]>
Chapter 10
On Securing Electronic Healthcare Records Using Hyperledger Fabric Across the Network Edge
CONTENTS
10.2 Existing Decentralized Security Methods: Can Blockchain Be Used At the Edge?
10.2.1 Current EHR System in Canada
10.2.2 Challenges with the Traditional EHR Systems
10.2.3 Security Measures for Health Records
10.3 Current Challenges Faced by the Healthcare Workers in Covid-19 Pandemic
10.3.1 Importance and Role of Medical Records During Pandemic
10.3.2 Challenges Faced by Doctors
10.3.3 Understanding the Proposed Architecture Using COVID-19 Example
10.4 Scalable Secure Management and Access Control of Electronic Health Records at the Edge
10.4.1 The Importance of Integrating Blockchain and Edge Computing?
10.5 Overview of Blockchain and Hyper Ledger Methodologies
10.5.2 Electronic Health Records (EHRs)
10.5.4 Access Control in Medical Domain
10.5.9 User Experience From Patient’s Side
10.6 Hyper Ledger-Based Proposed Architecture for Protecting Electronic Health Records
10.6.1 Proposed Architecture of the Blockchain System
10.7.1 Performance of the Proposed Model
10.1 Introduction
Recently, healthcare systems have been identified as a critical infrastructure, often targeted by malicious adversaries. Healthcare data interception due to improper handling of the patient-data may result in not only financial losses for both the care-giving entities (hospitals, clinics, physicians, nurses, insurance companies) and victims but also identity theft, damage of reputation and other social issues. While healthcare systems are currently supported by an assortment of technologies to improve the patient-experience within the entire healthcare ecosystem, numerous operational challenges still exist [1]. In particular, the challenge related to unified management of Electronic Health Records (EHRs) requires researchers to design a scalable technique to enable multiple physicians to have access to the complete health history of a given patient, at the same time, maintaining privacy of the health data. This challenge has become even more daunting recently because the patients are nowadays able to collect their own physiological and mental health data using Internet of Things (IoT) sensors and wearables, use pain-management applications and so forth, which need to be collected from their edge devices (e.g., user-smartphones), and converted and stored as EHRs. The proliferation of patients’ edge devices generating a large stream of medical data from IoT-based, remote monitoring means that it is important to secure their data across the healthcare ecosystem so that they are not exposed to third parties. In order to have a secure access control of the health data, our aim in this chapter is to put the patient in control of their respective health data, by empowering them to share which relevant physicians and other caregivers they are willing to share their data with in a unified format. The use of blockchain in various domains, including healthcare, has recently garnered much attention from government, academicians and industry [2]. Due to its ability to support such unified medical records, data security, privacy improvement and insurance decisions/transactions, the blockchain technology may be regarded as an effective solution for the aforementioned healthcare technology challenges. Apart from several function of blockchain in financial domains, it also has usage in the non-financial domains such as reputation systems [3], public services [4], protection and IoT [5, 6]. However, blockchain also faces some technological difficulties, some of them being consistency, safety and scalability [7].
Blockchain is an advanced technology which has modified the ways to store, transact and record the data. The concepts partially match to that of a conventional database; however, the only difference is that the intermediary can be avoided here. The issues of interoperability in data safety are largely studied in recent years. The critical issue is to figure out a way to enable public access to confidential health data, anonymity, safeguarding the protection of personal data and preventing abuse of data. Blockchain technology and smart contracts offer a creative and exciting way for EHRs to hold a reference. With the help of the proposed concept, patients, healthcare providers and hospitals can have better control over their data, which are collected by other organizations. In brief, blockchain has the potential to boost the safety and interoperability of EHR solutions. This chapter discusses how to use blockchain and smart contracts to develop EHR. We address some non-technical aspects that make data on health valuable first. Next, we are proposing an architecture that could boost the existing EHR structures. The key goal is to ensure safe access to patient data without permission, restricting access by third parties, and only permitting access to the patient and doctor and the medical centers.
E-Health is a value-developing technology that can access medical data remotely as well as share patient data in real-time that are collected from various sensors. This had stated that the use of EHRs had grown largely from 9% in 2008 to a peak of 96% by 2015 [8]. An EHR is typically the automated patient health data collection which has different attributes such as text documents, video, image data, etc. The main purpose of EHR systems is to store and manipulate patient data in order to monitor the health of a patient over time. For cross-EHR sharing, the question of legal interoperability arises because there are legal requirements many healthcare systems and providers have to utilize EHRs, which prohibits any medical data sharing. The absence of structured management of data and sharing contributes to a fragmentation rather than unity of personal medical data [9]. This kind of technology is important nowadays because it encourages patients to engage in activities concerning their healthcare and restore intermediaries about their health records [10]. The concepts of blockchain provide exciting prospects for technical progress to tackle these healthcare problems [11].
In short, it is decentralized, authenticated and a database that keeps a series of transactions in the form of blocks where a consensus-driven mechanism is implemented with the help of the ledger to achieve consensus between various individuals who might not be trusted. This will require any individual in the medical system, such as provider, patient, insurance company, pharmacist, to apply the required credentials and identities to get control on the blockchain. Every participant will have permission to access the ledger and other digitally collected data with the authorization of candidate or if they are sanctioned. [5]. The failure to access healthcare data is a persistent issue specially while collecting it efficiently in the provision of healthcare worldwide. The EHRs placed in position presume that one patient only visits one doctor at a clinic. Also, patients are not limited to only one doctor or clinic. In a study it was seen that on average a U.S. patient can have approximately 19 different health records, and in 2010, a study reported that patients see18.7 different doctors in their lifetime [7]. Patients are not limited to a single zone protected by EHR. People move for jobs, for recreation and they relocate for a long period of time. Individuals are also willing to protect their health by using data created by wearable gadgets.
In this chapter, we first discuss the contribution of the state-of-the-art blockchain technology and smart contracts in various practical situations of healthcare industries which is regarding data access, interoperability and management. The concept of implementing an extensive information architecture is proposed in order to maintain EHRs based on hyperledger fabric model. The hyperledger fabric model is a distributed ledger that consists of assets, chaincode, ledger features, channels, security and membership services and consensus. Setting distributed ledger of the blockchain node (assigned patient to doctor) can be used for setting up central network of the edge computing; this could be visualized as the vectorized decentralized edge computing. The act of ensuring that the patients have access to their data can be referred to as data privacy, and data accessibility ensures that the access of information is unconstrained. Data accessibility by the user always raises a concern of privacy, which should be taken into account specially in the field of healthcare [12]. The issues regarding data health interoperability are being studied more than ever [13]. One of the crucial challenges is to enable open access to sensitive health data while maintaining personal data privacy and avoiding data misuses while maintaining anonymity. Blockchain can contribute significantly in order to manage data of such patients. It is a set of distributed ledger architectures that is heavily applied for various cryptocurrency applications starting from Ethereum to bitcoin. These permission-less blockchains can affect the financial services industry by being disruptive [14]. Permissioned chains can be prone to demands of resource storage [3]. Therefore, our main contribution, in this chapter, is to use the concepts of an integrated blockchain-based architecture to address the issues related to accesibility and data privacy in healthcare. The limitation that is addressed through this chapter is – the use of permissioned blockchain integrated with off-chain storage of data which is accessed with the help of a mobile application or browser. The framework is implemented by employing an example use of healthcare data which are patient centered.
