Diagnosis Coding: A Number for Every Disease
What Is a Diagnosis?
A diagnosis is the identification of a disease from its symptoms. Obviously, the next question is, “What is a symptom?” You are the best judge of that, because a symptom is a perceptible change in your body or its functions that can indicate disease. Although it is possible to be sick or have a disease and have no symptoms, a symptom is a hint that there may be a problem and that you should seek professional help.
When you have a sore throat, that is a symptom. If the sore throat lasts more than a day or two, you will probably visit your doctor to get his or her opinion about the cause of the sore throat. Based on your symptom, the sore throat, and an exam of your physical condition, the doctor may arrive at a diagnosis. More than 100 diagnoses could possibly be the cause of your sore throat. How will the doctor arrive at the correct diagnosis?
Deducing the Diagnosis: History
The first step in the path toward a diagnosis is the history. The doctor may ask you questions such as the following:
![]() How long have you had the sore throat? (duration)
How long have you had the sore throat? (duration)
![]() What part of your throat hurts? (location)
What part of your throat hurts? (location)
![]() Is the pain continuous? Does it become better or worse? (timing)
Is the pain continuous? Does it become better or worse? (timing)
![]() How does it compare to other sore throats you have had? (severity)
How does it compare to other sore throats you have had? (severity)
![]() Do you also have other symptoms? (associated signs and symptoms)
Do you also have other symptoms? (associated signs and symptoms)
![]() What are you doing when it hurts? (context)
What are you doing when it hurts? (context)
![]() How would you describe the pain? (quality)
How would you describe the pain? (quality)
![]() What have you done to obtain relief? Did it work? (modifying factors)
What have you done to obtain relief? Did it work? (modifying factors)
These eight categories of questions are known as the History of Present Illness (HPI). They constitute a chronological description of your present illness from the first sign or symptom to the present. Once you have responded to these questions, the direction to go next will usually be clearer to the doctor.
A Review of Systems (ROS) is an inventory of body systems obtained through a series of questions that seek to identify signs and/or symptoms that you may be experiencing (Figure 2-1). Your doctor may give you a check-off form to fill out in order to get your responses to these questions.
There are 14 systems that the doctor may review:

FIGURE 2-1 “Review of symptoms” form your doctor may ask you to complete.
The doctor may perform all or part of the review of systems, depending on your presenting problem. The review of systems is intended to identify symptoms you may have forgotten to mention. It also explores and provides support for the doctor’s theory about the cause of your symptom. If he feels that the sore throat is due to a respiratory allergy, you can expect to see the respiratory and allergy portions emphasized in the review of systems.
Because hereditary or environmental factors contribute to many diseases, the final part of the history performed by the doctor is the past, family, and social history.
Past history includes illnesses, surgeries, medications, and allergic reactions. A thorough documentation of past history should include checking by the physician for objective evidence that the reported conditions actually existed. Lab results and diagnostic testing reports in your medical record should support the history.
Family history covers any factor within your immediate family that may affect you or the probability that you will have specific conditions, such as cancer, diabetes, heart disease, or other hereditary risk factors. The presence of communicable diseases that are not hereditary can also be important if you are exposed through contact with your family.
Social history encompasses a wide variety of habits, including the following:
![]() Smoking history: How much, how long
Smoking history: How much, how long
![]() Alcohol intake: Type, quantity, frequency
Alcohol intake: Type, quantity, frequency
![]() Other drug use: Type, route, frequency, duration
Other drug use: Type, route, frequency, duration
![]() Sexual activity: Gender orientation, birth control, marital status, risk factors
Sexual activity: Gender orientation, birth control, marital status, risk factors
![]() Work history: Occupation, risk factors
Work history: Occupation, risk factors
![]() Hobbies, activities, interests
Hobbies, activities, interests
The information in the social history not only provides additional information relevant to determining the cause of the presenting symptoms but also can facilitate the physician–patient relationship if your doctor knows more about you as a person and not just as a body.
Deducing the Diagnosis: Exam
According to the federal government’s Center for Medicare and Medicaid Services (CMS), your doctor can perform 12 different types of physical examinations. Unless you are seeing a specialist, your doctor will usually perform a “general multisystem examination,” including the systems he or she feels are relevant to your presenting problem or symptom.
The following are a few definitions of terms used in describing physical exam procedures:
![]() Palpation: Examination by pressing on the surface of the body to feel the organs or tissues underneath.
Palpation: Examination by pressing on the surface of the body to feel the organs or tissues underneath.
![]() Auscultation: Listening to sounds within the body, either by direct application of the ear or through a stethoscope.
Auscultation: Listening to sounds within the body, either by direct application of the ear or through a stethoscope.
![]() Percussion: A method of examination by tapping the fingers at various points on the body to determine the position and size of structures beneath the surface.
Percussion: A method of examination by tapping the fingers at various points on the body to determine the position and size of structures beneath the surface.
The officially defined “general multisystem examination” includes the following (Center for Medicare and Medicaid Services, n.d.) categories.
CONSTITUTIONAL
![]() Measurement of any three of the following seven vital signs:
Measurement of any three of the following seven vital signs:
![]() Sitting or standing blood pressure
Sitting or standing blood pressure
![]() Supine blood pressure
Supine blood pressure
![]() Pulse rate and regularity
Pulse rate and regularity
![]() Respiration
Respiration
![]() Temperature
Temperature
![]() Height
Height
![]() Weight
Weight
![]() General appearance of the patient (e.g., development, nutrition, body habits, deformities, attention to grooming)
General appearance of the patient (e.g., development, nutrition, body habits, deformities, attention to grooming)
EYES
![]() Inspection of conjunctivae and lids
Inspection of conjunctivae and lids
![]() Examination of pupils and irises (e.g., reaction to light and accommodation, size and symmetry)
Examination of pupils and irises (e.g., reaction to light and accommodation, size and symmetry)
![]() Ophthalmoscopic examination of optic discs (e.g., size, C/D ratio, appearance) and posterior segments (e.g., vessel changes, exudates, hemorrhages)
Ophthalmoscopic examination of optic discs (e.g., size, C/D ratio, appearance) and posterior segments (e.g., vessel changes, exudates, hemorrhages)
EARS, NOSE, MOUTH, AND THROAT
![]() External inspection of ears and nose (e.g., overall appearance, scars, lesions, masses)
External inspection of ears and nose (e.g., overall appearance, scars, lesions, masses)
![]() Otoscopic examination of external auditory canals and tympanic membranes
Otoscopic examination of external auditory canals and tympanic membranes
![]() Assessment of hearing (e.g., whispered voice, finger rub, tuning fork)
Assessment of hearing (e.g., whispered voice, finger rub, tuning fork)
![]() Inspection of nasal mucosa, septum, and turbinates
Inspection of nasal mucosa, septum, and turbinates
![]() Inspection of lips, teeth, and gums
Inspection of lips, teeth, and gums
![]() Examination of oropharynx: oral mucosa, salivary glands, hard and soft palates, tongue, tonsils, and posterior pharynx
Examination of oropharynx: oral mucosa, salivary glands, hard and soft palates, tongue, tonsils, and posterior pharynx
![]() Examination of neck (e.g., masses, overall appearance, symmetry, tracheal position, crepitus)
Examination of neck (e.g., masses, overall appearance, symmetry, tracheal position, crepitus)
![]() Examination of thyroid (e.g., enlargement, tenderness, mass)
Examination of thyroid (e.g., enlargement, tenderness, mass)
RESPIRATORY
![]() Assessment of respiratory effort (e.g., intercostals retractions, use of accessory muscles, diaphragmatic movement)
Assessment of respiratory effort (e.g., intercostals retractions, use of accessory muscles, diaphragmatic movement)
![]() Percussion of chest (e.g., dullness, flatness, hyperresonance)
Percussion of chest (e.g., dullness, flatness, hyperresonance)
![]() Palpation of chest (e.g., tactile fremitus)
Palpation of chest (e.g., tactile fremitus)
![]() Auscultation of lungs (e.g., breath sounds, adventitious sounds, rubs)
Auscultation of lungs (e.g., breath sounds, adventitious sounds, rubs)
CARDIOVASCULAR
![]() Palpation of heart (e.g., location, size, thrills)
Palpation of heart (e.g., location, size, thrills)
![]() Auscultation of heart with notation of abnormal sounds and murmurs
Auscultation of heart with notation of abnormal sounds and murmurs
![]() Examination of
Examination of
![]() Carotid arteries (e.g., pulse amplitude, bruits)
Carotid arteries (e.g., pulse amplitude, bruits)
![]() Abdominal aorta (e.g., size, bruits)
Abdominal aorta (e.g., size, bruits)
![]() Femoral arteries (e.g., pulse amplitude, bruits)
Femoral arteries (e.g., pulse amplitude, bruits)
![]() Pedal pulses (e.g., pulse amplitude)
Pedal pulses (e.g., pulse amplitude)
![]() Extremities for edema and/or varicosities
Extremities for edema and/or varicosities
CHEST (BREASTS)
![]() Inspection of breasts (e.g., symmetry, nipple discharge)
Inspection of breasts (e.g., symmetry, nipple discharge)
![]() Palpation of breasts and axillae (e.g., masses or lumps, tenderness)
Palpation of breasts and axillae (e.g., masses or lumps, tenderness)
GASTROINTESTINAL (ABDOMEN)
![]() Examination of abdomen with notation of presence of masses or tenderness
Examination of abdomen with notation of presence of masses or tenderness
![]() Examination of liver and spleen
Examination of liver and spleen
![]() Examination for presence or absence of hernia
Examination for presence or absence of hernia
![]() Examination (when indicated) of anus, perineum, and rectum, including sphincter tone, presence of hemorrhoids, rectal masses
Examination (when indicated) of anus, perineum, and rectum, including sphincter tone, presence of hemorrhoids, rectal masses
![]() Obtain stool sample for occult blood test when indicated
Obtain stool sample for occult blood test when indicated
GENITOURINARY
Male
![]() Examination of the scrotal contents (e.g., hydrocele, spermatocele, tenderness of cord, testicular mass)
Examination of the scrotal contents (e.g., hydrocele, spermatocele, tenderness of cord, testicular mass)
![]() Examination of the penis
Examination of the penis
![]() Digital rectal examination of prostate gland (e.g., size, symmetry, nodularity, tenderness)
Digital rectal examination of prostate gland (e.g., size, symmetry, nodularity, tenderness)
Female
Pelvic examination (with or without specimen collection for smears and cultures) including:
![]() Examination of external genitalia (e.g., general appearance, hair distribution, lesions) and vagina (e.g., general appearance, estrogen effect, discharge, lesions, pelvic support, cystocele, rectocele)
Examination of external genitalia (e.g., general appearance, hair distribution, lesions) and vagina (e.g., general appearance, estrogen effect, discharge, lesions, pelvic support, cystocele, rectocele)
![]() Examination of urethra (e.g., masses, tenderness, scarring)
Examination of urethra (e.g., masses, tenderness, scarring)
![]() Examination of bladder (e.g., fullness, masses, tenderness)
Examination of bladder (e.g., fullness, masses, tenderness)
![]() Examination of the cervix (e.g., general appearance, lesions, discharge)
Examination of the cervix (e.g., general appearance, lesions, discharge)
![]() Examination of the uterus (e.g., size, contour, position, mobility, tenderness, consistency, descent, or support)
Examination of the uterus (e.g., size, contour, position, mobility, tenderness, consistency, descent, or support)
![]() Examination of the adnexa/parametria (e.g., masses, tenderness, organomegaly, nodularity)
Examination of the adnexa/parametria (e.g., masses, tenderness, organomegaly, nodularity)
LYMPHATIC
Palpation of lymph nodes in two or more areas:
![]() Neck
Neck
![]() Axillae
Axillae
![]() Groin
Groin
![]() Other
Other
![]() Examination of gait and station
Examination of gait and station
![]() Inspection and/or palpation of digits and nails (e.g., clubbing, cyanosis, inflammatory conditions, petechiae, ischemia, infections, nodes)
Inspection and/or palpation of digits and nails (e.g., clubbing, cyanosis, inflammatory conditions, petechiae, ischemia, infections, nodes)
![]() Examination of joints, bones, and muscles of one or more of the following six areas: (1) head and neck; (2) spine, ribs, and pelvis; (3) right upper extremity; (4) left upper extremity; (5) right lower extremity; and (6) left lower extremity. The examination of a given area includes:
Examination of joints, bones, and muscles of one or more of the following six areas: (1) head and neck; (2) spine, ribs, and pelvis; (3) right upper extremity; (4) left upper extremity; (5) right lower extremity; and (6) left lower extremity. The examination of a given area includes:
![]() Inspection and/or palpation with notation of presence of any misalignment, asymmetry, crepitation, defects, tenderness, masses, effusions
Inspection and/or palpation with notation of presence of any misalignment, asymmetry, crepitation, defects, tenderness, masses, effusions
![]() Assessment of range of motion with notation of any pain, crepitation, or contracture
Assessment of range of motion with notation of any pain, crepitation, or contracture
![]() Assessment of stability with notation of any dislocation (luxation), subluxation, or laxity
Assessment of stability with notation of any dislocation (luxation), subluxation, or laxity
![]() Assessment of muscle strength and tone (e.g., flaccid, cogwheel, spastic, with notation of any atrophy or abnormal movements
Assessment of muscle strength and tone (e.g., flaccid, cogwheel, spastic, with notation of any atrophy or abnormal movements
SKIN
![]() Inspection of skin and subcutaneous tissue (e.g., rashes, lesions, ulcers)
Inspection of skin and subcutaneous tissue (e.g., rashes, lesions, ulcers)
![]() Palpation of skin and subcutaneous tissue (e.g., induration, subcutaneous nodules, tightening)
Palpation of skin and subcutaneous tissue (e.g., induration, subcutaneous nodules, tightening)
NEUROLOGIC
![]() Test cranial nerves with notation of any deficit
Test cranial nerves with notation of any deficit
![]() Examination of deep tendon reflexes with notation of any pathological reflexes (e.g., Babinski)
Examination of deep tendon reflexes with notation of any pathological reflexes (e.g., Babinski)
![]() Examination of sensation (e.g., by touch, pin vibration, proprioception)
Examination of sensation (e.g., by touch, pin vibration, proprioception)
PSYCHIATRIC
![]() Description of patient’s judgment and insight
Description of patient’s judgment and insight
![]() Brief assessment of mental status, including:
Brief assessment of mental status, including:
![]() Orientation to time, place, and person
Orientation to time, place, and person
![]() Recent and remote memory
Recent and remote memory
![]() Mood and affect (e.g., depression, anxiety, agitation)
Mood and affect (e.g., depression, anxiety, agitation)
Reality Check
You are thinking, “My doctor spent 15 minutes with me and didn’t do half of this stuff!” You are correct. The extent of the examination will depend on what your doctor needs to examine or measure in order to identify the cause of your sore throat. A likely scenario would be taking your vital signs (done by the nurse), examining your throat, looking at your ears to see if your tympanic membranes are involved, listening to your chest, and possibly palpating your lymph nodes. The doctor will also observe your general appearance for additional signs.
