5
The Health Scenario
S. N. Jha
The provision of health services constitutes an important element of the Directive Principles of State Policy. To fulfil this mandate, a number of institutions have been created. At the national level, the official organs of the health system consist of the Union Ministry of Health and Family Welfare, the Directorate General of Health Services (DGHS) and the Central Council of Health and Family Welfare. The Centre is mainly responsible for policy making, planning, guiding, assisting, evaluating and co-ordinating the work of the State Health Ministries, so that health services cover the entire country. Constitutionally, ‘public health and sanitation, hospitals and dispensaries’ are in the State List. Like the Centre, the states too have ministries and directorates of health.
PLAN ACHIEVEMENTS
Achievements in the health sector during the First Plan period included setting up of health infrastructure—the opening of new hospitals, dispensaries, health units and maternity and child-health centres. The principal developments related to the expansion of health services were initiatives to improve water supply and sanitation, control communicable diseases, and train personnel. Following the recommendation of the Health Survey and Development Committee of 1946, a chain of primary health centres was envisaged. These were intended to serve as focal points for the development of curative and preventive health in rural areas. They were a part of the Community Development Blocks and were financed under the Community Development Programme. Seven hundred and twenty-five Primary Health Centres were established during the First Plan. Training facilities for the personnel in the health centres were provided at three reorientation centres at Singure, Poonamale and Najafgarh.
Water supply and sanitation (both rural and urban) constituted a major thrust area under the health services: ‘The provision of safe and adequate water supply is a basic pre-requisite in a country in which a large number of persons become victims of water and filth-borne diseases’. The central government also set up a nucleus central public health engineering organization at the office of the DGHS for examining the technical aspects of the schemes proposed by state governments. Some steps were taken to expand training facilities in Public Health Engineering as well, with the All India Institute of Hygiene and Public Health, Calcutta, the Roorkee Engineering University, and the Guindy Engineering College providing a year's course leading to a Master's degree in the subject.
For the control of communicable diseases like malaria and filariasis, special programmes were undertaken. Measures for combating tuberculosis included the BCG vaccination, which began in 1948 and was soon expanded. Further programmes of treatment, study, survey and research were undertaken for curing leprosy and a beginning was made with regard to the treatment of and research on several other diseases. The government also provided for research in alternative medicine, including indigenous medicinal systems. Under this programme, assistance was extended to the Central Institute of Research in Indigenous Systems of Medicine at Jamnagar, and support was given to research in ayurvedic, unani, homeopathic and nature cure systems.
In view of the shortages of medical and auxiliary staff, the training of health personnel had a high priority in the programme for developing health services. During the First Plan, the number of medical colleges increased from 30 to 42 and the number of annual admissions to them rose from 2,500 to 3,500. The training of personnel like nurses, midwives, dais, nurse-dais and the ANM (auxiliary nurse and midwife) was also expanded. The All India Institute of Medical Sciences was set up and research and training facilities were improved in several of the institutes and research centres. With the establishment of a public sector penicillin factory in March 1955, facilities for drug production were improved.
A new phase began with the Fifth and Sixth Plans. These were, in general, ‘improvement plans’. Their programmes aimed at increasing the accessibility of health services, correcting regional imbalances, and developing referral services by removing the deficiencies in district and sub-divisional hospitals. Further, a policy emphasis was made on the intensification of the programme for control and eradication of communicable diseases like malaria and smallpox. In the Fifth Plan, a substantial increase in the outlay for the National Malaria Eradication Programme became necessary to contain the disease according to a revised strategy. Provision also became more effective for the implementation of National Leprosy Control and the control of blindness. Another policy prong was the education and training of health personal and the development of referral services via provision of specialist attention to common diseases in rural areas. The Minimum Needs Programme was the main instrument through which health infrastructure in the rural areas was expanded and further strengthened to ensure primary health care to the rural population. It is noteworthy also that the Fifth Plan for the first time proposed inclusion of health education in the school curriculum.
Developments in the international sphere also had a role to play in the health scene. Thus, India adopted the policy of ‘Health for All by 2000 AD’, enunciated at Alma Ata Declaration in 1977. In this context, rural health care was proposed to be developed as a speciality and various programs of education, water supply and sanitation, control of communicable diseases, family planning, maternal and child health care were to be implemented in a coordinated manner. More medical personnel were to be put into action for better performance.