The proposed architecture consists of three parts which are the access control module based on blockchain, off-chain data storage and a role-centered web interface. The resource containing all kinds of data such as test results, diagnostic images and other paperwork of the patient are made secured through encryption which are then stored on a cloud repository in order to maximize the performance of the model and also make it economically reasonable. These methods can associate the on-chain and off-chain data without having to pay any additional computational or storage-related expense in the user edge devices, which is common aspect in blockchain architectures [15]. The smart contracts facilitate doctors and patients to provide access to their respective users with their edge device flexibly and securely. The web interfaces can then be used by the doctors and patients to carry out multiple activities such as writing a prescription, allowing the read-only access to other doctors over the patient who require the medical attention from specialists, revoke rights from doctors once the patient has acquired the treatment, patients can track their medical records from any place, check current prescription, book appointments for recommended test, etc. more easily. In order to keep track of EHRs, blockchain technology and smart contracts are employed as an effectual solution [16]. Therefore, the concerns regarding privacy and interoperability of the data can be addressed through the concepts of blockchain and smart contracts to improve EHR systems which arepropositioned in this chapter.
10.2 Existing Decentralized Security Methods: Can Blockchain Be Used At the Edge?
Blockchain technology is at the core of digital cryptocurrency and its applications are being considered for various application domains. The topic of how blockchain could be leveraged at the edge is garnering much research attention. The crucial growth of blockchain has fascinated a wide range of people starting from technology giants to manufacturers. The change from a centralized model to the decentralized model has made blockchain a foundational technology. Because of the features like decentralization, security, automation, immutability and transparency, all the agreed mental obligations and rights and ownership of assets can be recorded on the blockchain. However, there is an essential and critical disadvantage of a blockchain, i.e., lack of ability to scale. This drawback of scalability restricts to see the success of applications. Nevertheless, with the development of computing technology, a multitude of applications are devised. Due to this, mobile cloud and fog computing are introduced like an addition to the cloud edge computing. The edge computing facilitates execution of programs at the edge of the network. Moreover, edge computing also provides a superior solution to data storage, low latency maintenance, computation power and application services. Therefore, integrating the concepts of edge computing with blockchain has facilitated the construction of exceptional systems by providing better storage of distributed nodes, reliable access of the network, better computation and so forth. Therefore, the systems are better in terms of security, data integrity and computation validation. However, the fusion consumes a lot of storage and computational resources, which affects the computation of mining and storage of the blockchain in resource-constrained devices. Additionally, the computation and storage on the blockchain are facilitated by off-chain computation and storage in edge nodes. The concepts of blockchain with edge computing are very popular; however, there are some problems that need to be addressed. Many approaches will be used at different levels for scalability refinement. Although by adding new autonomic mechanisms, the complexity of management reduces these additional results to security problems that still need to be studied. Furthermore, from different views and with stability and flexibility, the blockchain and edge computing-based functionalities need to be incorporated deeply. Also, the relationship between edge computing and blockchain needs to be promoted by AI and Big Data [15].
10.2.1 Current EHR System in Canada
It is seen that the healthcare industry has done many developments in their respective territory, and the development graph of healthcare is still growing. The expansion in the popularity of the medical field enables health professionals and service providers to enhance their specializations. Daily life habits like less workout, junk food diet, and less sleep, etc. result in chronic diseases [17]. Apart from primary and secondary prevention, there is a need to pay heed to early diagnostics. Having an incorporated electronic well-being record makes it workable for the specialist co-ops to put together their activities concerning what is as of now known about the client’s well-being history. In any care delivery setting, EHR is known as a longitudinal electronic record of patient health information, which includes the medical history of the patient, radiology reports, problems, medications. Personal health records (PHR) which are also called Electronic Personal health record is a complimentary record which has been created as a need for people to take an interest in their health. With the help of electronic health tools and information data set, PHR manages health-related data, assists the management of chronic. As far as EHRs are concerned, the primary key point is secured documents, which include current as well as past medical records. These health records include information from labs, different hospitals, clinics, etc. Executing electronic well-being records in Canada is a Canadian skillet activity that requires the cooperation of partners, including the government, Canada Health Infoway Inc. and the commonplace and regional governments, just as different associations engaged with the conveyance of medicinal services. Each inspected purview has, in any event, one center electronic well-being/health record (EHR) framework setup, and a few territories have nearly wrapped up their EHR frameworks. Given the noteworthy difficulties of this venture and the considerable potential advantages of EHRs, partners need to report on progress made and benefits accomplished to lawmaking bodies and Canadians. The Auditor General of Canada and the auditor generals of Alberta, Nova Scotia, Ontario, Prince Edward, British Columbia and Saskatchewan conducted execution reviews of the implementation of EHR in their jurisdictions [18, 19]. For EHR studies, the common objective has been created by different representatives of a committee. The main focus and concentration are being given to organizations like ministries of health who are answerable and liable for implementing EHR. Ensuring the compatibility of EHR is a primary task before implementing it. EHR, with excellent compatibility, result in better accessibility of medical information to healthcare professionals. At the administration level, Infoway was practicing due respect in managing assets from the national government to achieve its goals and objective in implementing EHR in Canada [18]. Infoway, as a fundamental and essential speculator, backs up each venture that relies on task potential. Moreover, based on project potential, Infoway accepts and approves each project to satisfy the needs of the project. Nevertheless, Infoway has done many works in support of implementing EHR across Canada:
Infoway has employed approval process to figure out the EHR requirements and inspect them.
Infoway funds the projects through a gated funding model. This gated funding model operates by binding repayment to the accomplishment of project milestone.
Infoway also settles legal agreements for each project in order to verify the projects.
However, when it comes to testing the system to check whether the projects have satisfied the requirements, Infoway does not involve the conformance testing results of the EHR system. Also, Infoway does not provide a guaranteed compatibility to EHR across Canada. It is surely compatible in cases where the standards have variances in the conformance. It is found that most of the people in Canada prefer to get healthcare from their native province but not all provinces have assurance about the compatibility of their EHR systems [18]. The compatibility of EHR systems has still not been properly established. To have a decent EHR system, it is important to have effective systems with better performance monitoring and reduced risks. However, it is found that there are different ways of handling project management. It depends and varies from province to province as follows:
In Ontario, projects expenditures with insufficient supervision, insufficient deliverable was reported [18].