Some of the information obtained during the physical exam is noted solely by observation. The doctor can tell just by looking whether you have a rash that might indicate a disease related to a sore throat. Likewise, your ability to walk across the room and climb up on the exam table will provide clues to your gait. The discussion between you and your doctor will yield information about your judgment and insight into your mental status.
Deducing the Diagnosis: Medical Decision Making
Now that your doctor knows the history of your sore throat and has examined you, the next step in the process of arriving at a diagnosis is medical decision making. This involves assessment of the objective data and selection of the most likely cause of your sore throat. It may involve additional diagnostic testing, such as a throat culture to check for bacteria. If you are a smoker or if it is goldenrod season, the doctor may suspect other causes.
In complicated cases with many presenting symptoms, the doctor may use the process of differential diagnosis, which is weighing the probability of one disease versus another as the cause of the patient’s symptoms. Sore throat can be caused by bacterial or viral infection, throat irritation or inflammation, allergic reaction, fungal infection, or even just dry air.
Your doctor will make a decision about why your throat is sore and provide a treatment plan that may involve prescription or over-the-counter medications; symptomatic treatments, such as gargles; or environmental changes, such as a humidifier.
Documenting the Diagnosis
Once the decision-making process is complete, the doctor must document the diagnosis in your medical record. A complete diagnostic statement always includes the following:
![]() Site: The physical location; if the location has laterality (left or right), it must be documented as well.
Site: The physical location; if the location has laterality (left or right), it must be documented as well.
![]() Etiology: The cause of the condition.
Etiology: The cause of the condition.
For your sore throat, a complete diagnostic statement might be the following:
![]() “Strep pharyngitis”
“Strep pharyngitis”
![]() Site = pharynx
Site = pharynx
![]() Etiology = streptococcal bacteria
Etiology = streptococcal bacteria
What Number Is My Diagnosis?
Now that you have a diagnosis documented in words by your doctor, it can be converted into a diagnosis code number. The International Classification of Diseases, Revision 10, Clinical Modification (ICD-10-CM) will be used in the United States for diagnosis coding as of 2015. It contains over 71,000 unique codes. This does not mean that each of the more than 100,000 known disease entities has a separate code. When the phrase “diagnosis code” is used, its actual meaning is “diagnosis category code.”
An example of a diagnosis category is R79.0, “Abnormal level of blood mineral.” This code category includes abnormal blood levels of cobalt, copper, iron, magnesium, or zinc. Use of R79.0 does not tell you which mineral is abnormal. Nor does it tell you whether the blood level is abnormally low or abnormally high.
A diagnosis code category is analogous to a zip code. The zip code 04558 is for Maine, but it covers two towns, New Harbor and Pemaquid. With just the zip code number, it is not possible to positively identify which town is intended.
The translation process known as coding takes the words documented as a diagnosis and converts them into a diagnosis category code number. This is necessary not only for statistical purposes, but also because of the variation in the naming conventions for diseases. Regional differences in medical terminology in the United States may result in several different terms for the same disease entity.
Your sore throat diagnosis, “strep pharyngitis,” is assigned to a category code number by a two-step process.
1. The main term or noun, “pharyngitis,” is located in the alphabetical part of ICD-10-CM, the index to diseases; the subterm or adjective “strep” is searched for under “pharyngitis” (Figure 2-2).
2. A category code number, J02.0, is listed next to the entry for “Pharyngitis, streptococcal.” In order to ensure that this number is correct, it is necessary to verify the number in the numerical part of ICD-10-CM, known as the tabular list (Figure 2-3).
The diagnostic terms listed under J02.0 include not only streptococcal pharyngitis, but also septic pharyngitis and streptococcal sore throat. Previously, in ICD-9-CM, the code for strep pharyngitis also included strep laryngitis and strep tonsillitis. These have their own codes in ICD-10-CM, an example of its higher specificity.

FIGURE 2-2 Pharyngitis index entries.
Reproduced from ICD-10-CM Code Index to Diseases and Injuries, 2014. Centers for Medicare and Medicaid Services. Available at http://www.cms.gov/Medicare/Coding/ICD10/2014-ICD-10-CM-and-GEMs.html.
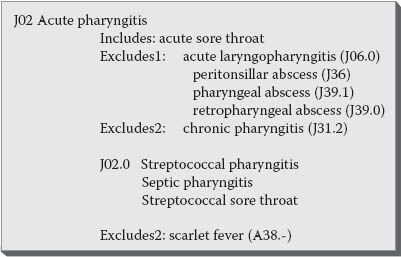
FIGURE 2-3 Pharyngitis tabular entries.
Reproduced from ICD-10-CM Tabular List of Diseases and Injuries, 2014. Centers for Medicare and Medicaid Services. Available at http://www.cms.gov/Medicare/Coding/ICD10/2014-ICD-10-CM-and-GEMs.html.
The two-step coding process just described sounds straightforward: look in the alphabetical index and then verify the number in the tabular list. Why can’t this be done by a computer? In fact, most hospitals and other medical facilities do use computerized coding tools called encoders to facilitate the coding process. They range from simple programs that are only replications of the coding books in a computerized format to sophisticated interactive software that asks all of the questions necessary to arrive at the correct diagnosis category code.
For your sore throat diagnosis, the simple encoder would bring up the list of pharyngitis entries, and the coding analyst would have to select “streptococcal” from that list. The sophisticated encoder would find pharyngitis and then ask the user the questions “Due to bacteria?” and then “Due to which bacteria?” before selecting a code. Branching logic in the sophisticated products ensures correct code selection in complex disease entities.
Why can’t the computer do it all? The coding process is subject to any number of potential problems that make it essential that a coding analyst, a knowledgeable human being, be involved. Because diagnosis codes are often used to determine reimbursement, the coding process is governed by rules that must be followed by any entity submitting a claim for payment by a third party such as a government program or private insurance.
Failure to follow these rules can result in the submission of a false claim, which is subject to criminal and civil penalties, including imprisonment and fines.
What can go wrong in the diagnosis coding process?
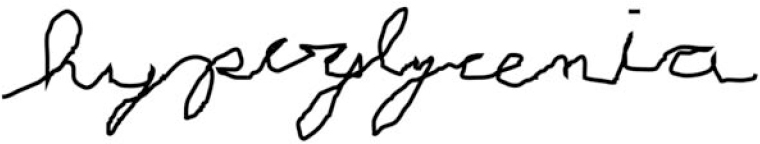
![]() Illegible physician handwriting
Illegible physician handwriting
![]() Look at Figure 2-4. What do you think it says?
Look at Figure 2-4. What do you think it says?
![]() Illogical physician diagnosis documentation
Illogical physician diagnosis documentation
![]() “#1) Chest pain secondary to #1”
“#1) Chest pain secondary to #1”
![]() “Fractured ear lobe” (not anatomically possible)
“Fractured ear lobe” (not anatomically possible)
![]() Lack of physician documentation
Lack of physician documentation
![]() Transcription errors by typist or voice-recognition systems
Transcription errors by typist or voice-recognition systems
![]() “Baloney amputation” (should be below-knee amputation)
“Baloney amputation” (should be below-knee amputation)
![]() “Liver birth” (should be live birth)
“Liver birth” (should be live birth)
![]() Content of the rest of the patient’s medical record does not support the diagnosis documented
Content of the rest of the patient’s medical record does not support the diagnosis documented
![]() Lack of specificity
Lack of specificity
![]() “Anemia” (there are several hundred different types of anemia)
“Anemia” (there are several hundred different types of anemia)
Each of these issues must be resolved before an accurate diagnosis code can be assigned.
What Are the Rules?
The rules for diagnosis coding in the United States are developed and approved by the Cooperating Parties for ICD-10-CM, which include the CMS, the National Center for Health Statistics (NCHS), the American Hospital Association (AHA), and the American Health Information Management Association (AHIMA). Both ICD-10-CM and the Official Guidelines for Coding and Reporting are in the public domain and may be accessed at no charge on the Internet or via public document depository library services (National Center for Health Statistics, 2014).
The rules are 117 pages and consist of the following:
![]() Conventions and general coding guidelines
Conventions and general coding guidelines
![]() Chapter-specific guidelines
Chapter-specific guidelines
![]() Selection of principal diagnosis for inpatients
Selection of principal diagnosis for inpatients
![]() Reporting additional diagnoses for inpatients
Reporting additional diagnoses for inpatients
![]() Diagnostic coding and reporting guidelines for outpatient services
Diagnostic coding and reporting guidelines for outpatient services
![]() Present-on-admission reporting guidelines
Present-on-admission reporting guidelines
In addition to the official rules, federal and state government programs such as Medicare and Medicaid promulgate regulations intended to define appropriate code usage or add the weight of law to the guidelines. An example was the Medicare transmittal that defined for its contractors the appropriate rules for ICD-9-CM coding for diagnostic tests (Department of Health and Human Services, 2001). This transmittal was initially issued because of concerns about contractors in different geographic locations inconsistently interpreting the official guidelines. The transmittal language was later incorporated into the official claims processing manual.
Conventions: Section I.A.
Punctuation:
![]() Brackets [ ] are used in the tabular list to enclose synonyms, alternative wording, or explanatory phrases.
Brackets [ ] are used in the tabular list to enclose synonyms, alternative wording, or explanatory phrases.
![]() Parentheses ( ) are used to enclose supplementary words that may be either present or absent in the statement of a disease without affecting the code number to which it is assigned. For example, see the following index entry:
Parentheses ( ) are used to enclose supplementary words that may be either present or absent in the statement of a disease without affecting the code number to which it is assigned. For example, see the following index entry:
Hallucinosis (chronic) F28
It makes no difference whether the word chronic is present in the diagnosis.
![]() Colons (:) are used in the tabular list after an incomplete term that needs one or more of the words following the colon to make it assignable to a specific category.
Colons (:) are used in the tabular list after an incomplete term that needs one or more of the words following the colon to make it assignable to a specific category.
Abbreviations:
![]() NEC means “not elsewhere classifiable.” This is equivalent to “other specified,” which means the documentation in the medical record provides detail for which a specific code does not exist.
NEC means “not elsewhere classifiable.” This is equivalent to “other specified,” which means the documentation in the medical record provides detail for which a specific code does not exist.
![]() NOS means “not otherwise specified.” This is equivalent to “unspecified,” indicating that the documentation in the medical record is insufficient to assign a more specific code.
NOS means “not otherwise specified.” This is equivalent to “unspecified,” indicating that the documentation in the medical record is insufficient to assign a more specific code.
Standard meanings:
![]() “And” should be interpreted to mean either “and” or “or.”
“And” should be interpreted to mean either “and” or “or.”
![]() “With” should be interpreted to mean “associated with” or “due to.”
“With” should be interpreted to mean “associated with” or “due to.”
Instructional Notes: Section I.A.
![]() “See” following a main term in the alphabetic index means that another term should be referenced. The correct code will not be located unless this instruction is followed.
“See” following a main term in the alphabetic index means that another term should be referenced. The correct code will not be located unless this instruction is followed.
![]() “See also” means that there is another main term that may have useful additional index entries that are helpful, but it is not mandatory to follow the “see also” instruction if the necessary code is found under the original main term.
“See also” means that there is another main term that may have useful additional index entries that are helpful, but it is not mandatory to follow the “see also” instruction if the necessary code is found under the original main term.
![]() “Code first” mandates that the underlying etiology or cause of the condition to be coded must be coded first, and then the manifestation.
“Code first” mandates that the underlying etiology or cause of the condition to be coded must be coded first, and then the manifestation.
![]() “Use additional code” will be found at the etiology listing to remind coders that the manifestation should also be coded.
“Use additional code” will be found at the etiology listing to remind coders that the manifestation should also be coded.
![]() “Code also” means that two codes may be needed to fully describe a condition, but the sequence of those codes is not defined.
“Code also” means that two codes may be needed to fully describe a condition, but the sequence of those codes is not defined.
![]() “Excludes type 1” is used when two conditions cannot occur together and should not be coded together.
“Excludes type 1” is used when two conditions cannot occur together and should not be coded together.
![]() “Excludes type 2” means the excluded condition is not part of the condition represented by the code, but the two codes may be used together, if appropriate.
“Excludes type 2” means the excluded condition is not part of the condition represented by the code, but the two codes may be used together, if appropriate.
General Coding Guidelines: Section I.A.
These guidelines tell coding analysts the basic information they need in order to code correctly, based on physician documentation.
![]() Locate each term in the alphabetic index and verify the code selected in the tabular list. The alphabetic index does not always provide the full code, so it is mandatory to reference the tabular list as well. Read and be guided by any instructional notations.
Locate each term in the alphabetic index and verify the code selected in the tabular list. The alphabetic index does not always provide the full code, so it is mandatory to reference the tabular list as well. Read and be guided by any instructional notations.
![]() Valid diagnosis codes may have three, four, five, six, or seven characters. Any code with more than three characters has a decimal point after the third character. A code with fewer than seven characters may only be used if it is not further subdivided.
Valid diagnosis codes may have three, four, five, six, or seven characters. Any code with more than three characters has a decimal point after the third character. A code with fewer than seven characters may only be used if it is not further subdivided.
Example: “J14 Hemophilus pneumonia” may be used because it is not further subdivided. “J15 Bacterial pneumonia, NEC” may not be used with only three characters, because it is further subdivided into several four-character codes.
ICD-10-CM uses a placeholder, character “X,” at certain codes to allow for future expansion. The “X” placeholder may also be needed if a code that requires a seventh character is not a six-character code; the X must be used to fill in the empty characters.
![]() Codes that describe symptoms and signs, as opposed to diagnoses, are acceptable if a related definitive diagnosis has not been established by the physician.
Codes that describe symptoms and signs, as opposed to diagnoses, are acceptable if a related definitive diagnosis has not been established by the physician.
Example: R55, syncope (fainting), is a symptom code. It may be used if the physician does not identify and document a diagnosis responsible for the fainting.
![]() Signs and symptoms that are an integral part of a disease process should not be assigned as additional codes.
Signs and symptoms that are an integral part of a disease process should not be assigned as additional codes.
Example: Shortness of breath is integral to congestive heart failure and would not be coded separately.
![]() Signs and symptoms that may not be associated routinely with a disease process should be coded when present.
Signs and symptoms that may not be associated routinely with a disease process should be coded when present.
![]() Some single conditions may require more than one code for a full description. Generally, one code is for the etiology and the other is for the manifestation of the disease. Additional situations requiring more than one code are related to sequelae, complications, and obstetrical cases.
Some single conditions may require more than one code for a full description. Generally, one code is for the etiology and the other is for the manifestation of the disease. Additional situations requiring more than one code are related to sequelae, complications, and obstetrical cases.
