Chapter 4. Digitization and AI
Consider the following story in comparison to Bethanie’s story in the opener of Chapter 3. It’s the summer of 2025, Bethanie, a 28-year-old school teacher, Generation Z, experiences troubling symptoms, her most concerning questions, “why am I always thirsty” and “why am I so tired recently.” She thinks it might be due to her being in Nevada’s arid climate, where she helped a friend move just a day earlier. She believes it explains her exhaustion as a consequence of helping her friend move. She drives back home to Southern California and hopes she feels better but needs to stop and get something to drink. She decides to have a conversation with her My Digital Twin app while driving home, and a voice dialog begins.
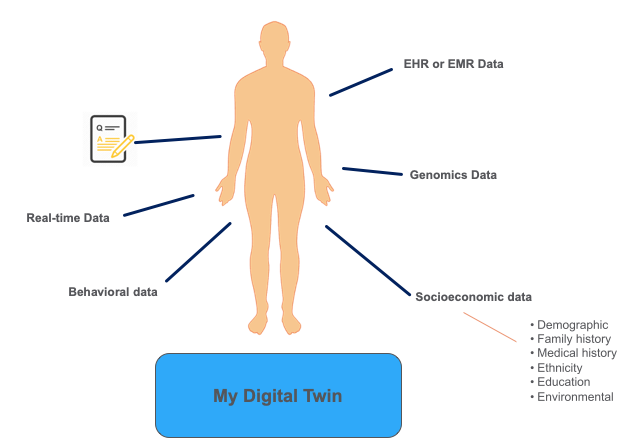
As a reminder, my digital twin serves as a diagnostic, monitoring, and visual health tool. Feeding genomic, behavioral, and social media data, the digital twin’s knowledge and insights grow continuously. Encounters with clinicians feed the app and signals from wearables like her pulse, weight, and BMI. Her physical fitness wearable sends in real-time data on her pulse, weight, and BMI. Bethanie loves engaging with her digital twin as she can model future health states projecting ten or twenty years in the future about her health. Her digital twin knows her medical history, family history, education, and social, economic status. Flu, pandemic outbreak, or air quality issues using public data feeds the digital twin, and alerts appear if Bethanie lives or enters a high-risk area.
During her drive home, the app, My Digital Twin begins asking Bethanie a series of questions about how she feels. The app learns Bethanie can’t seem to quench her thirst. It asks more questions and learns she is feeling fatigued for several days. The app concludes and then suggests she might have diabetes and advises she purchase an over the counter saliva glucose biosensor. These biosensors recently came on the market in the last nine months. Bethanie buys a $20 biosensor from a nearby pharmacy. When she arrives home, she administers the test, and she tests positive for diabetes. Bethanie’s digital twin app receives a signal of diabetes.
Bethanie’s My Digital Twin application begins scheduling an appointment with Bethanie’s primary care physician provider’s office. A telemedicine, virtual doctor appointment is scheduled for later in the day. Her digital twin asks Bethanie to continue to wear her fitness tracker, which detects pulse. The digital twin enters concern mode, and unbeknownst to Bethanie; it’s checking her pulse via the fitness app periodically trying to identify her for an episodic event. Her digital twin pings Bethanie every hour to verify she is functional, and if she were not, it would call her designated emergency contact and her primary care physician.
Bethanie uses another phone app, providing a portal into her health insurance. She sees out of pocket expenses incurred to-date. She also determines any projected costs for her and allows schedules for her telemedicine call. Price transparency and instant cost notifications are the norm.
The virtual telemedicine call begins. Bethanie describes her symptoms and communicates to the doctor that she might have type 1 or type 2 diabetes. She reads the analysis provided by her digital twin app to the doctor. The report provides a rationale for why it might be type 1 and hence recommends getting an autoantibodies test to test for type 1 diabetes, and the physician agrees and orders the blood tests. The blood tests confirm type 1 diabetes, and the doctor advises Bethanis to go to the emergency room for care immediately.
She spent two days in the intensive care unit, and three more days after that in the hospital while she stabilized, and eventually, her blood sugar stabilized, and she understands she is a type 1 diabetes. Her Digital Twin provides tutorials and education on nutrition and diet, which Bethanie reads and becomes knowledgeable about Type 1 diabetes care.
