Chapter 7
Self-Testing for Glucose and Other Key Tests
In This Chapter
![]() Understanding why monitoring is a must
Understanding why monitoring is a must
![]() Checking glucose with meters and A1c
Checking glucose with meters and A1c
![]() Testing for kidney damage
Testing for kidney damage
![]() Examining your eyes and feet
Examining your eyes and feet
![]() Finding your level of cholesterol and other fats
Finding your level of cholesterol and other fats
![]() Gauging your blood pressure, weight, and other details
Gauging your blood pressure, weight, and other details
You may wonder what you have to do to prevent the complications of diabetes that I describe in Chapters 4 through 6, and the answer is a fair amount, which I discuss in this chapter. But when you weigh the benefits that add up to a longer, better-quality life against the loss of time and money from preventive care, the benefits of preventive care win by a landslide.
With preventive care, you can take advantage of an explosion of new tests and treatments that have only been available for the last 35 years, beginning with self-testing of blood glucose in 1980 right up to new tests for overall diabetic control and multiple new hardware and software tools made possible by the latest advances in computer and Internet technology.
As Woody Allen points out, “I don’t want to achieve immortality through my work; I want to achieve it through not dying.” On the other hand, he says, “On the plus side, death is one of the few things that can be done just as easily lying down.” Well, I don’t want you to take your diabetes lying down. I want to give you the benefit of every important advance. You may not achieve immortality, but you can enjoy every day that you live.
This chapter gives you all the tools you need to detect complications in their earliest stages. And if, by chance, you are reading this section for the first time and complications have already developed, this chapter also shows you how to measure the progression or, hopefully, regression of your complications.
Testing, Testing: Tests You Need to Stay Healthy
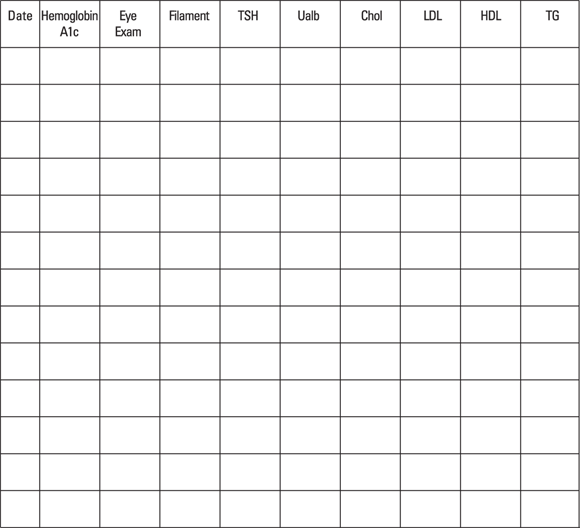
A number of tests and measurements should be done on a regular basis. To best make sure that you get your tests done regularly, you can use the chart in Figure 7-1. This form lists the tests and you can list the results underneath. Simply copy the one in this figure and keep it up-to-date. Don’t expect your doctor to keep this chart updated for you. He has too much on his mind and too many patients to get it exactly right for each one.
© John Wiley & Sons, Inc.
Figure 7-1: A sample testing chart that you can copy to track your testing results.
- Blood glucose: At each visit, evaluate the blood glucose measurements you’ve been taking. (See the section “Monitoring Blood Glucose: It’s a Must,” later in this chapter.)
- Hemoglobin A1c: Obtain hemoglobin A1c four times a year if you take insulin and twice a year if you don’t. (See the section “Tracking Your Glucose over Time: Hemoglobin A1c,” later in this chapter.)
- Eye exam: Have a dilated eye examination by an ophthalmologist or optometrist once a year or every two years if no disease is present. (See the section “Checking for Eye Problems,” later in this chapter.)
-
Filament: Examine your bare feet at each visit and have your doctor perform a filament test. (See the section “Examining Your Feet,” later in this chapter.)
In addition to looking at the feet, you should also have an ankle-brachial index performed at least every five years.
- TSH: Your doctor should check your thyroid-stimulating hormone level when your diabetes is diagnosed and every five years thereafter if it is normal.
- Ualb: Check for microalbuminuria once a year. (See the section “Testing for Kidney Damage: Moderately Increased Albumin (MIA),” later in this chapter.)
- Chol/LDL/HDL/TG: Obtain a lipid panel once a year to monitor your total cholesterol, LDL (bad cholesterol), HDL (good cholesterol), and triglycerides. (See the section “Tracking Cholesterol and Other Fats,” later in this chapter.)
In addition to the preceding tests, you should also have your doctor take your blood pressure and measure your weight at each visit. (See the sections “Measuring Blood Pressure” and “Checking Your Weight and BMI,” later in this chapter.)
Are doctors and patients with diabetes doing the best job of managing diabetes? Government statistics on Preventive Care Practices from the Centers for Disease Control and Prevention (CDC) suggest that they aren’t. Doctors and patients are getting a little better as diabetes becomes a major health problem in the United States. The latest statistics compare the annual rates of testing for various abnormalities associated with diabetes between 1994 and 2010. They indicate some improvement, but as a whole they should be doing a lot better. Only about 60 percent of diabetic patients are doing frequent testing of blood glucose, A1C tests at least twice a year, annual eye exams, and annual foot exams.
As diabetes knowledge has grown, the guidelines for how high various tests should be in people with diabetes have changed. Unfortunately, they seem to have no effect on the results of clinical practice:
- The Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure lowered its guidelines for blood pressure in people with diabetes in 1997 and again in 2003, but as of 2008 there was no better control, according to the CDC.
- The American Diabetes Association lowered its goal for LDL cholesterol (see later in this chapter) to less than 100 mg/dl in 1998. As late as 2010, there was no indication that patients were meeting the new goal more often than they had in 1994.
Much can be done. And that’s what this chapter is all about.
Monitoring Blood Glucose: It’s a Must
Insulin was extracted and used for the first time more than 90 years ago. Since that time, nothing has improved the life of the person with diabetes as much as the ability to measure his or her own blood glucose with a drop of blood.