In the Sixth Plan period, the National Health Policy was formulated. ‘The National Health Policy (1982) was evolved within a fully integrated planning framework which sought to provide universal comprehensive primary health care services relevant to the actual needs and priorities of the community at a cost which people can afford. The planning and implementation of various health programs were to be through the organised involvement and participation of the community, and also by adequately utilising the services being rendered by private voluntary organisation active in the health sector’.1 The policy underlined the need of restructuring health services around the following approaches:
- Provision of a well-dispersed network of primary health care services with the organized support of volunteers, auxiliaries, paramedics, and adequately trained multipurpose workers.
- Backup support to primary health care through a well worked out referral system.
- Full utilization of untapped resources through organized logical and technical support to voluntary agencies active in the health field.
- Priority to be accorded to people living in tribal, hill and backward areas and to populations affected by endemic diseases.
With its stress on rural health infrastructure, the Sixth Plan outlined these norms for making a stronger rural health sector.
- One Community Health Volunteer for every village or a population of 1,000 chosen by the community to form the base unit.
- One sub-centre for a population of 5,000 in plains and 3,000 in hilly and tribal areas.
- One Public Health Centre for 30,000 population in the plains and 20,000 in hilly and tribal areas.
- One Community Health Centre for population of one lakh or one C.D. Block.2
- The Community Health Volunteer Scheme and the scheme of training and employment of multipurpose workers to be continued under the Minimum Needs Programme.
The Seventh Plan sought to actively promote the norms envisaged in the Sixth Plan and aimed at the consolidation of the health infrastructure by making up the deficiencies with regard to training of personnel, equipment and other physical facilities.
In the urban areas, the health services were to be made more widespread and efficient by creating a network of hospitals with specialized services in district hospitals. It was recognized that urban hospitals and medical facilities act as a referral system as well for the rural areas; hence, there was a need to develop them further. Drug Control and Medical Stores Organization, Prevention of Food Adulteration, Training and Manpower Development, Blood Bank and Transfusion Services were other important areas focused upon in the Seventh Plan.
The Eighth Plan's thrust areas were on the following:
- Major investment in development and strengthening of primary health care infrastructure, aimed at improvement in quality and outreach of services.
- Consolidation and expansion of the secondary health care infrastructure up to and including the district level services.
- Optimization of the functioning of tertiary care.
- Building up of referral and linkage system so that optional utilization of available facilities is possible at each level.3
Concerted efforts were made to ensure that essential health care for the neediest sections of the populations are met. Some important steps in this regard included efforts to consolidate and strengthen the primary health care infrastructure with earmarked funding under the Minimum Needs Programme; enhanced assistance to regions with severe problems, for example, 100 per cent assistance under the National Malaria Eradication Programme (NMEP) for tribal areas and northeastern states plagued by Falciparum malaria; enhanced central assistance to specific programmes to meet the cost of treatment, such as tests for the screening of donated blood so as to check whether it is infected with the human immunodeficiency virus (HIV); cost of drugs for short course chemotherapy for tuberculosis; and cost for cataract surgery for the elderly. Specific efforts were also made to promote the Indian system of medicare and homeopathy. Another notable feature of the Eighth Plan was its support to the involvement of voluntary organizations.4
The Ninth Plan resolved to improve access to and enhance quality of primary health care in both rural and urban areas by providing an optimally functioning primary health care system as a part of basic minimum services. The plan also introduced a concept of horizontal integration of the vertical programmes such as disease surveillance, production and distribution of vaccines, improvement of water quality and environmental sanitation, and hospital infection control and waste management. Panchayati Raj Institutions were put in charge of planning and monitoring of health programmes at the local levels so as to facilitate greater responsiveness to health needs of the people, greater accountability, inter-sectoral coordination, and better utilization of local and community resources. The role of voluntary and private organizations and self-help groups was sought to be increased in provision of health care and inter-sectoral coordination in implementation of health programmes and health care activities.
Operationalization of the Health Management Information System (HMIS) was emphasized as one of the strategies to promote efficiency of the existing health care infrastructure. Likewise, an integrated program for the prevention and control of non-communicable diseases was to be developed and implemented. A disease surveillance and response mechanism with focus on rapid recognition, report and response at the district level was accorded high priority to ensure rapid containment and control of outbreak of communicable disease. Health impact assessment was introduced as a part of environmental impact assessment in developmental projects as a part of the drive for prevention, detection and management of the health consequences of the continuing deterioration of ecosystems.
