6
Private and Public partnership in Healthcare
Bharathi Ghanashyam
Public-private partnerships have sprung up in several states in India to deliver primary healthcare to rural populations. Bharathi Ghanashyam takes a look at one example and asks experts whether similar partnerships should be scaled up to cover the country's entire health sector.
Pattanayakanahalli village lies at a distance of about 172 km from Bangalore on the Bangalore–Mumbai highway in Southern India, 18 km from the nearest town. It is home to a population that is largely made up of landless farmers and small farm holders. Most of these people live below the poverty line and earn less than US$420 each year. The village houses a government Primary Health Centre (PHC) that provides services to 47 surrounding villages, and a population of around thirty nine thousand people 24 hours a day, seven days a week.
It is 12 noon and the outpatient department in the PHC is overflowing with people who have come in with common ailments.
33-year-old Satyamma, however, is not just a routine patient. She has been married for 16 years and is childless. After two abortions and the death of one child who was born with abnormalities, she is in the third month of her fourth pregnancy and is anxious how it will progress. The gynaecologist who is visiting from Bangalore examines her and reassures her that all will be well. Satyamma is under the care of a private gynaecologist and has come in only for a second opinion. At the end of the examination, she shyly inquires whether she can continue visiting the PHC for the rest of her pregnancy.
Another patient—66-year-old Kadirappa—is recovering from tuberculosis and is on the Directly Observed Treatment (DOTS) regimen. He recalls his innumerable trips in the past to private doctors, who he says, merely offered him symptomatic treatment. At the end of two months he had spent around ![]() 2000 ($46), which he had to borrow, and was much worse off than he was when he began treatment. A relative referred him to the PHC where his condition was diagnosed. Two months later, he is feeling much better and, with encouragement from the PHC staff, he says he will complete his treatment.
2000 ($46), which he had to borrow, and was much worse off than he was when he began treatment. A relative referred him to the PHC where his condition was diagnosed. Two months later, he is feeling much better and, with encouragement from the PHC staff, he says he will complete his treatment.
Nagaraj, who has recovered from tuberculosis, has just been diagnosed as HIV positive. He was tested for HIV/AIDS as part of the routine screening for tuberculosis patients at the PHC. The test was done after he was counselled at the integrated counselling and testing centre at the PHC. He is now being persuaded to begin antiretroviral treatment as his CD4 cell count has fallen below desirable levels.
Satyamma, Kadirappa and Nagaraj have one thing in common—they have all used the facilities offered by the Pattanayakanahalli PHC, some of which are unique to it and are not offered at other PHCs. This is because the PHC is being run in a public-private partnership between two entities: Karuna Trust—a public charitable trust based in Bangalore—and the Government of Karnataka—a southern state of India.
Karuna Trust also manages 25 other PHCs across the state of Karnataka, as well as nine in Arunachal Pradesh in northeast India. It has ensured that PHCs under its management provide round-the-clock emergency and casualty services, outpatient facilities six days a week, a five to ten bed in-patient department, and 24-hour labour and essential obstetric facilities. Additionally, the Trust has introduced innovations such as integration of mental health services, eye care, and specialist services at the primary care level.
Karuna Trust has come a long way since taking over the management of its first PHC at Gumballi in Karnataka in 1996 (see table). Its success has led the Karnataka Government to issue a formal policy on public–private partnerships in 2000.
India is a signatory to the Alma-Ata Declaration, which calls for ‘Health for All’ to be achieved in countries through a primary healthcare approach. In 1983, the country's National Health Policy adopted the Alma-Ata definition of primary healthcare to mean the provision of curative, preventive, promotive, and rehabilitative health services. This development was a shift from curative to integrated healthcare with an emphasis on increasing access to health services in rural areas.
To give form to this commitment, a huge infrastructure was established, consisting of a three tier system, that is, primary, secondary, and tertiary care. PHCs are units that provide integrated rural healthcare and also provide referral to secondary and tertiary care. Each PHC covers a population of 20 to 30 thousand. India has about 23 000 PHCs, 1 30 000 subcentres, and one lakh fifty thousand healthcare institutions. Karnataka alone has two thousand one hundred ninty three PHCs. The state of these centres, however, leaves much to be desired.
Hanumappa Sudarshan, founder of Karuna Trust says, ‘Notwithstanding the infrastructure available, all is not well with the primary healthcare system. It has become decrepit and use of PHCs has fallen to abysmal levels, thereby necessitating the involvement of civil-society organisations to shore up the deficiencies’.
Studies indicate that only 69 per cent of PHCs in India have at least one bed. Absence rates among health workers range between 35–58 per cent in different Indian states. Devi Shetty, chairman of the Narayana Hurudayalaya Institute of Cardiac Studies, points out:
Insufficient staff, unavailability of essential drugs, and other problems at government-run PHCs make it difficult for rural communities to get treatment and they are forced to purchase healthcare services from private practitioners. The greater danger, however, is that they will delay accessing treatment for fear of losing wages and bearing out-of-pocket expenses.