Prior to blood glucose self-monitoring, testing the urine for glucose was the only way to determine whether your blood glucose was high, but urine testing could not tell at all whether the glucose was low. The urine test for glucose is worthless for controlling blood glucose — it actually provides misinformation. All the thousands of research papers in the medical literature before 1980, which used urine testing for glucose, are of no value and should be burned. (However, testing urine for other things, such as ketones and protein, can be of value.)
Basically, two kinds of test strips are used today. Both require that glucose in a drop of your blood reacts with an enzyme. In one strip, the reaction produces a color. A meter then reads the amount of color to give a glucose reading. In the other strip, the reaction produces electrons, and a meter converts the amount of electrons into a glucose reading.
One of the first things that was learned when frequent testing of blood glucose became feasible is that a person with diabetes, even a person who works hard to control his glucose, can experience tremendous variation in glucose levels in a relatively short time, as little as 30 minutes. This variation is especially true in association with food, but it can occur even in the fasting state before breakfast. For this reason, multiple tests are needed.
How often should you test?
How often you test is determined by the kind of diabetes you have, the kind of treatment you’re using, and the level of stability of your blood glucose.
-
If you have type 1 or type 2 diabetes and you’re taking before-meal insulin, you need to test before each meal and at bedtime. The reason for this frequent testing is that you’re constantly using this information to make adjustments in your insulin dose. No matter how good you think your control is, you cannot feel the level of the blood glucose without testing unless you’re hypoglycemic. In fact, on numerous occasions I have had my patients try to guess their level before I test it. They are close less than 50 percent of the time. That degree of accuracy is not sufficient for good glucose control.
People with type 1 diabetes should occasionally test one or two hours after a meal and in the middle of the night to see just how high their glucose goes after eating and whether it drops too low in the middle of the night. These results guide you and your physician to make the changes you need.
Numerous studies have shown that increased daily frequency of blood glucose testing is significantly associated with lower levels of hemoglobin A1c and fewer complications of diabetes in patients who take insulin. There is a 0.2 percent lowering of A1c for each extra test up to a maximum of five tests.
- If you have type 2 diabetes and you’re on pills or just diet and exercise, testing doesn’t seem to make a major difference in your glucose control. In a large study, regular testing resulted in just a .25 percent reduction in hemoglobin A1c and even this improvement was gone by 12 months. The main reason is that patients don’t use the test results to make changes in treatment.
- If you’re pregnant, see the testing guidelines I outline in Chapter 6. I would guess that you’re probably willing to test numerous times in a day to keep your developing fetus as healthy as possible.
- If you eat something off your diet and want to test its effect on your glucose, do a test.
- If you’re about to exercise, a blood glucose test can tell you if you need to eat before starting the exercise or if you can use the exercise to bring your glucose down.
- If your diabetes is temporarily unstable and you’re about to drive, you may want to test before getting into the car to make sure that you’re not on the verge of hypoglycemia. Even if your diabetes is stable, testing at the beginning and after every couple of hours of a long drive can prevent serious hypoglycemia.
Keep in mind that the occasional blood glucose test done in your doctor’s office is of little or no value in understanding the big picture of your glucose control. It is like trying to visualize an entire painting by Seurat (who painted using dots of color) by looking at one dot on the canvas.
How do you use a lancet?
To get the drop of blood you need to perform a glucose test, you have to use a spring-loaded device that contains a sharp lancet. You push the button of the device, and the lancet springs out and pokes your finger. Devices that allow different depths of penetration are useful for small children.
One product that seems less painful than the others is the Accu-Chek Softclix Lancet Device. It allows you to select one of 11 depth settings so that you can penetrate your finger no deeper than necessary. Many glucose meters allow testing at other sites besides your finger, which require different depths of penetration to reach blood, so these settings can be very useful. However, the Softclix uses its own type of lancet that is a little more expensive than others on the market.
Accu-Chek also offers the Multiclix device, which holds a drum of six preloaded lancets. Its great advantage is that there is no handling of lancets. In most devices, you have to push the lancet into the device and pull it out to discard it. In this one, as you use one lancet it re-enters the drum and the next clean lancet drops into place. When you have used all six, you throw away the drum and put a new one in the device. It too offers 11 penetration depths. The downside is that each lancet can be used only once.
Becton Dickinson (BD) makes another lancet, called BDGenie Lancet, that works like a lancet and lancing device all in one. It is less painful and a little less expensive than other devices on the market. Becton Dickinson also makes the thinnest lancets currently available, called the BD Ultra-Fine 33 Lancets.
Although you do not have to use alcohol on your fingers, they should be reasonably clean. (My patients have done millions of finger sticks, and I’ve never known one of them to have an infection result.) Use the side of your finger to avoid the more sensitive tips that you don’t want to hurt, especially if you use a keyboard frequently. Change fingers often so that no finger becomes very sensitive.
Remember never to use a used lancet on someone else. Each lancet lasts for a few pokes and should then be discarded in a special sharps container so it can’t poke someone else accidentally. Sharps containers are available in drugstores, or you can use an empty plastic laundry detergent bottle. Check with your refuse service to make sure it is okay to leave the sealed bottle in the garbage.
How do you perform the test?
If you don’t already own a blood glucose meter, be sure to check out the next section. All meters require a drop of blood, usually from the finger. (See the previous section, “How do you use a lancet?”) You place the blood on a specific part of a test strip and allow enough time, usually between five seconds and one minute, for a reaction to occur. Some strips allow you to add more blood within 30 seconds if the quantity is insufficient. The need for a second stick of your finger is rare if you use a test strip that requires less blood. In less than a minute, the meter reads the product of that reaction, which is determined by the amount of glucose in the blood sample.
- If you have trouble getting blood, you can wrap a rubber band around the point where your finger joins your hand. You will be amazed at the flow of blood. Take off the rubber band before a major hemorrhage occurs (just joking).