The Tenth Plan continued the focus on access to health services and improvement of the quality of services. The horizontal integration of all aspects of the current programmes is re-emphasized. The re-organization and re-structuring of the existing governmental health care system at the primary, secondary and tertiary levels with appropriate referral linkages is being focused upon so as to make them capable of handling all health problems and provide all required services in a particular geographical area. The document also talks of building an effective system of disease surveillance and response at different levels. There is an emphasis on decentralization and devolution of funds and responsibilities to Panchayati Raj Institutions. The HMIS is emphasized again, as an instrument for making readily available information on births, deaths, diseases, drugs and the like and also, facilitate decentralized planning, implementation and monitoring of health services. There is also an expressed need to improve the efficiency of the health care systems and build appropriate linkages between the government, private and voluntary sectors. Increasing involvement of the voluntary and private organizations, self-help groups and social marketing organizations has been focused upon in improving access to health care. Health has been linked to the environment and health impact assessment is sought to be made a part of environmental impact assessment of developmental projects. Screening of common nutritional deficiencies especially among vulnerable groups to enable appropriate measures is also talked about, maybe for the first time.
PUBLIC EXPENDITURE ON HEALTH
Despite continuous increase in non-defence expenditure, the percentage of expenditure allotted for health has been sluggish over the years. It may be noted that the Health Survey and Development Committee of 1946 (the Bhore Committee) recommended that 15 per cent of the total public expenditure should be on the health sector. The Health Survey and Planning Committee of 1961 (Mudaliar Committee) had reduced the target to a 10 per cent of the total public expenditure, but even by that criterion, the expenditures in the first six plans have been insufficient, varying between 3 and 5 per cent. Given the magnitude of health needs, the government's expenditure on health has been extremely inadequate.
PREVENTIVE HEALTH PROGRAMMES
A number of National Health Programmes are in operation in India for taking concerted measures to combat certain communicable, non-communicable and other major diseases. These not only have a bearing on the reduction of mortality and morbidity and make an effort to improve the quality of life of the common man, but also reinforce the delivery of primary, secondary and tertiary health care throughout the country.
National Malaria Control Programme (NMCP)
This programme was launched in 1953. According to the estimates for 1952–1953, about 200 million people were residing in the endemic areas, with 75 million cases of malaria occurring annually and 8 lakh deaths resulting directly from malaria. The objective of the NMCP was to spray affected areas periodically with DDT (dichlorodiphenyltrichloroethane) so as to lower the transmission level. The success of this programme was phenomenal. The number of malaria cases for every 100 persons visiting hospitals or dispensaries declined form 10.2 per cent in 1953–1954 to 4.0 per cent in 1958–1959. This led the planners to think in terms of a complete eradication of malaria.5 NMCP was upgraded in 1958 and renamed as the National Malaria Eradication Programme. This programme was also a success. While the number of malaria cases in 1947 was 75 million, in 1963, incidence came down to a mere 49,151, with annual mortality down to zero.
In 1963, a committee to review the NMEP was appointed, with the Director General of Health Services as the chairman. The committee suggested the ‘vigilance’ operation with respect to NMEP as being the responsibility of general health services, at the primary health centre at the block level. One basic health worker per 10,000 of the population was recommended. These workers would also have the additional responsibilities for the collection of vital statistics and family planning. Family planning health assistants were to supervise three or four of basic health workers.
Some states (seven) also had an Enhanced Malaria Control Programme funded by the World Bank in the hyper-endemic areas. It was a 5-year programme that started in 1997–1998. The components of this programme are Early Detection and Prompt Treatment (EDPT), selective vector control, personal protection, epidemic planning and institutional strengthening through training to all categories of staff, improvement of the management information service and IEC (information, education and communication) activities.
National Tuberculosis Control Programme
The District Tuberculosis Control Programme was initiated in 1962. Community control of tuberculosis was started by organized domiciliary treatment. This programme is centrally sponsored on a 50:50 shared basis between the Government of India and the state governments. Its strategy comprises (a) detecting active cases in the early stage and treatment through the District Tuberculosis Control Programme and (b) protecting the health of especially those less than 20 years of age by BCG vaccination. Assistance for the programme has been received from international bodies like the Swedish International Development Agency and UNICEF.
