Chapter 14
Environmental Health in Built Environments
14.1 Environmental Hazards and Built Environments
Environmental health in built environments is central to public health. The existence of a wide range of contaminants of both indoor and outdoor origin, the great source strength per area and the high proportion of time spent in various indoor environments mean that exposure can have a significant impact on human well-being. The amount of time spent in different built environments (residential, occupational, transport and recreational) varies across the globe. However, people around the world typically spend a higher proportion of their time inside than outside.
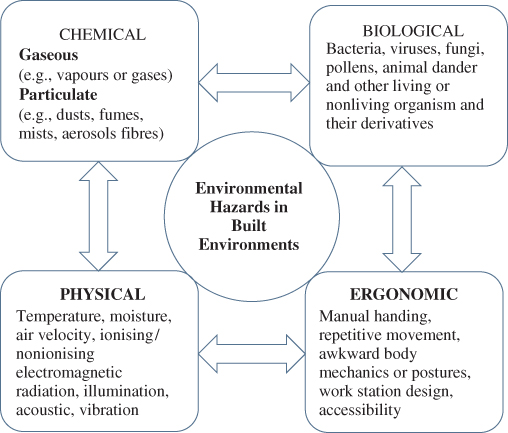
Broadly, ‘built environment’ refers to ‘human-made space in which people live, work, and recreate on a day-to-day basis’ (Roof and Oleru, 2008). It is a material, spatial and cultural product of human labour that combines physical elements and energy in forms necessary to life, work and play (Doleman and Brooks, 2011). In the twenty-first century, humans are exposed to a range of physical, chemical, biological and ergonomic hazards in various built environments. Worldwide, there is considerable variation in the degree of exposure to these hazards, due to noticeable differences in their types and strengths; they are closely linked to socioeconomic developments. Environmental, social, economic, political, technological and climatic changes are constantly altering principles and practices in the design, construction, operation and management of built environments, leading to shifts in exposure patterns and having the potential to create new exposure pathways. Figure 14.1 depicts some environmental hazards that can influence human well-being.
Figure 14.1 Environmental hazards influencing the well-being of the occupants of various built environments.
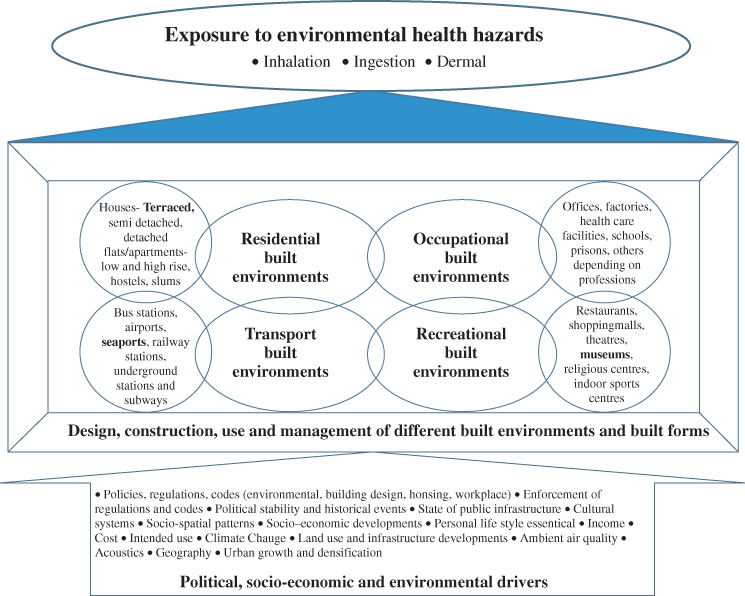
There is good body of knowledge on the routes of exposure to these hazards (inhalation, dermal contact and/or absorption, ingestion), their levels in different built environments and their possible association with ill-health effects. However, what is less understood is the role of diverse human, social, economic, political and environmental factors in the design, construction, use and management of different built environments and how complexity and connectivity among these might influence exposure pathways to these hazards. The degree of risk to public health in different built environments depends on the nature and strength of the harmful effects of a hazard, the social and physical vulnerability of the population, the susceptibility of the persons exposed and the concentration and duration of exposure. Hence, numerous factors can greatly influence the magnitude and duration of exposure.
Most of the current exposure models use either outdoor concentrations of contaminants or individual contaminants in different built environments to predict human exposure. However, in order to estimate the total risk of exposure, there is a dire need to calculate the cumulative exposure to all of the environmental hazards across built environments. This approach will assist greatly in gaining a holistic understanding of environmental health issues in different built environments and in designing the mitigation and prevention strategies that will help reduce the total population exposure to environmental hazards.
These hazards have a variety of sources, including ambient air pollutants, building materials, furniture and furnishing (especially wet or damp furnishing), occupants and their personal care, household cleaning, maintenance and leisure activities, combustion sources (oil, gas, kerosene, coal and wood appliances, tobacco products), photocopying/printing, underground transport, pesticides, organic chemicals, building technologies (air-handling systems, water distribution systems), indoor plants/animals, outdoor plants/animals, insect infestation, agricultural and livestock production, waste management, manufacturing and packing, electrical equipment, poor ergonomics and accessibility. A range of design, construction, operation and management factors can greatly influence the risk of exposure to environmental hazards in built environments. It is notable that while the design and construction of the built environment are intrinsic, its use and management are largely dependent on the inhabitants' behaviour, which can be influenced by a wide range of factors. Figure 14.2 reflects various factors influencing the design, construction, use and management of the built environment that might implicate exposure to different environmental hazards.
Figure 14.2 Factors influencing the design, construction, use and management of various built environments.

It is also worthwhile to mention that built environments undergo change both spatially and temporally and that the design, construction, use and management of built environments and of different built forms in a geographical region are the result of complex political, socioeconomic and environmental factors. These factors constantly alter the parameters influencing built environments, leading to a wide variation in the magnitude of exposure to environmental hazards across the globe. This is evidenced by the substantial differences in the environmental burden of disease among low-, middle- and high-income countries.
14.2 Particulate Contaminants
Particulate matter (small solid and liquid particles of various sizes, shapes and chemical properties suspended in the air) is a major air pollutant. It can be of both anthropogenic and natural origin and is classified according to its size, generation processes and ability to enter the human respiratory system (Morawska and Salthammer, 2003). In brief, particles can be categorized according to their size based on: (i) their observed modal distribution, (ii) the 50% cut-off diameter or (iii) dosimetric variables related to human exposure. In category (i), several subcategories can be observed:
Classification according to the site of deposition in the lungs includes:
Particles in the air are a complex mixture generated by a wide range of sources and exhibit a significant variation in their shape and size distribution (see Chapter 2). In addition, once airborne, they are subject to multiple processes, interactions and reactions, leading to changes in their chemical composition and size. This is due to a variety of physical and chemical processes, such as nucleation (new particle formation), condensation, evaporation, coagulation, deposition (both wet and dry), activation due to water and other gaseous species and aqueous-phase reactions (Finlayson-Pitts and Pitts, 2000; Seinfeld and Pandis, 2006). Fine particles are generated mainly by combustion processes, gas-to-particle conversion and photochemical processes, while coarse particles result from mechanical processes. Different terminology has been used to refer to their sizes, generation processes and composition characteristics (see Chapter 1).
The fate of the particles in the air is largely determined by their physical properties, particularly their size. Aerosol particle size spans over several orders of magnitude, ranging from almost macroscopic dimensions down to near molecular sizes (Hinds, 2005; Seinfeld and Pandis, 2006). Particle size distribution is a crucial parameter that determines the dynamics of aerosols in the atmosphere and their transport, deposition and residence time (Colbeck and Lazaridis, 2010).
