13
Brigham and Women’s Physicians Organization
Jessica Dudley, MD, Former Chief Medical Officer, Chief Clinical Officer, Press Ganey, Inc.
Sunil Eappen, MD, Chief Medical Officer
Each individual burns out in different ways.
SUNIL EAPPEN
Happy families are all alike; every unhappy family is unhappy in its own way.
LEO TOLSTOY, ANNA KARENINA
Starting the Journey
Brigham and Women’s Physicians Organization (BWPO) began its journey to reduce or eliminate physician burnout while increasing fulfillment in 2016 through three primary initiatives:
1. In local department initiatives, chairs worked with faculty to engage in wellness efforts.
2. There was an identified need for institution-wide effort.
• A physicians council and frontline physicians identified key priorities.
• A decision was made to formally survey physicians for burnout and fulfillment.
3. A governance and accountability structure was established (Figure 13-1).
• The BWPO Executive Committee created a wellness measure.
• A wellness task force was established with the physician organization and the hospital that included the chief medical officer, the chief nursing officer, and HR representatives from both groups. This partnership was critical in responding to the needs of the frontline physicians.
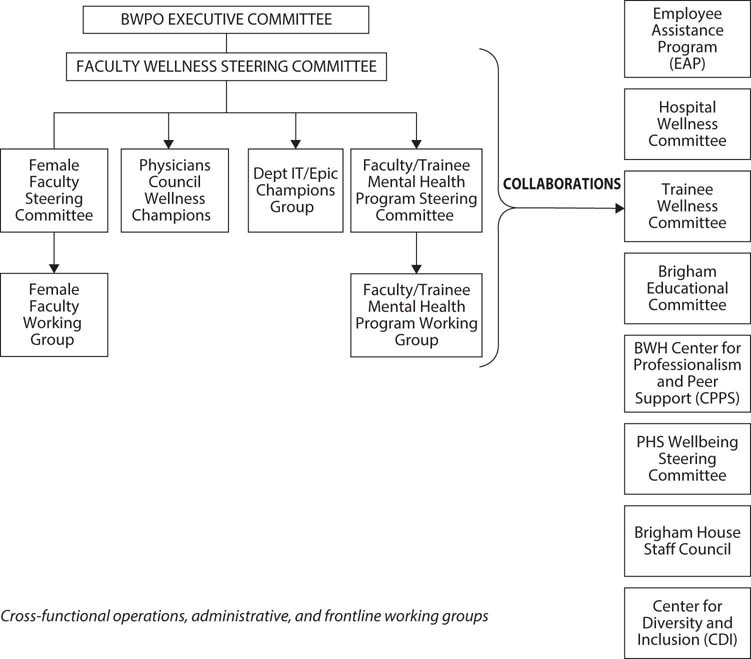
Figure 13-1: Governance Structure of the Brigham and Women’s Physicians Organization Faculty Wellness Steering Committee
BWPO had a rich history of investing in leadership through a physician leadership development program designed and implemented with Harvard Business School, the Brigham Leadership Program. In addition, a culture of fostering innovation through the Frontline Innovation Program and the Brigham Care Redesign Incubator and Startup Program is a part of the organization. This culture of leadership and innovation made the burnout initiative easier, given the background of change, innovation, and leadership tools already present.
Governance Structure
Governance structure is always important in an academic medical center. The Faculty Wellness Steering Committee consisted of 12 physicians and one additional administrative executive, including department chairs, hospital and physicians organization chief medical officers, and leaders from various other departments. The committee reported directly to the BWPO Executive Committee, emphasizing the importance of the initiative. Four groups report to the steering committee:
• Female Faculty Steering Committee
• Physicians Council Wellness Champions
• Department IT/Epic Champions Group
• Faculty/Trainee Mental Health Program Steering Committee
All these efforts worked in coordination and collaboration across the medical center’s boundaries, including with the Employee Assistance Program, the Center for Diversity and Inclusion, the Center for Professionalism and Peer Support, and others. This governance structure was critical to ensuring that all voices were sought in the design and implementation of the program and that efforts were collaborative in nature, thereby reducing resistance to change.
BWPO did not create a position of chief wellness officer or chief human experience officer, instead assigning accountability to the steering committee, which worked with the chief medical officer and the president of BWPO.