- Testing blood from sites other than your fingers is generally reliable, except for an hour after eating, immediately after exercise, or if your blood glucose is low. These other sites don’t reflect the rapid changes in blood glucose that are occurring.
- Some meters use whole blood, and some use the liquid part of the blood, called the plasma. A lab glucose tests the plasma. The whole blood value is about 12 percent less than the plasma value, so you need to know which you’re measuring. The various recommendations for appropriate levels of glucose are plasma values unless specifically stated otherwise. Most of the newer meters are calibrated to give a plasma reading, but check yours to be sure.
- Studies have shown that the quality of test strips, which are loose in a vial, deteriorate rapidly if the vial is left open. Be sure to cap the vial. Two hours of exposure to air may ruin the strips. Strips that are individually foil-wrapped do not have this problem.
- Check the expiration date of the strips. Expired strips won’t give correct results.
- Don’t let other people use your meter. Their test results will be mixed in with your tests when they are downloaded into a computer. In addition, a meter invariably gets a little blood on it and can be a source of infection.
Choosing a Blood Glucose Meter
The meter business must be a profitable one because many new meters are on the market each time I update this book. But the cost of the meter should play little part in your decision about which one to get. Most manufacturers are happy to practically give you the meter so that you’re forced to buy their test strips. Each manufacturer makes a different test strip, and they’re not interchangeable in other machines. Some companies even make a different strip for each different machine that they make.
The accuracy of the various machines also isn’t a consideration. All are accurate to a degree acceptable for managing your diabetes. Keep in mind, though, that they do not have the accuracy of a laboratory. Meters are probably about plus or minus 10 percent compared to the lab.
Factors that may influence your purchase
Your doctor may have a meter that he or she prefers to work with because a computer program can download the test results from the meter and display them in a certain way. This analysis can be enormously helpful in deciding how to alter your therapy for the best control of your glucose.
Your insurance company also may mandate a certain meter, in which case you may have no choice.
- If a small child is to use it, can the child easily use the meter and strips?
- Are the batteries common ones, or are they hard to get and expensive?
- Does the meter have a memory that I and my doctor can check?
- Is the meter downloadable to a computer program that can manipulate the data?
- Do I have to calibrate the meter every time I change to a new box of strips (an inconvenient step)?
Profiles of different meters
More than a dozen companies vie for your meter purchase. Among them, they produce more than 50 machines. Like everything in business, mergers and acquisitions have occurred and will continue to happen so that the field narrows. In the following sections, I give an overview of a number of the most common options.
In addition to these options, many other manufacturers make glucose meters including Arkay, Bionime, Fifty50 Medical, Fora Care, Infopia, Oak Tree Health, Omnis Health, U.S. Diagnostics, Walmart, and others. These companies’ meters have no particular advantages not present in the meters that I describe here.
Abbott Laboratories
Abbott Laboratories purchased the MediSense Company, which first made and sold blood glucose meters. This company, which has one of the longest warranties on its meters (four years), is speedy about taking care of problems that arise. The batteries are good for 4,000 tests. They can generally be replaced by you unless otherwise noted. One clue that Abbott is really interested in customer service is that you can find the owner’s guides for all their meters on the Internet.
- FreeStyle Freedom Lite: The FreeStyle Freedom Lite requires a tiny sample of blood, and you can add more up to a minute from the first application if you don’t have enough on the strip. The Freedom Lite works with a data-management program called CoPilot Health Management System. It holds up to 400 tests, eliminating the oldest as new ones are added beyond 400, just like all the other meters described in this section. You can see a 7-, 14-, and 30-day average on the screen. No calibration is required. The meter has four programmable alarms to remind you to test. It uses CR2032 coin cell batteries available at drugstores and grocery stores. You can test away from your finger with this meter.
- FreeStyle InsuLinx: This meter has a touch screen that allows you to record your insulin dose. It holds 500 tests. It uses the CR2032 coin batteries and is associated with a data management program.
- FreeStyle Lite: This meter is identical to the Freedom Lite but is smaller, with a smaller screen and smaller buttons.
- Precision Xtra: This meter allows measurement of blood ketones as well as glucose. It uses its own test strips that require calibration of the meter with each new vial. The vial contains a calibration strip that is inserted into the meter before using the test strips in that vial. If you want to do a blood ketone test, you use the calibration strip that comes in that vial before inserting the ketone strip. The meter remembers the last 450 tests that you do and you can view 7-, 14-, and 30-day averages on the screen. It uses its own test strips. It has its own data-management system called Precision Xtra Advanced Diabetes Management System.
AgaMatrix
AgaMatrix was the first company to manufacture a meter that attaches to the iPhone and uses the iPhone screen to provide information. AgaMatrix also manufactures three other meters that use a CR2032 lithium coin-cell battery. They also use the Zero-Click software for data management. And they all need only a 5-microliter drop of blood.
- Wave Sense Jazz: The Jazz requires no calibration. It can remember 1,865 tests. It has seven user-settable alarms.
- Wave Sense KeyNote: The KeyNote is one of the smallest meters on the market. It remembers 300 tests. It can provide 14-, 30-, and 90-day averages on the screen. It has six alarms you can set, and it alerts you if the glucose is too low or too high. You have to calibrate the KeyNote.
- Wave Sense Presto: The Presto also remembers 300 tests and provides the same averages as the KeyNote. It also has the same alarms. You don’t have to calibrate this meter.
- IBGStar: With Sanofi-Aventis, AgroMatrix developed IBGStar, the tiny meter that attaches to your iPhone, turning its screen into a meter screen. It is available for sale in Europe, and it has been approved by the FDA in the U.S. but is not yet available for sale there.
Bayer HealthCare LLC
Bayer HealthCare LLC sells five meters in the United States. The meters are accurate and carry the longest warranty in the industry (five years). You can replace the batteries at home. The meters are descendants of some of the first meters available. They allow testing away from your fingers, and no coding of the meters is required. One of them, the Contour USB, is particularly interesting.
