19
Tools for Hardwiring Flow and Fulfillment
The six tools for hardwiring flow and fulfillment are designed to assist you and the team in your efforts to make the work easier and more fulfilling by adding value and eliminating waste from every system and process. For more detail on flow, see the “Additional Readings” section at the end of the chapter.
Tool 1: Stop Doing Stupid Stuff, Start Doing Smart Stuff—Send a Signal of Hope
This tool is excellent for the “why” of hardwiring flow and fulfillment, which is a part of organizational resiliency. “Stop doing stupid stuff, start doing smart stuff, and send a signal of hope” is the quintessential “why” of the systems and processes we devise and in which our teams work.1
For those whose healthcare systems have used lean methods, this is the type of “value-added, waste reduction” exercise with which you are familiar.
Everyone benefits, but everyone needs to actively participate in identifying what to stop, what to start, and how to send a signal of hope.
1. Frame the discussion by making clear that all ideas are equally valid until shown to be impossible, innovation is the key to creating “the new normal,” and there are no “sacred cows” or processes that are off-limits.
2. Stress that no criticisms of “stupid stuff” should be personal in nature or perceived to be so. Transparency and confidentiality of attribution but not of ideas should frame all discussions.
3. Start with “stop doing stupid stuff”:
– What are we doing that we need to consider not doing, and why?
– How can we do it a different way?
– Which groups of stakeholders on the teams could best work collaboratively to solve this problem, using creative and innovative ideas?
– When could they complete a draft plan for review?
4. Move quickly to “start doing smart stuff”:
– What smart stuff are we doing, and how can we accelerate and accentuate that?
– What smart stuff can we use to replace the “stupid stuff”?
– Which stakeholders can help devise and deliver these improved solutions?
– How will we use the “three constant questions” of “What are the data? What’s the delta? What’s the decision?”?
5. Send a signal of hope by celebrating the change from “stupid” to “smart,” thereby letting the team know that their innovative efforts are working.
Tool 2: Taxi, Takeoff, Flight Plans, Landings
This concept derives from evidence-based principles and makes the job easier by increasing consistency, predictability, reliability, and safety.2 All work should be consensus based and should cut across the boundaries of the team. The concept applies to the entire team and should be presented at unit or department meetings so there is a shared mental model. Work groups should be developed across the most common clinical entities that the unit treats, which then report back to the larger group.
1. Introduce the idea with the analogy of naval aircraft carrier operations.
– Taxi: moving into position safely and effectively, with the right information
– Takeoff: the most thrilling launch possible when entering the room to meet the patient, with the most succinct but necessary information
– Flight plan: evidence, experience, hardwiring flow, utilization of resources, safety, and so on
– Landing: discharging the patient with attention to detail and Druckenbrod’s queries (Figure 19-1)
2. Discuss the best practices of the “taxi.”
– What information is needed by each team member before greeting the patient?
– Have you reviewed the information for accuracy and consistency?
– Is there any other information needed? How will we get it?
– Pause for a moment to prepare for the “takeoff,” which is next.
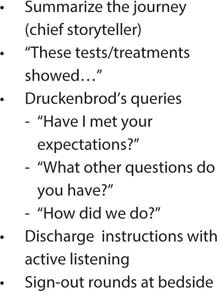
Figure 19-1: Landing: Discharging the Patient
3. Discuss the best practices of the “takeoff.”
– “You never get a second chance to make a first impression” should be a guiding principle.
– What information does each team member want to communicate most effectively when you first greet the patient?
– Think carefully about body language.
– What can be done to “make the patient a part of the team”—moving from “What’s the matter with you?” to “What matters to you?”
– Use precision patient care: “What’s the most important thing we can do to make this an excellent visit?”
– Discuss common elements across team members.
– Discuss using practice, filming, and so on to view “takeoffs” for critique.
4. Discuss the general principle of the “flight plan” without getting too far into the weeds on details.
– Frame the metaphor with airlines and aircraft carriers—each has clearly delineated plans specific to the mission. In the case of healthcare, plans should be developed for the most common clinical entities.
– Discuss using demand-capacity questions to identify the most common clinical and patient experience presentations seen on the clinical unit.
– Recruit cross-functional teams to develop “flight plans” for the most common clinical entities.
5. Discuss the concept of the “landing”: the principle of completing the clinical encounter in the best possible way.
– Summarize the journey—be the chief storyteller.
– Make sense of the journey—be the chief sensemaker.
– Provide discharge instructions with active listening.
– Ask Druckenbrod’s queries:
◦ “Have we met your expectations?”
◦ “What questions do you have?”
◦ “How did we do?”
Tool 3: Making the Patient a Part of the Team
Making the patient part of the team—and the center of the team—makes the job exponentially easier.3 This transition is intuitive, but rarely executed as well as it needs to be, giving lots of room for improvement. This tool is an essential leadership tool for all team members at all levels.
1. Frame the discussion by emphasizing that patients are the only reason we have healthcare teams.
2. As logical and intuitive as “making the patient a part of the team” may be, it is not commonly enacted, in my experience. How do we make this a reality?
3. It starts with the following process:
– Move away from “What’s the matter with you?”
– Move toward “What matters to you?”
– Make clear that this does not mean that we are ignoring the clinical, technical aspects of care.
– It does mean that we can’t ignore what matters to the patient as we make them part of the team.
– Have the team talk about one to three of the most common clinical entities and the differences between “with you” and “to you.”
4. Discuss moving from perceiving patients as recipients of care to perceiving them as participants in their care:
– “If that were your husband or wife/your dad or mom/your son or daughter, would you prefer them to be a recipient or a participant?”