Defining and Measuring Burnout and Fulfillment
BWPO employed the classic Maslach definition of burnout as a syndrome of the following:
• emotional exhaustion
• cynicism or depersonalization
• personal accomplishment
Professional fulfillment was defined by Tait Shanafelt as “happiness or meaningfulness, self-worth, self-efficacy and satisfaction in work.”
MODELS, MEASUREMENTS, AND RESOURCES
As the BWPO burnout journey progressed, outreach efforts were made to learn from other leaders and organizations. Tait Shanafelt, then at Mayo Clinic and now at Stanford, met with members of the BWPO physicians’ council to share background and experiences from Mayo, including the importance of engaging in regular measurement, addressing burnout openly, and sharing successes, as well as the critical nature of leadership accountability. Additionally, the physicians’ council reached out to Stanford—which had developed its own model, called the Professional Fulfillment Index (PFI)—regarding use of its survey tool, which addressed both burnout and professional fulfillment. This survey was valuable because it also included questions to help identify drivers of burnout and professional fulfillment that were grouped into the areas of (1) culture of wellness, (2) efficiency of practice, and (3) personal resilience. The decision was made to use the Stanford Wellness framework and the Stanford Wellbeing survey tool. The Stanford survey was selected specifically because it encompassed both burnout and professional fulfillment measures and was designed to identify potential drivers of both. The PFI was included in the Stanford Wellbeing survey. The PFI is a 16-question, five-point Likert scale. The scale measures the following:
• professional fulfillment (6 questions)
• work exhaustion (4 questions)
• interpersonal disengagement (6 questions)
After review and edits from the physicians’ council and Medical Executive Committee, in 2017, the first Brigham Wellbeing Survey (Stanford Wellbeing survey including the PFI, with some adjustments in response to feedback from the Brigham physician community) was conducted and the decision was made to join the National Physician Wellness Academic Consortium with the intent of learning along with others across the country and allowing for national benchmarking.
INITIAL (2017) SURVEY RESULTS
The results of the initial 2017 survey were striking in many ways. First, the response rate to the burnout survey was 64 percent, double the typical response rate from previous surveys. The high response rate was driven by several factors:
• chair and leadership commitment to the importance of physician burnout
• incentive program for leadership driven by metrics of completion
• presentation at faculty meetings
• inclusion of all faculty (including research and clinical)
• physician perception of the importance of this topic
Second, the burnout and fulfillment rates varied widely by department, from a high of 54 percent to a low of 21 percent, with a mean of 37 percent, reiterating that every individual burns out in his or her own way. Third, the survey process itself served a convening function, in that it served notice that burnout was important to the leaders (Figure 13-2).
Conversely, fulfillment ranged from a high of 70 percent to a low of 29 percent, with a mean of 42 percent (Figure 13-3). Interestingly, there was not a clear inverse relationship between burnout and fulfillment; in fact, some physicians with the highest fulfillment had high rates of burnout, potentially indicating that the job stressors for those physicians were excessive. (Resiliency was not measured in the surveys.)
The free text responses from the survey were particularly instructive in designing solutions, in both positives and negatives. The most common negatives raised were the electronic health record (EHR) (Epic), high work volumes, and lack of appreciation, while the top positives were interaction with colleagues, a stimulating research environment, and the passion for caring for patients.