National Leprosy Control Programme
The programme was launched in 1954–1955, in collaboration with state governments, to control the disease and enable leprosy patients to benefit from modern treatment facilities. The programme was implemented through the establishment of the Leprosy Control Units/Centres (LCU), the Survey Education Treatment (SET) Centres, Urban Leprosy Centres, temporary hospitalization wards, reconstructive surgery units, etc. The programme initially progressed very slowly and developed in phases over 25 years. From the Fourth Plan onwards, it was made a centrally sponsored scheme.
National Programme for Control of Blindness
The National Programme for Control of Blindness was started in 1976 with the objective of providing comprehensive eye care services at the primary, secondary and tertiary health care level and achieving substantial reduction in the prevalence of eye diseases in general and blindness in particular. Substantial progress has been made over the years in developing institutional capacities and strengthening service delivery, but the objective of reducing blindness from 1.4 to 0.3 per cent by 2000 was not achieved. Quality of care in the eye camps has been sub-optimal. The realization has brought on the drive towards upgradation of medical colleges and district hospitals, and the training of ophthalmologists. The World Bank-assisted Cataract Blindness Project is being implemented in seven states of the country with the aim of reducing the prevalence of blindness from 1.4 to 0.3 per cent by providing training to ophthalmic manpower, by upgrading the existing infrastructure and providing new infrastructure facilities for treatment of blindness and for providing eye care facilities to the people.
National AIDS Control Programme
In India, the National Sexually Transmitted Diseases (STD) Control Programme started in 1967. However, the programme's outreach and coverage have been sub-optimal, and there is no nationwide surveillance system for STD. As the gravity of the HIV epidemic was realized in India, the National AIDS Control Programme was begun in 1992 as a 100 per cent centrally sponsored scheme. The objective was to prevent and minimize the spread of the epidemic. The programme operates through the existing health care systems, and is geared to collect epidemiological data on HIV infection through Sentinel Sero Surveillance and AIDS Surveillance. It seeks to strengthen STD control and AIDS control, and seeks to improve facilities for clinical management of AIDS cases, as also, awareness about HIV/AIDS through IEC.
Universal Immunization Programme
The Universal Immunization Programme, previously known as the Expanded Programme of Immunization (EPI), is a long-term programme aided by UNICEF. This most well-known of the country's preventive programmes was launched by the Central government in 1978. Its main objectives were to (a) deliver an integrated immunization service through primary health centres and sub-centres in rural areas, (b) reduce the incidence of diphtheria, whooping cough, tetanus, polio, tuberculosis, and typhoid fever by making vaccination services available to all children and pregnant women, and (c) develop a surveillance system to collect adequate information on the diseases preventable by immunization.6 Findings from a recent study indicates that overall, immunization of children was far more extensive in districts covered by the CSSM (Child Survival and Safe Motherhood) Programme.7
Other Programmes
There are other programmes also like the Filarial Control Programme, STD and AIDS Control Programmes, and the programme for the control of goitre. India is also a part of the worldwide WHO programme to protect children from six major diseases: diphtheria, whooping cough, tetanus, tuberculosis, polio and measles.
Preventive Programmes—Policy Implications
These preventive programmes had a major influence on the growth and development of health services. Called vertical programmes, they are sponsored by the central government and have a uniform line of command for implementation. Each of these programmes has had its own specially trained personnel. Since communicable diseases have accounted for a substantial mortality and morbidity, mass national campaigns have been of much help. But preoccupation with these programmes has meant that an integrated approach for the health sector has suffered.
NUTRITION AND CHILD SURVIVAL
Malnutrition was seen in the plans mainly as a problem of poverty, due to which a large number of the poor could not afford a ‘balanced diet’.8 Since the early plans, schemes to combat malnutrition have been introduced. It was recognized that food production had to be increased to tackle malnutrition and to improve the nutritional status of the population, hence the need for a stress on agriculture and allied activities. It was also recognized that children and pregnant and nursing mothers were especially vulnerable. Over the years, the range of direct interventions expanded to cover supplementary feeding of children and mothers, production of nutritious foods, fortification of foods, nutrition and health education of mothers, and prophylactic programmes against identified nutritional deficiencies. In the Fifth Plan, supplementary feeding programmes were brought under the Minimum Needs Programme (MNP) and also became a component of Integrated Child Development Scheme (ICDS). In the Sixth Plan, a substantial increase in allocation for poverty alleviation programmes was visualized as a means to increase the purchasing power of the rural poor so as to enhance food intake.