In Saskatchewan, according to recognized project management, by ignoring the timelines and overall cost projects were managed [18].
In Prince Edward Island, cost for monitoring the projects was always a problem [18].
In Alberta, according to accepted project technique, EHR projects were handled. But monitoring of total cost for EHR systems still needs to be addressed [18].
10.2.2 Challenges with the Traditional EHR Systems
While there is no doubt that the EHR system is progressing day by day across Canada, there are still some issues regarding challenges listed below in implementing EHR system that needs to be addressed.
Achieving the goal: In March 2009, it was found that EHR healthcare professionals were available to only 17% of Canadians [18]. The main goal is to have 100% EHR of Canadians available to healthcare professionals which was stated to be very difficult by Infoway.
System upgradation: Compatibility funds are essential to construct the complete EHR, but it is often tough to determine how these funds will be provided and when.
Realizing benefits: From research conducted by Infoway it is found that $6 billion will be saved each year once they are deployed. However, jurisdictions are failing to realize the various advantages.
Patient healthcare solutions: The advancement of healthcare industries have enabled patients to access their own records. But the new EHR systems are not compatible with the old systems and therefore, there is a need for more solutions [18].
Sharing personal health information: EHR should be available across the country since many people move from one place to another place in search of jobs or living, sharing the personal medical data from one province to another is important. There are different laws for collection of medical data in different provinces. Thus, the laws also should be compatible between jurisdictions for an easier transfer of data between provinces.
Initiation of funding: At long last, questions stay about how the activity will be financed. The absolute expense to build the EHR system is also a crucial part to consider [18].
10.2.3 Security Measures for Health Records
As the technologies are advancing in every field, the risk of data loss and cybercrime is also increasing which results in destructive ramifications. Data security should be given the highest priority in all domains including healthcare industries. Data security is important in healthcare domain because losing healthcare data of a patient brings the question of life and death. As cybercrime in healthcare is a serious issue, the department of health and human services (HHS) in the USA has launched centers of cybersecurity and communication integration center. The main goal of these centers is to familiarize consumers and healthcare organizations about the risks of using mobile technology in the industry. There are many ways through which data can flow in and out of healthcare systems. EHR is considered to be one of the foremost information hubs from which the data can be lost. Since cloud-based EHRs effectively manage the exchange of data for the providers, the data is also at risk there. Although the sharing of data is helpful for the healthcare industries, there is a risk of data integrity being disrupted. The best way to eliminate threats to data integrity can be addressed by the four security measures that can provide security to the patient’s data:
Compliance to HIPAA and HITECH as a standard: Health Insurance Portability and Accountability Act (HIPAA) and Health Information Technology for Economic and Clinical Health Act (HITECH) provide best information security baseline standard and administrative guidelines for information security. For example, a bank-level (SSL) encryption algorithm is employed to check for secure transmission.
Critical clues provided by an audit trail: The main objective of audit trail is to track user actions to eliminate loss of information of hacking from the system. This tracking answers what, when, where and who, i.e.,
What was the data that was retrieved?
When was the data retrieved?
Where was the data retrieved?
And who retrieved the data?
State-of-the-art data centers: The state-of-the-art data centers maintain real-time surveillance, bank-level security and so forth. These data centers stop private information from being hacked, and also it shields from physical threats. For example, web apt saves the data in the IO data center which provides a qualified advantage for securing the data.
Accessibility to expertise on real-time: It is very crucial to have specialized staff in online security measures. The staff should be able to solve any data security related problems and other issues including security threat as protecting data means protecting people from these threats [20].
10.3 Current Challenges Faced by the Healthcare Workers in Covid-19 Pandemic
In the current state of rise in number of people impacted by Coronavirus Disease 2019 (COVID-19) in every corner across the world, clinical trials for the development of life-saving drugs have seen enormous growth [21]. Since its first detection in China, Coronavirus Disease 2019 (COVID-19) has now spread to over 210 countries/territories, with reports of local transmission happening across the world. According to World Health Organization (as of 10th April 2020), there have been a total of 15,21,252 confirmed cases and 92,798 deaths due to COVID-19 worldwide [22] and the number is still increasing. Recently, the FDA released guidance for industries, investigators and institutional review boards to consider for ongoing trials, incorporate policies and procedures, and solutions for trials that are impacted by COVID-19 in this pandemic [21].
10.3.1 Importance and Role of Medical Records During Pandemic
Medical records are an important part of the management of a patient. It is crucial for the doctor to responsibly record the patients’ health data who are under their care. The record keeping of health data can be considered a significant part of the system. This document can be used as both private and impersonal document which will address any patient management issues and help with scientific evaluations. The private documents are considered to be very confidential, and hence it cannot be accessed by anyone else without the patients’ consent, except for some cases. On the other hand, impersonal document can be accessed without patient’s permission and it can be used for multiple purposes, one of them being research. It is very important to maintain confidentiality of a patient and therefore hospitals must maintain privacy of patient’s private medical data. If confidentiality is breached, the patient has the right to file complaints claiming the negligence of the doctor or hospital authorities [23].
10.3.2 Challenges Faced by Doctors
In recent scenario, coronavirus is spreading to other countries by means of traveling. Most of the cases found positive in the first wave of the coronavirus were the people traveling to or contacting the locals in Wuhan, China. Locals and internationals who reported the initial symptoms and did not have access to their medical records had to follow the standard procedure in clinics which includes getting the blood report, EMR, ECG, stool and urine reports, etc. as the symptoms start to grow. These reports take time, and, in the meantime, patient is given antibiotics and anti-allergen supplements by the doctor to make sure the patient’s condition doesn’t worsen further which can have a reverse impact on the patient like allergic reaction or so forth. In absence of medical records of the patient chances of such mishaps are high. Another possible error could be misinterpretation of the symptoms shown by the patients, for example, if a patient has respiratory issues and has common fever and cough but the patient hides this information and with absence of medical records doctors might suspect it to be another coronavirus positive case and start with the medications.
Such accidents could be avoided by making the medical records electronic. If all the medical records were made electronic following same standards across the world it would have been easier to share, update, maintain and preserve the medical records. With easy access to medical records of each patient, doctors would be able to identify it much quickly whether the patient is showing positive symptoms for coronavirus disease or it is one of the other health irregularities causing it. Doctors would also be able to learn about the patient’s dietary restrictions, past and current medications and all the other medical history of the patient since the first logged entry.