With reference to built environments, particles present in enclosed environments can have both indoor and outdoor sources. These include but are not limited to: human occupants (i.e. skin, hair, respiratory aerosols, etc.), plants, pets, household cleaning and maintenance activities, building material and furnishings, combustion appliances, personal-care products and tobacco products (Morawska and Salthammer, 2003). There is a considerable variation in the contribution of different sources to the concentration of indoor particles, and the relative importance of a source depends upon its emission strength and toxicity. Some sources release particles more or less continuously, while others are intermittent. In most cases, the particles generated by different sources or even from the same source can differ in their concentration according to a number of factors. According to Morawska (2004), these factors are:
All these factors vary to a great extent in different built environments and are greatly influenced by elements of design, construction, use and management. There is thus a substantial variation in the concentration of particles and in their subsequent exposure in various indoor environments.
14.2.1 Transport and Behaviour of Particles in Built Environments
Upon emission from a source, particles can undergo a range of physical and chemical process, which can also transform their concentration (see Chapters 2 and 7). These processes include: sedimentation, deposition on surfaces, coagulation and changes by evaporation or condensation. The degree of transformation and the residence time of the particles are largely dependent on the source type. For example, emission from combustion sources can undergo much more rapid changes than can mechanically formed dust (Morawska, 2004). The following are the most important processes affecting indoor particle concentrations after emission: infiltration, penetration of outdoor particles indoors, particle deposition, resuspension of particles, ventilation, phase change, mixing and coagulation. A number of studies have focussed on measuring and modelling indoor particle dynamics. In an extensive review, Chen and Zhao (2011) found a large variation in infiltration (0.3–0.82 for PM2.5 and 0.17–0.52 for PM10) and penetration factors (0.6–1.0 for particles >0.05 and <2 µm) in real buildings. These are size-dependent and are influenced by many other factors (air exchange rate, indoor/outdoor pressure difference, wind direction and speed, the geometry of cracks in building envelopes). Similarly, many studies have quantified deposition and resuspension rates, finding that deposition of particles on indoor surfaces is size-dependent and that many mechanisms can contribute to this process (Lai, 2002; Wallace, Emmerich and Howard-Reed, 2004; He, Morawska and Gilbert, 2005; Chen, Yu and Lai, 2006; Hussein et al., 2006, 2009; Hamdani et al., 2008). Advection and turbulent diffusion are generally strong enough to rapidly transport particles from core air to boundary layers, and thus their deposition on various surfaces. For ultrafine particles, Brownian diffusion is an important deposition mechanism, while gravitational settling amplified by impaction is responsible for coarse-particle deposition. On the other hand, accumulation-mode particles deposit the least effectively (Nazaroff, 2004). Among other factors affecting the deposition are increased air flow, surface area (Thatcher et al., 2002) and surface charges (Lai, 2006).
With reference to resuspension, many household activities and airflows in ventilation ducts can result to particle resuspension. A number of studies have demonstrated that a variety of factors (particle size, surface material and roughness, air velocity, particle composition, air flow characteristics, relative humidity) influence the introduction of particles previously deposited on various indoor surfaces into the air (Wu, Davidson and Russell, 1992; Thatcher and Layton, 1995; Ibrahim, Dunn and Brach, 2003, 2004; Ferro, Kopperud and Hildemann, 2004; Gomes, Freihaut and Bahnfleth, 2007; Qian and Ferro, 2008; Mukai, Siegel and Novoselac, 2009; Shaughnessy and Vu, 2012; Goldasteh, Ahmadi and Ferro, 2012a, 2012b; Boor, Siegel and Novoselac, 2013; Kassab et al., 2013). In addition, apart from affecting the levels of indoor particles, resuspension may provide an exposure pathway for allergens and for semivolatile species.
Ventilation, the process of exchanging indoor air with that outdoors, is an important factor in quantifying the emission strength of indoor sources. The three main modes are mechanical ventilation, natural ventilation and infiltration or leakage flow. He et al. (2005) have shown that ventilation rate is an important factor affecting deposition rates for particles in the size range 0.08–1.0 µm. Ventilation rate varies significantly with the type and location of a building, the climate and the lifestyle of the inhabitants (Morawska, 2004). Mechanical ventilation systems are commonly equipped with fibrous filters to limit the introduction of outdoor air pollutants indoors. The efficiency of a filtration system depends on the filter properties and the aerodynamic size of the particles (Jamriska, Morawska and Ensor, 2003).
Additionally, indoor particles can undergo phase-change processes involving vapours and gases that lead to particle generation and hence affect their number and mass concentration (Morawska, 2004). A number of phase-change processes have been reported in previous studies, such as growth associated with changing humidity conditions (Dua and Hopke, 1996), phase division of semivolatile organic compounds found between the gas phase and sorbed on to indoor airborne particles (Weschler and Shields, 2003), formation of secondary organic particulate matter (Fan et al., 2003; Sarwar et al., 2003) and dissociation of outdoor particles into their gaseous constituents (Lunden et al., 2003). Coagulation does not affect the mass concentration but can change the size distribution of particles, so it can be important when concentrations are high. However, Morawska (2004) has argued that the significance of coagulation in affecting indoor concentration is lower than that of other process.
It is clear from this that many factors play major roles in determining the fate of indoor particles and it is thus difficult to study individual processes. However, it is important to highlight that most of these processes will be greatly affected by various elements of the design, construction, use and management of built environments. In an extensive review of personal exposure to indoor particulate matter and risk assessment, Morawska et al. (2013) suggested that in developed countries, 10–30% of the total burden of disease from particulate-matter exposure was due to that generated indoors.
14.3 Gas Contaminants
The gaseous class encompasses contaminants that exist as atoms or free molecules in air and can be divided into two important subclasses: gases and vapours. Table 14.1 shows the main gaseous contaminants of particular significance in built environments, along with examples and brief descriptions of their occurrence and use.
Table 14.1 Brief overview of the main chemical families of gaseous air contaminants and their occurrence and use (Adapted from ASHRAE, 2009)
| Family | Example | Occurrence and use |
| Inorganic contaminants | ||
| Oxidants | Ozone, nitrogen dioxide | Both members are corrosive and act as respiratory irritants |
| Reducing agents | Carbon monoxide | Carbon monoxide is a toxic fuel-combustion product |
| Acid gases | Carbon dioxide, hydrogen chloride, hydrogen fluoride, hydrogen sulfide, nitric acid, sulfur dioxide, sulfuric acid | Carbon dioxide and hydrogen sulfide are only weakly acidic. Hydrogen sulfide is the main agent in sewer gas. Other members are corrosive and respiratory irritants. Some are important outdoor contaminants |
| Nitrogen compounds | Ammonia, hydrazine, nitrous oxide | Ammonia is used in cleaning products. It is a strong irritant. Hydrazine is used as an anticorrosion agent. Nitrous oxide is used as an aesthetic |
| Organic contaminants | ||
| Chlorinated hydrocarbons | Carbon tetrachloride, chloroform, dichloromethane, 1,1,1-trichloroethane, trichloroethylene, tetrachloroethylene, p-dichlorobenzene | Dichlorobenzene is a solid used as an air freshener. The others shown are liquids and are effective nonpolar solvents. Some are used as degreasers or in the dry-cleaning industry |
| Alcohols | Methanol, ethanol, 2-propanol (isopropanol), 3-methyl 1-butanol, ethylene glycol, 2-butoxyethanol, phenol | Alcohols are strongly polar. Some are used as solvents in water-based products. Phenol is used as a disinfectant. 3-Methyl 1-butanol is emitted by some moulds |
| Aldehydes | Formaldehyde, acetaldehyde, acrolein, benzaldehyde | Formaldehyde, acetaldehyde and acrolein have unpleasant odours and are strong irritants |
| Ketones | 2-Propanone (acetone), 2-butanone (MEK), methyl isobutyl ketone (MIBK), 2-hexanone | Ketones are medium-polarity chemicals. Acetone and 2-hexanone are emitted by some moulds |
| Esters | Ethyl acetate, vinyl acetate, butyl acetate | Esters are medium-polarity chemicals. Some have pleasant odours and are added as fragrances to consumer products |
| Aromatic hydrocarbons | Benzene, toluene, p-xylene, styrene, 1,2,4 trimethyl benzene, naphthalene, benz-α-pyrene | Benzene, toluene and xylene are widely used as solvents and in manufacturing, and are ubiquitous in indoor air. Naphthalene is used as a moth repellent |
| Terpenes | a-Pinene, limonene | A variety of terpenes are emitted by wood. The two listed here have pleasant odours and are used as fragrances in cleaners, perfumes and so on |
| Heterocyclics | Ethylene oxide, tetrahydrofuran, 3-methyl furan, 1, 4-dioxane, pyridine, nicotine | Most heterocyclics are of medium polarity. Ethylene oxide is used as a disinfectant. Tetrahydrofuran and pyridine are used as solvents. Nicotine is a component of tobacco smoke |
It is evident that many elements of the construction, use and management of built environments possess the potential to contaminate the air with a range of gaseous contaminants. A great number of studies have been carried out to investigate the levels of these contaminants, particularly volatile organic compounds and inorganic gases (CO, NOX, SO2, O3, NH3), in various built environments across the globe. Volatile organic compounds and carbonyl compounds are currently attracting the greatest attention, especially in high-income countries, due to their emission from building materials, furnishings (carpets, composite-wood furniture), interior decoration (wall coverings, paints, adhesives) and household cleaning products. A recent review by Sarigiannis et al. (2011) concerning organic compounds (benzene, toluene, xylenes, styrene, acetaldehyde, formaldehyde, naphthalene, limonene, α-pinene and ammonia) has reported that there is a great variation in their levels within and among European countries due to differences in their sources and emission strengths.