Bethanie’s appetite returns, and when she receives the first meal, she immediately gets concerned about what’s on her plate. Bethanie immediately informs the nurse that her understanding is that a few items on the plate might aggravate her diabetes, namely the bread and brownie. The nurse on closer examination agrees, apologies, and indicates delivery of the wrong meal.
Disruption in healthcare is happening, albeit slowly with high potential for acceleration. Costs are skyrocketing. Quality of care appears to be declining. Patients don’t feel in charge of their healthcare. They are further exasperated by medical crises such as the COVID 19 pandemic. Lack of testing supplies, lack of tests, lack of standard personal protective equipment, lack of preparation by healthcare providers to evaluate possibly contagious patients, lack of medical supplies such as ventilators, and lack of hospital capacity became evident to the broader public. It’s only during times of stress do the pain points in our healthcare system become truly visible. Now that public awareness exists, there is an outcry for immediate change to our healthcare systems.
Improving access and efficacy of healthcare requires real-time healthcare leading to increased digitization of healthcare. Both require artificial intelligence as its engine and building block. Technology is not enough, it’s not the solution, but it represents a component for rethinking of the healthcare model as it exists. This change, digital healthcare, brings about enormous potential for personalized healthcare resulting in potentially longer and healthier lives for us today. In this chapter, we’ll explore the different ways that digitizing healthcare can improve both patient and caregiver experiences.
Digitization of Healthcare
Digitization of healthcare is a broad area addressing a wide swath of domains like patient care, health wellness, diagnostics, decision support systems, hospital and provider systems, EMR systems, triage, back-office administrative systems, home care, urgent care, emergency room, chronic care management, mental health and more. Digitization means using technology to provide real-time, fast, immediate outcomes, whether it’s approving a claim, approving prescription coverage, performing a diagnostic, getting test results. Digitization eliminates the need for phone calls by making information readily and instantly accessible and available, whether it’s determining your benefits, getting your lab test results, or getting approval for a prescription. It means substantially reducing misdiagnosis and medical errors because of highly interactive decision support systems at play in doctor’s offices or hospital settings. Digitization means price transparency, where patients know the cost of a service at the time of inquiry and delivery. There exists an abundant set of opportunities to make healthcare digitized. The number of use cases is limitless but let’s explore a few through the lens of three paths.
Three distinct paths should be pursued by healthcare incumbents, government and every organization tasked with making healthcare better, faster, more accessible and better efficacy. in the digitization of healthcare, illustrated in Figure 4-1, Paths to Digitization.

Figure 4-1. Paths to Digitization
All three paths require employing transitional and game-changing technologies like artificial intelligence. The aspects of artificial intelligence apply depending on the problem. Still, if organizations are not using deep learning, machine learning, computer vision, and natural language processing, they will not achieve optimal digitization. AI won’t be enough; blockchain, mobile, cloud computing, and graph technologies are essential technologies. State of Healthcare Technology, published by O’Reilly, provides a summary of healthcare technologies required for optimizing healthcare and making healthcare digital. We’ll discuss the three different paths next.
Path A: Creating Digital Operations and Processes
Path A creates and integrates digital operations and processes delivering on the customer value propositions. Customers include the ecosystem in healthcare, including patients, consumers, clinicians, hospitals, providers, health services companies, and more. In this path, organizations focus on changing existing processes and their legacy systems supporting those processes to a digital state. Path A concentrates mainly on the as-is state to a future state of current operations and processes.
Healthcare digitization is held hostage to several IT applications and systems. For example, healthcare electronic medical records (EMRs) and electronic health records (EHRs) systems provide digitized records of a patient’s healthcare encounters. Making a record of patient encounters digital represented state of the art at one time. Today, time spent on EHR systems reduces the amount of time physicians spend with their patients, negatively affecting patient relationships. Storing data is not a clinical tool; it doesn’t provide healthcare. A Harris Poll1 conducted on behalf of Stanford Medicine delivers a treasure trove of AI use cases for EHRs: disease diagnosis, disease prevention, and population health management. In this study 9 of 10 physicians want their EHRS to be intuitive and responsive, a perfect storm for AI adoption. Short term improvements include voice as a modality acting as a scribe during patient’s visits, a highly viable AI engineering effort using deep learning and natural language processing.