– Participants have input in the generation of care plans; recipients are passive receivers of care plans.
5. Introduce the motto that patients should have: “Nothing about me without me.”
– Are we committed to asking questions to assess the patients’ input on their care so nothing is done to them without them?
– Are we willing to hear what patients and families say to help guide our care?
– Are we willing to act on addressing this input to incorporate patient and family choices and preferences?
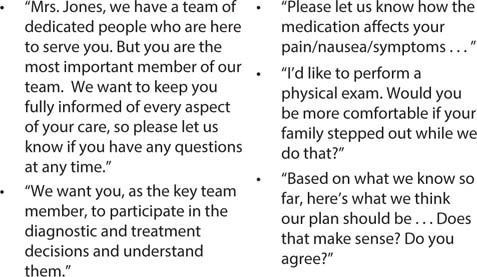
Figure 19-2: Scripts for Making the Patient Part of the Team
– (In most cases, this does not dramatically change the actual evidence-based clinical diagnostic and therapeutic plan, but it does assure that the patient and family feel more a part of the process and decision-making.)
6. Discuss these questions:
– What actions are we taking to “make the patient part of the team”?
– What, specifically, are we doing differently?
– Is the entire team doing that?
– If we asked the team, would they agree?
– If we asked the patients, would they agree?
7. Begin to develop evidence-based language (scripts) to let patients know they are not only a part of the team but the most important part of the team (Figure 19-2).
Tool 4: Precision Patient Care
What could make the job easier than knowing the patient’s expectations, as well as the most important thing the team could do? Leading yourself and leading the team requires clarity about the patient’s viewpoint.
1. Frame the discussion with the concept that every patient approaches the patient encounter carrying “baggage” that may not be visible but is nonetheless present.
2. That baggage is their expectations. Every patient has expectations for what the medical encounter will be like (Figure 19-3).
3. How can we discover the complex calculus of patient expectations? Simply ask them, “What are your expectations?”
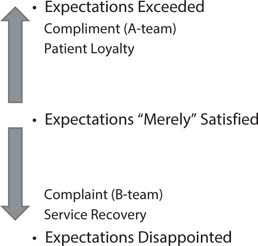
Figure 19-3: Understanding Patient Expectations
4. When expectations are not met, that creates dissatisfaction and patient complaints. But exceeding expectations is the key to patient loyalty.
5. The key to the ability to exceed expectations is precision patient care, which simply asks, “What is the most important thing we can do to make this an excellent experience?”
6. Ask the team members whether they are comfortable with this question.
7. If not, why not?
8. Ask, “Wouldn’t it make our jobs easier if we knew what the most important thing was that we could do to make the experience excellent?”
Tool 5: Clinical Huddles and Demand-Capacity Management Tools
One of the most powerful ways to make the job easier is to be able to anticipate the work, deal with the rate-limiting steps and bottlenecks of the existing work, and be able to implement a plan for them. The combination of clinical huddles and demand-capacity tools can make this possible, since they are specifically focused on decreasing job stressors and increasing the team’s resiliency.
1. Frame the discussion by defining the work done with the five demand-capacity questions (Figure 19-4) and clinical huddles (Figure 19-5).
2. Focus on the intent of both to do the following:
– Decrease job stressors by anticipating demands and sharing current workloads, bottlenecks, and so on.
– Increase team resiliency to adapt to the circumstances.
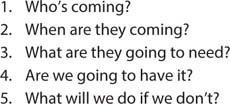
Figure 19-4: The Five Demand-Capacity Questions

Figure 19-5: The Function of Clinical Huddles
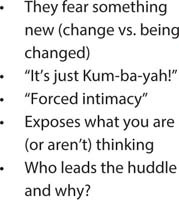
Figure 19-6: Sources of Resistance to Clinical Huddles
3. Open a discussion of, at a minimum, these points:
– How are the huddles working?
– What are the positives?
– What are the negatives?
– Are there discussions of bottlenecks or rate-limiting steps?
– Are they effective in easing the problem?
– How would you change the huddles to make them more effective?
– Are the five demand-capacity questions being used?
– What are the sources of resistance to clinical huddles (Figure 19-6)?
Tool 6: The EHR Solutions Summarized
The electronic health record (EHR) solutions are woven into all the other tools, so the time needed is variable. In most cases this will best be handled through assigned workgroups. Every team member who interfaces with the EHR is affected by its requirements and needs to be involved in devising solutions or work-arounds. Start with nurse- and physician-specific workgroups but integrate results early and often.
1. Make an early and visible commitment to “take on the EHR” and transition quickly to finding ways to work with the EHR.
2. Get a commitment from IT, preferably from the chief information officer and chief medical information officer, to work with your teams in a collegial fashion. If at all possible, have them come to the “kickoff” meeting where the work will be discussed.
3. Identify nursing and physician superusers and superstars to help guide the work. Working from within is always better than mandating solutions from outside.
4. The “love, hate, tolerate” tool is particularly helpful in finding EHR solutions.
5. Follow the principles delineated in Chapter 11 as templates for improvement.
6. Summarize successes early and often.
7. Identify obstacles and a plan to attack them.
Additional Readings
Mayer T, Jensen K. Hardwiring Flow: Systems and Processes for Seamless Patient Care. 2009; Gulf Breeze, FL: Fire Starter Press.
Mayer T, Jensen K. Hardwiring hospital-wide flow to drive sustainable competitive performance. Management in Healthcare 2019; 2: 27–35.
Jensen K, Mayer T. The Patient Flow Advantage: How Hardwiring Hospital-Wide Flow Provides Sustained Competitive Advantage. 2014; Pensacola, FL: Fire Starter Press.