![]() When a condition is described as both acute and chronic, code both and sequence the acute code first.
When a condition is described as both acute and chronic, code both and sequence the acute code first.
Example: Acute sinusitis is J01.90. Chronic sinusitis is J32.9. Both codes would be used for a diagnostic statement of “Acute and chronic sinusitis.”
![]() Combination codes are single codes used for a combination of two diagnoses, or a diagnosis with an associated manifestation or complication. Do not use multiple codes if a combination code describes all of the elements.
Combination codes are single codes used for a combination of two diagnoses, or a diagnosis with an associated manifestation or complication. Do not use multiple codes if a combination code describes all of the elements.
Example: Acute cholecystitis is K81.0. Chronic cholecystitis is K81.1. Acute cholecystitis with chronic cholecystitis is K81.2. Only K81.2 would be used to describe both.
![]() A sequela, or late effect, is the residual effect after the acute phase of an illness or injury has terminated. There is no time limit as to when a sequela code can be used. The condition or nature of the sequela is coded first, and the sequela code second.
A sequela, or late effect, is the residual effect after the acute phase of an illness or injury has terminated. There is no time limit as to when a sequela code can be used. The condition or nature of the sequela is coded first, and the sequela code second.
What Is the Structure of the Diagnosis Codes?
How is the diagnosis system set up to handle the thousands of coding categories in a logical fashion? The 21 chapters in the Classification of Diseases and Injuries are divided along two major schemes:
1. Anatomic system chapters, such as “Diseases of the Digestive System”
2. Disease or condition categories, such as the “Neoplasms” chapter, where all neoplasms are found, regardless of anatomic location
Chapter Title |
Code Range |
1. Certain Infectious and Parasitic Diseases |
A00–B99 |
2. Neoplasms |
C00–D49 |
3. Diseases of the Blood and Blood-Forming Organs and Certain Disorders Involving the Immune Mechanism |
D50–D89 |
4. Endocrine, Nutritional, and Metabolic Diseases |
E00–E89 |
5. Mental, Behavioral, and Neurodevelopmental Disorders |
F01–F99 |
6. Diseases of the Nervous System |
G00–G99 |
7. Diseases of the Eye and Adnexa |
H00–H59 |
8. Diseases of the Ear and Mastoid Process |
H60–H95 |
9. Diseases of the Circulatory System |
I00–I99 |
10. Diseases of the Respiratory System |
J00–J99 |
11. Diseases of the Digestive System |
K00–K95 |
12. Diseases of the Skin and Subcutaneous Tissue |
L00–L99 |
13. Diseases of the Musculoskeletal System and Connective Tissue |
M00–M99 |
14. Diseases of the Genitourinary System |
N00–N99 |
15. Pregnancy, Childbirth, and the Puerperium |
O00–O9A |
16. Certain Conditions Originating in the Perinatal Period |
P00–P96 |
17. Congenital Malformations, Deformations, and Chromosomal Abnormalities |
Q00–Q99 |
18. Symptoms, Signs, and Abnormal Clinical and Laboratory Findings, Not Elsewhere Classified |
R00–R99 |
19. Injury, Poisoning, and Certain Other Consequences of External Causes |
S00–T88 |
20. External Causes of Morbidity |
V00–Y99 |
21. Factors Influencing Health Status and Contact with Health Services |
Z00–Z99 |
Within each ICD-10-CM chapter and section, there are categories that are arranged in a mostly logical fashion, either by body site or by the cause or etiology. Subcategories are arranged the same way, with a fourth character of “8” generally used to indicate some “other” specified condition, and the fourth character “9” usually reserved for unspecified conditions.
Which Diagnosis Is Listed First?
The sequencing of diagnosis codes is intimately linked to reimbursement, and thus is also defined by official rules.
INPATIENT
The Uniform Hospital Discharge Data Set, or UHDDS, applies to diagnosis sequencing for all non-outpatient settings (inpatient, short-term care, acute care, psychiatric, and long-term care hospitals; home health agencies; rehab facilities; and nursing homes). It has been in use since 1985 and defines the principal diagnosis as “that condition established after study to be chiefly responsible for occasioning the admission of the patient to the hospital for care” (“1984 Revision,” 1985). According to this definition, if you are admitted to the hospital because of chest pain but fall out of bed and break your hip, the chest pain will still be your principal diagnosis, even if you end up staying an extra 2 weeks to have your hip repaired.
The sequencing rules for inpatients are found in Sections II and III.
![]() Do not use a symptom or sign as the principal diagnosis if a definitive diagnosis has been established.
Do not use a symptom or sign as the principal diagnosis if a definitive diagnosis has been established.
![]() If there are two or more interrelated conditions that could each meet the definition of principal diagnosis, either may be sequenced first.
If there are two or more interrelated conditions that could each meet the definition of principal diagnosis, either may be sequenced first.
![]() Comparative/contrasting conditions documented as “either/or” are sequenced according to the circumstances of the admission.
Comparative/contrasting conditions documented as “either/or” are sequenced according to the circumstances of the admission.
![]() If a symptom is followed by comparative/contrasting conditions, all are coded, with the symptom first. However, if the symptom is integral to the conditions listed, no code for the symptom is reported.
If a symptom is followed by comparative/contrasting conditions, all are coded, with the symptom first. However, if the symptom is integral to the conditions listed, no code for the symptom is reported.
![]() Even if the original treatment plan is not carried out, follow the definition for principal diagnosis.
Even if the original treatment plan is not carried out, follow the definition for principal diagnosis.
![]() If admission is for treatment of a complication, the complication code is sequenced first.
If admission is for treatment of a complication, the complication code is sequenced first.
![]() If a patient is admitted for inpatient care after outpatient surgery at the same hospital, and if the reason for admission is a complication, that code would be sequenced first. If the admission is for another condition unrelated to the surgery, the unrelated condition goes first. If no complication or other condition is documented as responsible for the admission, use the reason for the outpatient surgery as the principal diagnosis.
If a patient is admitted for inpatient care after outpatient surgery at the same hospital, and if the reason for admission is a complication, that code would be sequenced first. If the admission is for another condition unrelated to the surgery, the unrelated condition goes first. If no complication or other condition is documented as responsible for the admission, use the reason for the outpatient surgery as the principal diagnosis.
![]() When the admission is for rehab, use the condition for which the service is being performed as the principal diagnosis. If that condition is no longer present, such as in a patient who is being admitted after a hip replacement, use the appropriate aftercare code as the principal diagnosis.
When the admission is for rehab, use the condition for which the service is being performed as the principal diagnosis. If that condition is no longer present, such as in a patient who is being admitted after a hip replacement, use the appropriate aftercare code as the principal diagnosis.
![]() If the diagnosis is documented as “probable,” “suspected,” “likely,” “questionable,” “possible,” or “rule out,” the condition is coded as if it existed. Note that this rule varies significantly from that for outpatients (see the following section).
If the diagnosis is documented as “probable,” “suspected,” “likely,” “questionable,” “possible,” or “rule out,” the condition is coded as if it existed. Note that this rule varies significantly from that for outpatients (see the following section).
OUTPATIENT AND PHYSICIAN OFFICE
Because the UHDDS does not apply to outpatients, the selection of the first diagnosis is governed by the ICD-10-CM official guidelines. The first-listed diagnosis is defined as “the diagnosis, condition, problem, or other reason for encounter/visit shown in the medical record to be chiefly responsible for the services provided” (National Center for Health Statistics, 2014). Additional rules for outpatient sequencing are as follows:
![]() Do not code diagnoses documented as “probable,” “suspected,” “questionable,” “rule out,” or “working diagnosis.” Rather, code the condition to the highest degree of certainty for that encounter/visit, such as signs, symptoms, abnormal test results, or other reason for the visit. Note that this rule for outpatient sequencing differs significantly from that noted previously for inpatients.
Do not code diagnoses documented as “probable,” “suspected,” “questionable,” “rule out,” or “working diagnosis.” Rather, code the condition to the highest degree of certainty for that encounter/visit, such as signs, symptoms, abnormal test results, or other reason for the visit. Note that this rule for outpatient sequencing differs significantly from that noted previously for inpatients.
![]() For patients receiving diagnostic services only, sequence first the diagnosis, condition, problem, or other reason shown to be responsible for the service. For encounters for routine laboratory/radiology testing in the absence of any signs, symptoms, or associated diagnoses, assign code Z01.89. If routine testing is performed during the same encounter as a test to evaluate a sign, symptom, or diagnosis, it is appropriate to assign both the Z code and the code describing the reason for the nonroutine test. For outpatient encounters for diagnostic tests that have been interpreted by a physician and the final report is available at the time of coding, code any confirmed or definitive diagnoses documented in the interpretation.
For patients receiving diagnostic services only, sequence first the diagnosis, condition, problem, or other reason shown to be responsible for the service. For encounters for routine laboratory/radiology testing in the absence of any signs, symptoms, or associated diagnoses, assign code Z01.89. If routine testing is performed during the same encounter as a test to evaluate a sign, symptom, or diagnosis, it is appropriate to assign both the Z code and the code describing the reason for the nonroutine test. For outpatient encounters for diagnostic tests that have been interpreted by a physician and the final report is available at the time of coding, code any confirmed or definitive diagnoses documented in the interpretation.
![]() For patients receiving therapeutic services only, code first the diagnosis responsible for the service. An exception to this rule occurs if the encounter is for chemotherapy or radiation therapy, in which case the Z code for the service is listed first and the diagnosis second.
For patients receiving therapeutic services only, code first the diagnosis responsible for the service. An exception to this rule occurs if the encounter is for chemotherapy or radiation therapy, in which case the Z code for the service is listed first and the diagnosis second.
![]() For pre-op exams, use the appropriate Z code, followed by the condition necessitating the surgery and any findings related to the pre-op evaluation.
For pre-op exams, use the appropriate Z code, followed by the condition necessitating the surgery and any findings related to the pre-op evaluation.
![]() For ambulatory surgery, use the diagnosis for which the surgery was performed. If the post-op diagnosis differs from the pre-op, select the post-op for coding.
For ambulatory surgery, use the diagnosis for which the surgery was performed. If the post-op diagnosis differs from the pre-op, select the post-op for coding.
![]() For routine prenatal visits when no complications are present, use the Z34 code for supervision of pregnancy. If the pregnancy is high-risk, a code from category O09 should be used.
For routine prenatal visits when no complications are present, use the Z34 code for supervision of pregnancy. If the pregnancy is high-risk, a code from category O09 should be used.
![]() Encounters for general medical examinations should be coded according to whether abnormal findings resulted; a code for the finding should be used as an additional diagnosis.
Encounters for general medical examinations should be coded according to whether abnormal findings resulted; a code for the finding should be used as an additional diagnosis.
What’s in Each Diagnosis Chapter?
As each ICD-10-CM diagnosis chapter is discussed, any applicable coding rules from the official guidelines will be included.
CHAPTER 1: CERTAIN INFECTIOUS AND PARASITIC DISEASES (A00–B99)
The diseases in this chapter are those considered to be communicable, either from human to human or from another host, such as a mosquito, to humans. Parasites are organisms that live in or feed on humans, such as worms. This chapter is the realm of public health departments across the nation that monitor and try to prevent outbreaks of communicable diseases.
The structure of this chapter is based primarily on the organism causing the condition to be coded, but it can also be grouped according to the primary body system affected. An example is the intestinal infectious diseases section (A00–A09), which includes cholera, typhoid, salmonella, shigellosis, food poisoning, and other intestinal infections. As new organisms are identified and new outbreaks of infectious diseases occur, additional codes are added to this chapter. Some of the conditions in this chapter represent diseases thought to be eradicated, such as smallpox. The last known case was in 1977. However, small quantities of the virus exist in research laboratories, and the potential for accidental exposure is still present, so it is necessary to retain the code for possible future use. For some conditions, vaccines have been developed for prevention but the diseases continue to occur in other age groups where many individuals have not been vaccinated. An example is whooping cough in adults.
In some coding categories, lots of detailed codes are available but the usual medical record documentation is too scanty to allow their use. An example from this chapter is tuberculosis. In ICD-9-CM, fifth-digit code assignment was based on the method by which the mycobacterium infection was confirmed (i.e., microscopy, bacterial culture, histological examination). This information was almost never readily available; in ICD-10-CM the classification of tuberculosis is based solely on the organs involved.
Specific official coding guidelines for conditions in this chapter include the following:
HIV (Human Immunodeficiency Virus Infections)
Seven code categories are available to describe HIV situations:
B20 |
HIV disease (includes AIDS) |
O98.7_ |
HIV disease complicating pregnancy, childbirth, and the puerperium |
Z21 |
Asymptomatic HIV infection status |
R75 |
Inconclusive laboratory evidence of HIV |
Z20.6 |
Exposure to HIV |
Z11.4 |
Encounter for HIV screening |
Z71.7 |
HIV counseling |
The physician’s diagnostic statement that the patient is HIV positive or has an HIV-related illness is sufficient to code. Current documentation of positive serology or culture is not required.
HIV (Human Immunodeficiency Virus Infections)
Reason for Encounter |
Use Codes |
Treatment of HIV-related condition, AIDS |
B20 plus additional codes for HIV-related conditions |
Treatment of unrelated condition, such as an injury |
Code for unrelated condition plus B20, plus codes for HIV-related conditions |
Patient is “HIV-positive” without symptoms |
Z21 |
Inconclusive HIV serology, no definitive diagnosis and no manifestations |
R75 |
Previously diagnosed HIV-related illness; once the patient has developed an HIV-related illness, he or she should always be assigned to B20, never R75 or Z21 |
B20 |
HIV infection in pregnancy Note: Codes from Chapter 15 always take sequencing priority |
O98.7_ plus B20, plus codes for HIV-related conditions |
Asymptomatic HIV during pregnancy |
O98.7_ plus Z21 |
HIV testing |
Z11.4 |
Receive results of HIV testing if results are negative Note: If results are positive, see previous guidelines above |
Z71.7 |
Source: Data from International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM), 2014. Centers for Medicare and Medicaid Services and the National Center for Health Statistics. Available at http://www.cdc.gov/nchs/data/icd/icd10cm_guidelines_2014.pdf.
Sepsis, Severe Sepsis, and Septic Shock
Sepsis is an illness in which the body has a severe response to bacteria or other germs. This response may be called systemic inflammatory response syndrome (SIRS). Septic shock refers to circulatory failure associated with severe sepsis.