10.3.3 Understanding the Proposed Architecture Using COVID-19 Example
We look forward to three main roles/participants in proposed consensus mechanisms which are committer, endorsers and consenters. In the current state of Pandemic, the doctors update the number of positive cases, new cases, total deaths to their respective Country Health Organizations. These organizations update their statistics to World Health Organization, and they update it on their website which is then acknowledged by the rest of the world. In this scenario, the country passing the stats becomes the committer, WHO becomes the endorser and rest of the World becomes the consenters as shown in Figure 10.1.

Figure 10.1 Proposed consensus mechanism.
10.4 Scalable Secure Management and Access Control of Electronic Health Records at the Edge
The primary concern of blockchain refers to the capacity to allow the number of different participants in a distributed shared ledger to document the system. The crux of blockchain is having better privacy and security with the need for enhancement in scalability. Among the various advantages of edge computing like achieving better scalability, better network performance, computing in distributed edge and storage, edge computing mainly focuses on management and service support along with the need for efficient control. Therefore, the main aim of coupling blockchain with edge computing is to take storage, computation and network into consideration while satisfying the requirements of the applications.
10.4.1 The Importance of Integrating Blockchain and Edge Computing?
Security of Edge Computing: In edge computing, there are high chances of losing the data packets or even storing the data incorrectly which might hamper integrity of data. This is due to data being stored across different storage locations. Also, as edge computing provides heavy storage overhead, ensuring the reliability of data has become a challenge in edge computing. In addition to this, uploading computational tasks to edge computation nodes while maintaining privacy and security is also another challenge for edge computing. Thus, these security problems need to be addressed while taking the problem of excessive encryption overheads into consideration.
Technical Challenges and Limitations of Blockchain: There are many advantages of blockchain like immutability, security that makes blockchain appealing, but at the same time, there are many challenges that obstruct its wide usage. There are various limitations like low scalability, high latency, low throughput that blocks the efficacy of the blockchain-based solution. In blockchain, with the increase in transactions, the issue of storage capacity arises. For example, public blockchains like Ethereum and bitcoin can only process 8–20 records each second that is smaller than common payment processor. However, if the block size is increased for a greater throughput, it results in centralization risk and cost of security increasing and thus it is not considered as an option.
Advantages of Integrating Blockchain and Edge Computing: Coupling blockchain with edge computing is advantageous as it increases the automation resource usage, security and privacy. The edge nodes can be employed to implement distributed control in blockchain technology. Moreover, with the help of mining process blockchain assures the accuracy, validity and consistency of data. Privacy of edge computing is being challenged as data is stored among multiple parties. Since there is no role of the third party to access and control data in the blockchain, privacy preservation with blockchain is comparatively easier. Resource is exchanged among edge nodes with dynamic coordination. But with the help of blockchain, the resources in edge computing is enabled, as by running a specified resource algorithm to run a demanded service of smart contracts of blockchain the on-demand resources can be used [15].
10.4.2 Challenges
When it comes to using blockchain with edge computing despite of having so many advantages there are still some challenges that need to be addressed:
Scalability Enhancements
Security and Privacy
Self-Organization
Function Integration
Resource Management
10.5 Overview of Blockchain and Hyper Ledger Methodologies
Our platform is a blockchain framework based on Hyperledger that addresses the previously discussed issues by constructing an architecture that will allow the software to be scalable and extensible. This model has three key device components which are an access control module based on blockchain, an off-chain data storage and a web user interface that is dissented for patient and doctor. In order to construct an efficient model, the different kinds of data that are collected such as laboratory test results, diagnostic images, care plans, prescriptions, etc. are encoded and saved in the cloud server and a hash value of the data is kept in the model. Smart contracts help the patient to control access permits flexibly and safely to each of their data assets. The web interface lets patients, physicians, quickly access the application. Today this technology is the foundation of most recent cryptocurrencies in circulation. A publicly distributed ledger is the key feature of this system, where the ledger is not owned by any individual, and a duplicate of the ledger is stored in all the nodes of the network. In the following sections, a further discussion of the methodologies has been provided.
10.5.1 Blockchain
Blockchain was originally created as the underlying technology in 2008 that enabled transactions of cryptocurrencies like bitcoin between peers. After recovering from the economic crisis of 2008, bitcoin being a new cryptocurrency was expected to address the double expenditure dilemma by blockchain usage. Stuart Haber and W. Scott Stornetta initially suggested the concept of cryptographic timestamps to store digital data in a block network [24]. In 1991, it was nevertheless initially introduced by creator(s) being named Satoshi Nakamoto, to create a bitcoin transaction blockchain in 2009. The transactions take place in this decentralized network which is peer-to-peer (P2P) instead of relying or requiring confirmation from third parties. The Economist article, published in 2015, announced blockchain technology as a trusted system by referring it as the ‘trust machine’ which is expected to change the operating style of the world economies. Blockchain provides a simple and sophisticated system despite of looking complex in various cases. Blockchain is a robust database or distributed digital ledger which allows direct P2P transactions of financial assets such as bonds and stocks, money, intellectual property, art, contracts, music, data and votes in some cases. Blockchain achieved this trust through a systematic consensus, collaboration and cryptography network rather than by banks, governments or intermediaries of third parties. The data blocks are stored securely and will be continuously updated with every new transaction. All parties involved in the transaction are provided a list through a distributed computer network. The concept of blockchain includes chronological blocks of transactions acting as distributed database where all the blocks are assigned individual hash values of newly verified transactions as well as the entire blockchain and are connected to the adjacent blocks based on the block’s hash value. For validating transactions, various algorithms are used by blockchain utilizing consensuses. A block can only be erased or removed when the copies on the distributed nodes are out of synch with them. Thus, three main characteristics are attained which are immutability, longevity and reliability characteristics. Figure 10.1 represents a generic application focused on blockchain. Participants in the blockchain system are not reviewed before transaction, and without involving any third parties, the transactions can be carried out. It is a licensing setting in which participants can stay unknown. Such resources have progressed the rise of blockchain technology to build cryptocurrencies along with transacting them. It has been the dominant cryptocurrency since the introduction of bitcoin. Its success has highlighted weaknesses in feature. The calculation cycles necessary to employ the proof of work consensus require heavy computation, often exceeding the expense of a transaction of bitcoin.