- Breeze 2: The Breeze 2 uses a ten-test cartridge that calibrates the meter. It remembers 420 tests. It can provide 1-, 7-, 14-, and 30-day averages. The meter uses WinGlucofacts software for data management.
- Contour Next: This meter uses individual test strips that require no coding. It remembers up to 800 tests that can be downloaded and viewed with the same data-management system as the Breeze 2. It can provide a 7-, 14-, and 30-day average on the screen. It uses 3-volt lithium batteries. Contour meters use individual Contour test strips.
- Contour Next USB: The Contour Next USB is a small meter that plugs directly into the USB port of your computer and opens the Glucofacts Deluxe software, which analyzes your tests and shows you patterns, allowing you to make changes for better control, while charging your battery at the same time. The meter remembers 2,000 tests.
- Didget: Didget is a meter that plugs into the Nintendo DS and DS Lite gaming systems, rewarding your child for frequent testing, although it can be used alone. Kids who test get reward points that unlock new levels of the Nintendo games and buy in-game items. It provides 7-, 14-, and 30-day averages. It, too, uses the Contour test strips. It remembers 480 tests.
Prodigy Diabetes Care
Prodigy Diabetes Care makes three meters for the United States called Prodigy meters. The Prodigy Pocket is a small, very portable meter that comes in five colors and remembers 120 tests. The other two meters are more interesting. None of the meters require calibration. You can download them all to Prodigy’s free diabetes management software.
- Prodigy Voice: This meter is meant for the blind. It has raised buttons. When a strip is inserted, it turns on and verbally takes the user through the setup steps and provides the reading verbally as well. It remembers 450 tests.
- Prodigy AutoCode: Prodigy AutoCode talks the user through the steps of testing and speaks the result. It speaks in English, Spanish, French, and Arabic. It remembers 120 tests.
LifeScan
Johnson & Johnson purchased LifeScan, one of the older meter companies. They have a number of meters in competition with one another. The company is very reliable, taking care of problems within 24 hours. You can replace the batteries in LifeScan meters at home. This company also posts its owner’s manuals online in case you need to refer to them. All of their meters require user calibration, an inconvenient step.
- OneTouch UltraMini: This meter is small and portable. It uses a tiny blood sample. Each new vial of UltraMini test strips must be coded in the meter. It remembers 500 tests. It uses a 3-volt CR2032 coin cell battery. However, it has no way to download test results to a computer and no data-management system. Therefore, I don’t recommend it.
- OneTouch Ultra2: This system allows testing away from the fingers. It uses a tiny sample and, therefore, can work with LifeScan’s ultrafine lancets. The result is displayed in five seconds, and the blood is drawn up by capillary action. The meter has a 500-test memory that allows averaging on the screen and connects to a data port using OneTouch Diabetes Management software. You can see 7-, 14-, and 30-day averages. It uses Ultra test strips. You use buttons on the meter to set the code on the meter to the code on the bottle of test strips. You can add flags to each blood glucose test to specify whether the glucose was taken before or after a meal and whether food or exercise was involved. It uses two 3-volt CR2032 coin cell batteries, one for the meter and one for the backlight. The test is measured from whole blood but expressed in plasma-referenced units.
- OneTouchVerio: The Verio has a color-coded dot on the screen to tell you if your result is high, in-range, or low, which you set. It uses two included AAA batteries and comes with the OneTouch Lancing device. Only finger sticks are approved for this device. You can see 7-, 14-, 30-, and 90-day averages on the screen. It remembers 500 test results.
Nipro Diagnostics
Nipro Diagnostics makes five meters that are sold in the United States. Three of them, the TRUEtrack, TRUEbalance, and TRUEresult, have no features that differ from previous meters, but the following two are unusual:
- TRUE2go: The TRUE2go is claimed to be the world’s smallest meter. It twists on the top of a new vial of strips. It uses a 3-volt CR2032 coin cell battery. The memory holds just 99 results. It does not work with a data-management system, so I don’t recommend it.
- Sidekick: This meter is similar to TRUE2go in being a small meter on top of a bottle of strips, but in this case you throw away the entire meter and bottle when you use up the strips, so battery replacement is not necessary. It has a 50-test memory and no data-management system. I don’t recommend it.
Roche Diagnostics
Roche Diagnostics merged with Boehringer Mannheim and now sells its meters. The batteries in these meters are replaceable at home. The meters may be used at alternate sites besides the fingers.
- Accu-Chek Aviva: This meter works with diabetes-management software (DMS). It has a very large memory, storing up to 500 blood glucose values, with 7-, 14-, and 30- day averages onscreen. It requires a tiny sample of blood. It comes with Spanish-language instructions and a phone number for a Spanish-speaking representative. It has a code key with each new bottle of test strips that are made just for this meter. You can set test reminders for up to four times a day with the built-in alarm. It uses a coin cell CR2032 battery.
- Accu-Chek Compact Plus: This meter uses a 17-test drum that requires no test-strip handling or calibration. The results are displayed in five seconds, and it has a 300-test memory that is downloadable to a DMS. You can see onscreen 7-, 24-, and 30-day averages. It uses two AAA batteries.
- Accu-Chek Nano: The Nano “fits in the palm of your hand.” It has a downloadable 500-test memory that can be evaluated by a data management system with all the features of the other two meters.
Roche also makes a software program for people with diabetes called Accu-Chek Compass. It helps patients to better manage their diabetes by providing reports and summaries of the glucose tests.
Four noninvasive meters: Continuous glucose monitoring
Individual blood glucose measurements represent only a moment in time, and blood glucose levels can change in minutes. Potentially more useful devices that can measure blood glucose almost continuously, store the measurements, and download them to a computer are being developed. They may replace the meters in the preceding sections after they improve, but for now they often lag behind finger-stick measurements, especially after a meal or exercise. Each device still requires that you take blood glucose measurements using a finger-stick meter to calibrate these continuous meters. Many patients reject the idea of wearing the devices on their body.