In many cases legacy systems must address poor system availability and stop the mindset that systems which read and write data cannot have the same reliability and availability seen in the platforms of the large technology companies, Google’s search engine or Amazon’s commerce site or Netflix streaming videos. High availability, high reliability and use of mobile and cloud technologies remains
Path B: Building New Capabilities
Path B builds a new set of capabilities around the desired customer end state and operating model in lock-step with Path A. Path B means thinking about how to use the Internet of Things and AI, creating new products and services. The ever-growing number of medical devices embedded with AI that live in homes or on the body makes creating new healthcare products and services more possible. Path B enables enhanced healthcare experiences but redefining even better experiences and healthcare outcomes.
Path C: Transforming Business Processes
Path C transforms business processes. Often requiring taking an enterprise view and eliminating duplicative processing or reimagining the new process. This path is fraught with risk and high rewards. Path C includes moonshot projects or as Safi Bahcall writes, Loonshots, crazy ideas that cure diseases, and transform industries. The Digital Twin app is a moonshot where the healthcare system engages consumers and people. The number of moonshots is a long list starting with real time healthcare.
Digital Healthcare
In general, digital healthcare applies technology, using the data acquired through technology, to improve our health and wellness. This technology includes apps, wearable devices, remote or ambient monitoring devices, telemedicine, health-related email, and electronic health records to incorporate your related data into your health management.
The benefits are apparent. For example, if diagnosed with hypertension, doctors, and other caregivers will have real-time or close to real-time data on how your blood pressure management works. As a result, this scenario allows more immediate adjustments or micro-adjustments to one’s care that would not exist in our current healthcare model. Typically a person starts treatment with medication or lifestyle change and then returns for a follow-up visit to your doctor to have your blood pressure rechecked in several weeks. Micro-adjustments result in improved care for you as a patient. Your doctor will be able to tell if the treatment prescribed worked, or if further adjustments are warranted. As a patient, the less time your blood pressure is out of control, the safer your kidneys and other vital organs are from the damage resulting from uncontrolled hypertension. Your doctor has more tools and information to help manage your condition, making her job more comfortable and efficient.
Digital tools can help identify new issues by identifying medical conditions that would not be apparent otherwise (captured during a doctor visit). As in the example, digital tools can help monitor the effectiveness of treatment and identify the worsening of chronic conditions. As we discussed in the last chapter, identification of medical issues allows physicians to intervene faster, thus either treating immediately or preventing the development of medical disease. Better management of disease symptoms occurs, improving a patient’s quality of life. You also avoided long term complications resulting from untreated disease. For hypertension, these complications include kidney and eye injury, as well as increasing your risk for stroke. Avoiding these complications of the disease improves your quality and length of life. It avoids healthcare costs associated with the development and management of these complications. The sicker you are, the higher the healthcare cost as it takes more resources to treat your condition.
To take this a step further. You and your doctor now have your hypertension managed with medication therapy, correctly. Your blood pressure readings are consistently within a healthy range. What else is left to do?
AI Applied to Digital Healthcare
Elevating individual responsibility through AI helps create digital healthcare. AI adds another dimension to your care. Using the same example, hypertension, AI now points out to you as a patient and your doctor that a decrease in weight of 20 lbs can control your blood pressure without medication. In the office, a clinician is usually harried and potentially running behind schedule with numerous demands on their time. For example, physicians see patients, supervise other clinicians, such as students, physician assistants, responding to patient emails, phone calls, responding to insurance coverage issues, billing complaints, all while covering for other physicians for these same responsibilities who are out of office. Unfortunately, it is easy for patient care to sometimes slip between the cracks—patient care increases where AI’s role eliminates or streamlines these non-clinical tasks. AI fills the role of safety net for the clinician to ensure appropriate and timely care is not accidentally overseen.
AI can serve many functions in the clinical space. AI can perform as a safety net in the above example, reminding the clinician that counseling and perhaps enrollment in a health and wellbeing program for weight loss may help with non-medication management of hypertension. Also, AI can be used to provide doctors with reminders about best practice management for chronic conditions.
Your blood pressure is well controlled on medication therapy. You also start working on healthy weight loss and regular aerobic exercise. Your connected device provides timely input to your doctor that your regimen is working well, and your blood pressure is now not only controlled but borderline low. AI is used to identify abnormally low blood pressures, taking both the data from your biometric device and your input from your iPad that indicates you have been feeling dizzy intermittently. AI analyzes all this information and research of the clinical database and hypertension management guidelines to form a recommendation for intervention by your doctor.
Your doctor takes this packaged and easily digestible information to make an immediate decrease in your medication dosage. Over time, with close connected monitoring and AI assistance, you can stop all medication therapy. Your hypertension has resolved as long as you continue to adhere to your healthy lifestyle.