14.3.1 Biological Hazards
Biological agents are ubiquitous and can originate from almost any natural or artificial surface, and each source can give rise to an entirely unique assemblage of bioaerosols (see Chapter 16). Wind action on soil, agitation of open water, raindrop impaction, animal farming facilities, compositing, harvesting, HVAC (heating, ventilation and air conditioning) systems, industrial processes, food processing units and wastewater/sewage treatment plants are some examples of major outdoor sources. Indoor bioaerosols are mostly of outdoor origin (Burge, 1990; Levetin et al., 1995), but building materials, carpets, pets, plants and HVAC systems can contribute to their levels, particularly in moisture-damage spaces, which can provide the substrate/conditions for microbes to grow and multiply (Lehtonen, Reponen and Nevalainen, 1993; DeKoster and Thorne, 1995; Ren et al., 2001). Microorganisms can get indoors through HVAC systems, doors, windows, cracks in the walls and the potable drinking-water system. They can also be brought in on people's shoes and clothes (Pasanen et al., 1989). Once in the indoor environment, a range of abiotic factors (water, humidity, temperature, nutrients, oxygen and light) determines their growth on indoor surfaces. Indeed, built environments are complex ecosystems in which there is a complicated relationship between humans, microorganisms and physical structures. With the growing use of molecular approaches, a number of studies have been carried out to elucidate the microbiology of built environments (Kelley and Gilbert, 2013; Robertson et al., 2013). It has been found that building attributes (sources of ventilation air, airflow rates, relative humidity and temperature) influence the diversity and composition of indoor bacterial communities (Kembel et al., 2012).
A large body of knowledge is available concerning the levels of bioaerosols in different built environments, but very often the focus is on their allergenic and toxic potential, with less attention being paid to airborne infection. A range of factors can enhance the probability of disease transmission in built environments (see Chapter 11): enhanced exposure of individuals to infectious people in a small, enclosed spaces, inadequate ventilation, recirculation of contaminated air, increased duration of exposure and susceptibility of the exposed person. Over the years, it has been established that poor housing structures and conditions (inadequate ventilation, limited space and overcrowding) enhance the risk of airborne transmission of diseases. For example, tuberculosis (TB) has long been associated with crowded and poorly ventilated environments (CCDA, 2007), as there is an increased possibility of inhaling droplets expelled by infectious individuals (Wanyeki et al., 2006). Additionally, ventilation and air movement in built environments have been strongly associated with airborne transmission of infectious diseases (Li et al., 2007).
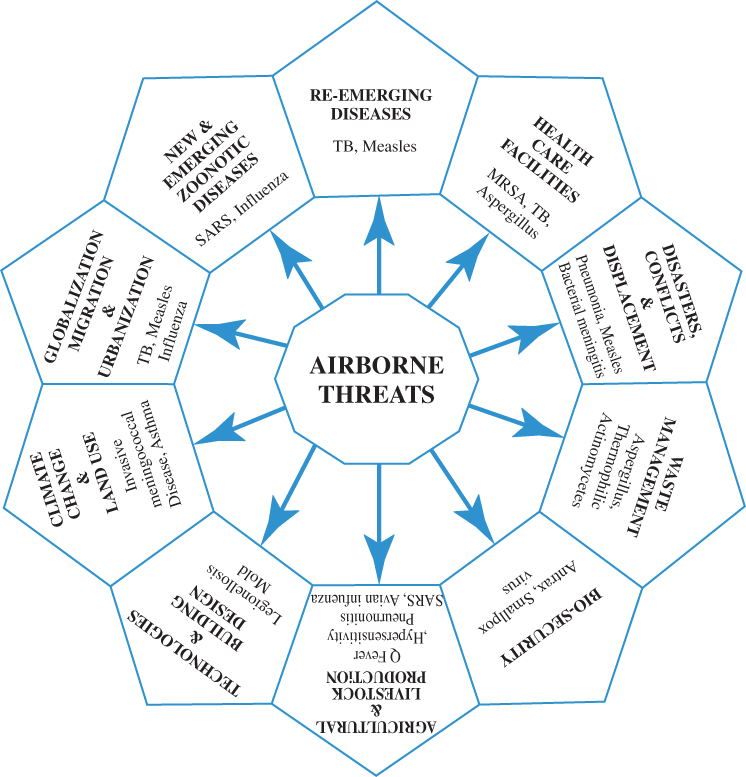
Upon the discovery of antibiotics over half a century ago, far-reaching predictions were made of the end of the infectious disease era. However, over the past 2 decades it has seemed that we are losing the battle against them. Environmental, social, economic, technological and climatic changes are constantly altering disease transmission cycles, which is leading to shifts in the distribution, prevalence and severity of existing and newly emerging infectious diseases. Those spread via airborne transmission have the potential to cause global pandemics; they are a serious threat to twenty-first-century humanity. Figure 14.3 shows airborne biological threats from diverse anthropogenic activities, settings and natural and man-initiated phenomena.
Figure 14.3 Current and future threats from airborne disease transmission.
In health-care facilities, the airborne transmission of measles virus, chickenpox virus (Varicella), rhinoviruses, adenoviruses, Staphylococcus aureus, Mycobacterium tuberculosis and Aspergillus is a global problem (CDC, 2003). Aside from human sources, certain medical procedures (e.g. intubation, bronchoscopy), building maintenance activities (e.g. construction, demolition, renovation and repair) and daily cleaning procedures (e.g. laundry, bedding, clinical waste) enhance the risk of health-care-associated infections (HCAIs). Globally, HCAIs are responsible for significant mortality and financial burden in health-care systems. According to the World Health Organization (WHO), HCAI prevalence in developed and developing countries was 7.6 and 10.1%, respectively, in 2011. In Europe, HCAIs are responsible for 16 million extra days of hospital stay, 37 000 attributable deaths and annual financial losses of up to €7 billion (WHO, 2011).
Similarly, waste-management processes are associated with increased exposure to airborne microorganisms and their toxins. Various mechanical activities associated with these processes generate significant numbers and types of airborne microorganism, which may pose a potential health hazard to workers and those in their vicinity. However, the degree of human exposure to airborne microorganisms may vary with the type and capacity of these facilities, the activities performed there and meteorological conditions (Swan et al., 2003; Stagg et al., 2010; Korzeniewska, 2011; Dehghani et al., 2012).