Sepsis, Severe Sepsis, and Septic Shock
Reason for Encounter |
Use Code |
Urosepsis |
This is a nonspecific term with no default code. The provider must be queried for clarification if this term is used. |
Bacteremia/septicemia (bacteria in blood) without documented sepsis diagnosis |
Use R78.81. |
Sepsis |
Code for underlying systemic infection, or A41.9 if organism not specified. |
Severe sepsis (sepsis with organ dysfunction) |
Code for underlying systemic infection plus a code from R65.2_ denoting severe sepsis, plus codes for the associated acute organ dysfunctions. |
Septic shock (severe sepsis with circulatory failure) |
Code for systemic infection plus R65.21, plus codes for other acute organ dysfunctions. |
Sepsis or septic shock due to a postprocedural infection |
T81.4, infection following a procedure or O86.0, infection of obstetrical surgical wound, is coded first, plus the code for the specific infection and any acute organ dysfunctions. |
Source: Data from International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM), 2014. Centers for Medicare and Medicaid Services and the National Center for Health Statistics. Available at http://www.cdc.gov/nchs/data/icd/icd10cm_guidelines_2014.pdf.
Infections Resistant to Antibiotics
Related to the infectious disease codes are the Z16 codes for infection with antimicrobial-resistant organisms, which would be used as additional codes secondary to the infection code. In some cases, the infection codes themselves include resistance, such as A41.02, infection due to methicillin-resistant Staphylococcus aureus (MRSA), in which case a Z16 code would not be used.
CHAPTER 2: NEOPLASMS (Coo–D49)
The word neoplasm means “new growth.” From a coding perspective, there are four types of neoplasms:
![]() Malignant: In common usage, the term cancer is used to describe a malignant neoplasm. These new growths are usually invasive, spreading to the lymph system and to distant sites in the body (metastases).
Malignant: In common usage, the term cancer is used to describe a malignant neoplasm. These new growths are usually invasive, spreading to the lymph system and to distant sites in the body (metastases).
![]() Primary: Malignant neoplasm in the site where it originated
Primary: Malignant neoplasm in the site where it originated
![]() Secondary: Malignant neoplasm in the site it has metastasized to, or spread to
Secondary: Malignant neoplasm in the site it has metastasized to, or spread to
![]() In situ: Carcinoma cells that are still confined to the original site and are undergoing malignant changes
In situ: Carcinoma cells that are still confined to the original site and are undergoing malignant changes
![]() Benign: Although benign neoplasms do not spread to other sites, their growth may cause problems due to size, putting extra pressure on nearby structures. Some benign neoplasms, such as adenomatous polyps of the colon, are classified as benign but are considered “precancerous,” requiring ongoing monitoring.
Benign: Although benign neoplasms do not spread to other sites, their growth may cause problems due to size, putting extra pressure on nearby structures. Some benign neoplasms, such as adenomatous polyps of the colon, are classified as benign but are considered “precancerous,” requiring ongoing monitoring.
![]() Uncertain behavior: For some tumors, a decision cannot be made about whether they are benign or malignant, even upon pathology examination.
Uncertain behavior: For some tumors, a decision cannot be made about whether they are benign or malignant, even upon pathology examination.
![]() Unspecified nature: This category is for neoplasm documentation that is not specific enough to determine the behavior.
Unspecified nature: This category is for neoplasm documentation that is not specific enough to determine the behavior.
Specific official coding guidelines for conditions in this chapter include the following.
Neoplasms
Reason for Encounter |
Use Code |
Treatment of the primary malignancy (not chemo or radiation) |
Code for malignant neoplasm of primary site |
Treatment of a secondary (metastatic) site only |
Code for malignant neoplasm of secondary site |
Treatment of anemia associated with malignancy |
Code for malignancy plus code for anemia |
Treatment of anemia associated with chemotherapy, immunotherapy, or radiation therapy |
Code for anemia plus code for neoplasm, plus code for the adverse effect |
Treatment of dehydration due to malignancy or therapy |
Code for dehydration plus code for malignancy |
Treatment of complication of surgery |
Code for complication |
Treatment of pathological fracture due to neoplasm |
Code for fracture plus code for neoplasm |
Chemotherapy |
Z51.11 plus code for malignancy |
Radiation therapy |
Z51.0 plus code for malignancy |
Immunotherapy |
Z51.12 plus code for malignancy |
Cancer in a pregnant patient |
Code from O9A.1_ malignant neoplasm complicating pregnancy, childbirth, or the puerperium, plus code for malignancy |
Source: Data from International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM), 2014. Centers for Medicare and Medicaid Services and the National Center for Health Statistics. Available at http://www.cdc.gov/nchs/data/icd/icd10cm_guidelines_2014.pdf.
Care must be taken when the term metastatic is used. It can mean either a primary neoplasm that is spreading, such as a laryngeal tumor that has spread to a cervical lymph node, or it can be documented by the physician to refer to the metastatic site, such as “metastatic cancer, lymph node.”
In assigning neoplasm codes, it is essential that the search begin by looking for the morphologic type (name such as carcinoma, glioma, or leiomyoma). This is necessary in order to learn whether the neoplasm is malignant, benign, or other. Once this information is in hand, the search moves to the anatomic site. ICD-10-CM, like its predecessor, contains a Neoplasm Table arranged alphabetically by anatomic site.
Neoplasm Table Sample

Source: Data from International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM), 2014. Centers for Medicare and Medicaid Services and the National Center for Health Statistics. Available at http://www.cdc.gov/nchs/data/icd/icd10cm_guidelines_2014.pdf.
The guidelines include several rules about coding based on the extent of involvement of the neoplasm:
![]() A primary malignant neoplasm that overlaps two or more contiguous sites should be classified to the subcategory .8 (overlapping lesion) unless the combination is specifically indexed elsewhere. For multiple neoplasms of the same site that are not contiguous, such as tumors in different quadrants of the same breast, codes for each site should be assigned.
A primary malignant neoplasm that overlaps two or more contiguous sites should be classified to the subcategory .8 (overlapping lesion) unless the combination is specifically indexed elsewhere. For multiple neoplasms of the same site that are not contiguous, such as tumors in different quadrants of the same breast, codes for each site should be assigned.
![]() Code C80.0, disseminated malignant neoplasm, unspecified, is for use only in those cases where the patient has advanced metastatic disease and no known primary or secondary sites are specified.
Code C80.0, disseminated malignant neoplasm, unspecified, is for use only in those cases where the patient has advanced metastatic disease and no known primary or secondary sites are specified.
![]() When a primary malignancy has been previously excised or eradicated from its site and there is no further treatment directed to that site and no evidence of any existing primary malignancy, a personal history of malignant neoplasm code from Z85 should be used.
When a primary malignancy has been previously excised or eradicated from its site and there is no further treatment directed to that site and no evidence of any existing primary malignancy, a personal history of malignant neoplasm code from Z85 should be used.
CHAPTER 3: DISEASES OF THE BLOOD AND BLOOD-FORMING ORGANS (D50–D89)
Anemia accounts for the largest portion of this chapter. In order to classify it correctly, detailed documentation is needed. Deficiency anemias can be due to blood loss, malabsorption of nutrients, or nutritional deficiencies. Hemolytic anemias, in which red cells are destroyed at an abnormal rate, can be hereditary or acquired. Aplastic anemia occurs when the bone marrow fails to produce the normal amount of blood components. The other major part of this chapter is coagulation defects—when the blood does not clot properly. The most well-known condition of this type is hemophilia. Diseases of the white blood cells, with the exception of leukemia, also are in this chapter. Leukemia is in the neoplasms chapter.
Diseases of the spleen are included in this chapter, as are complications of spleen procedures.
There are no official coding guidelines related to this chapter.
CHAPTER 4: ENDOCRINE, NUTRITIONAL, AND METABOLIC DISEASES (E00–E89)
Endocrine glands secrete hormones directly into the bloodstream. The hormones travel to target organs and often are involved with metabolism, the chemical processes that take place in living tissues that are necessary for the maintenance of the organism. A disease state in an endocrine gland can affect not only the target organ but also related systems. This is demonstrated clearly in the complications of diabetes, which can affect the kidneys, eyes, nerves, and peripheral vascular system.
The endocrine diseases are organized according to the involved endocrine gland: thyroid, pancreas, parathyroid, pituitary, thymus, adrenal, ovarian, and testicular. The nutritional deficiencies are arranged with malnutrition first, followed by the various vitamin and mineral deficiencies. The metabolic disorders follow the substance being metabolized, such as carbohydrates, proteins, lipids. Additional codes for obesity round out the chapter.
Diabetes Mellitus
Diabetes coding changed radically with the introduction of ICD-10-CM. Previously, it was categorized as insulin-dependent or non-insulin-dependent and controlled or uncontrolled. ICD-10-CM has five categories of diabetes that are then further subdivided based on the body systems involved and the complications affecting them:
E08 |
Diabetes mellitus due to an underlying condition (secondary diabetes) |
E09 |
Drug or chemical-induced diabetes mellitus (secondary diabetes) |
E10 |
Type 1 diabetes |
E11 |
Type 2 diabetes |
E13 |
Other specified diabetes mellitus |
Physician documentation of the type of diabetes is essential. It cannot be assumed that all patients on insulin are Type 1. If the type is not documented in the medical record, the default is E11, Type 2.
Diabetes Mellitus
Reason for Encounter |
Use Code |
Treatment of Type 1 diabetes (includes “brittle diabetes,” juvenile onset diabetes) |
E10._: Use as many codes from this category as needed to describe all the complications of the disease. Use Z79.4 to denote long-term (current) use of insulin. |
Treatment of Type 2 diabetes |
E11._: Use as many codes from this category as needed to describe all the complications of the disease. If the patient uses insulin on an ongoing basis, use Z79.4. |
Complications of diabetes, such as retinopathy, nephropathy, ketoacidosis, coma, ulcer |
Code to the type of diabetes and organ system involvement. |
Treatment of a secondary diabetes |
Code first the underlying condition or the drug or chemical causing the diabetes, then the E08, E09, or E13 codes for the type of diabetes and organ involvement. If the patient uses insulin on an ongoing basis, use Z79.4. |
Dietary counseling |
Z71.3 plus code for diabetes. |
Preexisting diabetes in pregnancy |
O24.0_ or O24.1_: Code is based on the type of diabetes and trimester of pregnancy or childbirth or puerperium. |
Gestational diabetes |
O24.4_: Code based on trimester of pregnancy or childbirth or puerperium. |
Source: Data from International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM), 2014. Centers for Medicare and Medicaid Services and the National Center for Health Statistics. Available at http://www.cdc.gov/nchs/data/icd/icd10cm_guidelines_2014.pdf.
A potentially problematic diagnosis category in this chapter is thyroid disorders (E00–E07). If the physician does not enunciate clearly or spell the words when dictating, you could end up with the wrong disease. “Hypothyroidism” and “hyperthyroidism” sound very similar to voice-recognition systems.
CHAPTER 5: MENTAL, BEHAVIORAL, AND NEURODEVELOPMENTAL DISORDERS (F01–F99)
The American Psychiatric Association (APA) has defined a mental disorder as “a syndrome characterized by clinically significant disturbance in an individual’s cognition, emotional regulation or behavior that reflects a dysfunction in the psychological, biological or developmental processes underlying mental functioning” (Maisel, 2013). The APA’s Diagnostic and Statistical Manual of Mental Disorders, 5th edition (known as DSM-5) is a tool to assist clinicians in the diagnosis of mental disorders. It consists of an index of mental illnesses accompanied by listings of possible symptoms and diagnostic criteria. This classification is not used for healthcare billing purposes. In many cases, the clinician uses the DSM criteria to arrive at a DSM diagnosis that is then cross-walked to an ICD-10-CM diagnosis code.
More than other specialties, psychiatry is likely to have codeable services that are rendered by providers other than physicians. Clinical psychologists, counselors, social workers, and therapists participate in services for psychiatric patients. Psychiatry is also heavily involved with the legal system because of the need for involuntary treatment of some patients and the use of mental illness as a defense in legal cases.
ICD-10-CM includes some new terminology in this chapter. Mental retardation is now known as “intellectual disabilities.” Stuttering has the new title of “childhood onset fluency disorder.” Areas where DSM-5 and ICD-10-CM are no longer in sync include “autism spectrum disorder.” In DSM-5, this new diagnostic entity encompasses autistic disorder, Asperger’s disorder, childhood disintegrative disorder, and pervasive developmental disorder, which are all still separate in ICD-10-CM.
Official coding guidelines for this chapter include the following:
![]() Pain that is exclusively related to psychological disorders should be coded using F45.41. Code F45.42, pain disorders with related psychological factors, should be used along with a code from category G89, pain, if there is documentation of a psychological component for a patient with acute or chronic pain.
Pain that is exclusively related to psychological disorders should be coded using F45.41. Code F45.42, pain disorders with related psychological factors, should be used along with a code from category G89, pain, if there is documentation of a psychological component for a patient with acute or chronic pain.
![]() The section on mental and behavioral disorders due to psychoactive substance use includes coding categories of use, abuse, and dependence for various substances. If provider documentation refers to more than one pattern of use, the following hierarchy should be used to assign the code.
The section on mental and behavioral disorders due to psychoactive substance use includes coding categories of use, abuse, and dependence for various substances. If provider documentation refers to more than one pattern of use, the following hierarchy should be used to assign the code.
Use, Abuse, and Dependence
Documented |
Assign Only the Code For |
Use and abuse |
Abuse |
Abuse and dependence |
Dependence |
Use and dependence |
Dependence |
Use, abuse, and dependence |
Dependence |
Source: Data from International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM), 2014. Centers for Medicare and Medicaid Services and the National Center for Health Statistics. Available at http://www.cdc.gov/nchs/data/icd/icd10cm_guidelines_2014.pdf.
Some of the dependence category codes have subdivisions for “in remission.” These codes should only be used when provider documentation of remission is present.
CHAPTER 6: DISEASES OF THE NERVOUS SYSTEM (G00–G99)
The nervous system is responsible for sensory and motor activities, for behavior, and for regulation of the internal organs. Sensory functions are those of vision, smell, hearing, taste, touch, and proprioception (the body’s awareness of itself). Motor functions are those of movements, such as swallowing and heartbeat. In ICD-10-CM, diseases of the eye and ear have been moved from the nervous system chapter to their own chapters.
Coding nervous systems conditions requires knowledge of the location or site of the condition. The central nervous system is the brain and the spinal cord. The peripheral nervous system includes all other nervous system elements, such as the facial nerves, cranial nerves, and nerves in the extremities.
Central nervous system diseases include infections, such as encephalitis and meningitis, and degenerative disorders, such as Alzheimer’s disease, Parkinson’s disease, and other types of tremor. Some of these diseases are hereditary and some are acquired. Multiple sclerosis, cerebral palsy, migraine, and epilepsy are other central nervous system conditions.
The hemiplegia (paralysis of one side of the body) and monoplegia (paralysis of one upper or lower limb) codes in this chapter (G81 and G83.1–G83.3) are intended for use only when the condition is reported without further specification or is stated to be old or longstanding but of unspecified cause. A fifth digit is used with these codes to indicate whether the patient’s dominant or nondominant side is affected. If the affected side is documented but not specified as dominant or nondominant, the code selection is as follows.