As one ages, your blood vessels become less compliant, genetics may catch up to you, and you may require medication therapy again. In your entire lifecycle with this condition, from elevated blood pressure to fully diagnosed hypertension to resolution of hypertension to chronic hypertension AI and digital connections have been used to provide personalized care with optimal outcomes.
AI, Digitization, and Corporate Healthcare Strategy
Predictably large companies are joining the digital healthcare bandwagon,such as Google with its deployment into the wearables market with Google Wear, and Fit (a health platform launched in 2014). Moreover, Google recognizes the impact of AI on digital healthcare and has been exploring and has created ventures that include the DeepMind unit, where AI is used to identify eye disease from imaging scans. Google’s parent company, Alphabet, has a health sciences arm named Verily. Verily is working on such exciting projects as the Aurora study, where AI is being used to identify physical biomarkers of mental trauma. They created their wearable, specifically for this study.
While some companies are investing in future AI with digital solutions, Apple, on the other hand, has focused on current-day applications. The Apple watch has been expanding the watch’s health care uses with additions of falls detection and an ECG monitor. The corporate goal is to create other offerings for Providers (such as Apple’s Health Kit, which we’ll discuss in the next sectiono) as well; the Apple watch would be the relied upon device to connect patients to their Providers for care. Amazon, in partnership with others, has created its own healthcare company, Haven, in an attempt to reimagine the healthcare market and how technology is used.
Corporate interest in healthcare is expanding for a variety of reasons. Healthcare has traditionally been recession-proof with high spending, and growing demands on healthcare resources lead to the need for cost-saving strategies. To date, the market appears to be focused on preventive strategies,such as the one given in our example above. The deterrent aspect would be where an overweight or obese patient is identified before the development of hypertension. Other preventive strategies using AI and digital health are being applied to chronic diseases like diabetes and hypertension. Preventing disease is much less costly than treating illness, and we’ll explore that topic further in the next section.
Preventive and Chronic Disease Management
The American Medical Association (AMA) supports the integration of AI into the healthcare system to improve patient care safely and effectively. Wearable devices can track multiple health measures, but the large amount of data and its current incompatibility with most electronic health records (EHR)s makes their use unwieldy. Apple’s Health Kit is one tool that integrates data from wearables into the EHR. As mentioned earlier, the Apple watch is expanding its healthcare capabilities to be of use to both consumers and providers.
Digital AI and Prevention
Preventive medicine or lifestyle Digital AI solutions abound. They range from stress management solutions to monitoring of data associated with our health trackers to indicate a potential risk for disease development with counseling on management and prevention.
Weight management, stress, sleep, exercise, financial support are all the major categories of digital AI that are in place today. Consumers/patients use this technology to assess and take ownership of their health. Status today is that the majority of consumers are comfortable and embrace this technology for wellness.
Not only can hypertension possibly be averted through prevention with exercise, healthy weight, and diet, but other conditions can be as well. The range for the prevention of diseases is broad. To use another example, our digital AI can currently monitor our sleep. Rather than a patient being required to spend the night attached to monitors at a medical office, at-home sleep studies are now the standard. Digital AI has the capability of identifying abnormal sleep patterns or restless sleep. AI applied to this digital data, and overweight or obese status taken into consideration with alcohol intake, which may worsen sleep disorders can lead to assessments that notify the patient that discussion with a doctor is needed. An early sleep disorder is identified, or the consumer can change their lifestyle, modify their diet with weight loss, and have immediate data available to them and their provider on the management of their possible sleep disorder. The Apple Watch ECG is being used to identify potential heart rhythm disorders that predispose to stroke. The examples are numerous, and the extension from the use of digital AI for preventive medicine naturally extends to chronic disease management once it develops.
Digital AI and Chronic Disease
Type 2 Diabetes and hypertension are two of the most common chronic medical conditions today. The US Centers for Disease Control and Prevention (CDC) report that 1 in 9 Americans have Type 2 Diabetes, and 1 in 3 Americans have hypertension. Each of these conditions is a significant risk factor for heart disease, which remains the leading cause of death in America. 7 out of 10 people with their first heart attack have hypertension, and people with diabetes are twice as likely to have heart disease or a stroke as compared to people without diabetes, and at an earlier age. 60% of patients who have hypertension also have diabetes, and the health risk increases exponentially with the development of long term nerve, eye, and kidney damage.
