, men > women) and the assumption that age-related permanent threshold shift (ARPTS) and NIPTS are additive in decibels.
Figure 16.3 shows median ARPTS curves for men and women, from the US database included in ISO 1999, averaged across the speech frequencies. Note that ARPTS is an accelerating process. Contrast this with Figure 16.4, which shows median speech frequency NIPTS for exposures ranging from 85 to 100 dBA. NIPTS decelerates; approximately 60% of the 40-year total is present after 10 years.
FIGURE 16.3 Speech frequency age-related permanent threshold shift as a function of age and gender.
FIGURE 16.4 Speech frequency noise-induced permanent threshold shift as a function of time for different exposure levels.
Susceptibility to both age-related hearing loss and noise-induced hearing loss varies widely. It seems likely that genetic differences underlie much of this variation,11 but when those with worse hearing are found to have particular genetic markers, it is difficult to know whether these are markers for age effects or noise effects.12 To date, genetic tests have not been shown to assist in the diagnosis or prevention of NIHL.
DIAGNOSIS
The American College of Occupational and Environmental Medicine13 has enumerated a series of criteria for the diagnosis of occupational NIHL, which they have described as:
- Sensorineural
- Bilateral and symmetrical
- Not profound
- Not progressive after cessation of noise exposure
- Decelerating
- Greatest in 3–6-kHz range
- Stable after 10–15 years in high frequencies
- Less severe after interrupted exposures than after continuous daily exposures of the same level and duration
Occupational NIHL is too frequently diagnosed casually, without adequate attention to the patient’s noise exposure history, both occupational and nonoccupational. Employers and HCP managers can improve the quality of medical reports by providing examining physicians with noise exposure data, especially dosimetry, relevant to the individuals being evaluated.
Except in very young workers, noise and aging must be considered together. At retirement age, most workers exposed at levels below 100 dBA (the vast majority of noise-exposed workers) will have more age-related loss than noise-induced loss. Statistical methods for estimating the relative contributions of aging, various periods of occupational exposure, nonoccupational exposure, and other otologic disorders have been developed.14
TREATMENT
No medical or surgical treatment has been shown to be helpful for NIHL in humans, and none is usually offered. Some authorities have recommended treatments aimed at improving cochlear blood supply in cases of acoustic trauma, and multiple antioxidants, vitamins, and minerals have been shown to partially prevent hearing loss in animals when given prior to noise exposure,15 but NIHL remains a disorder without medical treatment of proven efficacy.
NIHL can be palliated with hearing aids and assistive listening devices, such as “TV ears.” However, hearing aids rarely if ever compensate completely for sensorineural hearing loss; they can amplify inaudible sounds into the patient’s audible range, but distortions usually persist, especially with loud sounds.
The lack of available medical treatment and the inadequacy of hearing aids combine to emphasize the role of prevention. A well-organized HCP can dramatically reduce the risk of NIHL and acoustic trauma for motivated workers.
MEDICAL SURVEILLANCE
The Hearing Conservation Amendment3 requires HCPs for all workers with exposures exceeding 85-dBA TWA. An HCP must include baseline and annual pure-tone air-conduction audiometry (0.5, 1, 2, 3, 4, and 6 kHz), with monitoring for standard threshold shifts (STS), defined as a 10-dB or greater change for the worse in either ear for the average of 2, 3, and 4 kHz. In determining whether an STS has occurred, age correction is optional. Audiometry within the HCP (usually on-site or in a mobile audiometric van) does not require bone conduction, speech, or middle-ear tympanometric tests.
Otoacoustic emissions (OAEs) are soft sounds emitted by the healthy cochlea in response to acoustic stimulation (they were initially called “cochlear echoes”). People with weak OAEs appear to be more susceptible to NIHL,16 perhaps because they have already suffered subclinical noise-induced cochlear damage, but OAEs have not been shown to be useful in HCPs, either to replace or to supplement conventional pure-tone audiometry.
OSHA requires every HCP to be supervised by an otolaryngologist or other physician, or by an audiologist. If an STS occurs, the professional supervisor may elect either to retest within 30 days or to accept the STS without confirmation. An accepted or confirmed STS requires the initiation of earplug or earmuff use for all workers in the 85–90-dBA TWA zone who were not previously required to use HPDs, or the refitting of HPDs for those previously using them. Employee notification and counseling are required for all STSs. When the 2-, 3-, and 4-kHz average is 25 dB or greater after an STS, OSHA requires that the STS be recorded on Form 300, unless it is determined not to be work related.17
The National Institute for Occupational Safety and Health (NIOSH) published the revised Criteria for a Recommended Standard: Occupational Noise Exposure in 1998,18 reaffirming their support for an 85-dBA recommended exposure limit. With a 40-year lifetime exposure at 85 dBA, NIOSH estimates an excess risk of developing “material hearing impairment” of 8%—considerably lower than the 25% excess risk they calculate at the 90-dBA PEL currently enforced by OSHA. However, NIOSH changed their definition of material hearing impairment, to give more weight to high frequencies and less weight to low frequencies, prior to calculating excess risk. When excess risk is calculated using the definition most widely used in the United States (that of the AMA10), the corresponding figures are 3% for 85 dBA and 8% for 90 dBA.6
NIOSH now recommends an exchange rate (ER) of 3 dB for the calculation of TWA exposures to noise. The 5-dB exchange rate remains in the OSHA regulations and appears to be more accurate than the 3-dB exchange rate for intermittent and fluctuating exposures,4 but the most appropriate exchange rate remains controversial.4 NIOSH also recommends a new criterion for significant threshold shift—an increase of 15 dB in the hearing threshold level (HTL) at 500, 1000, 2000, 3000, 4000, or 6000 Hz in either ear, as determined by two consecutive audiometric tests. OSHA has not adopted this recommendation. NIOSH no longer recommends age correction on individual audiograms. This practice is felt by some not to be scientifically valid; on the good side, it can decrease false positives (STSs not due to noise), but on the bad side it can increase false negatives, delaying intervention to prevent further hearing losses in workers whose HTLs have increased because of occupational noise exposure. OSHA still allows age correction as an option.