Hemiplegia and Monoplegia
Side Affected |
Default |
Ambidextrous |
Dominant |
Left side |
Nondominant |
Right side |
Dominant |
Source: Data from International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM), 2014. Centers for Medicare and Medicaid Services and the National Center for Health Statistics. Available at http://www.cdc.gov/nchs/data/icd/icd10cm_guidelines_2014.pdf.
The peripheral nervous system is involved in many common conditions, such as carpal tunnel syndrome, peripheral neuropathy, Bell’s palsy, and hereditary conditions such as muscular dystrophy.
Most of the official guidelines for this chapter are related to pain coding. Category G89, pain, not elsewhere classified, has subcategories defining central pain syndromes, acute pain, chronic pain, neoplasm-related pain, and chronic pain syndrome. A code from this section should not be assigned if the underlying diagnosis is known, unless the reason for the encounter is for pain control/management, and not management of the underlying condition.
Pain
Reason for Encounter |
Use Codes |
Pain control or management |
Code from G89 plus code for underlying cause and site of the pain |
Post-op pain not associated with a specific complication |
G89 |
Pain associated with a specific post-op complication |
Code from Chapter 19 plus additional code for acute or chronic pain, G89.18 or G89.28 |
Insertion of neurostimulator for pain control |
Code from G89 |
Treatment of underlying condition and neurostimulator is inserted for pain control during same encounter |
Code for underlying condition plus pain code from G89 |
Treatment of underlying condition only |
Code for underlying condition |
Treatment of chronic pain |
Code for chronic pain—no time limit to define when it becomes chronic. Do not use codes for chronic pain syndrome or central pain syndrome unless documented as such |
Treatment of neoplasm-related pain |
Code G89.3 plus code for underlying neoplasm |
Treatment of neoplasm and pain is also documented |
Code for neoplasm plus code G89.3 |
Source: Data from International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM), 2014. Centers for Medicare and Medicaid Services and the National Center for Health Statistics. Available at http://www.cdc.gov/nchs/data/icd/icd10cm_guidelines_2014.pdf.
CHAPTER 7: DISEASES OF THE EYE AND ADNEXA (H00–H59)
This brand-new chapter includes diseases of the eye, visual disturbances, glaucoma, disorders of the optic nerve and visual pathway, disorders of the ocular muscles, blindness, and complications of eye procedures. Many codes in this chapter have subdivisions for left eye, right eye, bilateral eyes, and unspecified laterality. If no bilateral code is available and the condition is bilateral, assign codes for both the right and left sides. If the laterality is not documented, use the “unspecified” code.
The official guidelines for Chapter 7 are all related to glaucoma coding. Most glaucoma categories define the type of glaucoma, the laterality, and the stage of the disease (i.e., mild, moderate, severe, indeterminate, and unspecified).
![]() Use as many codes from category H40 as needed to fully identify the glaucoma.
Use as many codes from category H40 as needed to fully identify the glaucoma.
![]() If the patient has bilateral glaucoma and both eyes are the same type and stage, assign only one code, for bilateral. If the patient has bilateral glaucoma of the same type and stage and the code does not include a bilateral option, assign only one code for the type and stage.
If the patient has bilateral glaucoma and both eyes are the same type and stage, assign only one code, for bilateral. If the patient has bilateral glaucoma of the same type and stage and the code does not include a bilateral option, assign only one code for the type and stage.
![]() If the patient has bilateral glaucoma and each eye is different and the category includes laterality codes, assign an individual code for each eye based on its characteristics.
If the patient has bilateral glaucoma and each eye is different and the category includes laterality codes, assign an individual code for each eye based on its characteristics.
![]() If the patient is admitted with glaucoma and the stage progresses during the admission, assign the code for the highest stage.
If the patient is admitted with glaucoma and the stage progresses during the admission, assign the code for the highest stage.
![]() “Indeterminate stage” is used when there is documentation that the stage cannot be determined. “Unspecified” is used when there is no documentation regarding the stage.
“Indeterminate stage” is used when there is documentation that the stage cannot be determined. “Unspecified” is used when there is no documentation regarding the stage.
CHAPTER 8: DISEASES OF THE EAR AND MASTOID PROCESS (H60–H95)
As in Chapter 7 on the eye, this chapter includes left, right, bilateral, and unspecified laterality codes. Although there are no official guidelines for this chapter, logic would dictate that the laterality guideline for the eye chapter be followed for ears. If the condition is bilateral and no bilateral code is available, use two codes for left and right. If the laterality is not documented, use unspecified.
The categories for otitis media (H65, nonsuppurative, and H66, suppurative and unspecified) include “use additional code” instructional notes to identify various types of exposure to tobacco smoke. In addition, allergic otitis media is separately identified and subdivided into acute and subacute and chronic. Codes for perforation of the tympanic membrane are located in this chapter (H72) but it is important to note that this does not include a traumatic rupture.
CHAPTER 9: DISEASES OF THE CIRCULATORY SYSTEM (I00–I99)
The circulatory system encompasses the heart, arteries, veins, and capillaries. Its purpose is to obtain oxygen from the lungs, distribute it to tissues via blood flow, and release carbon dioxide, the waste product of the body’s metabolism or energy consumption. The heart is the pump that makes the circulatory system work.
The lymph system, which produces and distributes immune cells, is also included in this chapter. Congenital heart conditions are found in Chapter 17, whereas circulatory conditions related to pregnancy are in Chapter 15.
Interestingly, this chapter starts with an infectious disease. Rheumatic fever is a febrile inflammatory condition that may occur after infection with group A strep. It can cause arthritis and other joint symptoms, but its primary complication is carditis and damage to the heart, particularly the valves.
Hypertension, or high blood pressure, is defined as blood pressure consistently greater than 140 mm Hg systolic or 90 mm Hg diastolic. Systolic is the top number in your blood pressure and represents the pressure when the heart beats. Diastolic is the bottom number and represents the pressure when the heart rests. In ICD-9-CM, hypertension was categorized as benign, malignant, or unspecified; in ICD-10-CM, it is either essential (primary) or secondary, with additional code categories to define heart and/or kidney disease due to hypertension.
Heart attack, or myocardial infarction (MI), is another group of codes in this chapter. It is a form of ischemic heart disease, in which the supply of blood to the heart is blocked, usually due to arteriosclerosis. Distinctions are made between “STEMI” and “non-STEMI” myocardial infarctions, based on ECG patterns. An ECG (electrocardiogram) translates the electrical activity of the heart into line tracings. Points on the line are known by the initials P, Q, R, S, and T. The ST segment represents the period when the ventricle of the heart is contracting but no electricity is flowing through it (Figure 2-5). STEMI stands for “ST elevation myocardial infarction,” in which a coronary artery is blocked, causing damage to the heart muscle supplied by the artery. This causes a characteristic elevation in the ST segment of the ECG, hence the name. In a non-STEMI, or NSTEMI, the artery is partially or temporarily blocked, resulting in less damage and no ST elevation.
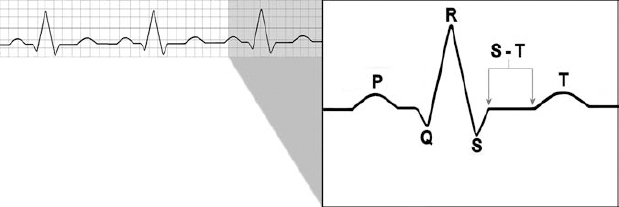
FIGURE 2-5 EKG S-T segment.
Varicose veins, thrombophlebitis, hemorrhoids, and deep vein thrombosis are the most commonly seen conditions of the arteries and veins.
This chapter has a number of official coding rules.
Circulatory System
Reason for Encounter |
Use Code |
Hypertension with heart disease—causal relationship stated (due to hypertension) or implied (hypertensive) |
I11: Hypertensive heart disease. Use additional code from I50 to identify the type of heart failure, if present. |
Hypertension with heart disease—causal relationship not documented |
Code heart disease and hypertension separately. Sequence according to the circumstances of the encounter. |
Hypertensive renal disease with chronic renal failure |
Assign a code from category I12. ICD-10-CM assumes a causal relationship is present. Use additional code from N18 to identify the stage of chronic kidney disease. |
Hypertensive heart and renal disease—causal statement for heart disease present |
Category I13. Use an additional code from I50 if the patient has heart failure and a code from N18 to identify the stage of chronic kidney disease. |
Hypertensive cerebrovascular disease |
Code from I60–I69 plus hypertension code. |
Hypertensive retinopathy |
H35.0 plus code from I10–I15. |
Secondary hypertension |
Code for underlying cause and code from I15 for hypertension. Sequence according to the circumstances of the admission. |
Transient hypertension, or elevated blood pressure without hypertension diagnosis |
R03.0: Elevated blood pressure reading without diagnosis of hypertension. |
Hypertension stated as controlled or uncontrolled |
Appropriate code from I10–I15. |
Sequelae of cerebrovascular disease, such as neurological deficits |
Code for deficit plus code from category I69. |
Angina due to coronary artery disease |
Causal relationship is assumed in patients with both angina and atherosclerosis, unless the documentation indicates otherwise. Use combination code from I25.11_ or I25.7_. |
Acute NSTEMI evolving to STEMI during encounter |
Use code for STEMI. |
Acute STEMI converts to NSTEMI due to use of antithrombolytic |
Use code for STEMI. |
Subsequent acute STEMI or NSTEMI within 28 days of previous acute MI |
Code from I22 to describe new MI and code from I21 to indicate existing MI. Sequence according to circumstances of admission. |
Chest pain, no cause identified |
Chest pain code is R07.9. |
Chest pain, cause identified |
Code for cause. |
Cerebrovascular accident (CVA, stroke) with positive diagnostic tests and symptoms still occurring after 24 hours |
CVA code is I63_. |
Presentation as stroke/CVA but diagnostic tests are negative and symptoms are resolved within 24 hours |
TIA (transient ischemic attack) G45.9. |
Source: Data from International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM), 2014. Centers for Medicare and Medicaid Services and the National Center for Health Statistics. Available at http://www.cdc.gov/nchs/data/icd/icd10cm_guidelines_2014.pdf.
CHAPTER 10: DISEASES OF THE RESPIRATORY SYSTEM (J00–J99)
Starting at the top, the respiratory system consists of the nasal cavity and sinuses, the mouth, throat (pharynx and larynx), bronchi, and lungs. Its function is to bring in air, containing oxygen, and to release carbon dioxide. The oxygen passes into the blood in an exchange process that takes place in the alveoli of the lungs; carbon dioxide passes from the blood into the lungs and is exhaled.
The coding categories for lung diseases due to external agents read like a list of poor labor conditions from American history: coal workers’ pneumoconiosis (black lung disease), mushroom workers’ lung, farmers’ lung, cheese washers’ lung, bauxite fibrosis, and chemical bronchitis.
In ICD-10-CM, asthma is classified as mild intermittent, mild persistent, moderate persistent, or severe persistent. The definitions of these levels of severity were formulated by the National Institutes of Health (U.S. Department of Health and Human Services, 2012). If the provider does not document the level of severity, the asthma should be classified as J45.90_ unspecified.
Official coding guidelines for this chapter are as follows.
Respiratory System
Reason for Encounter |
Use Code |
Pneumonia, unspecified organism |
J18.9. |
Pneumonia, known cause. Physician must document bacterial or viral cause |
Code from J12–J16. |
Pneumonia in diseases classified elsewhere |
Code for underlying disease (read “Excludes I” note), then J17. |
Lobar pneumonia (the same term is sometimes used for two different diseases) |
J18.1 for lobar pneumonia, unspecified organism, for site (lobe). J13 for pneumococcal (lobar is synonym). |
Chronic obstructive pulmonary disease (COPD) with acute exacerbation (worsening or decompensation), cause not identified |
J44.1. |
COPD with acute lower respiratory infection |
J44.0 plus additional code to identify infection. |
COPD with asthma |
COPD code plus code from category J45 to identify type of asthma. |
Acute respiratory failure |
Acute respiratory failure (J96.0) or acute and chronic respiratory failure (J96.2) may be listed as a principal diagnosis if appropriate, or as a secondary diagnosis if it occurs after admission or is present on admission but does not meet the criteria for principal diagnosis. |
Asthma; the physician must document the level of severity and whether acute exacerbation or status asthmaticus is present |
J45_. |
Ventilator-associated pneumonia (VAP) |
Assign J95.851 only when the provider has documented VAP. Should not be assigned when the patient has pneumonia and is on a ventilator and the provider has not stated it is VAP. |
Source: Data from International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM), 2014. Centers for Medicare and Medicaid Services and the National Center for Health Statistics. Available at http://www.cdc.gov/nchs/data/icd/icd10cm_guidelines_2014.pdf.
CHAPTER 11: DISEASES OF THE DIGESTIVE SYSTEM (K00–K94)
The length of the average digestive system is an amazing 27 to 28 feet! The basic function of this system is to prepare food for absorption by mechanical and chemical methods. In mechanical digestion, food is ground, torn, chewed, shaken, and mixed with saliva and stomach juices. In the small intestine, the dissolved food particles are mixed with enzymes and are absorbed through the lining of the intestine into the intestinal–hepatic portal venous system where nutrients move into the bloodstream and then are delivered to the rest of the body.
Coding categories for the digestive system are arranged according to the physical site of the disease: teeth, gums, jaw, salivary glands, oral soft tissues, tongue, esophagus, stomach, duodenum, appendix, abdominal cavity, intestine, colon, rectum, anus, liver, gallbladder, and pancreas. The pancreas serves an endocrine function by producing insulin, but it is also considered a digestive organ because it secretes enzymes that aid in digestion of proteins, fats, and carbohydrates.
Gastrointestinal infections that are contagious are located in the infectious disease chapter; gastrointestinal neoplasms are located in Chapter 2. Conditions of the jaw have been moved to the musculoskeletal diseases in Chapter 13.
There are no official coding guidelines for the digestive system disease chapter.
Some digestive conditions will require more provider documentation to code accurately in ICD-10-CM. For example, hemorrhoids are now coded according to stage:
![]() First degree: Hemorrhoids (bleeding) without prolapse outside anal canal
First degree: Hemorrhoids (bleeding) without prolapse outside anal canal
![]() Second degree: Hemorrhoids (bleeding) that prolapse with straining but retract spontaneously
Second degree: Hemorrhoids (bleeding) that prolapse with straining but retract spontaneously
![]() Third degree: Hemorrhoids (bleeding) that prolapse with straining and require manual replacement inside anal canal
Third degree: Hemorrhoids (bleeding) that prolapse with straining and require manual replacement inside anal canal
![]() Fourth degree: Hemorrhoids (bleeding) with prolapsed tissue that cannot be manually replaced
Fourth degree: Hemorrhoids (bleeding) with prolapsed tissue that cannot be manually replaced
The term bleeding is in parentheses, indicating that it is a nonessential modifier, so the bleeding can be present or absent.