Interestingly, diabetes and hypertension can be “silent” for a prolonged period until a crisis is reached. People with diabetes may slowly develop increased thirst and urination and not know that this may indicate an underlying disease state. Similarly, hypertension is known as the “silent killer” as frequently patients will present with stroke or other neurological symptoms later tied back to undiagnosed and untreated hypertension. Both are managed through a healthy diet, lifestyle, and medication therapies.
Patients self monitor their blood sugar levels and blood pressures. This data input to health care providers and systems can be enormous through the use of connected devices. Digital AI health solutions can track, understand, and report results from this patient-generated healthcare data (PGHD). For example, digital AI has been developed where abnormal results are sent to healthcare management systems that can then reach out and provide telephonic counseling to improve disease management. Alternative interventions through digital AI include the use of apps and virtual consultants to address abnormal results.
Besides digital AI to enhance chronic disease management, digital AI can also promote and improve self-education for the patient. For example, a patient can enter a query or question regarding their diabetic diet and what is allowed intake. The chatbot then utilizes AI and identification of keywords to provide advice on diabetic diet to the patient. In cases where keywords are not identified, or the question is not understood, the chatbot will direct the patient to their provider. PGHD is of benefit to providers as well. Doctors now have access to close to real-time data to perform micro-adjustments to their patients’ care, which leads to avoidance of complications of the disease and associated cost avoidance.
Digital AI provides benefits to healthcare payers as well. As mentioned in the telephonic case management program above, patient members are given customized guidance and counseling. At the same time, clinical decision support is used to guide the patient to the next best step in care action. Providers may be contacted for care integration. All of this leads to enhanced disease management and improved quality of life without requiring the patient to self manage, identify, or necessarily understand the underlying connections leading to integrated care and improvement in their disease management.
Through these digital AI modalities come several other benefits: health care costs are decreased, and quality of life increased for patients, increased accessibility and application of data to improve disease outcomes, decreased cost from complications associated with the unmanaged or mismanaged disease, permanent end-organ damage is mitigated by improved management, loss is avoided from hospital or emergency department visits that do not occur because digital AI allowed intervention and care before a crisis.
Digital AI and Mental Health
Digital AI is not limited to medical conditions alone. Mental illness is common in the US. Nearly one in five adults live with a mental illness, that’s 46.6 million people in 2017 per NIH statistics. There are current apps that allow AI, digital healthcare, monitoring behavioral health via monitoring one’s smartphone to follow how many social interactions have occurred that day, including social network site visits, texts, calls, physical activity level, and general smartphone use. That data is then analyzed by AI to determine if depression or other behavioral health disorders are on the increase, or managed. In this way, Digital AI allows self-assessment and connection to one’s provider for close to real-time monitoring of one’s mental health. Some chatbots provide mental health counseling and apps for cognitive behavioral therapy. The development and use of these tools is essential as there is a growing gap between the amount of mental health care needed and the number of providers who can care for them.
Technology usage for mental health care is on the rise, and people’s comfort level is growing. Digital AI for mental health makes sense as more consumers are taking responsibility for their mental healthcare. Again, the COVID 19 pandemic brought digital technology to the forefront as people were in isolation, with their states shut down. Estimates show the mental health burden rose in proportion to the prolongation of isolation associated with social distancing during the pandemic. Because the population was encouraged to stay at home and avoid social contact, digital healthcare rose. COVID 19 may inadvertently impact and drive the increased utilization of digital technologies based on necessity. Time will tell if the trend continues, but we believe the pandemic has changed the healthcare paradigm, Digital Healthcare made possible with AI.
Digital AI and Telemedicine
To reiterate, digital AI takes in all the data from connected devices which is then processed by AI to provide quick and timely interventions in healthcare, all of which is supported by AI analysis of the most up to date and relevant treatment options. Connected devices facilitate remote delivery of care, or telemedicine. Telemedicine, as evidenced by the COVID 19 pandemic has broad reach and has made billions of users aware of a new modality of healthcare. Digital AI has a special and significant role in telemedicine.