Continuous monitors are most useful when the finger-stick results do not correlate well with the hemoglobin A1c measurements, which is especially the case in people with diabetes who take insulin, both type 1 and type 2. The doctor, knowing the direction of the blood glucose throughout 24 hours, can adjust the rapid-acting and long-acting insulin more accurately without causing hypoglycemia.
Several reports in Diabetes Care since 2010 have shown that continuous glucose monitoring is effective in lowering the hemoglobin A1c in poorly controlled patients on insulin who have type 1 diabetes and even in well-controlled type 1 patients. It is also effective in type 2 patients on multiple insulin injections. It lowers hemoglobin A1c without increased low blood glucose and has a positive effect on quality of life. A report in January 2012 in that journal showed that even type 2 patients on pills benefited from continuous monitoring. They did significantly better during the 12 weeks they were on continuous monitoring and maintained this improvement for 40 more weeks after the continuous monitoring was stopped compared to patients who continued to use finger-stick monitoring.
These studies almost always depend on the manufacturer of the device to provide the device and to fund the study. I leave it to you to decide the effect of such support on the results of the study.
Dexcom G4 Platinum Continuous Blood Glucose Monitor
The G4 Platinum monitor by Dexcom uses a sensor that is changed after seven days. The receiver collects the information every five minutes and displays it onscreen. The screen can show one-, three-, and nine-hour trends as well as alert you when the blood glucose goes above or below a set level. An alarm also sounds when the glucose is below 55 mg/dl. Software called Data Manager 3 helps to display the data on a computer for further understanding of trends. The device is calibrated with a finger-stick glucose reading every 12 hours. It can store up to 30 days of data.
Medtronic Guardian Real-Time
The Medtronic Guardian Real-Time is a continuous glucose meter that uses a sensor that lasts three days and then must be changed. You have to calibrate the meter two hours and six hours after inserting the sensor and every 12 hours after that. You set upper and lower limits, and an alarm alerts you 30 minutes before those limits are reached. It comes in a pediatric model for children and teens. Another nice feature is that the sensor and receiver can be worn under water up to 8 feet deep for up to 30 minutes.
This monitor works with data-management software to show you trends that help you to improve your glucose control. All the results can be viewed with the CareLink Personal Therapy Software. Both the transmitter and the receiver use one AAA battery.
MiniMed Paradigm Real-Time Revel
The MiniMed Paradigm Real-Time Revel is another continuous glucose meter. Medtronic, which makes this meter and the preceding one, has a long history of working in the field of insulin pumps (see Chapter 11). This meter is combined in one apparatus with an insulin pump to accomplish the longstanding goal of creating a “closed loop” system that has been shown to be effective in controlling the blood glucose in children, adolescents, and adults with type 1 diabetes. The sensor must be changed every three days. Closed loop means the monitor uses the measured glucose to determine how much insulin to pump into the patient.
A report in Diabetes Care (December 2011) confirms the potential of the closed-loop system. In this case, the system was used in 6 of 12 pregnant women with type 1 diabetes who were well controlled (with hemoglobin A1c 6.4 percent). The other six women used conventional continuous insulin infusion without connecting to the meter. Both groups remained well controlled during their pregnancy, but the closed-loop group had less severe hypoglycemia and spent less time with low blood glucose levels.
This monitor uses the same CareLink Personal software as the Guardian Real-Time, and its features are similar.
Medtronic Minimed 530G With Enlite CGM
Just like the previous instrument, this one functions as both a glucose receiver and an insulin pump, but its sensor lasts for six days. The Enlite sensor is supposed to be more comfortable and smaller than other sensors. It isn’t yet approved for use in children.
Tracking Your Glucose over Time: Hemoglobin A1c
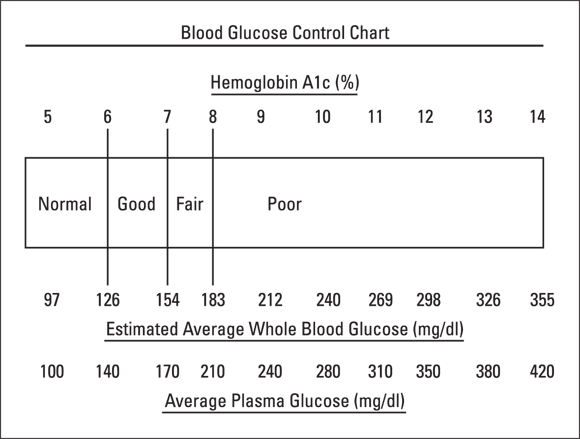
In order to follow your improvement with treatment, you need a test that gives you the big picture, the average blood glucose over time. As I explain in Chapter 2, the hemoglobin A1c is that test. Figure 7-2 shows you the correlation between the hemoglobin A1c and the estimated average blood glucose. By correlating the A1c with the estimated average blood glucose, you can think of the A1c in the same units as the blood glucose that you measure several times a day.
© John Wiley & Sons, Inc.
Figure 7-2: Comparison between hemoglobin A1c and blood glucose.
As you can see in the figure, a normal hemoglobin A1c of less than 6 percent corresponds to an estimated average blood glucose of less than 126, while a fair hemoglobin A1c of 7 percent reflects an average blood glucose of 155.
Large-scale studies have shown that the average hemoglobin A1c in the United States for type 2 diabetes is around 9.4 percent, which means the average blood glucose is 223. The American Diabetes Association recommends taking action to control the blood glucose if the hemoglobin A1c is 8 percent or greater, with the goal being less than 7 percent.
The American Association of Clinical Endocrinologists suggests a goal of 6.5 percent or less. Although I wish all of my patients would achieve a level of 6.5 percent, I try to get them as low as possible but still consistent with a decent quality of life, which means few to no severe hypoglycemic episodes.
- Four times a year if you have type 1 or type 2 diabetes and are on insulin
- Two times a year if you have type 2 diabetes and are not on insulin
In my own practice, I test all patients every three months. A good hemoglobin A1c is highly motivating to keep up good self-care, whereas a poor result gives immediate feedback as to the need for tighter control.