A timely upgrade of a blockchain of this size requires substantial computational and storage capacity, underlining existing nodes. The chain has developed to the size of around 160 GB [25], while still continuing to expand. Bitcoin’s block size is actually 1MB which is not likely to rise in the immediate years. The use cases that can be included in the architecture are also limited in this system along with the complexity of the carried out transactions. Ethereum is a newer blockchain platform that has no fixed block size in MB. For every individual transaction, the overall cost is limited. Businesses can, theoretically, ensure efficient and economical operation of an Ethereum-based chain. Ethereum has introduced features called smart contracts which allow virtually unlimited complexity of the transaction rules. Smart contracts [6] automatically try to validate conditions and implement the actions in the blockchain by building programmable triggers. By the time of launch of the blockchain the structure of each form of smart contract is decided. Participants possess individual values for each contract duration which allows flexibility as well as complexity of transactions. The above adds to the list of drawbacks of permission-less blockchains by being an obstacle to their usage in a wide variety of cases of business usage.
10.5.2 Electronic Health Records (EHRs)
EHRs are digital data of patient’s records such as their history and knowledge of medication that are traditionally kept on paper. The database can be accessed by certain healthcare providers and doctors for efficient treatment purposes as it allows long-term tracking of patient data. With the use of EHR, a large amount of paperwork can be avoided by removing a large amount of patient data from paper-based tracking.
10.5.3 Smart Contract
Smart contracts are electronic executable programs. A high-level computer programming language is needed to write these contracts to apply arbitrary business logic or pre-determined parameters to cause value transfer. A blockchain transaction has a specified target smart contract method, a payload that includes input values for the feature call and is always signed by the submitter. A transaction can be sent to any node in the blockchain network that transmits the transaction to the entire network. At some point the transaction is performed by any single node using the smart contract. With a successful execution of transaction, the internal state of the blockchain may change. However, the state is not affected when the input is detected to be invalid by the smart contract and the transaction will be rejected as failed. A majority of blockchain nodes run with this independently where each node maintains its own state database by conducting its own transactions using the chaincode.
10.5.4 Access Control in Medical Domain
The perfect way to address the health and medical data resource problems outlined in the introduction is through a blockchain which is based on hyperledger. A permitted smart contract in a blockchain gives the stakeholders (i.e., doctors and patients) full authority, enables immutability and cryptography, provides security and privacy and also permits identified participants to carry out trusted transactions. A basic digital transfer can be attained by used interface of data by drag and drop. Hyperledger blockchains have the disadvantage of storing large block sizes in addition to the cost of their computation. The digital asset’s size, and therefore the network size, would model performance problems that are going to deteriorate experience of the users and increase operating expenses in many companies [3]. Our implementation strategy is constructed to address such issues
10.5.5 Hyperledger
Hyperledger is a project that is a distributed ledger having open source, which is approved by the Linux Foundation. It consists of various subprojects like: Fabric, Sawtooth, Indy, Burrow, Iroha, etc. In this chapter, we have concentrated on the hyperledger fabric project only. Hyperledger fabric provides an open source platform which is enterprise-grade developed by the IBM and Linux Foundations. Like Ethereum and bitcoin, there is no blockchain in it, where limited network participants can access the network, and no one can join it. The utilized approach to validate the transactions and generate blocks at hyperledger fabric is PBFT (Practical Byzantine Fault Tolerance) [26]. The transactions are handled using chaincode in hyperledger fabric, which is a software code that allows writing and configuration of the application to communicate with the network. An insulation mechanism known as the channel is used to assess the privacy of the participant’s network transactions. The channel only shares data with the nodes which are channel members and have the transaction and the data. The hyperledger fabric’s official documentation defined transaction as an instant request or invoke transaction which is submitted by the peer to order and validate. A chaincode is generated from the instilled request in each path, when the invoked transactions perform operations such as read/write on the ledger. The key elements of hyperledger fabric Architecture are ordering nodes, peer nodes and client applications [27]. The task of responsible certificate authorities is to create identities of the component. The transactions are received and ordered by the ordering nodes from various requests inside a block [6].
10.5.6 Composer Tools
Hyperledger technologies are very popular for designing and decentralizing blockchain applications. The most widely used tools are especially the hyperledger fabric and Hyperledger Composer. Hyperledger Composer is a stable, open tool set and framework for designing blockchain applications. Hyperledger Composer follows the existing hyperledger fabric blockchain architecture and runtime, which uses pluggable blockchain consensus protocols to ensure that the transactions are being authenticated by authorized business network participants with respect to the policy. Everyday applications can use business network data and provide end-users with simple and controlled access points. Hyperledger Composer is a series of collaboration resources used by business owners and developers that render hyperledger fabric and Decentralized Applications (also known as smart contracts) easy to write chaincode. Proof-of-Concept can be quickly build using Composer and adopt chaincode in the blockchain within a short time. Composer Hyperledger consists of the following toolkits:
Modeling language called CTO: a domain modeling language that defines the requirements of the principle, business model and business network.
Playground: It is used for rapid business network configuration, deployment and testing.
Command-line interface (CLI) tools: The client command-line interface is used to integrate business networks with hyperledger fabric Composer-CLI as the most effective tool for business networking. Some other effective tools are REST servers, Hyperledger Composer Generator, Yeoman and Playground. Composer CLI offers many useful tools for the developers. The Composer REST server is used to build a REST interface to a blockchain-deployed business network.
10.5.7 Playground
The Hyperledger Composer Playground offers a user interface for configuring business network, deployment and testing. Playground has a wide range of advanced features that allow users to control the business network security, invite business networking participants and connect to multiple business blockchain networks.
10.5.8 Off-chain Storage
Off-chain storage is used to store the medical and health data assets securely to preserve the efficiency and economic viability of an application, and the block’s data item which is dedicated to the chain is considered as the hash of the data asset’s URI. The transactions of data asset are authorized with a sign of the data owner with a private key (patient or caregiver). An extra layer of data asset security is added when the size of an individual block can be reduced by employing URI hash.
10.5.9 User Experience From Patient’s Side
Playground is a software framework used to access the application functionality. The general idea is to always keep the patient at the center of a treatment circle. Patients have the liberty to choose the people to be included in their circle of treatment and what knowledge is exchanged with each of them. For the patients who require a reliable assistance, the domain is further expanded to involve a secondary opinion like a caregiver / another doctor who can work on behalf of the patient. The web platform connects using the well-known RESTful API to the network. Hyperledger Composer can call external APIs utilizing smart contracts or transaction processor function. We have built a stable, reliable and accessible component for introducing modularity and unified extensibility by connecting users to the blockchain. This portion is partly developed with Secure Hypertext Transfer Protocol (HTTPS). The users can then keep tract of their digital assets by running the application in any device that supports HTTPS requests.
10.6 Hyper Ledger-Based Proposed Architecture for Protecting Electronic Health Records
As discussed above, our system is a permissioned blockchain where nodes are organized in committer, endorser and consenter.
The committers’ ordered and validated transactions are appended to their respective ledger once it is returned by the consenter.