Natural disasters and conflicts can also provide a paradise for disease transmission, due to massive population displacement, sudden environmental changes, loss of public utilities, disruption of basic health facilities and people's increased vulnerability. Airborne diseases such as pneumonia, measles and bacterial meningitis have an epidemic potential during droughts, tsunami, tornados, earthquakes and flooding. Overcrowding, poor ventilation and inadequate hygiene in closed shelters, lack of nutrition and limited access to medical facilities all enhance the risk of acute respiratory infections (WHO, 2006; Watson, Gayer and Connolly, 2007; Kouadio et al., 2012).
Climate, seasonality and climate change affect the prevalence and geographical distribution of airborne diseases. For example, the epidemic activity of respiratory syncytial virus (RSV) is related to meteorological conditions. In tropical climatic conditions, RSV infection peaks in summer and early autumn, while in temperate climates, RSV infection is highest in the winter (Yusuf et al., 2007). Similarly, the incidence and geographical distribution of invasive meningococcal disease (IMD) is likely to be affected by climate change (Palmgren, 2009). The recent emergence of Cryptococcosis gatti (naturally restricted to tropical and subtropical regions) in the more temperate climates of the Pacific Northwest of the USA has been hypothesised to be linked to climate change (Cooney, 2011). Climate change might also increase the duration of the pollen season and change the spatial distribution of vegetation and regional pollen production (Beggs and Bambrick, 2005; IPCC, 2007), causing people with allergic rhinitis and asthma to be at increased risk of exacerbation. Additionally, more frequent precipitation events, along with urban densification and land use changes, especially in flood plains, have increased the risk and severity of urban flooding, which can have a profound impact on airborne disease transmission. For instance, flooding can trigger extensive growth of biological agents (e.g. mould, bacteria) due to the dampness of surfaces, structures and the air in buildings, leading to enhanced exposure of occupants to aeroallergens, mycotoxins, endotoxins, ß-glucans, volatile organic compounds and infections (WHO, 2009).
Airborne transmission of new and emerging zoonotic disease holds serious epidemic potential. For example, severe acute respiratory syndrome (SARS) and avian flu may become pandemics. The 1918–1919 H1N1 influenza pandemic, which killed an estimated 50–100 million people, clearly shows the severity and consequences of such an event, and the recent spread of H5N1 avian influenza viruses highlights the high risk of pandemic emergence (Morens and Fauci, 2007). Due to the intensification of human-, pathogen- and environment/climate-related factors influencing the emergence of infectious diseases, it is very likely that most of the future infectious disease outbreak caused by either a novel or a recurring agent will be zoonotic (Cascio et al., 2011). Apart from serious harm to human health, a pandemic could result in great social and economic damage.
Along with the new and emerging diseases, airborne transmission of reemerging infectious diseases is also posing an overwhelming threat to humanity. For example, TB is an increasing problem worldwide. In 2009, 1.7 million people around the world died from TB, and there were an estimated 9.4 million new cases (WHO, 2010a). The emerging threat of multidrug-resistant tuberculosis (MDR-TB) and extensively drug-resistant tuberculosis (XDR-TB) is a serious global health concern. In 2008, there were an estimated 390 000–510 000 cases of MDR-TB: 3.6% of all incident TB cases. 5.4% of MDR-TB cases were found to have XDR-TB (WHO, 2010b). Recently cases of totally drug-resistant tuberculosis (TDR-TB) have been reported from Mumbai, India (Loewenberg, 2012).
Globalisation, increased travel, migration and urbanisation may influence the prevalence, geographical distribution and severity of infectious diseases in certain population groups, the reemergence of previously known pathogens and the emergence of new pathogens, due to changes in biological, social and environmental factors associated with these phenomena (WHO, 2004; Ka-Wai Hui, 2006; Alirol et al., 2011). The total number of international migrants has increased from an estimated 178 million in 2000 to 213 million in 2010 (UN DESA, 2009). In 2010, for the first time, more than 50% of the world's population was living in urban areas (United Nations, 2010). Urbanisation is increasingly affecting the epidemiological characteristics of infectious diseases and is having a profound effect on global health. In low-income countries, urbanisation can lead to the development of slums and shanty towns, with poor housing conditions that facilitate the proliferation of airborne diseases. High population density and an increased amount of shared space, heterogeneity in health status and increased mobility in urban areas all enhance exposure to influenza, measles and TB. In fact, densely populated cities have become hubs for the global spread of airborne diseases such as SARS and H1N1 influenza (Alirol et al., 2011).
The continuous shift from traditional agriculture and livestock production to intensive industrial production systems in both developing and developed countries poses a significant threat to global public health, with the risk of not only the increased prevalence of already known infectious diseases but also the emergence of new pathogens. Bacterial concentrations with multidrug resistance have been recovered up to 150 m downwind of a swine-farming installation (Gibbs et al., 2006). Similarly, the emergence of livestock-associated Methicillin-resistant S. aureus ST398 (LA-MRSA) and its transmission to humans clearly shows potential for the emergence of novel pathogens (Smith and Pearson, 2011). In agricultural work environments, bioaerosols and their secondary metabolites can be a cause of allergic rhinitis, toxic pneumonitis, hypersensitivity pneumonitis and asthma (Dutkiewicz et al., 2011).
Technologies such as air-handling systems, cooling towers and architectural fountains have the potential to harbour infectious pathogens (e.g., Legionella) and aid in their airborne transmission. The increased use of mechanical air-conditioning and wet-cooling systems may lead to an increase in cases of Legionnaires' disease. Building design can also enhance the exposure of occupants to airborne pathogens. Energy-efficient and environmentally sustainable buildings (green buildings) have been of great interest in recent years. However, certain of their components may provide ecological niches for the growth of microorganisms and for pathways of dispersal in enclosed spaces. For example, the use of green roofs and green atriums may proliferate human pathogens associated with soil (Morey, 2010). In addition, the ‘build-tight’ approach (reduced dilution of indoor air) may increase the likelihood of airborne infection. Current technologies and building design are more focussed on energy conservation than public health protection.
Moreover, biological agents might be secretly prepared, transported and intentionally released by terrorists and rogue states. The airborne transmission of these weaponised pathogens poses a significant risk to the world population. For example, the deliberate dissemination of Anthrax through postal services in the USA in 2001 clearly shows the threat (Lane, La Montagne and Fauci, 2001). In addition, accidental release of biological agents from lab facilities is also of great concern and could cause a significant threat to the public. The current research on avian influenza viruses (H5N1) and the recent report of recombinant virus (ferret-transmissible H5 HA) has generated wide concern regarding the development and maintenance of these modified strains (Fouchier, García-Sastre and Kawaoka, 2012; Muller, 2012). We are therefore facing a wide range of airborne threats, which necessitates a new focus on control of airborne biological agents.
A range of design, construction, use and management factors (presented in Figure 14.2) may implicate airborne disease transmission. The SARS outbreak in a housing estate (Amoy Gardens) in Hong Kong in 2003 demonstrated how elements of housing and the environment can contribute to the airborne transmission of infectious diseases (Yu et al., 2004). Similarly, outbreaks of Legionnaires' disease highlight the potential for built environments to act as reservoirs of infectious pathogens and aid in their transmission. There is thus a dire need to rethink the role of built environments in airborne disease transmission. Greater attention must be given to the implications of existing practices in the design, construction, use and management of built environments for airborne disease transmission.