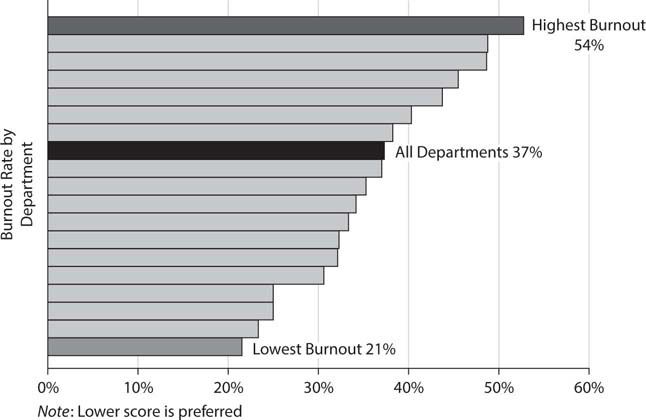
Figure 13-2: Burnout Distribution across All Brigham Health Departments
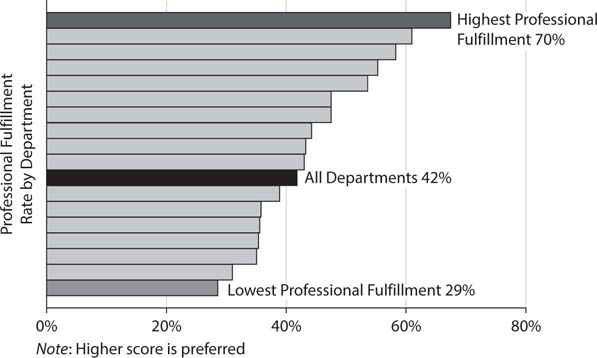
Figure 13-3: Professional Fulfillment Distribution across All Brigham Health Departments
SIGNIFICANT GENDER GAP IN BURNOUT AND FULFILLMENT
Of considerable concern was the finding that female physician faculty had substantially higher burnout rates and lower professional fulfillment scores when compared with their male counterparts (Figure 13-4). Based on the 2017 survey, female physicians had a burnout rate of 44 percent and male physicians had a rate of 34 percent, while professional fulfillment was higher among male physicians, 50 percent compared with 34 percent in females. These findings led to a concerted effort to address these data with the Brigham and Women’s Female Faculty Initiative (see later in this chapter).
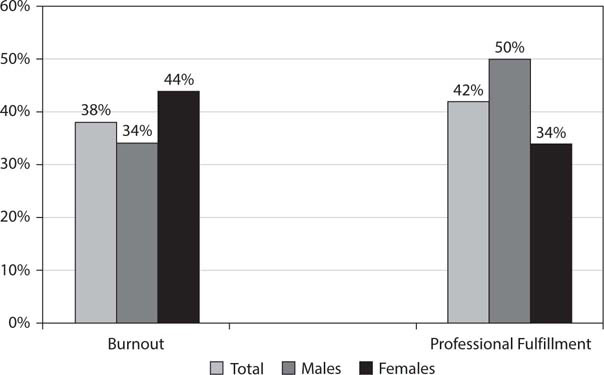
Figure 13-4: Brigham Health, All Departments: Burnout and Professional Fulfillment by Gender, 2017
INITIAL SOLUTIONS AND FUNDING
Initial funding for the burnout and wellness initiative came in fiscal year 2017 for $1.6 million and covered the following:
• Epic 1:1 “at the elbow” training
• launch of the Departmental Wellness Accelerator program
• initiation of planning for the Faculty/Trainee Mental Health Program
• Female Faculty Engagement Program
• launch of B-Well Brigham pilot projects
A return-on-investment approach was used to secure funding, focusing on the impacts of burnout and taking into account the known literature (at the time) that indicated that burnout increases medical error rate, decreases professional effort, and decreases productivity.
Fundamental Dichotomy in Defining Burnout
Among all the data from the surveys on the prevalence of burnout the single biggest driver of burnout was a fundamental dichotomy between the following:
1. The defining image of what life as a physician should be
2. The reality of what current physician practice comprises
The image that most physicians had in entering medicine was one of autonomy in service of caring for patients under humane and scientific principles (as well as teaching and research) in a milieu of respect and appreciation. The reality, however, was found to be different and consisted of feeling a constant pressure to do more with less while being compensated less for more stressors. As the stressors mount, the days grow longer and yet less satisfying with less professional fulfillment.
As disconcerting as that insight may be, having a clear understanding of it is essential to designing effective solutions. What is clear is that the goal of the work of decreasing burnout and increasing professional fulfillment is to reconnect physicians with their passion for patient care, teaching, and research while making their workdays better, easier, and shorter. It is both that simple—and that difficult.
T. S. Eliot notes in “The Hollow Men,”
Between the idea
And the reality,
Between the motion
And the Act,
Falls the shadow
The dichotomy between the perception and the reality of current daily practice casts a shadow over physicians, which increases burnout and decreases fulfillment. It is our task to remove that shadow, to the extent possible, which the initiatives were designed to do.