Ulcers are classified according to site (i.e., duodenal, gastric) by acute, chronic, or unspecified, and by the presence or absence of hemorrhage and/or perforation.
One of the common conditions in the gastrointestinal (GI) tract is bleeding. If the cause of the bleeding is identified, the code for that condition, with hemorrhage, is used. The code for gastrointestinal hemorrhage, K92.2, is used only when the bleeding is documented but no bleeding site or cause is identified. The most common causes of GI bleeding are ulcers and diverticular disease.
CHAPTER 12: DISEASES OF THE SKIN AND SUBCUTANEOUS TISSUE (L00–L99)
The skin is part of what is known as the integument. This protective covering keeps the deeper tissues from drying out and protects them from injury and infection. The epidermis is the outer layer. It contains nerve endings, hair shafts, sweat gland openings, and several layers of cells. As old cells are worn away, they are replaced. The dermis is the next layer, consisting of hair follicles, sebaceous glands, sweat glands, nerves, arteries, veins, and connective tissue. The superficial fascia is the deepest layer of integument. It is the layer between the skin and the muscle or bone. In addition to the hair follicles and sebaceous and sweat glands, the nails are an important appendage to the skin. They grow through proliferation of cells at their roots, pushing the new nail growth out. Coding for skin conditions is divided into categories for infections, inflammatory conditions, and other diseases.
This chapter has a few differences from the regular coding schemes. Sunburn is in this chapter, not in the injury chapter that contains other types of burns. A number of skin infections, despite the fact that they may be contagious, such as impetigo, are in this chapter instead of Chapter 1 of ICD-10-CM. Acute lymphadenitis is in this chapter, while chronic lymphadenitis is in the circulatory chapter.
A common skin condition among those with limited mobility, particularly the elderly, is the ulcer. Decubitus ulcers, also known as pressure ulcers or bedsores, result from pressure on skin points from the patient’s body weight and the resulting lack of blood circulation. Other types of skin ulcers can result from hypertension, diabetes, or phlebitis, an inflammation of the veins.
All of the official guidelines for this chapter are related to pressure ulcers:
![]() Pressure ulcers are classified in ICD-10-CM according to a sixth digit describing severity:
Pressure ulcers are classified in ICD-10-CM according to a sixth digit describing severity:
1—Stage 1: Skin changes limited to erythema only
2—Stage 2: Pressure ulcer with abrasion, blister, partial thickness skin loss involving epidermis and dermis
3—Stage 3: Pressure ulcer with full thickness skin loss involving damage or necrosis of subcutaneous tissue extending to underlying fascia
4—Stage 4: Pressure ulcer with necrosis of muscle, bone, and supporting structures (tendon or joint capsule)
0—Unstageable: Pressure ulcer whose stage cannot be clinically determined (covered by eschar or treated with skin or muscle graft, or documented as deep tissue injury but not due to trauma)
The stages defined in ICD-10-CM are aligned with those defined by the National Pressure Ulcer Advisory Panel in 2007 (NPUAP, n.d.).
An additional sixth digit (9) is used for unspecified stage. When there is no documentation regarding the stage of the ulcer, assign the code for unspecified stage.
Note that according to section 1.B.14 of the official guidelines the documentation of ulcer stage may be done by a clinician who is not the patient’s attending provider.
![]() No ulcer code is assigned if the patient is admitted with an ulcer documented as completely healed.
No ulcer code is assigned if the patient is admitted with an ulcer documented as completely healed.
![]() Ulcers documented as healing should be coded with the appropriate stage based on documentation.
Ulcers documented as healing should be coded with the appropriate stage based on documentation.
![]() If a pressure ulcer progresses to a higher stage during an encounter, assign the code for the highest stage reported for that site.
If a pressure ulcer progresses to a higher stage during an encounter, assign the code for the highest stage reported for that site.
Nonpressure chronic ulcers are classified to category L97. They include chronic ulcer of skin, nonhealing ulcer of skin, trophic ulcer of skin, tropical ulcer of skin, noninfected sinus of skin, and ulcer of skin, not otherwise specified. The severity classification of nonpressure chronic ulcers, represented by a sixth digit, is as follows:
1. Skin breakdown only
2. Exposed fat layer
3. Muscle necrosis
4. Bone necrosis
5. Unspecified severity
If the patient has an underlying condition contributing to the ulcers, it should be coded first. The additional code from L97 will provide better specificity about the site and depth of the ulcer.
CHAPTER 13: DISEASES OF THE MUSCULOSKELETAL SYSTEM AND CONNECTIVE TISSUE (MOO–M99)
This chapter covers the bones, joints, muscles, and fascia. The adult body contains more than 200 bones and approximately 600 muscles, so it is important to be specific in coding diseases and conditions of these systems. Because they are made primarily of mineral salts such as calcium and are more durable than other body tissues, bones are frequently the only thing left when remains must be examined in conjunction with scientific or legal investigations. The length of various individual bones can be used to estimate the height of a person, and the structure of the pelvis can be used to differentiate between male and female skeletons.
Three types of muscles produce movement within the body. Cardiac muscle in the heart wall and smooth muscle in the stomach, intestine, and blood vessels are known as involuntary muscles. They work without conscious direction from you, and you do not have conscious control over them. Your heart continues to beat without your telling it to do so; you are not able to prevent the smooth muscle in your stomach from contracting when you vomit. Skeletal muscles, those attached to the bones, are voluntary because they are under your control. Muscles make up more than 40% of your body weight.
Other parts of the musculoskeletal system are ligaments, which connect bone to bone, and tendons, which connect muscle to bone. Fascia is the covering of the muscles, and it also contains blood vessels and nerves.
Joints are points at which bones are connected to each other. The shape of the joint determines how it will be able to move:
![]() Ball and socket joints, such as the hip and shoulder joints, permit movement in basically three directions.
Ball and socket joints, such as the hip and shoulder joints, permit movement in basically three directions.
![]() Hinge joints, such as the elbow and ankle, permit movement that is mostly restricted to one plane.
Hinge joints, such as the elbow and ankle, permit movement that is mostly restricted to one plane.
![]() Pivot joints, such as the skull on the first vertebra in the neck, allow for rotation of the head from side to side.
Pivot joints, such as the skull on the first vertebra in the neck, allow for rotation of the head from side to side.
![]() Sutures between the bones of the skull are joints but are immovable after age 5.
Sutures between the bones of the skull are joints but are immovable after age 5.
![]() Cartilaginous joints, such as the discs between the vertebra, allow for only partial movement.
Cartilaginous joints, such as the discs between the vertebra, allow for only partial movement.
![]() Gliding joints occur where two flat surfaces of bone glide across each other.
Gliding joints occur where two flat surfaces of bone glide across each other.
Damage to joints, tendons, and ligaments occurs with aging, trauma, and with inappropriate use.
There are more than seven times as many codes in this chapter as there were in the same chapter in ICD-9-CM. The addition of laterality to many codes and the greater specificity of joint codes accounts for this increase.
The official coding guidelines for the musculoskeletal system chapter are as follows:
![]() For some conditions where more than one bone, joint, or muscle is usually involved, a “multiple sites” code is available. If no such code is available, multiple codes should be used to indicate the different sites involved.
For some conditions where more than one bone, joint, or muscle is usually involved, a “multiple sites” code is available. If no such code is available, multiple codes should be used to indicate the different sites involved.
![]() For certain conditions, the bone may be affected at the joint at an upper or lower end. Though the portion of the bone affected is at the joint, the site designation will be the bone, not the joint.
For certain conditions, the bone may be affected at the joint at an upper or lower end. Though the portion of the bone affected is at the joint, the site designation will be the bone, not the joint.
It is important to note that current acute bone or joint injuries are coded to the appropriate selection from Chapter 19, on injuries. If the musculoskeletal condition is the result of a previous injury or trauma or is a recurrent condition, it may be found in Chapter 13.
![]() Chapter 13 has several categories for pathological fractures:
Chapter 13 has several categories for pathological fractures:
M48.4_ Stress or fatigue fractures of vertebrae
M80.0_ Osteoporosis with current pathological fracture
M84.3_ Stress or fatigue fracture
M84.4_ Pathological fracture, NEC
M84.5_ Pathological fracture in neoplastic disease
M84.6_ Pathological fracture in other diseases
These categories require the use of a seventh character to identify the type of encounter and/or problems associated with healing:
A Initial encounter for fracture. Use this character as long as the patient is receiving active treatment for the fracture (surgical treatment, ER encounter, evaluation and treatment by new physician).
D Subsequent encounter for fracture with routine healing. To be used for encounters after the patient has completed active treatment.
G Subsequent encounter for fracture with delayed healing
K Subsequent encounter for fracture with nonunion
P Subsequent encounter for fracture with malunion
S Sequela
![]() A code from M80, not a traumatic fracture code, should be used for any patient with known osteoporosis who suffers a fracture, even if the patient had a minor fall or trauma, if that fall or trauma would not usually break a normal, healthy bone.
A code from M80, not a traumatic fracture code, should be used for any patient with known osteoporosis who suffers a fracture, even if the patient had a minor fall or trauma, if that fall or trauma would not usually break a normal, healthy bone.
CHAPTER 14: DISEASES OF THE GENITOURINARY SYSTEM (NOO–N99)
The urinary portion of this system comprises the kidneys, ureters (tubes connecting the kidneys to the bladder), bladder, and urethra (tube from bladder to the outside). Its function is to eliminate waste products and also to maintain chemical and body water balances. If it is a hot day and you do not drink enough water, the volume of your urine will decrease as the kidneys work to maintain the appropriate internal balance.
The genital portion of this system includes not only what is normally thought of as genitalia, but also the breasts. The male genital portion covers the prostate, penis, testes, spermatic cord, and seminal vesicles. The female portion includes the ovaries, fallopian tubes, uterus, vagina, cervix, clitoris, labia, and vulva. Reproduction and preservation of the human species are the tasks of these systems.
Kidney failure may lead to the need for the patient to undergo dialysis. In this procedure, a dialysis machine serves as a substitute for the kidney, filtering out salts and urea wastes into a solution that can be discarded.
The presence of stones, or calculi, can occur in the kidney, ureters, bladder, or urethra. Often painful, these stones are usually formed of calcium or uric acid. They can prevent the passage of urine if located in the wrong spot. The flow of urine can also be affected by conditions in the prostate because the urethra passes through the prostate on its way to the penis. Enlargement of the prostate is found in more than 40% of men over the age of 70. For coding purposes, the cause of the hypertrophy must be specified.
Breast disorders, with the exception of neoplasms, are also located in this chapter. They are not restricted to use in female patients. Breast neoplasms are found in Chapter 2, “Neoplasms.”
Coding for female genital tract conditions is organized along inflammatory versus noninflammatory conditions. Recurrent pregnancy loss (N96) and female infertility (N97) are also part of this chapter.
The official coding guidelines for this chapter are related to chronic kidney disease (CKD). There are individual codes for the five stages of CKD, plus an additional code for end-stage renal disease (ESRD).
![]() If both a stage of CKD and ESRD are documented, assign the code for ESRD only (N18.6).
If both a stage of CKD and ESRD are documented, assign the code for ESRD only (N18.6).
![]() 14.a.2. The presence of CKD in a patient who has undergone a kidney transplant does not automatically constitute a transplant complication. Assign the appropriate N18 code for the patient’s stage of CKD and code Z94.0 for kidney transplant status.
14.a.2. The presence of CKD in a patient who has undergone a kidney transplant does not automatically constitute a transplant complication. Assign the appropriate N18 code for the patient’s stage of CKD and code Z94.0 for kidney transplant status.
![]() CKD patients with other serious conditions, such as diabetes or hypertension, may have combination codes from those chapters as their principal or first-listed diagnosis. An N18 code should be used to indicate the stage of CKD.
CKD patients with other serious conditions, such as diabetes or hypertension, may have combination codes from those chapters as their principal or first-listed diagnosis. An N18 code should be used to indicate the stage of CKD.
CHAPTER 15: PREGNANCY, CHILDBIRTH, AND THE PUERPERIUM (OOO–O9A)
This chapter is the most complex within ICD-10-CM in terms of the official guidelines. It contains codes for many conditions that are classified elsewhere, but which are coded within this chapter if the patient is pregnant or has delivered and is within the puerperium, or postpartum period, defined as 6 weeks (42 days) after delivery. An additional term used in ICD-10-CM is the peripartum period, which is the last month of pregnancy and 5 months postpartum. General rules for obstetric cases are the following:
![]() Codes from Chapter 15 have sequencing priority over codes from other chapters. Additional codes from other chapters may be used with Chapter 15 codes to further specify conditions. If the patient is being seen for an unrelated condition and the provider documents incidental pregnancy, code Z33.1, pregnant state, incidental, should be used instead of a Chapter 15 code.
Codes from Chapter 15 have sequencing priority over codes from other chapters. Additional codes from other chapters may be used with Chapter 15 codes to further specify conditions. If the patient is being seen for an unrelated condition and the provider documents incidental pregnancy, code Z33.1, pregnant state, incidental, should be used instead of a Chapter 15 code.
![]() Codes from Chapter 15 are to be used only for coding maternal records, never newborn records.
Codes from Chapter 15 are to be used only for coding maternal records, never newborn records.
![]() Many of the codes in Chapter 15 have a final character specifying the trimester of the pregnancy:
Many of the codes in Chapter 15 have a final character specifying the trimester of the pregnancy:
First trimester: less than 14 weeks
Second trimester: 14 weeks, 0 days, to less than 28 weeks, 0 days
Third trimester: 28 weeks, 0 days, until delivery
Some codes do not have this component because the condition always appears in a specific trimester; other codes may only have trimester characters for two trimesters because that is when the condition occurs. Provider documentation of the number of weeks may be used to assign the appropriate trimester.
![]() If the patient is admitted for complications of pregnancy in one trimester and the encounter lasts into the next trimester, the code for the trimester in which the complication developed or when the admission occurred should be used, not the trimester of discharge.
If the patient is admitted for complications of pregnancy in one trimester and the encounter lasts into the next trimester, the code for the trimester in which the complication developed or when the admission occurred should be used, not the trimester of discharge.
![]() Although codes for “unspecified trimester” exist, they should only be used when it is not possible to obtain clarification of insufficient documentation in the record.
Although codes for “unspecified trimester” exist, they should only be used when it is not possible to obtain clarification of insufficient documentation in the record.
![]() Certain codes for complications require the use of a seventh character on the maternal record to identify the fetus with the condition. Assign a seventh character of “0” for single gestations or when the documentation is insufficient to determine which fetus, from multiple gestations, is affected and it is not possible to obtain clarification or when it is not clinically possible to determine which fetus is affected. If it is a multiple gestation, a seventh character 1–9 is used. A code from category O30, multiple gestation, must also be used to identify the type of multiple gestation.