He speaks from ground-level experience, since his institution has established, and runs PHCs as part of a pilot programme in Amethi in Uttar Pradesh.
The National Family Health Survey 2005–06 revealed that 46 per cent of children below the age of three years are underweight. India's infant mortality rate is 57 per 1000 livebirths and its maternal mortality ratio is 301 per 100 000 livebirths and should be reduced to below 42 and 109, respectively, to achieve Millennium Development Goals 4 and 5 on child and maternal health. India also has the largest pool of never-immunized children in the world—9·4 million. These are results that the primary healthcare system must account for. Despite its firm commitment to providing primary healthcare, why has India failed on so many counts? Madabhushi Madan Gopal, secretary of the Health and Family Welfare Department, Karnataka says, ‘The government lacks managerial skills and professionalism. We have also fallen behind in establishing community rapport and enabling convergence between the various departments that look at health, water, and sanitation, etc’.
Since public-private partnerships translate into benefits for those seeking healthcare, should they be scaled-up to cover the entire sector? Sudarshan disagrees firmly:
Primary healthcare is the responsibility of the state. PPPs [public–private partnerships] are not alternatives to poor governance and leadership. Even with the PHCs we manage, there are variable degrees of progress. In districts where the District Health Officer understands the rationale of the PPP and provides constructive leadership, the progress has been tremendous. In others, progress has been slow. PPPs can work only with the support of strong, honest, and able governance.
Devi Shetty, however, strikes a different note:
I believe that primary healthcare must be offered free, but it is not mandatory for the government to do this. Governments across the world have failed in providing free primary healthcare to the community. Private players can provide better services as they operate to economies of scale and bring in professionalism. If health insurance becomes mandatory, primary health services offered by the private sector will translate into benefits for the poor.
Madan Gopal believes,
primary healthcare must never be sold and, as a nation, we cannot afford profit at the expense of the poor. We need long-term planning and sustainable policies, as well as greater spending on healthcare. Partnerships to share skills and not substitution by business enterprises are what we require additionally. Most importantly, we need a community-centred approach to the health sector, as spelt out in the Alma-Ata Declaration, so that the community has a greater say and can force change.
Whether the primary healthcare in India will be opened up to the private sector remains to be seen. It is, however, a healthy sign that debate has begun.
Vocabulary
- Poverty line: The official level of income that is necessary to buy the basic necessities of life such as food, clothes, etc.
- Ailments: Illnesses that are not very serious
- Symptomatic treatment: A cure that depends on the external signs of a disease instead of its causes
- Innovations: New ways of doing thing
- Antiretroviral: A retrovirus is a virus that gets into the cell and reverses the general function of the cell which is to transcript DNA into RNA and RNA getting translated into proteins
- Referral: A healthcare facility where patients are sent by doctors for better treatment
- Decrepit: Old, feeble, not in good condition or health
- Abysmal: Extremely bad or of a very low standard
- Rapport: A friendly relationship between communities or people that helps in professional work
- Convergence: Meeting point of different directions or angles. In this case, it means the meeting of different public offices on the common goal of providing primary healthcare.
Reading Comprehension
- Define poverty line in keeping with the bench-mark the author of the above passage has employed.
- Quote one sentence from the second paragraph of the passage that suggests that the PHC at Pattanayakahalli is different from other such agencies. (Hint: It has something to do with the patient called Satyamma)
- Discuss three kinds of roles of the Karuna trust.
- Discuss the state of affairs of the PHCs in India. Bring in data into your discussuion. You also need to talk about the problems that plague the PHCs.
- Is private-public partnership the only way to make primary healthcare functional in India? Can you think of any problem that privatization entails?
Language
An article belongs to a word-class called determiners. They precede a noun and tell us whether the referent is definite or indefinite. In other words if a noun is the name of something, the article lets us know whether the thing can be identified specifically or not.
Now read the following passage:
India is a1 signatory to the2 Alma-Ata Declaration, which calls for ‘Health for All’ to be achieved in countries through a3 primary healthcare approach. In 1983, the4 country's National Health Policy adopted the Alma-Ata definition of primary healthcare to mean the provision of curative, preventive, promotive, and rehabilitative health services. This development was a shift from curative to integrated healthcare with an5 emphasis on increasing access to health services in rural areas.
In the above passage, 1, 3 and 5 signal nouns that are either one of many. There are many signatories to the Alma-Ata declaration and India is just one of the many. Similarly, there are many approaches to ensure that everybody receives healthcare; focusing on primary healthcare is just one of the many approaches. The emphasis on increasing access to health services in rural areas is one of the many possible areas of emphasis. On the other hand, 2 and 4 signal specific objects about which there is a consensus between the author and the reader. There can be only one Alma-Ata agreement—it is historically specific event. And, in 1983 there can be only one National Health Policy.