Summary of Initiatives
As the work of the steering committee progressed, a strategic approach was taken to decreasing burnout and increasing fulfillment, which included the following:
• regularly measuring well-being (burnout and professional fulfillment) using the PFI as a validated statistical survey with external benchmarks
• creating a governance and accountability structure with financial resources for reducing burnout and advancing faculty well-being
• adopting and adapting the Stanford Professional Fulfillment Model well-being framework to address three main areas of focus:
– culture: leadership development, appreciation, community, Brigham to Table (see later in this chapter)
– operational efficiency: Epic/EHR solutions, practice operations, administrative burden
– personal well-being: Faculty/Trainee Mental Health Program, yoga, massage, mindfulness, and other resources
• addressing the identified gender gap through the Female Faculty Initiative, which focuses on advancement, flexibility, and respect
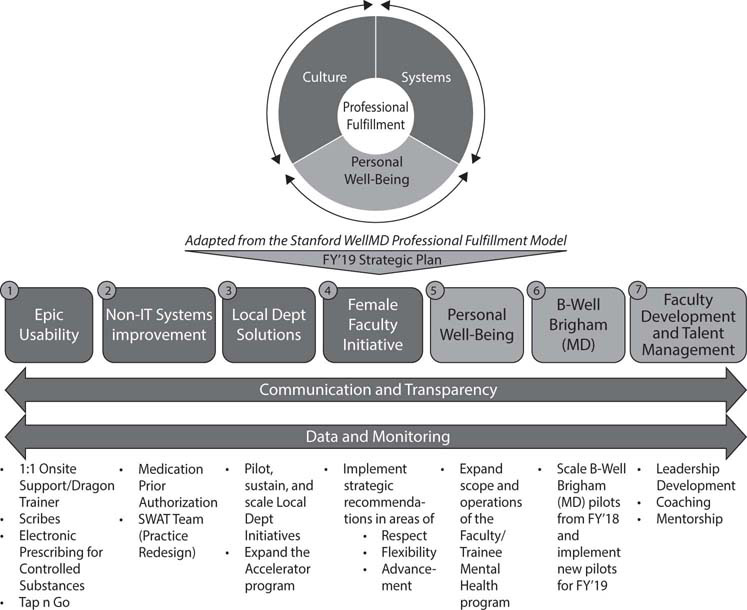
Figure 13-5: The Strategic Plan for the Faculty Development and Well-Being Effort, Fiscal Year 2019
• funding pilot programs that are department-specific and institution-wide, scale interventions that work—for example, B-Well Brigham modules and website access
• participating in benchmarking with the national consortium and across Partners Healthcare to share learning and identify best-practice solutions
The faculty development and well-being strategic plan for fiscal year 2019 is summarized in Figure 13-5. The budget for the program grew from $1.6 million in fiscal years 2017–2018 to $3 million in 2019, of which $1 million was spent and the remainder rolled over into the 2020 and 2021 budgets, with funding expected to remain at the same level, pending results.
ELECTRONIC HEALTH RECORD (EPIC) SOLUTIONS
The free text responses to the initial survey matched interviews with staff in identifying issues with the EHR—in our case, Epic—as the single biggest cause of stress and burnout. Accordingly, a number of solutions (Figure 13-6) designed to make the EHR more accessible were implemented, including the following:
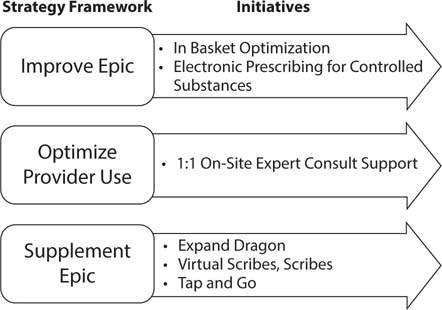
Figure 13-6: Epic Usability: Decreasing EHR Burden for Providers, Fiscal Years 2018–2019
• one-on-one, one-hour “at the elbow” on-site consultation with an expert in the physician’s specialty area
• trials of scribes and virtual scribes
• Dragon voice-recognition training
• electronic prescribing for controlled substances
• “Tap and Go”
Later a daytime EHR hotline was set up to deal with immediate Epic issues to gain resolution. Of these solutions, the “at the elbow” program to allow customization of physicians’ workflows and the hotline were deemed to have been most widely used and successful. Scribe programs are still undergoing rollouts and have been particularly well received in dermatology and emergency medicine.
FEMALE FACULTY INITIATIVE
As a result of the gender gap identified in the initial survey, a consultant was engaged to review the survey and conduct focus groups to further delineate the problem. The physician focus groups included 80 faculty, and an additional 22 senior leaders were consulted. The Female Faculty Working Group and the Female Faculty Steering Committee developed draft blueprints for action based on the findings. Following this, the Faculty Wellness Steering Committee developed a strategic framework for action that was presented to the BWPO Executive Leadership group, which approved the budget and actions of the initiative.