Endorsers run the transactions related to the network and also prevent the occurrence of non-deterministic and unstable transactions.
Consenters provide the validation of the transaction and update the distributed ledger with the latest transaction details that took place between the Committers and Endorsers.
10.6.1 Proposed Architecture of the Blockchain System
The novel technology blockchain is gaining popularity in every field, especially in healthcare industries since it has many benefits. Figure 10.2 represents the conceptual architecture where all the medical data (prescriptions, read access and IoT data) is stored in the medical blockchain. This medical data is an independent medical lake that is not only limited to hospital usage but also for disease prevention and research, and it is referred as the stored-off blockchain.

Figure 10.2 Overview of Proposed Architecture.
More specifically, the medical blockchain network is made up of trusted authenticating peers, and for the network every single peer holds copies of the ledger to keep the distributed ledger secure. The database is a part of the ledger which stores the unchangeable record of the transaction, blocks sequence record, and a data lake in order to hold different kinds of health data. The role of blockchain is to basically act as a logbook and document any alterations related to data lake. The data lake is the database having an off-chain state that carries, for example, latest digital patient data and the current data collection values. Medical IoT devices are capable of continuously collecting and transmitting data which can be used in data analyzing and eventually create a range of resources starting from response to critical care to preventive care.
A rapid transmission and processing of data enables healthcare providers to treat their patients more efficiently. For example, the user group includes people in various positions: the administrator who is capable of handling all the resources inside the hospital, the doctor who is able to review all patient details and give a prescription for the medication, the pharmacists who instruct and advise about the right usage and consequences of the medications and products that are prescribed. The patients can therefore access their medical data through the peer networks containing their health records. In addition, the patient can set up permission to allow access to any physician of their medical information who is in the same network. That can be achieved by defining the smart contract’s policies of access control which is distributed across complete network of blockchain to make sure that the patient’s data has privacy and protection. All end-user interactions in a blockchain require a digital signature so that the device is secured.
Figure 10.3 describes the key components and offers a good overview of the medical blockchain framework being proposed. Both the technical framework and user interface system have been depicted in the architecture where both the smart contract and distributed ledger are presented as services in the applications. The users (doctor, patient, admin, nurse, etc.) may send offers for transactions via the application toward the network of blockchain to obtain booking, EHR, payment and many other services. A transaction refers to the course of producing, modifying, transferring or deleting EHR data that exist between the peers that are connected.

Figure 10.3 Integrity management of proposed medical blockchain platform for EHR.
For facilitating transactions that are confidential and private, we split the complete network into various private networks to make it subnetwork which requires interactions between multiple departments that are listed. When the agencies wish to store health data privately so that it is not accessible by other agencies, they are permitted to initiate their subnetworks, which include the required units that need access to data. It is of particular significance for the use of businesses, because some participants might be rivals who do not want any deal, it is made available to everyone, for instance, an exclusive rate given to specific people. The proposed platform stands out from other blockchain systems because it is constructed on a permissioned network. Instead of using an open program which is permission-less and will permit unknown participants to enter the network, participants of the built network are added via a user manager that is trusted. Their role is to make every cryptographic process abstract and offer multiple resources for the certification. More specifically, these services include user registration, rules governing such identities and authentication and protected communications among the components or user of the blockchain.
The design of the proposed framework in the architecture enables the accommodation of complex business use case requirements, where the order of transactions in the pluggable consensus can be switched to and fro, the operation of smart contracts takes place inside a container environment and it supports various identity management protocols and finally multiple storage technologies can be used to store the ledger data. Departments attach to subnetwork through an interface that is provided by the consensus manager in addition to the order of transactions, and they also decide how it should be integrated with the final block. The medical blockchains have different peers in each of their departments which include storage of data and smart contract to support the transaction pitch or write a block of transaction in the ledger. The distributed ledger is responsible for recording the clear and fixed past that refers to all events which occurred in the network. Services such as hashing and digital signatures that are part of consensus protocol and cryptographic primitives are used to make the process more secure by ensuring the precision of the ledger.
10.6.2 Data Flow Diagrams
10.6.2.1 Doctors
Doctor/Physicians need to login to the application using their valid individual credentials. On login, they can see multiple options under their profile. Doctors can update their personal information under the profile tab. Doctors can view the list of other doctors available, the medical records of the assigned patients, grant/revoke the read-only access rights to/from the other doctors, transactions list over the blockchain and the list of patients assigned to them (Figure 10.4).

Figure 10.4 Data Flow Diagram for Doctor.
Figure 10.5 shows the Data Flow Diagram for GRANT/REVOKE the READ-ONLY Access Rights to/from Other Doctors.

Figure 10.5 Data Flow Diagram for Sharing Medical Records.
10.6.2.2 Patient
Patient needs to login to the application under the profile tab; they can view their own medical records, name of the assigned doctor, current and past prescriptions and transactions list over the blockchain as shown in Figure 10.6.

Figure 10.6 Data Flow Diagram for Patient.
10.6.2.3 Transaction Flow
Figure 10.7 shows the transaction control flow from point of login to transaction posted over the blockchain.