A/an are, thus, indefinite articles that are used with singular and countable nouns. There is also something called a Φ article, also known as a zero article. It refers to indefinite plurals. Now, re-read the sentence: This development was a shift from curative to integrated healthcare with an5 emphasis on increasing access to [Φ] health services in rural areas. ‘Health services’ refer to no particular strategy or service (primary healthcare or setting up super-speciality hospitals) and hence we can ‘sense’ the zero article. Understanding the concept of the zero article helps us avoid confused use of the definite/indefinite articles.
Exercise
- Fill in the blanks with the correct article following the instructions in parenthesis:
- There is _________ stapler on the desk. (no particular stapler)
- There is ___________ gentleman outside the office of Mrs Dutta. (no particular gentleman)
- _____ committee on public affairs (a particular committee) was set up by ____ new government. (a specific government)
- __________ good film (any good film) has to have ________ good script.
- __________ film that gave me great pleasure was Shoot the Piano Player.
- Fill in the blanks with the correct article:
- ___________ fresh air is needed by all growing children.
- __________ gust of fresh air can rid us of depression.
- ____________ photocopying machine in our office is seldom in order.
- We need __________ photocopying machine in our office.
- _________ moon has been enveloped by clouds. It was _________ gloomy day.
- _________ cup of hot chocolate is _______ drink you need on a cold and damp day.
- He likes to study ________ astrophysics.
- He went to _______ USA to get _________ degree in _________ astrophysics.
- _________ teaspoon of honey helps ________ lot in ________ winter.
- This year, we expect ______ good harvest. _____ rains were adequate.
Conveying information and eliciting information: agreeing and disagreeing
The following conversation between a nurse and a doctor is an example of how information ought to be exchanged between them. The conversation also teaches you to agree, disagree and make crucial interventions within a conversation. The doctor often depends on the nurse to understand the criticality of the patient. It is important that the nurse is clear about what she wants to convey.
Nurse: Good Morning Dr Varghese, your patient Mr Nayar is complaining of malaise and fever.
Doctor: Thanks for your prompt attention. Did you check his body temperature?
Nurse: It is 102 degree Fahrenheit. But, yesterday at 10 pm, it was within normal limits.
Doctor: Does he have fever with chill and rigor?
Nurse: The patient is complaining of chill but not rigor.
Doctor: What are the medicines that he is taking, right now?
Nurse: He is on Amlodipine 5 mg daily and Tablet MV once daily. His blood pressure is normal now. But, he has been catheterized for the last nine days.
Doctor: Good that you informed me of this. Prolonged catheterization might lead to urinary tract infection. Send her urine-sample for routine examination and culture sensitivity, please. Do inform the Department of Laboratory Medicine that it is urgent.
Nurse: Sure. Do we need to add any new medicine?
Doctor: Administer tablet Paracetamol 500 mg four times every day and continue with the other drugs. Do call me up when you get the provisional report as the final culture sensitivity test will take time. I will add antibiotics if required.
Nurse: Thank you. I will do as much. Have a good day.
Doctor: Thank you and you have a good day too!
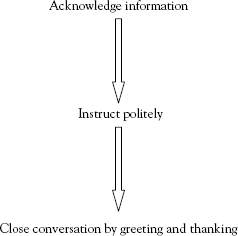
The above conversation teaches you to greet and begin or end a conversation. Observe how the doctor acknowledges information that the nurse passes on to him. Question forms using the ‘does…have’ form is used to request information. The basic form is to use the do verb with the have verb. In case of a singular subject, we use do + have form. Expressions like will do as much convey a sense of agreement.
Re-read what the doctor has to say in the extract, from the above conversation, that follows
Good that you informed me of this. Prolonged catheterization might lead to urinary tract infection. Send her urine-sample for routine examination and culture sensitivity, please. Do inform the Department of Laboratory Medicine that it is urgent.
In the above conversation, expressions note the use of the do + basic verb form to make requests. Again, adding a please after a comma, as in the second sentence, is a polite but firm way of placing a request.
A communication model that one can follow is this:
Practise in pairs
Use the words in the box to form a conversation similar to the one above:
Stethoscope, gasping patient, ventilator, intensive care unit, shift, Post-operative trauma, cardiovascular surgery, lipid profile check, chest x-ray, creatine phosphokinase test.
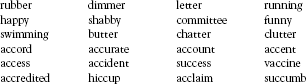
Pronunciation: Double consonants
All double consonants except ‘cc’ are pronounced as single consonant sounds. ‘cc’ may be pronounced as /ks/ when followed by ‘e’, ‘i’, or ‘y’ or /k/ when followed by the rest of the letters. Check these words in a good dictionary:
Writing
Write a diary-entry about a nurse's day in a ward.