The transformation to our healthcare system is already happening. COVID 19 was the impetus to drive a rapid and exponential increase in utilization of telemedicine. Digital AI is being used in decreasing hospital readmission programs. In one hospital readmission reduction program, a patient is given a wifi enabled device at discharge from the hospital that transmits important patient data, such as vital signs (heart rate, blood pressure, temperature, etc) to their providers for ongoing outpatient management. AI is constantly monitoring this data and at the sign of any abnormality both the patient, their provider and any other caregiver can be notified to address this finding and hopefully avert a hospital readmission or emergency department visit. It’s all about timely intervention. An example of just such a partnership in the market currently is a pilot program between NHS (National Health Systems) hospitals at Dartford and Gravesham working with Current (formerly Snap40) aimed at remote monitoring of patient vital signs with AI analysis. The patients in this pilot were fitted with wi-fi enabled armbands and given a chatbot equipped tablet for medication reminders and remote communication with their providers. The patients received all their tools prior to discharge from the hospital. In this manner, provider and care teams were able to keep close remote eyes on their patients with the ability to perform micro-adjustments to care that kept patients healthier and out of hospitals, but still provided quality care.
Telemedicine has now been widely accepted and can provide the clinical support to the world of data that digital AI has opened. This integration provides numerous benefits:
-
early diagnosis and timely intervention
-
personalized care, and
-
remote patient monitoring on a real time basis.
We’ve discussed early diagnosis and treatment several times throughout the book. Again, early diagnosis allows for interventions either in lifestyle, habits, diet or with medications prior to complications of disease development and prior to development of long term damage to the body related to uncontrolled disease. Traditionally, patients would have symptoms and no other associated information leading them to seek care at a doctor’s office. With digital AI symptoms are paired with personalized patient data generated by the patient’s connected devices. Therefore, telemedicine providers have more information at the time of patient evaluation. These teledoctors have: the patient to provide a description of their symptoms, data from connected devices with AI analysis pointing out any abnormal findings, and AI assisted analysis of clinical treatment guidelines, to ensure the most up to date and best care, or best next treatment, or evaluation step for each patient based on their own individual data.
Personalized care via digital AI is possible as all data generated from connected devices or alternate data input from other devices, such as ipad with symptom generators and checklists, are derived from an individual patient. Thus, doctors can make interventions or treatment decisions based on an individual patient’s data. For example, traditionally, someone with possible high blood pressure or hypertension would be seen in the clinic with maybe some accompanying blood pressure readings from pharmacy blood pressure machines. Their blood pressure would be taken in the doctor’s office as well. If abnormal, then a treatment decision is made as to whether the patient chooses to pursue diet and exercise, or if severe enough, to pursue medication therapy. The patient then continues to check their blood pressure outside of the office and has a follow up appointment with their doctor in a few weeks to months. At that point another treatment decision is made as to whether to pursue more aggressive therapy, to continue current treatment, or decrease current treatment. Digital AI allows abnormal findings to be sent in close to real time to their doctors for early intervention and management. Micro-adjustments and their impact on the disease are immediately available and allow for finer management based on individual patient data. In addition, AI can enhance the treatment algorithms to ensure the best quality of care and best next step in management for each individual patient. These treatment plans are then monitored through digital AI to ensure adherence, control of disease, and if any change occurs (such as an ability to lose weight resulting in need for less medication) treatments are changed accordingly.
Remote monitoring is a relatively new concept. Traditionally, in the hospital a set of vital signs are obtained on a scheduled basis. If the patient is sick enough, then monitors may be placed such that real time monitoring occurs and alarms go off for abnormal readings leading to clinical evaluation and possible adjustments in treatment. In the outpatient setting, there was no routine monitoring of any vital signs except in rare cases and this was done by the patient either having further appointments to have monitors placed on them for home evaluation, or patients having to stop in to clinics or other healthcare sites for follow up readings. Digital AI has transformed the process in the outpatient setting where devices are common and use has increased significantly. Now a constant stream of data in close to real time are available to both the clinician and the patient. Any abnormalities are analyzed by AI and early intervention and adjustments can be made. Timely intervention is key as timeliness is what prevents long term complications, and allows for fewer intolerable side effects of treatment (as monitoring would identify say too low a blood pressure).
Telemedicine is also quickly evolving almost in symbiosis with digital modalities. Co-evolution is a process whereby species develop based on the strengths of other species that support and help the dominant species to succeed. Consider humans and dogs. Humans were physically weaker, and dogs provided protection and support while humans returned dog’s support with food. Thus, humans never needed to develop the heightened senses of dogs for protection, and each provided for the need of the other. Similarly, telemedicine is now evolving its model. Telemedicine was once what is called a “one and done” visit. Previously used as an alternative to urgent care medicine, telemedicine is now evolving a primary care system. Several telemedicine providers are developing, or have deployed primary care provider telemedicine care platforms. To adequately perform ongoing telemedicine in a patient provider relationship that is ongoing and not a one time visit only, digital AI provides support for this type of patient engagement. Digital AI is the eyes and ears of the doctor for ongoing patient management.