The National Glycohemoglobin Standardization Program, created by the American Association for Clinical Chemistry, has standardized the hemoglobin A1c test so that a 6 percent result means the same thing for every patient.
Another option is to collect your own blood specimen and send it to a company that runs the test and gives you and your doctor a result. Following are some companies currently doing this test:
- AccuBase A1c Glycohemoglobin: Each test costs $29.59 and includes lab analysis and reporting. It can be ordered on the Internet at
Amazon.comor American Diabetes Wholesale.- Phone: 888-872-2443
- Website:
http://dtilaboratories.com/diagprod.htm
- Walgreen’s A1c at Home: This testing service costs $39.99 each including lab analysis and reporting.
- Phone: 800-925-4733
- Website:
www.walgreens.com/store/c/walgreens-at-home-a1c-test-kit/ID=prod6248361-product
Testing for Kidney Damage: Moderately Increased Albumin (MIA)
The finding of very small but abnormal amounts of protein in the urine, called moderately increased albumin (MIA) (formerly microalbuminuria), is the earliest sign that high glucose may be damaging your kidneys (see Chapter 5). When MIA is found, you still have time to reverse any damage.
As soon as you are diagnosed with type 2 diabetes, and within five years of being diagnosed with type 1, your doctor must order a urine test for MIA. If the test is negative, it must be repeated annually. If the test is positive, it should be done a second time to verify the result. If the second test is positive, your doctor should do the following:
- Put you on a drug called an ACE inhibitor: After you have been on this drug for some months, the test for MIA can be repeated to see whether it has turned negative. The ACE inhibitor can be stopped and restarted later if MIA appears again. If ACE inhibitors aren’t tolerated, then ARBs, another class of antihypertensives, may be used. Both classes have been shown to reverse MIA and the ongoing kidney damage it reflects.
- Bring your blood glucose under the tightest control possible. Bringing it under control helps to reverse the damaging process as well.
- Normalize your body fats so that your cholesterol and triglycerides are made normal. Elevated cholesterol and triglycerides have been found to damage the kidneys. (See the section “Tracking Cholesterol and Other Fats,” later in this chapter.)
- Bring your blood pressure under control. Lowering your blood pressure will help to minimize the damage to your kidneys that occurs when they are exposed to elevated blood pressure.
Checking for Eye Problems
All people with diabetes need to have a dilated eye exam done annually (or every two years if no eye disease is present) by an ophthalmologist or optometrist. No other physician, including the endocrinologist (yours truly excepted, of course), can do the exam properly.
For this exam, the doctor instills drops into your eyes and uses various instruments to examine the pressure, the appearance of your lens, and, most importantly, the retina of your eye.
All kinds of treatments can be done if abnormalities are found, but they must be discovered first. (See Chapter 5 for more information on eye problems.)
Examining Your Feet
Failing to take care of your feet leads to problems that often end in amputation. An amputation is really evidence of inadequate care. (For more on foot problems, see Chapter 5.) The doctor is not necessarily at fault here. The doctor sees you once in a while; you’re with yourself much more often.
- You must use your eyes to examine your feet every day.
- You must use your hand to test hot water before you step into it so that you do not get burned.
- You must shake out your shoes before you step into them to make sure no stone or other object is inside them.
- You must not go barefoot.
- You must keep the skin of your feet moist by soaking them in water, drying them with a towel, and applying a moisturizing lotion. (Soaking should always be accompanied by drying and moisturizing.)
Your doctor can test your ability to feel an injury by using a 10-gram filament, but, again, that is done only when you have an appointment. You can obtain one of these filaments for yourself. A couple of the places where you can get them include
- Lower Extremity Amputation Prevention (LEAP) Program:
www.hrsa.gov/hansensdisease/leap - Medical Monofilament Manufacturing, LLC:
www.medicalmonofilament.com, or call 508-746-7877
The other part of a foot examination involves checking the circulation of blood to your feet. To check the circulation, your doctor does a measurement called an ankle-brachial index at least once every five years. The systolic blood pressure is measured in the ankle and the arm. (See the sidebar “The meaning of your blood pressure,” later in this chapter, for an explanation of systolic blood pressure.) The value for the ankle is divided by the value for the arm. An index of greater than 0.9 is considered normal. A value between 0.4 and 0.9 indicates peripheral vascular disease (see Chapter 5), and a value less than 0.4 indicates severe disease.
The ankle-brachial index should be done for any person with diabetes over age 50. Patients under 50 require the study if risk factors such as smoking, high cholesterol, and high blood pressure are present.
Tracking Cholesterol and Other Fats
Most people these days know the level of their total cholesterol, but other tests that show levels of various types of fats in the blood are needed as well.
Cholesterol is a type of fat that circulates in the blood in small packages called lipoproteins. These tiny round particles contain fat (lipo, as in liposuction) and protein. Because cholesterol does not dissolve in water, it would separate from the blood if it were not surrounded by the protein, just like oil separates from water in salad dressing. (That’s why you have to shake the salad dressing each time you use it.)
A second kind of fat found in the lipoproteins is triglyceride. Triglyceride actually represents the form of most of the fat you eat each day. Although you may eat only a gram or less of cholesterol (an egg yolk has one-third of a gram of cholesterol), you eat up to 100 grams of triglyceride a day. (For more on the place of fats in your diet, see Chapter 8.) The fat in animal meats is mostly triglycerides.
Four types of lipoproteins exist:
- Chylomicrons: The largest of the fat particles, these lipoproteins contain the fat that is absorbed from the intestine after a meal. They are usually cleared from the blood rapidly. Ordinarily, chylomicrons are not a concern with respect to causing arteriosclerosis (hardening of the arteries).
- Very-low-density lipoprotein (VLDL): These particles contain mostly triglyceride as the fat. They’re smaller than chylomicrons.
- High-density lipoprotein (HDL): Known as “good” cholesterol, this lipoprotein is the next smallest in size. This particle functions to clean the arteries, helping to prevent coronary artery disease, peripheral vascular disease, and strokes.