Certain codes for complications require the use of a seventh character on the maternal record to identify the fetus with the condition. Assign a seventh character of “0” for single gestations or when the documentation is insufficient to determine which fetus, from multiple gestations, is affected and it is not possible to obtain clarification or when it is not clinically possible to determine which fetus is affected. If it is a multiple gestation, a seventh character 1–9 is used. A code from category O30, multiple gestation, must also be used to identify the type of multiple gestation.
Pregnancy, Childbirth, and the Puerperium
Source: Data from International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM), 2014. Centers for Medicare and Medicaid Services and the National Center for Health Statistics. Available at http://www.cdc.gov/nchs/data/icd/icd10cm_guidelines_2014.pdf.
The categories of abortion are spontaneous, termination of pregnancy, and failed attempted termination of pregnancy. Spontaneous abortions are classified as one of the following:
1 = incomplete (retained products of conception)
2 = complete (all products of conception have been expelled from the uterus)
The following official coding guidelines relate to abortion.
Abortion
Reason for Encounter |
Use Code |
Treatment of spontaneous abortion |
Category O03._. |
Elective termination of pregnancy, uncomplicated |
Z33.2. |
Treatment of complications following (induced) termination of pregnancy |
Category O04. |
Treatment after failed attempted termination of pregnancy |
Category O07. |
Complication of pregnancy leading to an abortion |
Abortion code plus additional Chapter 15 codes for complications of pregnancy. |
Attempted abortion with liveborn fetus |
Z33.2 plus Z37 outcome of delivery. |
Code from category O03, O07.4, or Z33.2. Appropriate even if the patient was discharged previously with a diagnosis of complete abortion. | |
Missed abortion (fetal death prior to 20 completed weeks, gestation, with retained fetus) |
Use code O02.1. Note the change from 22 weeks in ICD-9-CM to 20 weeks in ICD-10-CM. |
Ectopic pregnancy (outside the uterus) |
Category O00. |
Source: Data from International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM), 2014. Centers for Medicare and Medicaid Services and the National Center for Health Statistics. Available at http://www.cdc.gov/nchs/data/icd/icd10cm_guidelines_2014.pdf.
CHAPTER 16: CERTAIN CONDITIONS ORIGINATING IN THE PERINATAL PERIOD (POO–P96)
It is easy to confuse this chapter with the next chapter on congenital malformations because both are concerned with conditions present during early childhood. The congenital chapter is descriptive of structural defects and certain chromosomal abnormalities present at birth. The perinatal chapter includes not only some conditions that start in utero but also others that occur as a result of the birth process or shortly thereafter. The perinatal period is defined as beginning before birth and lasting through the 28th day of life.
It could be possible to use one of these codes in an adult patient if there is no other code defining the condition for which the patient is being treated. Most conditions in this chapter do not last beyond infancy. However, some, such as bronchopulmonary dysplasia, can last for the lifetime of the patient and be the cause of later problems.
All clinically significant conditions noted on routine newborn examination should be coded. A condition is clinically significant if it requires clinical evaluation, therapeutic treatment, diagnostic procedures, extended hospital stay, increased nursing care or monitoring, or has implications for future healthcare needs.
Official coding guidelines for the perinatal chapter are as follows.
Reason for Encounter |
Use Code |
Birth episode of newborn infant |
Category Z38. This code can only be used once. |
Care of infant transferred in after birth |
Code(s) for condition(s) being treated (do not use Z38). |
Observation and evaluation of newborn or infant for suspected condition not found |
The official guidelines for 2014 stated that this section is “reserved for future expansion.” |
Infant being treated for health problem caused by birth process or community-acquired conditions |
If not specified, the default is due to the birth process, and the Chapter 16 code should be used. If the condition is community acquired, do not use Chapter 16. |
Prematurity or fetal growth retardation |
Do not assign a prematurity code unless it is documented. Codes in categories P05 and P07 should be based on recorded birth weight and gestational age. Sequence birth weight before gestational age if both are available. Use when the listed conditions are affecting the patient’s current health status. |
Bacterial sepsis of newborn |
P36 includes congenital sepsis. If not documented as community acquired, the default is congenital. If the P36 code does not include the bacterial agents, add an additional code from B96. |
Source: Data from International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM), 2014. Centers for Medicare and Medicaid Services and the National Center for Health Statistics. Available at http://www.cdc.gov/nchs/data/icd/icd10cm_guidelines_2014.pdf.
If the institution maintains separate medical records for stillbirths, code P95 may be used. It should not be used on maternal records.
CHAPTER 17: CONGENITAL MALFORMATIONS, DEFORMATIONS, AND CHROMOSOMAL ABNORMALITIES (QOO–Q99)
Congenital anomalies are structural or metabolic defects that are present at birth. The common term for these conditions is birth defects. A major anomaly is apparent at birth in 3%–4% of newborns; up to 7.5% of children manifest a congenital defect by the time they are 5 years old. Such defects may be due to genetics or teratogens, which are chemical or radiologic in nature and affect normal fetal development. Approximately 4,000 congenital anomalies have been identified (CDC, n.d.).
For coding purposes, it is important that the physician define a condition as congenital if it is a condition that could be either congenital or acquired. For example spina bifida, which is a lack of closure of the spinal cord’s bony encasement, can only be congenital. However, obstruction of the intestine can be either congenital or acquired. For conditions where either possibility exists, the coder cannot make the assumption that the condition is congenital just because the patient is very young.
Likewise, it may be appropriate to use a code for a congenital condition for an older patient. It is legitimate to do this as long as the condition still exists and the patient is receiving treatment for it.
New medical terminology may result in the use of a term before a code exists. Syndromes are often eponymic, which means they are named after a person. An example of both is Partington syndrome. It is named after an Australian geneticist and describes X-linked intellectual disability and focal dystonia of the hands (National Library of Medicine, 2013). Because this syndrome does not have a code, it would be necessary to code the chromosome deficiency and the mental retardation separately.
For the birth admission, the appropriate code from category Z38, liveborn infants, according to place of birth and type of delivery, should be sequenced as the principal diagnosis, followed by any congenital anomaly codes.
CHAPTER 18: SYMPTOMS, SIGNS, AND ABNORMAL CLINICAL AND LABORATORY FINDINGS, NOT ELSEWHERE CLASSIFIED (ROO–R99)
Earlier, we defined a symptom as an observation you make about your body, a subjective opinion on your part. A sign is observable by the physician; it is an objective finding.
Because diagnosis sequencing is linked to payer reimbursement of healthcare providers, rules about sequencing signs and symptoms have been developed.
Signs and Symptoms
Reason for Encounter |
Use Code |
Treatment of a sign or symptom for which a definitive diagnosis is made |
Code for definitive diagnosis. Symptom codes may be reported as secondary if the sign or symptom is not routinely associated with that definitive diagnosis. Do not use an additional code for the symptom if the principal diagnosis is a combination code that includes the symptoms already. |
Treatment of a sign or symptom for which a definitive diagnosis has not yet been reached |
Code for the sign or symptom. |
Treatment of a sign or symptom in an outpatient setting where no additional workup is performed |
Code for the sign or symptom. |
The patient has recently fallen and the reason for the fall is being investigated |
Use R29.6, repeated falls. Use code Z91.81, history of falling, when the patient has fallen in the past. If appropriate, these two codes may be used together. |
Traumatic brain injury, acute cerebrovascular disease, or sequelae of cerebrovascular disease with documented coma scale score |
Use R40._ as a secondary code if documented. A seventh character must be used to denote when the score was documented. |
Lack of ability to use one’s limbs or to ambulate, due to extreme debility, is functional quadriplegia (R53.2) |
Do not use this code for cases of neurologic quadriplegia. |
SIRS (systemic inflammatory response syndrome) due to noninfectious disease process such as trauma, malignant neoplasm, or pancreatitis |
Use R65.10 without acute organ dysfunction or R65.11 with acute organ dysfunction. |
Death, not otherwise specified |
Use R99. Only use for patients who are pronounced dead on arrival at a healthcare facility. Not the same as the discharge disposition of death. |
Source: Data from International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM), 2014. Centers for Medicare and Medicaid Services and the National Center for Health Statistics. Available at http://www.cdc.gov/nchs/data/icd/icd10cm_guidelines_2014.pdf.
The positioning of some conditions in Chapter 18 and other similar wordings in the individual disease chapters is sometimes puzzling. Abdominal pain is in this chapter as a symptom, whereas joint pain would be considered a diagnosis because it is in the musculoskeletal chapter. Specific wording used by providers can cause unintended codes. “Seizures” is in the symptom chapter, whereas “epilepsy” is a diagnosis in the nervous system chapter. If health record documentation appears to indicate the patient has epilepsy, but the provider uses only the term seizures, an explanation of the coding differences should be provided and clarification sought.
This chapter also includes codes for nonspecific and nonspecific abnormal results of diagnostic tests. These codes would ordinarily not be used unless no additional information is available. They could, for example, be used as the reason for conducting additional testing to reach a clear diagnosis.
CHAPTER 19: INJURY, POISONING, AND CERTAIN OTHER CONSEQUENCES OF EXTERNAL CAUSES (SOO–T88)
This chapter in the ICD-10-CM tabular list is huge. It covers not only what we ordinarily think of as injury and poisoning, but also burns and toxic effects of nonmedicinal substances. Significant levels of detail are required in physician documentation to ensure correct coding of conditions from this chapter. In ICD-9-CM, injuries were grouped by type, but in ICD-10-CM they are grouped by body part, with all injuries of a specific site grouped together. Laterality is part of every coding scheme in this chapter where it is appropriate. Definitions of terms commonly used with injuries are helpful.
Fractures
A fracture is a break of any size in a bone:
![]() Closed: Skin is intact
Closed: Skin is intact
![]() Open: A break in the skin occurs (compound fracture)
Open: A break in the skin occurs (compound fracture)
If the type of fracture is not documented or available, the default is closed.
In some coding categories, it is also necessary to know if the fracture is displaced or nondisplaced:
![]() Displaced: The bone is broken into two or more pieces and moved, so the proper anatomical alignment is no longer maintained.
Displaced: The bone is broken into two or more pieces and moved, so the proper anatomical alignment is no longer maintained.
![]() Nondisplaced: The bone is cracked or broken all the way through but has not moved out of correct anatomical alignment.
Nondisplaced: The bone is cracked or broken all the way through but has not moved out of correct anatomical alignment.
If a fracture is not documented as displaced or nondisplaced, it is coded to displaced.
Fracture Character Extensions As in the musculoskeletal chapter, fracture codes require the use of a seventh character defining the episode of care:
A |
Initial encounter for closed fracture |
B |
Initial encounter for open fracture |
D |
Subsequent encounter for fracture with routine healing |
G |
Subsequent encounter for fracture with delayed healing |
K |
Subsequent encounter for fracture with nonunion |
P |
Subsequent encounter for fracture with malunion |
S |
Sequela of fracture |
Categories S52, fracture of forearm; S72, fracture of femur; and S82, fracture of lower leg use a different seventh character fracture extension based on a system known as the Gustilo open fracture classification. This system uses the mechanism of injury, extent of soft-tissue damage, and degree of bone injury or involvement to classify open fractures as type I, II, or III:
Type I: Wound less than 1 cm, clean
Type II: Wound greater than 1 cm with moderate soft-tissue damage
Type III: High-energy wound greater than 1 cm with extensive soft-tissue damage
Type IIIA: Adequate soft-tissue cover
Type IIIB: Extensive soft-tissue loss and bone exposure
Type IIIC: Arterial injury requiring repair (Kim & Leopold, 2012)
The additional seventh character fracture extensions for the forearm, femur, and lower leg open fractures are as follows:
B |
Initial encounter for open fracture type I or II |
C |
Initial encounter for open fracture type IIIA, IIIB, or IIIC |
E |
Subsequent encounter for open fracture type I or II with routine healing |
F |
Subsequent encounter for open fracture type IIIA or IIIB or IIIC with routine healing |
H |
Subsequent encounter for open fracture type I or II with delayed healing |
J |
Subsequent encounter for open fracture type IIIA or IIIB or IIIC with delayed healing |
M |
Subsequent encounter for open fracture type I or II with nonunion |
N |
Subsequent encounter for open fracture type IIIA or IIIB or IIIC with nonunion |
Q |
Subsequent encounter for open fracture type I or II with malunion |
R |
Subsequent encounter for open fracture type IIIA or IIIB or IIIC with malunion |
Stress fractures are hairline cracks in bone that are due to repeated or prolonged force against the bone, not a blow to the bone. Sports or exercise can cause stress fractures. Because they are not considered an injury, they are found in the musculoskeletal chapter in ICD-10-CM, not the injury chapter.
Pathological fractures are caused by disease, not injury. The most common causes are osteoporosis and cancer. In these fractures, the bone structure itself is abnormal, contributing to the break. This type of fracture is also found in the musculoskeletal chapter.
When a bone that forms part of a joint is displaced from that location, it is known as a dislocation. Dislocations can also be categorized as open if the skin is broken. A partial or incomplete dislocation is called a subluxation. These usually occur as a result of injury. In parallel with the classification of fractures, a dislocation due to disease rather than injury is found in the musculoskeletal chapter.
Open Wounds
In addition to cuts, lacerations, and punctures, open wounds also include injuries such as animal bites (including human), traumatic amputation, and avulsion. The latter is defined as forcible pulling away of tissue. Open wounds are further classified as to whether a foreign body is present.
Superficial Injuries
Superficial injuries include the following:
![]() Contusions
Contusions
![]() Abrasion or friction burns
Abrasion or friction burns
![]() Blisters (nonthermal)
Blisters (nonthermal)
![]() External constriction
External constriction
![]() Superficial foreign body (such as splinters)
Superficial foreign body (such as splinters)
![]() Insect bite (nonvenomous)
Insect bite (nonvenomous)
![]() Other superficial bites
Other superficial bites
![]() Unspecified superficial injuries
Unspecified superficial injuries
Foreign Bodies
Foreign bodies (nonsuperficial) in open wounds are classified in that coding category. Superficial foreign bodies are classified with superficial injuries, as described previously. A separate category is used for the effects of foreign bodies entering through an orifice, or natural opening in the body (T15–T19). This would include, for example, a pencil eraser in the ear or a piece of steak stuck in the throat.
Injury, Burn, and Corrosions Character Extensions
Injury and burn codes in Chapter 19, except for fractures, have a seventh character extension that describes, in general terms, the circumstances of the encounter:
A |
Initial encounter: Used while the patent is receiving active treatment for the injury. Examples include surgical treatment, an ER encounter, or treatment by a new provider. |
D |
Subsequent encounter: Used for encounters after the patient has received active treatment and is now receiving routine care during the healing or recovery phase. Examples include medication adjustment or removal of a cast or fixation device. |
S |
Sequela: Used for complications or conditions that arise as a direct result of an injury, such as a scar. |
The official diagnosis coding guidelines related to injuries are as follows.