The overall goal of the Female Faculty Initiative was to find opportunities to advance female faculty in each department, implement an intervention, and measure the outcomes.
The proposed interventions included the following:
• Work with departments to create a process for posting open leadership positions under Association of American Medical Colleges guidelines and developing standard work templates. Audit the process at least once.
• Pilot a coaching program to support female faculty performance and career advancement.
• Collaborate with the Office of Women’s Careers to create a dashboard for female faculty career development to allow the team to identify opportunities within departments and track progress.
Unfortunately, despite all these focused efforts to deal with the unique stressors of female physician faculty members, the repeat survey performed in 2019 showed that in the intervening two years, burnout in female physicians increased (from 44 percent to 48 percent) and professional fulfillment declined (from 34 percent to 28 percent) (Figure 13-7). During the same time frame, burnout and professional fulfillment rates did not significantly change in male physicians. (Burnout rates in males went from 34 percent in 2017 to 32 percent in 2019, while fulfillment went from 50 percent to 47 percent. Sample size and response rates did not change, indicating face validity and statistical similarity.)
There may be several explanations for this. First, the increase in organizational focus on burnout and fulfillment may have resulted in increased reporting, although that effect would have to have been differential for females versus males. This effect has been seen in some other surveys. Second, despite the focused efforts of the initiative, job stressors may have increased at a faster pace than adaptive capacity or resiliency. Third, factors and stressors arising from work-life balance in females may have increased differentially in the two-year period between the two surveys. Fourth, other institutions have noted a “penumbra effect,” meaning physicians become aware of the importance of burnout and professional fulfillment yet are caught in the penumbra between awareness of the problems and the solutions needed to correct them. Compounding this would be the fact that the programs, although initiated, were not in place long enough to have a measurable impact. Finally, it is possible the focused efforts simply were not effective, but this is not borne out by personal conversations with those engaged in these efforts. Clearly, more data will be needed to resolve these questions, but there is full commitment to the Female Faculty Initiative.
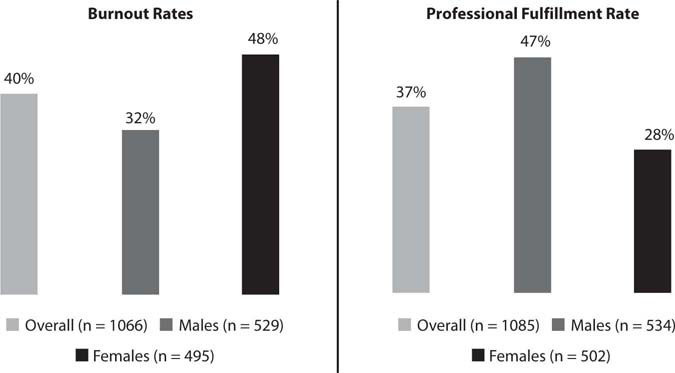
Figure 13-7: Brigham Health: 2019 Clinical Faculty Wellness Survey Data
FACULTY/TRAINEE MENTAL HEALTH PROGRAM
One of the more innovative and successful programs arose out of the survey and interview process. While the well-being survey did not specifically evaluate for mental health diagnoses, physicians are known to have higher rates of depression than the general population. In addition, review of the Brigham Emergency Action Plan utilization revealed low rates of use by physicians. Discussions with outside organizations, including Oregon Health and Science University, revealed models that had been developed specifically to support physician trainees and faculty. The Brigham physicians organization and hospital cofunded the Faculty/Trainee Mental Health Program. The program team comprised a psychiatrist and a psychologist who were hired specifically to support the program. These clinicians were experienced providers committed to addressing the mental health needs of physicians, trainees, and research faculty. The program was done by self-referral with an initial visit to discuss symptoms and determine whether the individual would benefit from ongoing treatment. If ongoing treatment was indicated, individuals could receive up to six confidential sessions to discuss these issues. The sessions were covered under the employee benefit program.
Feedback from the psychiatrist-psychologist team and the users of the program indicated that the perceived value of these sessions was high and that they ranged from coaching or mentoring through more formal therapy sessions. In addition to the therapeutic value, offering this resource was viewed as an important culture change, indicating that BWPO “truly cared and valued” its physicians. After the end of the six sessions, if necessary, a referral is made to an outside provider or alternative provider (Figure 13-8).