During the first three plans, nutrition formed one of the components of the health sector and was not singled out as such for specific plan programmes. It was only in the Fourth Plan that an Integrated Nutrition Programme was introduced. By 1973, the Applied Nutrition Programme introduced in 1960 was extended to all the states and union territories. It aimed at spreading the concept of balanced diets, production and consumption of protective food, and proper techniques of cooking. In the Fifth Plan, in 1962–1963, the Mid-Day Meal programme (MDM) for providing supplementary food to school children was introduced as a part of the Minimum Needs Programme. The Special Nutrition Programme (SNP) for school children and pregnant women and nursing mothers, introduced in 1970–1971 and originally launched as a Central programme, was transferred to the state sector in the Fifth Plan as a part of the Minimum Needs Programme. Since the start of the ICDS programme in 1975–1976, the Special Nutrition Programme has been in operation as a part of the ICDS projects, although there are feeding centres outside this project also.
The future government strategy reflects the need to emphasize the value of diversification and improvement of diets. These include increased production of cereals and pulses, green leafy vegetables, fruits, eggs, fish and milk, and their availability at an affordable rate. Direct nutrition intervention programmes will need to focus on children below 6 years of age, adolescent girls, and pregnant and nursing mothers, those belonging to lower income groups, scheduled castes and scheduled tribes, and those living in drought prone, backward and hill areas, and in urban slums. Special attention was to be given to tackle the nutritional problems of anaemia, vitamin A deficiency, goitre and fluorosis. Area-specific nutritional problems need especially to be looked into and community participation emphasized for the success of nutrition programmes and optimal utilization of the public distribution system. The long-term nutrition policy aims at increasing the functional efficiency of the labour force and other segments of the population by promoting the concept of balanced intake with locally available balanced food commodities. The nutrition policy should also achieve reduction in infant and maternal mortality rates and bring about changes in the prevailing patterns of morbidity.
PLANNING FOR HEALTH: REACH AND IMPACT
According to the World Development Indicators brought out by the World Bank in 2004, 5.1 per cent of GDP was spent on the health sector in India. This compares favourably with the corresponding figures for countries like Ethiopia, Tanzania, Bangladesh, Nigeria, Pakistan, Sudan, Egypt, Indonesia, Philippines, Morocco, Syria, Columbia, Peru, Thailand and Algeria. At the other extreme, countries like France, Canada, the United States and Germany spend at least double, in terms of GDP share. In terms of per capita expenditure also, India compares favourably with Bangladesh, Pakistan, Indonesia, Ethiopia and Tanzania, but lags behind other countries, especially countries of the West.
In India, the per capita expenditure on health grew by 12 times between 1980–1981 and 2000–2001 (Table 5.1). The union government's expenditure in the category ‘Medical, Public Health and Family Welfare’ also has increased from 13 per cent of the total revenue expenditure in 1989–1990 to 15 per cent in 1995–1996. However, according to a detailed analysis, most of the increase was on account of increased allocations since 1992–1993 for the National Tuberculosis Control Programme and the National AIDS Control Programme. The National Malaria Education Programme also recorded increased allocations since 1993–1994.9
Further, at a disaggregated level, data attest to significant state-wise variations in health expenditure. Between 1974–1975 and 1990–1991, real per capita government expenditure on ‘Medical and Public Health’ showed an increasing trend, but some states were ahead of others. Moreover, if this period is broken up into two segments, 1974–1975 to 1984–1985 and 1985–1986 to 1990–1991, we find that in the later period, as many as seven states reported a negative growth rate in real per capita revenue expenditure.
Table 5.1
Per capita expenditure on health, India, 1980–1981 to 2000–2001
| Year | Per Capita Expenditure (in Rupees, at Current Prices) |
| 1980–1981 | 14 |
| 1981–1982 | 17 |
| 1982–1983 | 19 |
| 1983–1984 | 22 |
| 1984–1985 | 26 |
| 1985–1986 | 29 |
| 1986–1987 | 33 |
| 1987–1988 | 37 |
| 1988–1989 | 42 |
| 1989–1990 | 46 |
| 1990–1991 | 54 |
| 1991–1992 | 57 |
| 1992–1993 | 64 |
| 1993–1994 | 70 |
| 1994–1995 | 76 |
| 1995–1996 | 85 |
| 1996–1997 | 98 |
| 1997–1998 | 112 |
| 1998–1999 | 137 |
| 1999–2000 | 156 |
| 2000–2001 | 167 |
Source: Selected Socio-Economic Statistics, 2002, Central Statistical Organization, Ministry of Statistics and Programme Implementation, Government of India. Table 4.11: Expenditure in rupees on education, health and social security and welfare services in India.