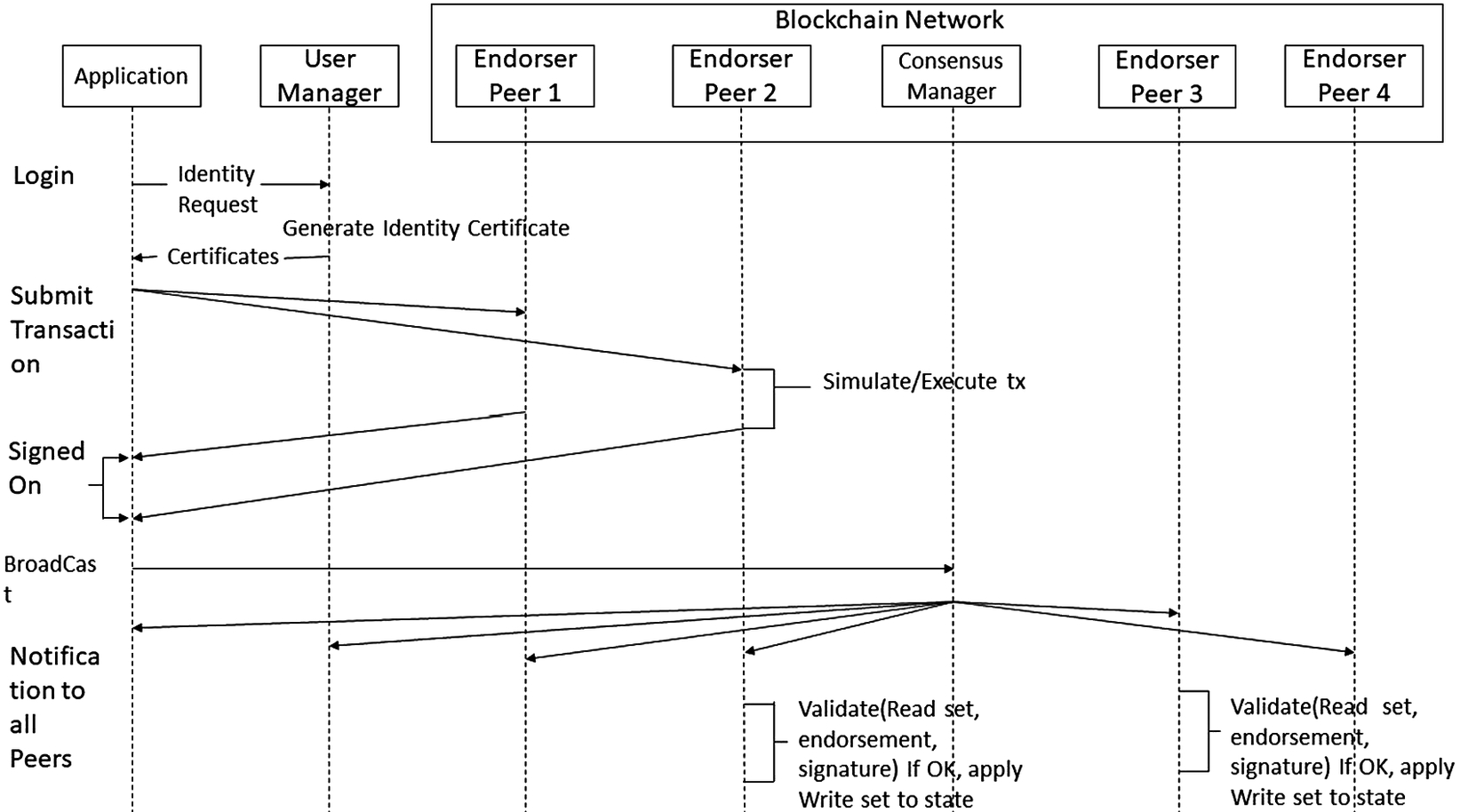
Figure 10.7 Transaction flow diagram over blockchain.
10.7 Performance Evaluation
10.7.1 Performance of the Proposed Model
We have used Quad core Skylake Processor: Intel® Core™ i5-6300U Processor (3M Cache, up to 3.00 GHz) along with 8 GB DDR3 RAM as the basic hardware to implement our project on the local system.
Figure 10.8 depicts the time taken to create number of patients and doctors. Since there are more parameters to be passed in creating the records for doctors, it is taking slightly higher time for creating the record as compared to the patients. Here, number of participants created are visible by the numbers used over the line graph and vertical columns/bar represent the time taken by doctors and patients. The performance was quite steady in the controlled environment and it was able to perform with great stability and provide better results.

Figure 10.8 Time taken to create records in application.
Figure 10.9 depicts the time taken to grant the read-only access over the medical records of a patient to one doctor or multiple doctors. Our reading shows that it took around 1second per transaction to complete when a single doctor was given read-only access rights over a patient. Similarly, when a batch of 240 doctors was granted read-only access over the medical records of a patient by the assigned doctor, it took about 6 seconds for the transaction to complete. According to these results, we can predict that one Cuda Core 600 MHz GDDR3 BUS type GPU computing module could be sufficient for a single hospital setup handling multiple transactions per second.

Figure 10.9 Read access over Electronic Health Records.
10.7.2 Performance Comparison
A comparative analysis was performed in Table 10.1 to compare our model with some of the existing relevant studies. It was found that our system provides a combination of features that is efficient and secured for the users. The study in [29] comes close to our model in terms of accessibility, smart contract employment and provides a developed application; however, due to resource management technique of the model, it did not surpass the performance of our model.
Table 10.1 Comparative analysis between various blockchain-based studies.
| Blockchain-based studies | Smart contract | Resource storage | Accessibility scheme | Website/Mobile application |
|---|---|---|---|---|
| Our approach | Yes | Off-chain | Permissioned | Yes |
| MediBchain: A Blockchain Based Privacy Preserving Platform for Healthcare Data [28] | Yes | Blockchain | Permissioned | No |
| OmniPHR: A distributed architecture model to integrate personal health records [29] | No | Blockchain | Permissioned | Yes |
| Managing IoT devices using blockchain platform [30] | Yes | Blockchain | Permission-less | No |
| Toward blockchain-based auditable storage and sharing of IoT data [31] | No | Off-chain | Permission-less | No |
10.8 Conclusions and Future Caveats
It can be concluded that many accessories are benefited for incorporating the concepts of blockchain technology in healthcare industries by enabling data sharing and tracking with required privacy and transparency for the users. This chapter proposes a unique way of designing and implementing a decentralized system to deal with EHRs with the help of blockchain technologies. The purpose of the system is to offer an essential secured and clear platform to aid the stakeholders such as patients, doctors and hospitals. Specific performance indexes are used to conduct experiments, showing a reasonable resource usage while maximizing efficiency. Also, a comparative analysis was performed which showed the efficacy of our proposed model compared to previous studies in terms of various characteristics. While the evolution of blockchain technologies in the field of healthcare is still evolving, the aim of this study is to propose a viable approach to construct an application integrating healthcare applications and healthcare, benefiting stakeholders and revolutionizing innovations throughout the healthcare industry.
Furthermore, we could replicate 60% of the setup activities and installation over Cloud platform using Ubuntu as OS and Google Cloud as the service provider. We would be working further in this direction to find an alternative for the REST server for composer tools to launch the application over the cloud environment instead of local computers, which could be a leading research area in itself as the IT giants are working in this area. In addition, the proposed work can be extended based on the developed framework to several other business settings. Some of the challenges of this work largely depend on scale of the blockchain network and the requirements of a device. Some of the future research directions are to address the problem of extending the size of network to a larger scale and incorporating the propositioned architecture in cloud.
References
- 1. K. M. Cresswell and A. Sheikh, “Health information technology in hospitals: current issues and future trends,” Futur. Hosp. J., 2015, doi: 10.7861/futurehosp.15.015.
- 2. S. A. Bragadeesh and A. Umamakeswari, “Role of blockchain in the Internet-of-Things (IoT),” Int. J. Eng. Technol., 2018, doi: 10.14419/ijet.v7i2.24.12011.