Specialty telemedicine providers are also emerging. Specifically, diabetes specialists, or endocrinologists are now being utilized in several different programs to help with ongoing care and timely micro-adjustment of insulin regimens to provide best possible care for diabetics. Digital AI again empowers these doctors by notifying them of abnormalities, and adherence, as well as supporting doctor treatment/management decisions based on best care practices identified by AI.
Medication Management and Digital AI
Digital AI continues to expand its reach and use cases andis taking a leading role in improving medication adherence. Medication adherence is the likelihood that a patient will take the medication prescribed for them as directed, or at all. Why is medication adherence important? Over the past two decades, healthcare costs have been rising exponentially. In large part prescription medications make up a large component of these costs. For example, of the $101 billion spent on Diabetes in 2013, half of this was spent on medications. Studies suggest that 33-50% of patients do not take their medication, or do not take it properly. This results in nearly 125,000 premature deaths each year, and costs the nation about $290 billion in associated hospitalizations and other complications from disease events per the New England Healthcare Institute and the American College of Preventive Medicine.
The technology response to this problem is digital therapeutics which encourages patients to take their medications and to take them as directed. Mobile devices and sensors capture data and provide real time alerts through browsers, apps and medical devices on medication adherence. Examples include smart packing and pill dispensers, wearables that provide reminders to take medications and can track medication use, tablet apps providing reminders on refills and taking medications, and even virtual pillboxes with images displaying the size and shape of pills for identification and to avoid confusion. When connected with sensors and combined with AI the possibilities for medication and patient management are tremendous.
Medication Adherence
In one study supported by the National Institutes of Health (NIH) a reinforcement learning-based medication health program was used to focus on medication adherence. Patients were randomized to either:
-
Medication Event Monitoring System (MEMS) cap on pill bottles + text messaging reminding patients to take medication and managed by AI to determine type of messaging and frequency, or
-
MEMS cap only.
The results showed improved medication adherence at 3 months for both study groups. Of note, medication adherence went from a baseline of 69% to 80% to 84-92% with use of digital AI.
Management of chronic conditions involves complex behaviors and patients vary in their medication adherence based on these behaviors. One study noted that after a heart attack episode at one month after hospital discharge <50% of these patients continued their daily low dose aspirin as prescribed during the heart attack. Another study showed that of 5,000 hypertensive patients, most patients took their medications only intermittently and 50% had stopped taking their medications without informing their provider. In the NIH study mentioned above there was greater medication adherence shown when accompanied with AI augmented text reminders. Mobile health services, such as text have shown up to two-fold increase in medication adherence.
Of note, the NIH study used AI to determine if patients were non-adherent with medication use and what type of messaging and what frequency of texting would lend itself to increased adherence. In one month AI had decreased text messages by 46%, due to AI learning that more frequent notifications did not lead to increased adherence. AI was also able to tailor notifications to those patients with the greatest need for reminders, and decreased, or stopped notifications to patients that were adherent as indicated by MEMS.
Digital Medication
Digital AI use in medication adherence is not limited to apps, sensors, and wearables between patient and provider/caregiver interactions. It extends into digital medication. Founded in 2001, Proteus Digital Health has created the world’s first Federal Drug Administration (FDA) approved digital medicine, a pill called Abilify MyCite. Abilify MyCite contains a sensor that digitally tracks if patients have ingested their pill(s). The way this works is outlined in Figure 4-3 below.

Figure 4-2. How Ingestibles Work
Abilify MyCite is specific to the medication Abilify used in the treatment of schizophrenia. This type of technology is very important as it is well known that schizophrenics that are not medication compliant have more psychotic episodes and may require more hospitalizations and intensive management, as well as being a potential harm to themselves and others.
AI applied to digital pills shows even more potential. Not only will medication adherence be tracked, but Providers and other caregivers will be able to apply AI to data intakes from wearables and other sensors to provide additional information on whether the medication is working and if real time micro-adjustments to treatment regimens need to be made. The potential for the benefits of digital AI are limitless.