14.3.2 Physical Hazards
Physical hazards in built environments involve thermal conditions (temperature, humidity, air velocity, radiant energy), electromagnetic radiation and visual and acoustic conditions. Physical factors can not only impact directly on occupants but also influence other environmental quality factors. British Standard BS EN ISO 7730 defines thermal comfort as ‘that condition of mind which expresses satisfaction with the thermal environment’. It is a person's psychological state of mind and a range of environmental and personal factors that influence the occupant's satisfaction with thermal conditions in different built environments. According to the British Health and Safety Executive (HSE), air temperature, radiant temperature, air velocity, humidity, clothing insulation and metabolic rates all contribute to a worker's thermal comfort. The predicted mean vote (PMV) and percentage people dissatisfied (PPD) index for general thermal comfort and the draught rate (DR) for local thermal discomfort have been widely used to measure thermal comfort. Details of the methods used to predict general thermal sensation and thermal dissatisfaction and the criteria requirements can be found in BS EN ISO 7730, BS EN ISO 10551 (subjective method) and ANSI/ASHRAE Standard 55-2010. Recently, Dear et al. (2013) reviewed thermal comfort research over the last 20 years and discussed the major trends, progress and paradigm shifts in this domain.
Design criteria for environmental factors affecting the thermal comfort of people in built environments are available (e.g. CIBSE Guide A – Environmental Design), but selection of suitable design conditions is still very difficult due to the subjective nature of comfort perception. The main goal is to keep most people thermally comfortable most of the time. According to the HSE, a reasonable limit for the minimum number of people who should be thermally comfortable in a given environment is 80% of occupants.
Over the last century, considerable changes have been made in the electromagnetic fields within built environments. An escalating increase in the amount of electrical equipment and the extent of wireless infrastructure has raised concerns over electromagnetic pollution. The health effects of electromagnetic fields and emission standards have been discussed in detail by Clements-Croome (2012). Electromagnetic compatibility is now a key design consideration (Lock, 2012) and recently a number of papers have looked at the implications of changing the electromagnetic nature of built environments for human well-being (Jamieson et al., 2010, 2011; Xing, 2012). Light can have biological, behavioural and psychological effects on people (e.g. circadian rhythm, body temperature, mood/behaviour, activity levels). There is a good body of literature available on the effects of light on human well-being and there is a growing trend to maximise the use of daylight in buildings (CIE, 2004; Webb, 2006; Boyce, 2010; Todorovic and Kim, 2012; Veitch and Galasiu, 2012). Sound and vibration can also affect well-being: excessive noise can cause annoyance, interference with the intelligibility of speech and even hearing damage; similarly, vibration can have both physical and biological effects, depending on its magnitude and frequency. Codes of practice and guidelines for noise and vibration control in different built environments have been proposed by various organisations (e.g. British standards, ASHRAE).
14.3.3 Ergonomic Hazards
According to the International Ergonomic Association, ergonomics (or ‘human factors’) is ‘the scientific discipline concerned with the understanding of the interactions among humans and other elements of a system, and the profession that applies theoretical principles, data and methods to design in order to optimize human well being and overall system performance’. Ergonomic design of the various elements in built environments (e.g. work station layout) assists people in interacting with the environment comfortably and efficiently, leading to increased productivity and a healthy working experience. Good ergonomics allows the environment to fit the physical activities of the occupants, rather than forcing the occupants to fit their activities to their environment. On the other hand, poor ergonomic design can result not only in low productivity but also in many visual and musculoskeletal disorders/cumulative trauma disorders/repetitive strain injuries. In addition, poor space ergonomics may result in alterations being made during building occupancy, which could have a significant impact on indoor environmental health. For example, the location and number of work stations, cabinets, printers and other equipment can disturb air flows, hygrothermal regulation and ventilation. During refurbishment or alteration, the need for effective ventilation may be overlooked. Often these alterations are focussed on efficiency of space usage or aesthetics and they are likely to be made without changes to the original ventilation design. Environmental health issues often arise due to poor space layout and high occupant densities, especially in work-related built environments. It is very likely that a space with low occupant density based on floor space will have high ‘net occupant density’ due to the concentration of work stations in a small space. Studies have shown an improvement in productivity and comfort and a decrease in musculoskeletal complaints following from good ergonomics design characteristics (Dainoff, Fraser and Taylor, 1982; Smith and Bayeh, 2003; Hemphälä and Eklund, 2012).
Exposure to environmental health hazards in built environments is a complex process. The proximal environmental determinants for enhanced exposure may include inadequate ventilation, ineffective air mixing, poor ergonomics and inadequate facility management. The distal determinants are much more complex and are often overlooked. Built environments undergo change both spatially and temporally, and their design and management in a geographical region are the result of complex political, socioeconomic and environmental factors (Figure 14.4). Political factors include policies and regulation concerning design and construction, as well as their enforcement. Socioeconomic factors include personal lifestyle essentials and cultural systems. Environmental factors include land use, urban growth and densification. The design and implementation of effective interventions/strategies to reduce the risk of exposure to different environmental hazards in built environments can thus only be achieved by following a holistic system approach that takes into account the ways in which political, social, economic and natural drivers affect the design, construction, use and management of different built environments.
Figure 14.4 Exposure to environmental health hazards in various built environments.
14.3.4 Ventilation and Environmental Hazards
Ventilation is one of the most crucial factors in reducing the risk of exposure to a range of air contaminants in built environments. Ventilation design over the past century has seen a shift in its role from infection control to mere thermal comfort. During the nineteenth and early twentieth centuries, when TB and other infectious diseases were common, high ventilation rates were recommended to minimise the risk of infection. With the decline of epidemic diseases, due to improvements in sanitation, hygiene and public health, the rationale for ventilation began to shift from contagion control to the creation of comfortable conditions and odour removal (Maston and Sherman, 2004). The energy crisis in the late 1970s led to further reductions in ventilation rates through the sealing of buildings, in order to reduce infiltration and increase energy efficiency. However, later in that decade the prevalence of sick building syndrome was attributed to inadequate ventilation resulting from this (Mendell and Fine, 1994). Modern buildings are designed to be energy efficient rather than to enhance environmental health and prevent illness, but over the past few decades increases in infectious diseases and respiratory illnesses have highlighted the importance of ventilation. Hobday (2010) has stated that the concept that housing should support and promote the health and well-being of its occupants has been surpassed by energy efficiency concerns and that over the years, interaction between housing and medical officials has declined. In a review of the role of ventilation in the airborne transmission of infectious agents, Li et al. (2007) concluded that ventilation and air movement are strongly associated with the spread of disease in built environments. In addition, they asserted that most epidemiological studies have used inadequate methods to study ventilation and air flow movement, reflecting the lack of interaction among epidemiologists, microbiologists and building engineers. Data on ventilation rates are limited, but the available information highlights that the use and management of a ventilation system greatly impact on its overall performance. An increased focus on energy conservation has led to the introduction of energy-efficient designs and the building of highly insulated, airtight structures with greater use of mechanical-ventilation-with-heat-recovery (MVHR) systems. A recent review of ventilation in European dwellings has concluded that despite the growing recognition of ventilation as an important component of healthy dwelling, in practice ventilation is poor and a large proportion of dwellings are underventilated (lower than 0.5 h−1) (Dimitroulopoulou, 2011). Furthermore, in various built environments, especially occupational, transport and other recreational built environments, the operation, maintenance and management of facilities (e.g. HVAC systems, water supply systems) by management can have a considerable impact on the overall environmental health. Moreover, the degree of interaction between facilities management and the organisations using the built environment, and their knowledge of cumulative exposure to various environmental hazards, has a vital role to play in ensuring appropriate environmental health. The lack of knowledge and awareness of various environmental hazards among the occupants of built environments, the personnel responsible for health and safety at work and facilities management can lead to enhanced exposure to various environmental hazards. For instance, incorrect operation and poor maintenance of ventilation and air-conditioning systems during a building's occupancy can lead to inadequate ventilation rates and poor air distribution, which in turn enhances the risk of exposure to a range of air contaminants. Furthermore, it is worth highlighting that very often the need for ventilation is governed by the psychological and physiological needs of the occupants and that spaces with hybrid ventilation design (mechanical and natural ventilation) can lead to uncontrolled ventilation and air mixing depending on the locations of the opened windows and doors and how long they remain open. Natural ventilation can provide higher air exchange rates at a lower cost and for lower maintenance than can mechanical ventilation. However, it is important to take into account the quality of the outdoor air. A large number of studies have shown an association between ambient air pollution and morbidity. What is required is not only a healthy design for new buildings but also the healthy use of existing built environments, in order to lessen the exposure to different environmental hazards.