- Low-density lipoprotein (LDL): Known as “bad” cholesterol, this smallest particle is the particle that seems to carry cholesterol to the arteries, where it’s deposited and causes hardening.
You don’t have to fast to test for total cholesterol and HDL cholesterol. However, you do need to fast for eight hours to find out your LDL cholesterol and triglycerides, because the blood has to be cleared of chylomicrons, which rise greatly when you eat.
Table 7-1 lists the current recommendations for the levels of these fats in terms of the risk for coronary artery disease.
Table 7-1 Levels of Fat and Risk for Coronary Artery Disease
|
Risk |
LDL Cholesterol |
HDL Cholesterol |
Triglycerides |
|
Higher |
Greater than 130 |
Less than 35 |
Greater than 400 |
|
Borderline |
100 to 130 |
35 to 45 |
151 to 400 |
|
Lower |
Less than 100 |
Greater than 45 |
Less than 150 |
You can see in Table 7-1 that the risk goes up as the LDL cholesterol goes up and the HDL cholesterol goes down. A huge study of thousands of citizens of Framingham, Massachusetts, shows that you can get a good picture of the risk by dividing the total cholesterol by the HDL cholesterol. If this result is less than 4.5, the risk is lower. If it’s greater than 4.5, you’re at higher risk for coronary artery disease. The higher it is, the worse the risk.
In March 2004, the story got a little more complicated. The New England Journal of Medicine published results of a study of more than 4,000 men who had just had heart attacks. In the study, some patients’ LDL cholesterol was reduced maximally (to a mean of 62) with a large dose of a powerful drug called atorvastatin. The result was a major reduction, starting in just 30 days after treatment with the drug, in subsequent heart attacks, chest pain, and strokes compared to a group whose LDL was lowered only to 95. This result calls for a major reappraisal of what LDL is considered normal. Experts agree that the lowest possible LDL level is best and that this policy applies to everyone, not only people who have just had a heart attack.
Diabetes adds its own complication because of metabolic syndrome (see Chapter 5). In metabolic syndrome, the total cholesterol may not be very high, but the HDL cholesterol is low and the triglycerides are elevated. These patients also have a lot of a dangerous form of LDL cholesterol, so they are at higher risk for coronary artery disease. This increased risk must be taken into account in considering treatment for the fats.
- You already have coronary artery disease, stroke, or peripheral vascular disease.
- You are a male over 45.
- You are a female over 55.
- You smoke cigarettes.
- You have high blood pressure.
- You have HDL cholesterol less than 35.
- You have a father or brother who had a heart attack before age 55.
- You have a mother or sister who had a heart attack before age 65.
- You have a body-mass index greater than 30.
You’re at low risk if you have none of the preceding risk factors.
The treatment for abnormal fats with statins (see Chapter 11) then depends on your age and the presence of these cardiovascular disease (CVD) risk factors (see Table 7-2).
Table 7-2 Statin Treatment Based on Risk Factors
|
Age |
Risk Factors |
Statin Dose |
|
<40 |
None CVD risk factors Overt CVD |
None Moderate or high High |
|
40–75 |
None CVD risk factors Overt CVD |
Moderate High High |
|
>75 |
None CVD risk factors Overt CVD |
Moderate Moderate or high High |
All these decisions depend on obtaining a lipid (fat) panel as needed to monitor adherence.
Measuring Blood Pressure
The United States is experiencing an epidemic of high blood pressure (hypertension) similar to the epidemic of diabetes. The reasons are the same:
- Americans are getting fatter.
- Americans are storing fat in the center of our bodies, the so-called abdominal visceral fat.
- Americans are getting older as a population. The fastest-growing segment of the population is over 75 years of age. Of people age 50 to 55 with diabetes, 50 percent have high blood pressure. Of people older than 75 with diabetes, 75 percent have high blood pressure.
- Americans are more sedentary than before.
People with diabetes have high blood pressure more often than the nondiabetic population for a lot of other reasons besides the preceding ones:
- People with diabetes get kidney disease.
- People with diabetes have increased sensitivity to salt, which raises blood pressure.
- People with diabetes lack the nighttime fall in blood pressure that normally occurs in people without diabetes.
Doctors generally agree that a normal blood pressure is less than 140/90. For years, the diastolic blood pressure (the lower reading) was considered more damaging, and an elevation in that pressure was treated with greater importance than an elevation in the systolic blood pressure (the higher reading). More recent studies have shown that the systolic blood pressure, not the diastolic blood pressure, may be more important. (See the sidebar “The meaning of your blood pressure” for more detailed explanations of each type of blood pressure.)
Evidence of the importance of controlling blood pressure in diabetes comes from the United Kingdom Prospective Diabetes Study, published in late 1998. This study found that a lowering of blood pressure by 10 mm systolic and 5 mm diastolic resulted in a 24 percent reduction in any diabetic complication and a 32 percent reduction in death related to diabetes.
For much more information on every aspect of high blood pressure, see my book High Blood Pressure For Dummies (John Wiley & Sons, Inc.).
Checking Your Weight and BMI
To give you a general idea of how much you ought to weigh, you can use the following formula:
- If you’re a woman, give yourself 100 pounds for being 5 feet tall and add 5 pounds for each inch over 5 feet. For example, if you’re 5 feet 3 inches, your appropriate weight should be approximately 115 pounds.
- If you’re a man, give yourself 106 pounds for being 5 feet tall and add 6 pounds for each inch over 5 feet. A 5-foot 6-inch male should weigh around 142 pounds.
Body-mass index (BMI) is a measurement that relates weight to height. A tall person has a lower BMI than a short person of the same weight. (See Chapter 3 for more on BMI, including instructions for calculating your own BMI.) A person with a BMI under 18.5 is considered underweight. A person with a BMI from 18.5 to 24.9 is normal. A person with a BMI from 25 to 29.9 is overweight, and a person with a BMI of 30 or over is obese. By this definition, more than 69 percent of the people in the United States are overweight or obese as of 2012.