Other ways in which Digital AI is transforming medication management include:
-
Improving medication safety (Digital data in conjunction with utilization review with AI can detect medication errors);
-
Predicting health risks and outcomes (Michigan is working on using patient’s medication histories along with electronic health records, and prescription drug monitoring programs to calculate drug overdose risk and predict risk of overdosing from a prescribed opioid); and
-
Improving the medication prior authorization process (regardless of improvements, many medications still entail duplicate data entry, delays and rework after criteria for authorization are not met--AI can be used to extract the relevant data for the prior authorization along with digital information/data that can help augment and streamline the process of authorization by providing and importing the relevant biometric data that may be required for approval of therapy).
AI and Digitization Applied to Administrative Tasks
Harvard Business Review published an article in 2016 on “How Artificial Intelligence Will Redefine Management.” In the article AI was noted to be more efficient and capable than humans and that digital transformation and transitioning of labor intensive tasks to AI just made sense. In previous chapters we’ve described how administrative tasks consume providers’ lives and prevent them from having the time to spend in face to face interactions with patients.
AI can simplify humans’ lives by giving them time to focus on human based interactions and efficiently performing the administrative tasks that continue to comprise a significant proportion of time.
We’ve also discussed how AI, by taking over administrative tasks, results in cost savings as AI is more efficient than humans in this area. The US spends a disproportionate amount on healthcare, with nearly double the spend compared to other high income countries such as Canada, Germany, Australia and the UK. However, higher spend does not result in increased quality of clinical care and improved patient management. In a study published by Journal of American Medical Association (JAMA) it was noted that about a little less than half the healthcare spend in America goes to planning, regulating and managing medical services at an administrative level. AI is being looked to for cost management and time savings.
Already, AI has made great strides in imaging tasks, such as analyzing X-ray images, detecting cancer and assisting doctors with clinical decision support and management of patients. By supporting clinicians with some of the “easier” tasks, this allows times for more human focused interactions with patients. You always hear, “my doctor saw me for 5 minutes, and charged me X amount.” With AI to support the doctor, more time can be spent between the doctor and patient.
Similarly, in population health management where physicians look for trends in cohorts of patients with similar disease conditions, age, risk factors, etcetera, AI can facilitate. The advent of EHRs has propelled the digitization of healthcare data on broad populations which AI can then be applied to. AI provides the analysis on these cohorts of patients with similar diseases, risk categories, ages, etcetera and parses out the details on who/which patients need management and/or intervention in care and at what time. Patterns and predictive trends used to rely on data scientists querying healthcare data sets, and clinician review along with experience to determine population health targets. Now AI can either perform this task for us, or augment the current process.
Why is this important for doctors? Doctors have relied on experience and evidence based medicine guidelines to help facilitate management of large populations. Today AI can augment that management through the above noted analysis. From this broad overview of patient populations, AI algorithms can then analyze millions of data points, and comb through the latest published research databases to quickly find relevant patterns and determine best next steps in action for the doctor and patient. This approach makes a big difference in costs and patient health. Dr. Robert Pearl a Stanford University Professor used consensus algorithms, along with oncology data entered in EHRs and cross walked with the hundreds of established treatment regimens to recommend the most appropriate combination of chemotherapy medications for a patient. Furthermore, this same research and use of AI allowed creation of a predictive model that could identify which cancer patients today would end up in the Intensive Care Unit tomorrow. AI facilitates doctors in saving lives and making judgments on management that save in cost, but more importantly, impact people.
AI also has the potential to go beyond the human experience by “unsupervised learning.” Unsupervised learning is a subset of machine learning that analyzes data and discovers patterns and anomalies with minimal human involvement. “Unsupervised learning” has the potential to uncover patterns and trends missed by clinicians based on clinician bias or inability to ask the right question for analysis.
Lastly, AI can augment claims and processing as well as prior authorizations (as mentioned above). All of this results in efficiency and time as well as cost savings. AI can empower transactions and data management such that patients should be able to pay for doctor visits in real time, with the claim processed and complete, and needed prior authorizations fulfilled by the time the appointment is over. All of which leads to improved quality of life and care for patients and clinicians.
Summary
Figure 4.4 shows a healthcare framework where AI applications and solutions exist and continue to evolve.

Figure 4-3. Healthcare Framework for AI Applications and Solutions
Digital solutions are involved in many of these solutions and indicate the significance and relevance of having real time data to help in patient management. In each of these six areas AI services and solutions exist and for which numerous opportunities exist.