14.3.5 Energy-Efficient Built Environments, Climate Change and Environmental Health
Due to their cumulative impact on natural resource depletion and degradation, waste generation and accumulation, ecosystems and climate change, governments around the world are putting forward new polices, laws and standards to reduce the environmental impacts of built environments. Consequently, depending on the implementation of these laws, stakeholders face new, complex and rapidly changing challenges, leading to significant changes in the design and construction of built environments. In order to reduce carbon dioxide emissions, energy efficiency has emerged as the guiding paradigm for the creation of a new kind of built environment. However, an increased focus on energy efficiency had raised the concern that various factors involved in the design, construction and operation of energy-efficient built environments might increase the vulnerability of their occupants to environmental hazards, especially airborne pollutants. In recent years, governments across the developed world have focussed their attentions on housing, due to its considerable share in energy use (e.g., codes for sustainable homes include ‘PassivHaus’, ‘Smart Energy Home’, ‘R-2000 homes’, ‘indoor airPLUS’). The UK government intends that all new homes in England will be zero-carbon by 2016. This approach/policy entails greater airtightness of the building envelope in order to improve energy efficiency, and concerns have been raised by builder and owners over issues surrounding poor indoor air quality (Davis and Harvey, 2008). Homes built to level 4 of the code for sustainable homes are expected to use MVHR in order to comply with energy-use and indoor-air-quality requirements. Crump et al. (2009) carried out an extensive review of indoor air quality in highly energy-efficient homes, of ventilation performance in dwellings construction and of ventilation provision in highly energy-efficient homes and concluded that there is a dearth of knowledge in this area and that more research is needed.
In recent years, the long-term challenges of climate change and its potential effects on indoor air quality and public health have been addressed in numerous publications. A report by the Institute of Medicine (IOM) concluded that the extensive body of literature highlights that poor indoor environmental quality is creating health problems but that there is inadequate evidence to associate climate-change-induced alterations in the indoor environment with any specific adverse health outcomes. However, climate change has the potential to worsen existing indoor environmental problems and to introduce new ones (IOM, 2011). Based on the IOM report, Spengler (2012) and Nazaroff (2013) have summarised and discussed the consequences of climate change for indoor air quality. A report by Crump (2011) on the health impacts arising from changes in the indoor environment in the UK also considered changes caused by the mitigation and adoption of actions as a result of climate change. Furthermore, a recent report by the UK Health Protection Agency on the health effects of climate change (HPA, 2012) concluded that climate change has the potential to modify risks in the indoor built environments by exacerbating the existing health risks associated with indoor air pollutants.
Florence Nightingale (1820–1910) recognised that ‘the connection between health and the dwellings of the population is one of the most important that exists’. This statement is still true today. It is evident that aerosol science is central to improving environmental health in the built environment. It draws on numerous branches of science, including ventilation engineering, aerobiology, chemistry, nanotechnology, occupational exposure and more.
References
Alirol, E., Getaz, L., Stoll, B. et al. (2011) Urbanisation and infectious diseases in a globalised world. The Lancet Infectious Diseases, 11, 131–141.
ASHRAE (2009) Air contaminants, in ASHRAE Handbook—Fundamentals (I-P Edition), American Society of Heating, Refrigerating and Air-Conditioning Engineers, Inc., pp. 11-1–11-22.
Beggs, P.J. and Bambrick, H.J. (2005) Is the global rise of asthma an early impact of anthropogenic climate change? Environmental Health Perspectives, 113(8), 915–919.
Boor, B.E., Siegel, J.A. and Novoselac, A. (2013) Wind tunnel study on aerodynamic particle resuspension from monolayer and multilayer deposits on linoleum flooring and galvanized sheet metal. Aerosol Science and Technology. doi: 10.1080/02786826.2013.794929.
Boyce, P.R. (2010) Review: the impact of light in buildings on human health. Indoor and Built environment, 19, 8–20.
Burge, H. (1990) Bioaerosols: prevalence and health effects in the indoor environment. Journal of Allergy and Clinical Immunology, 86, 687–701.
Cascio, A., Bosilkovski, M., Rodriguez-Morales, A.J. and Pappas, G. (2011) The socio-ecology of zoonotic infections. Clinical Microbiology and Infection 17, 336–342.
CCDA (2007) Housing Conditions that Serve as Risk Factors for Tuberculosis Infection and Disease. Canada Communicable Disease Report, 33(ACS 9).
CDC (Centers for Disease Control and Prevention) (2003) Guidelines for Environmental Infection Control in Health-care Facilities: Recommendations of CDC and the Healthcare Infection Control Practices Advisory Committee (HICPAC), U.S. Department of Health and Human Services, Centers for Disease Control and Prevention (CDC), Atlanta, GA.
Chen, F., Yu, S.C.M. and Lai, A.C.K. (2006) Modeling particle distribution and deposition in indoor environments with a new drift-flux model. Atmospheric Environment, 40, 357–367.
Chen, C. and Zhao, B. (2011) Review of relationship between indoor and outdoor particles: I/O ratio, infiltration factor and penetration factor. Atmospheric Environment, 45(2), 275–288.
CIE (2004) Ocular Lighting Effects on Human Physiology and Behaviour, Commission Internationale de l'Eclairage Publication, p. 158.
Clements-Croome, D. (ed) (2012) Electromagnetic Environments and Health in Building, Routledge.
Colbeck, I. and Lazaridis, M. (2010) Aerosols and environmental pollution. Naturwissenschaften, 97, 117–131.
Cooney, C.M. (2011) Climate change and infectious disease: is the future here? Environmental Health Perspectives, 119, a394.
Crump, D. (2011) Climate Change—Health Impacts Due to Changes in the Indoor Environment; Research Needs, Institute of Environment and Health, Cranfield University.
Crump, D., Dengel, A. and Swainson, M. (2009) Indoor Air Quality in Highly Energy Efficient Homes: A Review, NHBC Foundation Report NF18, National House Building Council, Milton Keynes.
Dainoff, M.J., Fraser, L. and Taylor, B.J. (1982) Visual, musculoskeletal, and performance differences between good and poor VDT workstations. Proceedings of the Human Factors and Ergonomics Society Annual Meeting, 26(2), 144. Sage Publications.
Davis, I. and Harvey, V. (2008) Zero Carbon: What does it Mean to Homeowners and Housebuilders? NHBC Foundation Report NF9, April 2008.
Dear, R., Akimoto, T., Arens, E. et al. (2013) Progress in thermal comfort research over the last twenty years. Indoor Air. doi: 10.1111/ina.12046.
Dehghani, R., Asadi, M.A., Charkhloo, E. et al. (2012) Identification of fungal communities in producing compost by windrow method. Journal of Environmental Protection, 3, 61–67.
DeKoster, J.A. and Thorne, P.S. (1995) Bioaerosol concentrations in noncompliant, complaint and intervention homes in the Midwest. American Industrial Hygiene Association Journal, 56, 576–580.
Dimitroulopoulou, C. (2011) Ventilation in European dwellings: a review. Building and Environment, 47, 109–125.
Doleman, R. and Brooks, D.J. (2011) A strategy to articulate the facility management knowledge categories within the built environment, in Proceedings of the 4th Australian Security and Intelligence Conference (eds D.J. Brooks and C. Valli), Secau –Security Research Centre, School of Computer and Security Science, Edith Cowan University, Perth, Western Australia, pp. 58–67.
Dua, S.K. and Hopke, P.K. (1996) Hygroscopic growth of assorted indoor aerosols. Aerosol Science and Technology, 24, 151–160.