Between May 2018 and August 2019, 159 people participated in the program, resulting in 672 visits, 21 percent of which were with faculty. Participation by department ranged from 2 percent to 10 percent. Females were 65 percent and males 35 percent of the visits.
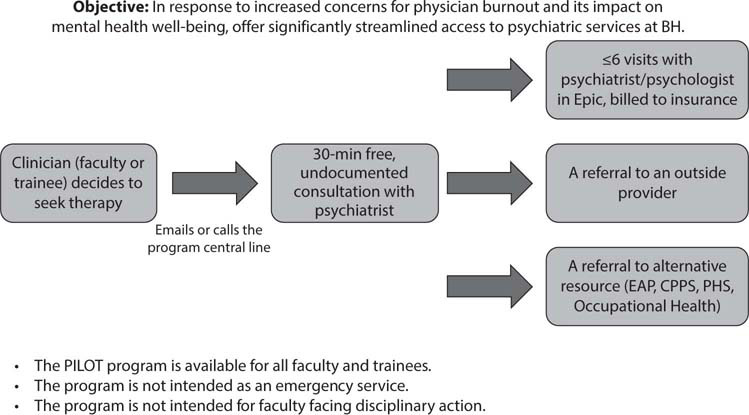
Figure 13-8: Personal Well-Being: Faculty/Trainee Mental Health Program
B-WELL BRIGHAM
B-Well Brigham is a pilot program designed to develop and implement well-being resources for the faculty, including a Faculty Development and Wellbeing website (http://fdw.brighamandwomens.org). The topics include reducing administrative and regulatory burdens, navigating Epic, managing high work volumes, and handling perceived lack of appreciation. A “Monthly Wellbeing Newsletter from the BWPO” was also developed and distributed (https://conta.cc/2m6qrcl).
BRIGHAM TO TABLE
The Brigham to Table program leverages the wisdom that those who “break bread together” work better together by providing lunches paid for by the department three times per week and reimbursing faculty for meals in which two or more faculty members gather to discuss physician well-being. Any opportunity to create communities for interaction combats burnout, and thus other means to bring people together should show equal value and be encouraged.
LOCAL DEPARTMENT SOLUTIONS
The top themes of work done to improve systems and processes to hardwire flow were improving scheduling flexibility, addressing staffing, redesigning workflow, working to understand and solve problems around the physician-nurse dynamic, and providing a 360-degree review process.
What Worked Best?
Feedback from the faculty and the steering committee indicated that some solutions were more effective and better accepted than others. First, the one-on-one “at the elbow” Epic consultations were extremely well received and effective from a practical standpoint, as well as emphasizing a change in culture toward one that invests in Epic workflow changes customized by individual and specialty. Second, the Epic/EHR hotline was also very successful for the same reasons, but more focused on real-time problems with real-time resources. The Faculty/Trainee Mental Health Program, while not used by a majority of faculty, was felt to provide significant value to those who did use the service and has supported many trainees. The trials of scribes, virtual scribes, and voice-recognition technology were effective, particularly in dermatology, where the cost of the programs was offset by increased productivity.
What Worked Less Well?
In general, programs such as yoga classes, meditation, massage, and mindfulness training were less effective. Many felt that work redesign to make clinical practice more effective and efficient was more important, since getting out of work earlier would allow the physicians to use their own resources for these programs. The Brigham to Table program was more used in primary care specialties than in general surgery and surgical subspecialties.
What’s Next?
BWPO is committed to decreasing burnout and increasing physician fulfillment and will continue both its efforts and the benchmarking work nationally and across Partners Healthcare. As new data and innovative programs evolve, they will guide our further efforts. In addition, the work will be coordinated with the hospital and the healthcare system.
Additional Readings
West CP, Dyrbye LN, Rabatin JT, et al. Intervention to promote physician well-being, job satisfaction, and professionalism: a randomized clinical trial. JAMA Intern Med 2014; 174 (4): 527–533.
Trockel M, Bohman B, Lesure E, et al. A brief instrument to assess both burnout and professional fulfillment in physicians: reliability and validity, including correlation with self-reported medical errors, in a sample of residents and practicing physicians. Acad Psychiatry 2018; 42: 11–24.