- 3. S. Rouhani, L. Butterworth, A. D. Simmons, D. G. Humphery, and R. Deters, “MediChainTM: A secure decentralized medical data asset management system,” In 2018 IEEE International Conference on Internet of Things (iThings) and IEEE Green Computing and Communications (GreenCom) and IEEE Cyber, Physical and Social Computing (CPSCom) and IEEE Smart Data (SmartData) (pp. 1533–1538). IEEE, 2018, doi: 10.1109/Cybermatics_2018.2018.00258.
- 4. R. Sharma, “Blockchain in Healthcare: 2017s successes,” Fr. Canada Chamb. Commer. Ontario, pp. 2017–2019, 2018, [Online]. Available: https://www.coindesk.com/blockchain- healthcare-2017s-successes/.
- 5. L. Hang, E. Choi, and D. H. Kim, “A novel EMR integrity management based on a medical blockchain platform in hospital,” Electron., 2019, doi: 10.3390/electronics8040467.
- 6. Q. Nasir, I. A. Qasse, M. Abu Talib, and A. B. Nassif, “Performance analysis of hyperledger fabric platforms,” Secur. Commun. Networks, 2018, doi: 10.1155/2018/3976093.
- 7. R. J. Krawiec et al., “Survey: Patients see 18.7 different doctors on average,” In Proc. NIST Workshop Blockchain Healthcare, 2010. [Online], Available: https://www.prnewswire.com/news-releases/survey-patients-see-187-different-doctors-on-average-92171874.html.
- 8. Charles, D., M. Gabriel, and T. Searcy. “Adoption of electronic health record systems among U.S. non-federal acute care hospitals: 2008-2014,” 2015. ONC Data Brief, no.23. Office of the National Coordinator for Health Information Technology: Washington DC.
- 9. K. D. Mandl, P. Szolovits, and I. S. Kohane, “Public standards and patients’ control: How to keep electronic medical records accessible but private,” Br. Med. J., 322, 283, 2001.
- 10. N. Rifi, E. Rachkidi, N. Agoulmine, and N. C. Taher, “Towards using blockchain technology for eHealth data access management,” In 2017 fourth international conference on advances in biomedical engineering (ICABME) (pp. 1–4). IEEE, 2017, doi: 10.1109/ICABME.2017.8167555.
- 11. S. Al-Megren et al., “Blockchain use cases in digital sectors: A review of the literature,” In 2018 IEEE International Conference on Internet of Things (iThings) and IEEE Green Computing and Communications (GreenCom) and IEEE Cyber, Physical and Social Computing (CPSCom) and IEEE Smart Data (SmartData) (pp. 1417–1424). IEEE, 2018, doi: 10.1109/Cybermatics_2018.2018.00242.
- 12. J. Lane and C. Schur, “Balancing access to health data and privacy: A review of the issues and approaches for the future,” Health Serv. Res. 2010, doi: 10.1111/j.1475-6773.2010.01141.x.
- 13. M. Reisman, “EHRs: The challenge of making electronic data usable and interoperable,” Pharm. Ther., 42, 572, 2017.
- 14. Y. Guo and C. Liang, “Blockchain application and outlook in the banking industry,” Financ. Innovation. 2016, doi: 10.1186/s40854-016-0034-9.
- 15. R. Yang, F. R. Yu, P. Si, Z. Yang, and Y. Zhang, “Integrated blockchain and edge computing systems: A survey, some research issues and challenges,” IEEE Commun Surv Tutor. 2019, doi: 10.1109/COMST.2019.2894727.
- 16. A. da Conceição, F. Silva, V. Rocha, A. Locoro, and J. Barguil, “Eletronic health records using blockchain Technology,” 2018.
- 17. F. W. Booth, C. K. Roberts, and M. J. Laye, “Lack of exercise is a major cause of chronic diseases,” Compr. Physiol., 2012, doi: 10.1002/cphy.c110025.
- 18.“2010 April report of the auditor general of Canada,” 2010. [Online]. Available: https://www.oag-bvg.gc.ca/internet/English/parl_oag_201004_07_e_33720.html.
- 19. A. Boonstra, A. Versluis, and J. F. J. Vos, “Implementing electronic health records in hospitals: A systematic literature review,” BMC Health Serv Res. 2014, doi: 10.1186/1472-6963-14-370.
- 20. H. Jannenga, “4 Crucial data security measures every EMR must have in place,” Available: https://www.beckershospitalreview.com/healthcare-information-technology/4-crucial-data-security-measures-every-emr-must-have-in-place.html (accessed Aug. 10, 2017).
- 21. D. Cohn-Emery, “Challenges for clinical trials and treating patients with cancer in light of the coronavirus,” Available: https://www.targetedonc.com/view/challenges-for-clinical-trials-and-treating-patients-with-cancer-in-light-of-the-coronavirus (accessed Mar. 20, 2020).
- 22. WHO, “Coronavirus disease 2019 (COVID-19) Situation Report –81,” 2020. [Online]. Available: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200410-sitrep-81-covid-19.pdf?sfvrsn=ca96eb84_2.
- 23. J. Thomas, “Medical records and issues in negligence,” 2009, doi: 10.4103/0970-1591.56208.
- 24. S. Haber and W. S. Stornetta, “How to time-stamp a digital document,” J. Cryptol., 1991, doi: 10.1007/BF00196791.
- 25.“How to build an electronic medical record secured by blockchain?” Available: https://www.devteam.space/blog/how-to-build-an-electronic-medical-record-secured-by-blockchain/.
- 26. M. Castro and B. Liskov, “Practical byzantine fault tolerance,” Proc. Symp. Oper. Syst. Des. Implement., 1999, doi: 10.1145/571637.571640.
- 27. C. Cachin, “Architecture of the hyperledger blockchain fabric,” Leibniz Int. Proc. Informatics, LIPIcs, 2017, doi: 10.4230/LIPIcs.OPODIS.2016.24.
- 28. A. Al Omar, M. S. Rahman, A. Basu, and S. Kiyomoto, “MediBchain: A blockchain based privacy preserving platform for healthcare data,” In International conference on security, privacy and anonymity in computation, communication and storage (pp. 534–543). Springer, Cham, 2017, doi: 10.1007/978-3-319-72395-2_49.
- 29. A. Roehrs, C. A. da Costa, and R. da Rosa Righi, “OmniPHR: A distributed architecture model to integrate personal health records,” J. Biomed. Inform., 2017, doi: 10.1016/j.jbi.2017.05.012.
- 30. S. Huh, S. Cho, and S. Kim, “Managing IoT devices using blockchain platform,” 2017, doi: 10.23919/ICACT.2017.7890132.
- 31. H. Shafagh, L. Burkhalter, A. Hithnawi, and S. Duquennoy, “Towards blockchain-based auditable storage and sharing of IoT data,” 2017, doi: 10.1145/3140649.3140656.