Dutkiewicz, J., Cisak, E., Sroka, J. et al. (2011) Biological agents as occupational hazards-selected issues. Annals of Agricultural and Environmental Medicine: AAEM, 18, 286.
Fan, Z.H., Lioy, P., Weschler, C. et al. (2003) Ozone-initiated reactions with mixtures of volatile organic compounds under simulated indoor conditions. Environmental Science and Technology, 37, 1811–1821.
Ferro, A.R., Kopperud, R.J. and Hildemann, L.M. (2004) Source strengths for indoor human activities that resuspend particulate matter. Environmental Science and Technology, 38, 1759–1764.
Finlayson-Pitts, B.J. and Pitts, J.N. (2000) Chemistry of the Upper and Lower Atmosphere, Academic Press.
Fouchier, R.A.M., García-Sastre, A. and Kawaoka, Y. (2012) Pause on avian flu transmission studies. Nature. doi: 10.1038/481443a.
Gibbs, S.G., Green, C.F., Tarwater, P.M. et al. (2006) Isolation of antibiotic-resistant bacteria from the air plume downwind of a swine confined or concentrated animal feeding operation. Environmental Health Perspectives, 114, 1032.
Goldasteh, I., Ahmadi, G. and Ferro, A. (2012a) A model for removal of compact, rough, irregularly shaped particles from surfaces in turbulent flows. The Journal of Adhesion, 88, 766–786.
Goldasteh, I., Ahmadi, G. and Ferro, A.R. (2012b) Wind tunnel study and numerical simulation of dust particle resuspension from indoor surfaces in turbulent flows. Journal of Adhesion Science and Technology. doi: 10.1080/01694243.2012.747729.
Gomes, C., Freihaut, J. and Bahnfleth, W. (2007) Resuspension of allergen containing particles under mechanical and aerodynamic disturbances from human walking. Atmospheric Environment, 41, 5257–5270.
Hamdani, S.E., Limam, K., Abadie, M.O. and Bendou, A. (2008) Deposition of fine particles on building internal surfaces. Atmospheric Environment, 42, 8893–8901.
He, C., Morawska, L. and Gilbert, D. (2005) Particle deposition rates in residential houses. Atmospheric Environment, 39, 3891–3899.
Health Protection Agency (2012) Health Effects of Climate Change in the UK 2012: Current Evidence, Recommendations and Research Gaps, UK Health Protection Agency, London.
Hemphälä, H. and Eklund, J. (2012) A visual ergonomics intervention in mail sorting facilities: effects on eyes, muscles and productivity. Applied Ergonomics, 43, 217–229.
Hinds, W.C. (2005) Aerosol properties, in Aerosols Handbook, Measurement, Dosimetry and Health Effects (eds Ruzer L.S. and Harley N.H.), CRC Press, Boca Raton, FL, pp. 19–33.
Hobday, R. (2010) Designing Houses for Health—A Review, Commissioned by the VELUX Company Ltd.
Hussein, T., Glytsos, T., Ondracek, J. et al. (2006) Particle size characterization and emission rates during indoor activities in a house. Atmospheric Environment, 40, 4285–4307.
Hussein, T., Hruska, A., Dohanyosova, P. et al. (2009) Deposition rate on smooth surfaces and coagulation of aerosol particles inside a test chamber. Atmospheric Environment, 43, 905–914.
Ibrahim, A.H., Dunn, P.F. and Brach, R.M. (2003) Microparticle detachment from surfaces exposed to turbulent air flow: controlled experiments and modeling. Journal of Aerosol Science, 34, 765–782.
Ibrahim, A.H., Dunn, P.F. and Brach, R.M. (2004) Experiments and validation of a model for microparticle detachment from a surface by turbulent air flow. Journal of Aerosol Science, 35, 805–821.
IOM (2011) Climate Change, The Indoor Environment, and Health, The National Academies Press, Washington, DC.
IPCC (Intergovernmental Panel on Climate Change) (2007) Climate Change 2007: Impacts, Adaptation and Vulnerability, IPCC, Geneva.
Jamieson, I.A., Holdstock, P., ApSimon, H.M. and Bell, J.N.B. (2010) Building health: the need for electromagnetic hygiene? IOP Conference Series: Earth and Environmental Science, 10(1), 012007.
Jamieson, I.A., Jamieson, S.S., ApSimon, H.M. and Bell, J.N.B. (2011) Grounding and human health—a review. Journal of Physics: Conference Series, 301(1), 012024.
Jamriska, M., Morawska, L. and Ensor, D.S. (2003) Control strategies for sub-micrometer particles indoors: model study of air filtration and ventilation. Indoor Air, 13, 96–105.
Kassab, A.S., Ugaz, V.M., King, M.D. and Hassan, Y.A. (2013) High resolution study of micrometer particle detachment on different surfaces. Aerosol Science and Technology, 47, 351–360.
Ka-Wai Hui, E. (2006) Reasons for the increase in emerging and re-emerging viral infectious diseases. Microbes and Infection, 8, 905–916.
Kelley, S.T. and Gilbert, J.A. (2013) Studying the microbiology of the indoor environment. Genome Biology, 14, 1–9.
Kembel, S.W., Jones, E., Kline, J. et al. (2012) Architectural design influences the diversity and structure of the built environment microbiome. The ISME Journal, 6, 1469–1479.
Korzeniewska, E. (2011) Emission of bacteria and fungi in the air from wastewater treatment plants-a review. Frontiers in Bioscience, 3, 393.
Kouadio, I.K., Aljunid, S., Kamigaki, T. et al. (2012) Infectious diseases following natural disasters: prevention and control measures. Expert Review of Anti-infective Therapy, 10, 95–104.
Lai, A.C.K. (2002) Particle deposition indoors: a review. Indoor Air, 12, 211–214.
Lai, A.C.K. (2006) Investigation of electrostatic forces on particle deposition in a test chamber. Indoor and Built Environment, 15, 179–186.
Lane, H.C., La Montagne, J. and Fauci, A.S. (2001) Bioterrorism: a clear and present danger. Nature Medicine, 7, 1271–1273.
Lehtonen, M., Reponen, T. and Nevalainen, A. (1993) Everyday activities and variation of fungal spore concentrations in indoor air. International Biodeterioration and Biodegradation, 31, 25–39.
Levetin, E., Shaugnessy, R., Fisher, E. et al. (1995) Indoor air quality in schools: exposure to fungal allergens. Aerobiologia, 11, 27–34.
Li, Y., Leung, G.M., Tang, J.W. et al. (2007) Role of ventilation in airborne transmission of infectious agents in the built environment—a multidisciplinary systematic review. Indoor Air, 17, 2–18.
Lock, K.S. (2012) EMC design in the built environment, in Electromagnetic Compatibility (APEMC), Asia-Pacific Symposium on 2012, IEEE, pp. 21–24.
Loewenberg, S. (2012) India reports cases of totally drug-resistant tuberculosis. The Lancet, 379(9812), 205.
Lunden, M.M., Revzan, K.L., Fischer, M.L. et al. (2003) The transformation of outdoor ammonium nitrate aerosols in the indoor environment. Atmospheric Environment, 37, 5633–5644.
Maston, N.E. and Sherman, M.H. (2004) Why we ventilate our houses-an historical look, in ACEEE Summer Study on Energy Efficiency in Buildings, Vol. 7, American Council for an Energy Efficient Economy, Washington, DC, Pacific Grove, CA, pp. 241–250.
Mendell, M. and Fine, L. (1994) Building ventilation and symptoms—where do we go from here? American Journal of Public Health, 84, 346.
Morawska, L. (2004) Indoor particles combustion products and fibers, in The Hand Book of Environmental Chemistry. Part—F Indoor Air Pollution, Vol. 4 (ed Pluschke P.), Springer-Verlag, Berlin, Heidelberg, pp. 117–147.
Morawska, L., Afshari, A., Bae, G. et al. (2013) Indoor aerosols: from personal exposure to risk assessment. Indoor Air. doi: 10.1111/ina.12044.