Non-white populations like South Asians, Chinese, and blacks develop diabetes at a lower BMI. Ethnicity must be considered in developing prevention techniques and targets for ideal body weight.
The National Heart, Lung, and Blood Institute makes knowing your BMI easy. Using the calculator at www.cdc.gov/healthyweight/assessing/bmi/adult_BMI/english_bmi_calculator/bmi_calculator.html, just fill in your weight in pounds and your height in feet and inches, click “Compute BMI,” and get your result.
Testing for Ketones
When your blood glucose rises above 250 mg/dl (13.9 mmol/L), or if you are pregnant with diabetes and your blood glucose is below 60 mg/dl (3.3 mmol/L), your doctor should probably check for ketones — products of the breakdown of fats. Finding ketones means that your body has turned to fat for energy. If you have high glucose and find ketones, you may need more insulin. If you have low glucose and find ketones during pregnancy, you may need more carbohydrates in your diet.
Testing the C-Reactive Protein
C-reactive protein (CRP) is a substance in the blood that is produced by the liver when infection or inflammation is present. It can be measured with a simple blood test. Diabetes is associated with several features that suggest that inflammation plays an important role in the disease. People who develop diabetes have higher C-reactive protein than those who don’t. (Other substances associated with inflammation are also elevated in diabetes.)
Half the people with diabetes who have heart attacks have low or low-normal levels of LDL (bad) cholesterol. It is believed that inflammation plays a major role in many of these patients. Elevated CRP in the blood has been shown to directly contribute to blood-vessel damage and the formation of blood clots that cause heart attacks.
Drugs that improve diabetes lower the amount of C-reactive protein, which is also considered a marker for coronary artery disease.
Checking the TSH
A screening test called the thyroid-stimulating hormone (TSH) level is done at the time that diabetes is diagnosed and every five years thereafter if it is normal. This test is done because people with diabetes (type 1) have a higher incidence of thyroid disease than the general population, because thyroid disease is often confused with other conditions, and because hypothyroidism can lead to weight gain, which obviously isn’t good for diabetes.
TSH is produced by the pituitary gland in the brain. When the thyroid gland makes the right amount of thyroid hormone, the pituitary produces the right amount of TSH to keep it working properly. The normal level in the blood is 0.5–2.5 microunits per milliliter (μU/ml).
When the thyroid makes inadequate amounts of thyroid hormone, the pituitary increases its production of TSH to stimulate the thyroid, and values of 10 or more μU/ml are not uncommon. When the thyroid makes too much thyroid hormone, it causes the pituitary to turn down its production of TSH, and values less than 0.5 μU/ml are found.
Too much thyroid hormone leads to insulin resistance, making diabetes worse than before. Too little thyroid hormone increases insulin sensitivity, so people with low thyroid function have reduced levels of blood glucose.
Much more about thyroid disease and its treatment can be found in my book Thyroid For Dummies (Wiley).
Evaluating Testosterone in Men with Type 2 Diabetes
About one third of men in the United States over the age of 65 have low levels of testosterone, and a similar percentage of those men have diabetes. Low testosterone is associated with changes in body composition that promote diabetes like increased fat and decreased muscle. According to tests done so far, giving testosterone to these men has not resulted in persistent improvement in glucose metabolism.
Older men who have significant reduction in muscle mass and increase in fat should have their testosterone measured. If very low, treatment with testosterone may be considered by you and your doctor. Such patients should at least make a major effort to increase exercise and decrease caloric intake, which often results in a rise in testosterone.
Checking Vitamin D
Recent studies suggest a relationship between low levels of vitamin D and the development of both type 1 and type 2 diabetes. Communities that live furthest from the equator, getting less sun to make vitamin D, have the highest incidence of type 1 diabetes. Vitamin D protects the body from autoimmunity (where the body attacks itself), and type 1 diabetes is an autoimmune disease. High levels of vitamin D are associated with a lower risk of developing type 2 diabetes. In a study, people who were prediabetic were given vitamin D over three months and showed a significant improvement in glucose metabolism and reduction in hemoglobin A1c. Severe vitamin D deficiency has been shown to predict death and heart attacks in both type 1 and type 2 diabetes.
A study in the Journal of Clinical Endocrinology and Metabolism in September 2010 showed that blood vitamin D levels were low in obese women. The greater the degree of obesity, the lower the vitamin D. When weight was lost, the vitamin D level rose and the insulin resistance declined.
 Certain procedures, explained in this chapter, should be done by your doctor (and you, if feasible) according to the following schedule:
Certain procedures, explained in this chapter, should be done by your doctor (and you, if feasible) according to the following schedule:  These tests are the minimum standards for proper care of diabetes. If an abnormality is found, the frequency of testing increases to check on the response to treatment.
These tests are the minimum standards for proper care of diabetes. If an abnormality is found, the frequency of testing increases to check on the response to treatment. Don’t buy a meter without the capability to download the results to a data-management system in a computer. Bring your meter with you to your appointments so that your doctor or an assistant can download your glucose test results and evaluate them with the aid of a data-management system. Evaluating pages of glucose readings in a log book is virtually impossible.
Don’t buy a meter without the capability to download the results to a data-management system in a computer. Bring your meter with you to your appointments so that your doctor or an assistant can download your glucose test results and evaluate them with the aid of a data-management system. Evaluating pages of glucose readings in a log book is virtually impossible. Testing for ketones is done by inserting a test strip into your urine and observing a purple color. The deeper the color, the greater the ketone level. If you find a large amount of ketones, you should contact your physician. Two sources for ketone test strips are Bayer Ketostix and Nipro Trueplus Ketone Test Strips.
Testing for ketones is done by inserting a test strip into your urine and observing a purple color. The deeper the color, the greater the ketone level. If you find a large amount of ketones, you should contact your physician. Two sources for ketone test strips are Bayer Ketostix and Nipro Trueplus Ketone Test Strips.