Referral is not required for STSs, but it is required when the program supervisor suspects a medical problem affecting the ears or believes that the audiometric data are questionable. The American Academy of Otolaryngology—Head and Neck Surgery19 has published criteria for otologic referral from HCPs that have been adopted by many companies. These criteria recommend referral based on otologic symptoms, baseline audiometry (with special emphasis on substantial asymmetries, which often indicate serious otologic disease), and changes seen on periodic audiometry (including the lower frequencies, where communicatively significant or medically serious hearing losses are more likely to be seen).
PREVENTION
The OSHA Hearing Conservation Amendment requires more than periodic audiometry and medical or audiologic surveillance. After all, audiograms do not prevent hearing loss; they only measure it. Health professionals responsible for an HCP should carefully review the entire standard. The additional important elements of an HCP include:
- Risk assessment using sound level meters or dosimetry
- Education and motivation of workers
- Exposure reduction through engineering control, administrative controls, and use of HPDs
- Recordkeeping
Education and motivation are important for two reasons. First, if the HCP includes the use of HPDs, there may be significant worker resistance and poor compliance unless they believe that hearing is really at risk, is worth saving, and can effectively be saved. Second, many—perhaps most—industrial workers have potentially hazardous nonoccupational noise exposures; if they fail to reduce their recreational exposures, NIHL will continue to accrue despite reduction of on-the-job exposures to safe levels.
Engineering controls are obviously the most desirable way to reduce occupational noise exposures. If all workplaces can be brought below 85 dBA and no workers spend >8 hours per day on the job, the employer no longer needs an HCP at all. Lesser reductions are also valuable if they reduce the number of workers who must be enrolled in the HCP, the number who must use HPDs, or the HPD performance requirements. Cost is sometimes an issue, but newer equipment is often designed to reduce noise output.
Administrative controls involve reducing the individual’s exposure to hazardous noise. Most experts in HCP design and administration have found that these changes are rarely feasible without unacceptable disruption of work routines.
In practice, then, most HCPs rely heavily on the use of HPDs to reduce exposures. Earplugs and earmuffs can both be effective if properly fitted and used. OSHA requires that employers offer their workers a variety of HPDs, recognizing that individuals and their jobs vary too much to permit specification of a single HPD for all. HPDs are rated by a noise reduction rating (NRR), which estimates the number of dB of attenuation obtained by proper use. However, most authorities believe that NRR numbers are usually too generous to apply to real-world situations. For conservative application, many recommend using half the NRR as a guide. For example, workers in a 100-dBA environment who use earplugs with a 30-dB NRR should be considered to be exposed to ~85 dBA (100 – 15 dB). Simple observation by supervisors is not enough to ensure proper use of HPDs. Earplugs are sometimes trimmed or perforated by uncooperative workers, and earmuffs can be stretched to reduce the spring force holding the muffs to the head, making them more comfortable but less protective. In either case, the worker would pass a cursory inspection.
It is now possible to measure HPD attenuation, as well as daily effective (“behind-the-HPD”) exposures, for individual workers in field situations; this technology could help supervisors to detect and remediate cases where HPDs are inadequately fit. However, in a recent nonrandomized trial, workers using a device that gave them and their management daily feedback on their effective daily exposures did not have significantly less future threshold shift than control group workers, after appropriate statistical controls.20
Workers should be urged to use HPDs on and off the job whenever they are exposed to loud noises (generally, when it is necessary to raise the voice to converse at arm’s length). For many workers, nonoccupational exposures—especially shooting—are more hazardous than occupational exposures.
The speech interference and safety risks (difficulty in hearing warning signals) of loud noise have already been mentioned. Simply making the desired signal louder than the background noise, for example, by shouting, can alleviate this problem. Once this has been done, the use of HPDs will not further degrade listening performance in normally hearing people. Both the signal and the noise will be reduced in intensity by the HPD, but as long as both are audible, the signal-to-noise ratio will be the same as without the HPD.