Despite the picture of increasing health expenditure and the growth of infrastructure, the health scene in India is quite dismal. Infant mortality rates are quite high and the figures are higher in backward states and in rural areas. The link between under-nutrition, morbidity and mortality is the main underlying factor.10
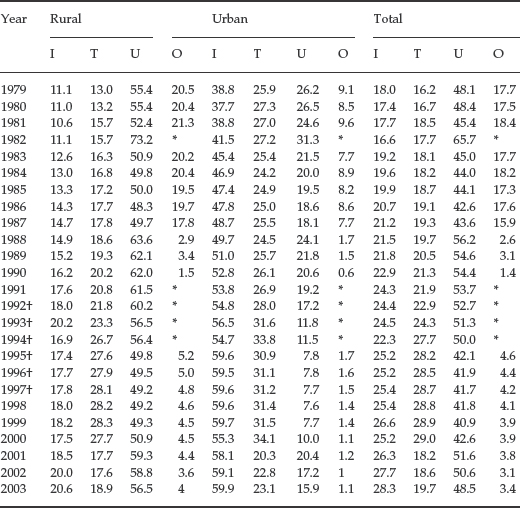
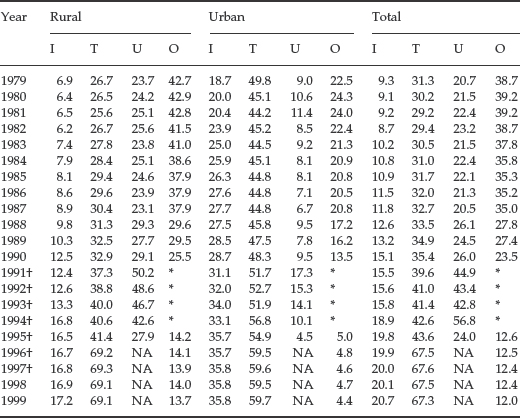
Medical attention at birth, also an important factor for child and maternal health, continues to be overwhelmingly of the traditional type, even though, over the years, the proportion of pregnant mothers accessing professional care has grown. We also see that the rural areas are far less served by professional care (Table 5.2). If we take a look at the picture for professional care at the time of death, the picture is broadly similar (Table 5.3).
Table 5.2
Pregnant mothers (in per cent) by type of medical attention at birth, India, 1979–2003
Source: Till 1998: Selected Socio-Economic Statistics, India, 2002. Central Statistical Organization, Ministry of Statistics and Programme Implementation, Government of India. Table 4.9: Type of medical attention at birth in India. 1999–2003: Women and Men in India, Tenth Issue. 2006. Government of India, Ministry of Statistics and Programme Implementation. Central Statistical Organization, Social Statistics Division. Table 18: Percentage distribution of live births by type of medical attention at the time of delivery by sector.
Note: Data from 1991 to 1997 exclude Jammu and Kashmir.
I Institutions like hospitals, maternity/nursing homes, health centres etc.
T Delivery conducted in the home by doctor, trained dai, trained midwife, trained nurse etc.
U Delivery conducted in the home by untrained village dai or other untrained professional functionary.
O Delivery conducted in the home by relation and others excluding the above.
* Included in category U.
† Excludes Jammu and Kashmir.
Table 5.3
Distribution of deaths (in per cent) during pregnancy by type of medical attention at death, India, 1979–1999
Source: Office of the Registrar General India, Sample Registration System Quoted in Selected Socio-Economic Statistics, India, 2002. Central Statistical Organization, Ministry of Statistics and Programme Implementation, Government of India.
I Death occurred in a hospital, dispensary, health centre, other medical institutions, etc.
T Death occurred at home but was attended by a qualified practitioner.
U Death occurred at home and was attended by an unqualified practitioner.
O No professional doctor/hakim/vaidya attended (others).
* Included in category U
† Excludes Jammu and Kashmir
For 1996, 1997, 1998 and 1999, the classification is as follows:
I Death occurred in a hospital, dispensary, health centre, other medical institutions, etc.
T Death occurred at home but was attended by a qualified practitioner.
U Death occurred at home and was attended by an unqualified practitioner.
O No medical attention
NA Not available.