Morawska, L. and Salthammer, T. (2003) Fundamental of indoor particles and and settled dust, in Indoor Environments (eds L. Morawska and T. Salthammer), Wiley-VCH Verlag GmbH & Co. KGaA, Weinheim, pp. 3–46.
Morens, D.M. and Fauci, A.S. (2007) The 1918 influenza pandemic: insights for the 21st century. Journal of Infectious Diseases, 195, 1018.
Morey, P.R. (2010) Climate Change and Potential Effects on Microbial Air Quality in the Built Environment, Preliminary Draft 2010, http://www.epa.gov/iaq/pdfs/climate_and_microbial_iaq.pdf (last accessed 9 August 2013).
Mukai, C., Siegel, J.A. and Novoselac, A. (2009) Impact of airflow characteristics on particle resuspension from indoor surfaces. Aerosol Science and Technology, 43, 1–11.
Müller, V. (2012) A plea for caution: huge risks associated with lab-bred flu. Viruses, 4, 276–279.
Nazaroff, W.W. (2004) Indoor particle dynamics. Indoor Air, 14(Suppl. 7), 175–183.
Nazaroff, W.W. (2013) Exploring the consequences of climate change for indoor air quality. Environmental Research Letters, 8, 015022.
Palmgren, H. (2009) Meningococcal disease and climate. Global Health Action, 2. doi: 10.3402/gha.v2i0.2061.
Pasanen, A.L., Kalliokoski, P., Pasanen, P. et al. (1989) Fungi carried from farmers work into farm homes. American Industrial Hygiene Association Journal, 50, 631–633.
Qian, J. and Ferro, A. (2008) Resuspension of dust particles in a chamber and associated environmental factors. Aerosol Science and Technology, 42, 566–578.
Ren, P., Jankun, T.M., Belanger, K. et al. (2001) The relation between fungal propagules in indoor air and home characteristics. Allergy, 56, 419–424.
Robertson, C.E., Baumgartner, L.K., Harris, J.K. et al. (2013) Culture-independent analysis of aerosol microbiology in a metropolitan subway system. Applied and Environmental Microbiology. doi: 10.1128/AEM.00331-13.
Roof, K. and Oleru, N. (2008) Public health: Seattle and King county's push for the built environment. Journal of Environmental Health, 71, 24–27.
Sarigiannis, D.A., Karakitsios, S.P., Gotti, A. et al. (2011) Exposure to major volatile organic compounds and carbonyls in European indoor environments and associated health risk. Environment International, 37, 743–765.
Sarwar, G., Corsi, R., Allen, D. and Weschler, C. (2003) The significance of secondary organic aerosol formation and growth in buildings: experimental and computational evidence. Atmospheric Environment, 37, 1365–1381.
Seinfeld, J.H. and Pandis, S.N. (2006) Atmospheric Chemistry and Physics, From Air Pollution to Climate Change, 2nd edn, John Wiley & Sons, Inc.
Shaughnessy, R. and Vu, H. (2012) Particle loadings and resuspension related to floor coverings in a chamber and in occupied school environments. Atmospheric Environment, 55, 515–524.
Smith, M.J. and Bayeh, A.D. (2003) Do ergonomics improvements increase computer workers' productivity?: an intervention study in a call centre. Ergonomics, 46, 3–18.
Smith, T.C. and Pearson, N. (2011) The emergence of Staphylococcus aureus ST398. Vector-Borne and Zoonotic Diseases, 11, 327–339.
Spengler, J.D. (2012) Climate change, indoor environments, and health. Indoor Air, 22, 89–95.
Stagg, S., Bowry, A., Kelsey, A. and Crook, B. (2010) Bioaerosol Emissions from Waste Composting and the Potential for Workers' Exposure. Health and Safety Executive Research Report 786, Health and Safety Laboratory Harpur Hill, Buxton, p. SK17 9JN.
Swan, J., Gilbert, E., Kelsey, A. and Crook, B. (2003) Occupational and Environmental Exposure to Bioaerosols from Composts and Potential Health Effects– A Critical Review of Published Data. HSE Report RR130, HSE Books, Sudbury.
Thatcher, T.L., Lai, A.C.K., Moreno-Jackson, R. et al. (2002) Effects of room furnishings and air speed on particle deposition rates indoors. Atmospheric Environment, 36, 1811–1819.
Thatcher, T.L. and Layton, D.W. (1995) Deposition re-suspension and penetration of particles within residence. Atmospheric Environment, 29, 1487–1497.
Todorovic, M.S. and Kim, J.T. (2012) Beyond the science and art of the healthy buildings daylighting dynamic control's performance prediction and validation. Energy and Buildings, 46, 159–166.
UN DESA (2009) United Nations Department of Economic and Social Affairs Trends in International Migrant Stock: The 2008 Revision, http://esa.un.org/migration/index.asp? (last accessed 9 August 2012).
United Nations (2010) Department of Economic and Social Affairs, Population Division. World Urbanization Prospects: The 2009 Revision. CD-ROM Edition—Data in Digital Form (POP/DB/WUP/Rev.2009), United Nations, New York.
Veitch, J.A. and Galasiu, A.D. (2012) The Physiological and Psychological Effects of Windows, Daylight, and View at Home: Review and Research Agenda. NRC-IRC Research Report RR-325, NRC Institute for Research in Construction, doi: http://dx.doi.org/10.4224/20375039.
Wallace, L.A., Emmerich, S.J. and Howard-Reed, C. (2004) Effect of central fans and induct filters on deposition rates of ultrafine and fine particles in an occupied townhouse. Atmospheric Environment, 38, 405–413.
Wanyeki, I., Olson, S., Brassard, P. et al. (2006) Dwellings, crowding, and tuberculosis in Montreal. Social Science & Medicine, 63, 501–511.
Watson, J.T., Gayer, M. and Connolly, M.A. (2007) Epidemics after natural disasters. Emerging Infectious Diseases, 13, 1.
Webb, A.R. (2006) Considerations for lighting in the built environment: non-visual effects of light. Energy and Buildings, 38, 721–727.
Weschler, C.J. and Shields, H.C. (2003) Experiments probing the influence of air exchange rates on secondary organic aerosols derived from indoor chemistry. Atmospheric Environment, 37, 5621–5631.
WHO (2004) Globalization and Infectious Diseases: A Review of the Linkages, Special Topics No. 3, Geneva.
WHO (2006) Communicable Diseases Following Natural Disasters. Risk Assessment and Priority Interventions. Programme on Disease Control in Humanitarian Emergencies Communicable Diseases Cluster, World Health Organization, Geneva.
WHO (2009) WHO Guidelines for Indoor Air Quality: Dampness and Mould, WHO Regional Office for Europe, Copenhagen.
WHO (2010a) Global Tuberculosis Control, WHO report 2010, Geneva.
WHO (2010b) Multidrug and Extensively Drug-Resistant TB (M/XDR-TB): 2010 Global Report on Surveillance and Response, Geneva.
WHO (2011) Report on the Burden of Endemic Health Care-associated Infection Worldwide, World Health Organization, Switzerland.
Wu, Y.L., Davidson, C.I. and Russell, A.G. (1992) Controlled wind tunnel experiments for particle bounceoff and resuspension. Aerosol Science and Technology, 17, 245–262.
Xing, J.Y. (2012) Electromagnetic radiation on human health hazards and protective measures in modern society. Advanced Materials Research, 518, 1022–1026.
Yu, I.T.S., Li, Y., Wong, T.W. et al. (2004) Evidence of airborne transmission of the severe acute respiratory syndrome virus. New England Journal of Medicine, 350(17), 1731–1739.
Yusuf, S., Piedimonte, G., Auais, A. et al. (2007) The relationship of meteorological conditions to the epidemic activity of respiratory syncytial virus. Epidemiology and Infection, 135, 1077–1090.