Persons with preexisting high-frequency hearing loss may have poorer detection and discrimination of speech and warning signals when using HPDs. This occurs because the HPD may actually make high-frequency signals (including the high-frequency portions of speech) inaudible.
Intermittent noise poses special safety hazards because what is protective in noisy environments may disrupt communication in quiet ones. Workers who wear HPDs during quiet periods may have difficulty in hearing and understanding normal speech. HPDs can make the worker’s own voice seem louder (try plugging your ears with your fingers while speaking at a constant level); thus, workers may speak less loudly than normal when wearing HPDs in quiet environments.
These risks may be managed by implementing special communication strategies, such as those often used in radio communication: using a restricted message set to increase redundancy, spelling out words, and having important messages repeated back by the listener, to mention a few. Communication headsets are available that combine an earplug or earmuff, for attenuation of ambient noise, with a built-in radio receiver. In addition, active HPDs are available as earmuffs with built-in microphone–amplifier circuits. In quiet environments, these units amplify sound to overcome the attenuation of the earmuff, while in high levels of noise, the amplifier is automatically disabled. These units are particularly helpful for workers with hearing loss, who may need amplification in quiet places, but still need protective attenuation in noisy ones. Provision of this type of equipment may constitute the sort of accommodation necessary to comply with the Americans with Disabilities Act (ADA). Earmuffs with active noise reduction circuits are also available. These headsets use noise cancellation technology, actively decrease low-frequency exposures, and are particularly helpful for pilots in general aviation (small planes) where cabin noise is dominated by low frequencies.
References
- 1. Franks R. Number of workers exposed to occupational noise. Semin Hear 1988; 9:287–97.
- 2. Dobie RA. The burdens of age-related and occupational noise-induced hearing loss in the United States. Ear Hear 2008; 29:565–77.
- 3. US Department of Labor, Occupational Safety and Health Administration. Occupational noise exposure: hearing conservation amendment final rule. Fed Regist 1983; 48:9738–84.
- 4. Dobie RA, Clark WW. Exchange rates for intermittent and fluctuating noise exposures: a systematic review of studies of human permanent threshold shift. Ear Hear 2014; 35:86–96.
- 5. US Department of Labor, Occupational Safety and Health Administration. Occupational safety and health standards, national consensus standards and established federal standards. Fed Regist 1971; 36:10518.
- 6. Jayne TR. Legal remedies for hearing loss. In: Dobie RA, ed. Medical-legal evaluation of hearing loss. 3rd edn. San Diego, CA: Plural Publishing, 2015. 243–64.
- 7. Kujawa SG, Liberman MC. Adding insult to injury: cochlear nerve degeneration after “temporary” noise-induced hearing loss. J Neurosci 2009; 29:14077–85.
- 8. Taylor W, Pearson J, Mair A, et al. Study of noise and hearing in jute weaving. J Acoust Soc Am 1965; 38:113–20.
- 9. International Organization for Standardization. Acoustics: determination of occupational noise exposure and estimation of noise-induced hearing impairment. ISO-1999. Geneva: International Organization for Standardization, 2013.
- 10. Dobie RA. The AMA method of estimation of hearing disability: a validation study. Ear Hear 2011; 32:732–40.
- 11. Konings A, Van Laer L, Van Camp G. Genetic studies on noise-induced hearing loss: a review. Ear Hear 2009; 30:151–9.
- 12. Kowalski TJ, Pawelczyk M, Rajkowska E, et al. Genetic variants of CDH23 associated with noise-induced hearing loss. Otol Neurotol 2014; 35:358–65.
- 13. Kirchner DB, Evenson E, Dobie RA, et al. ACOEM guidance statement: occupational noise-induced hearing loss. J Occup Environ Med 2012; 54:106–8.
- 14. Dobie RA. Diagnosis and allocation. In: Dobie RA, ed. Medical-legal evaluation of hearing loss. 3rd edn. San Diego: Singular Thomson Learning, 2015.
- 15. Oishi N, Schacht J. Emerging treatments for noise-induced hearing loss. Expert Opin Emerg Drugs 2011; 16:235–45.
- 16. Marshall L, Lapsley-Miller JA, Heller LM. Detecting incipient inner ear damage from impulse noise with otoacoustic emissions. J Acoust Soc Am 2009; 125:995–1013.
- 17. Dobie RA. Is this STS work-related? ISO 1999 predictions as an adjunct to clinical judgment. Am J Ind Med 2015; 58:1311–18.
- 18. National Institute for Occupational Safety and Health. Criteria for a recommended standard: occupational noise exposure. Revised criteria. DHHS (NIOSH) publication no. 98–126. Washington, DC: US Government Printing Office, 1998.
- 19. American Academy of Otolaryngology, Head and Neck Surgery, Medical Aspects of Noise Subcommittee. Otologic referral criteria for occupational hearing conservation programs. Alexandria, VA: American Academy of Otolaryngology, Head and Neck Surgery Foundation, 1997.
- 20. Rabinowitz PM, Galusha D, Kirsche SR, et al. Effect of daily noise exposure monitoring in annual rates of hearing loss in industrial workers. Occup Environ Med 2011; 68:414–18.