Injuries and Fractures
Reason for Encounter |
Use Code |
Multiple injuries |
Use separate code for each injury unless a combination code is available. Do not use the unspecified multiple injury code T07 unless information for specific codes is not available. Sequence the code for the most serious injury first. |
Abrasions or contusions |
Do not code if associated with more severe injuries of same site. |
Primary injury with minor damage to nerves or blood vessels |
Sequence primary injury first. |
Multiple fractures of same bones but different bone parts |
Code individually by site. |
Multiple fractures |
Sequence in order of severity. |
Dislocation associated with fracture of same site |
Code fracture only. |
Source: Data from International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM), 2014. Centers for Medicare and Medicaid Services and the National Center for Health Statistics. Available at http://www.cdc.gov/nchs/data/icd/icd10cm_guidelines_2014.pdf.
In addition to thermal burns due to flames, the ICD-10-CM burn classification includes burns caused by electricity, lightning, hot liquids (scalding), radiation, and hot objects. ICD-10-CM uses a new term, corrosions, to describe burns due to chemicals.
In addition to coding the location or site of the burn, it is necessary to assign a second code to indicate the percentage of body area involved in the burn. This is calculated using what is known as the “rule of nines.” Figure 2-6 illustrates the percentage of body surface associated with body areas.
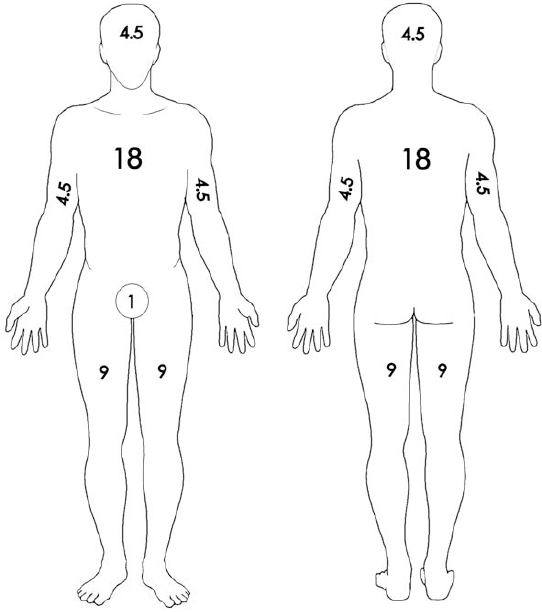
FIGURE 2-6 Rule of nines.
The “rule of palms” is useful for smaller areas. The size of the victim’s palm is approximately 1% of body area, so the number of palms will equal the percentage. The definition for the smallest area code in ICD-10-CM is 10% or less, so it is not necessary to measure precisely unless more than 10% is involved.
![]() First-degree burn: Only the outer layer of the skin, the epidermis, is involved. Symptoms include redness, tenderness, pain, and swelling.
First-degree burn: Only the outer layer of the skin, the epidermis, is involved. Symptoms include redness, tenderness, pain, and swelling.
![]() Second-degree burn: Penetrates into the dermis. Such burns are characterized by blisters, redness, swelling, and fluid seepage.
Second-degree burn: Penetrates into the dermis. Such burns are characterized by blisters, redness, swelling, and fluid seepage.
![]() Third-degree burns: Involves all three layers of the skin. The appearance of the skin is white, charred, and dry.
Third-degree burns: Involves all three layers of the skin. The appearance of the skin is white, charred, and dry.
Burns of the eye and internal organs (T26–T28) are classified by site, but not degree.
Official ICD-10-CM coding guidelines for burns are as follows.
Burns
Reason for Encounter |
Use Code |
Multiple external burns |
Sequence the code for the highest degree of burn first. Code separately. Only use the multiple burn code (T30) if location not documented. |
Multiple burns, both internal and external sites |
Circumstances of admission govern the principal or first-listed diagnosis. |
Nonhealing burns, including necrosis of burned skin |
Code as acute burns. |
Multiple burns of same local site but different degrees |
Classify to subcategory of the highest degree recorded. |
Infected burn site |
Use additional code to identify infection. |
Mortality of burn victim during episode of care, or third-degree burn of >20% body area |
Use category T31 or T32. |
Treatment of sequelae of burns (scars, joint contractures) |
Burn or corrosion code with a seventh character of S. |
Source: Data from International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM), 2014. Centers for Medicare and Medicaid Services and the National Center for Health Statistics. Available at http://www.cdc.gov/nchs/data/icd/icd10cm_guidelines_2014.pdf.
Poisoning, Adverse Effects, and Toxicity
The definitions of these terms are a little different than those used in the average murder mystery:
![]() Poisoning occurs when a drug, medicinal substance, or other biological substance is not used correctly. This can occur through:
Poisoning occurs when a drug, medicinal substance, or other biological substance is not used correctly. This can occur through:
![]() Wrong dosage taken by patient
Wrong dosage taken by patient
![]() Wrong dosage administered to patient
Wrong dosage administered to patient
![]() Medication taken by wrong person
Medication taken by wrong person
![]() Overdose (intentional or accidental)
Overdose (intentional or accidental)
![]() Nonprescribed drug taken with correctly prescribed and properly administered drug
Nonprescribed drug taken with correctly prescribed and properly administered drug
![]() Medications taken in combination with alcohol or over-the-counter medications
Medications taken in combination with alcohol or over-the-counter medications
![]() Adverse effects occur when a drug is correctly prescribed and properly administered but there are side effects:
Adverse effects occur when a drug is correctly prescribed and properly administered but there are side effects:
![]() Drug allergy or hypersensitivity
Drug allergy or hypersensitivity
![]() Drug intoxication
Drug intoxication
![]() Drug toxicity (including cumulative effects)
Drug toxicity (including cumulative effects)
Toxic effects, from a coding perspective, refer to exposure to or contact with nonmedicinal substances such as chemicals, gases, metals, foods, and substances such as latex and silicone.
Underdosing is a new category in ICD-10-CM, defined as taking less of a medication than is prescribed or as instructed by the manufacturer, either inadvertently or deliberately.
The ICD-10-CM includes a large table of drugs and chemicals that is used to locate the correct code for poisoning. Additional codes for external causes are not required because these are combination codes that include the cause. The table has columns for adverse effect and underdosing, as well as four columns for poisoning intent:
![]() Accidental or unintentional (default if no intent documented)
Accidental or unintentional (default if no intent documented)
![]() Intentional self-harm
Intentional self-harm
![]() Assault
Assault
![]() Undetermined (documentation that intent cannot be determined)
Undetermined (documentation that intent cannot be determined)
The official diagnosis coding rules for these categories are as follows.
Poisoning and Adverse Effects
Reason for Encounter |
Use Code |
Adverse effect of a drug correctly prescribed and properly administered |
Code for nature of the adverse effect plus T code for adverse effect of the drug |
Condition caused by error in prescription or administration of drug |
T code for accidental poisoning plus code for manifestation |
Intentional overdose |
T code for intentional self-harm poisoning plus code for manifestation |
Nonprescribed drug in combination with correctly prescribed and administered drug |
T code for accidental poisoning plus code for manifestation |
Toxic effect of nonmedicinal substances |
Code for toxic effect (T51–T65) plus code to specify nature of toxic effect |
Source: Data from International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM), 2014. Centers for Medicare and Medicaid Services and the National Center for Health Statistics. Available at http://www.cdc.gov/nchs/data/icd/icd10cm_guidelines_2014.pdf.
Codes are also available for effects of other external causes:
![]() Environmental factors, such as radiation, cold, heat and light, air pressure
Environmental factors, such as radiation, cold, heat and light, air pressure
![]() Anaphylactic shock due to food reactions
Anaphylactic shock due to food reactions
![]() Early complications of trauma, such as compartment syndrome, shock, fat embolism, subcutaneous emphysema
Early complications of trauma, such as compartment syndrome, shock, fat embolism, subcutaneous emphysema
![]() Adult and child abuse, neglect, and other maltreatment
Adult and child abuse, neglect, and other maltreatment
Codes for these conditions are classified as to whether they are suspected or confirmed, based on provider documentation. For confirmed cases, additional codes should be used to identify the cause of any physical injuries. A perpetrator code (Y07) can be added, if known.
Complications of Surgical and Medical Care
Assignment of a code from this section does not imply that the surgical or medical care was inadequate. It does denote that a relationship between the care and the current condition has been documented, and that the current condition is more than routinely expected. There is no officially defined time limit on when the complication must occur.
Some complications are due to the presence of internal prosthetic devices, implants, or grafts. They may involve mechanical complications, such as breakage, leaking, or obstructions, or they may involve infection or inflammatory reaction. Other complications, such as pain, hemorrhage, stenosis, and fibrosis, also have codes defined by the type of internal device.
Complications of organ transplants are also in this section, as are systemic conditions such as post-op shock, accidental laceration during the procedure, postop infections, blood transfusion reactions, foreign bodies accidentally left in the patient, and many of the other unfortunate circumstances that may occur. Some intraoperative and postprocedural complication codes are found within the body system chapters with codes specific to the organs and structures of that body system.
CHAPTER 20: EXTERNAL CAUSES OF MORBIDITY (VOO–Y99)
External cause codes identify the following:
![]() How an injury or health condition happened (cause)
How an injury or health condition happened (cause)
![]() The intent (unintentional/intentional)
The intent (unintentional/intentional)
![]() The place where the event occurred
The place where the event occurred
![]() The activity of the patient at the time of the event
The activity of the patient at the time of the event
![]() The patient’s status, such as civilian or military
The patient’s status, such as civilian or military
These are never used as the principal or first-listed code; they are always used in a supplementary fashion. They are used primarily for statistical purposes in gathering data on injury cause, extent, and location. This data can be used for injury prevention and education programs.
The major categories of external cause codes include transport accidents, falls, fire and flames, natural and environmental causes, assaults, self-inflicted injuries, and misadventures to patients during surgical and medical care.
A new feature of ICD-10-CM is the ability to code the patient’s documented blood alcohol level (Y90._).
Reporting of external causes is not mandatory on a national level, and such codes are not generally used in healthcare billing and reimbursement.
CHAPTER 21: FACTORS INFLUENCING HEALTH STATUS AND CONTACT WITH HEALTH SERVICES (ZOO–Z99)
This chapter in ICD-10-CM is used to identify situations in which patients who are not currently sick require health services.
Z codes are controversial in the healthcare reimbursement arena because they may represent services for which some payers will not pay. The official diagnosis coding guidelines and the enforcement of the HIPAA standard code set rules have helped in recent years to enforce appropriate coding and insurance coverage.
Z codes are used in the following circumstances:
![]() When a person who is not currently sick encounters health services for a specific reason, such as to act as an organ donor, to receive prophylactic care such as inoculations or screenings, or to receive counseling on a health-related issue.
When a person who is not currently sick encounters health services for a specific reason, such as to act as an organ donor, to receive prophylactic care such as inoculations or screenings, or to receive counseling on a health-related issue.
![]() When a person with a resolving disease or injury or a chronic long-term condition requiring continuous care encounters the health care system for specific aftercare of that disease or injury. Examples are dialysis for renal disease, chemotherapy for malignancy, and cast change. A diagnosis or symptom code should be used instead of a Z code whenever a current, acute diagnosis is being treated or a sign or symptom is being studied.
When a person with a resolving disease or injury or a chronic long-term condition requiring continuous care encounters the health care system for specific aftercare of that disease or injury. Examples are dialysis for renal disease, chemotherapy for malignancy, and cast change. A diagnosis or symptom code should be used instead of a Z code whenever a current, acute diagnosis is being treated or a sign or symptom is being studied.
![]() When circumstances or problems influence a person’s health status but are not in themselves a current illness or injury.
When circumstances or problems influence a person’s health status but are not in themselves a current illness or injury.
![]() For newborns, to indicate birth status.
For newborns, to indicate birth status.
Z Code Category Definitions
The official guidelines are specific about which Z code category each code belongs in and also define which Z codes must be only primary or only secondary.
Contact/Exposure
Z20 |
Patients do not show any sign or symptom of a communicable disease but have been exposed to it |
Z77 |
Contact or exposure hazardous to health (chemicals, pollution) |
Contact/exposure codes are used as a first-listed code to indicate a reason for testing or as a secondary code to identify a potential risk.
Inoculations and Vaccinations Patient is being seen for a prophylactic inoculation against a disease.
Z23 |
Because this is a single code for all vaccinations, the type given can only be identified via the procedure code. |
Status Codes The patient is either a carrier of a disease or has the sequelae or residual of a past disease or condition, which can include the presence of a prosthetic or mechanical device or transplanted organ from previous treatment. The status code differs from a history code because the latter indicates the patient no longer has the condition.
Z14 |
Genetic carrier |
Z15 |
Genetic susceptibility to disease (not principal or first listed) |
Z16 |
Resistance to antimicrobial drugs (sequence infection code first) |
Z17 |
Estrogen receptor status |
Z18 |
Retained foreign body fragments |
Z21 |
Asymptomatic HIV infection status (tested positive but no signs or symptoms) |
Z22 |
Carrier of infectious disease |
Z28.3 |
Underimmunization status |
Z33.1 |
Pregnant state, incidental (secondary only) |
Z66 |
Do not resuscitate (order must be documented) |
Z67 |
Blood type |
Z68 |
Body mass index (adult codes for ages 21 and older; pediatric codes for ages 2–20) |
Z74.01 |
Bed confinement status (bedridden) |
Z76.82 |
Awaiting organ transplant status |
Z78 |
Other specified health status |
Z79 |
Long-term (current) drug therapy (long-term therapeutic or prophylactic use, not for drug addiction or detox) |
Z88 |
Allergy status to drugs, medicaments, and biological substances |
Z89 |
Acquired absence of limb (post-traumatic, postprocedural) |
Z90 |
Acquired absence of organs NEC (a few are in other chapters) |
Z91.0 |
Allergy status, other than to drugs and biological substances (food, insects, latex, contrast media) |
Z92.82 |
Status post administration of tPa in different facility in last 24 hours (assign code for condition being treated with tPa first) |
Artificial opening status (not used if opening requires attention) | |
Z94 |
Transplanted organ and tissue status |
Z95 |
Presence of cardiac and vascular implants and grafts |
Z96 |
Presence of other functional implants |
Z97 |
Presence of other devices |
Z98 |
Other postprocedural states (includes Z98.85 to indicate a transplanted organ has been previously removed) |
Z99 |
Dependence on enabling machines and devices NEC |
History Codes History codes indicate personal or family history. Personal history codes explain a patient’s past medical condition that no longer exists and for which he or she is not receiving any treatment but that may have the potential for recurrence, and thus may require monitoring.
Family history codes are used when a patient has a family member who has had a particular disease that causes the patient to be at higher risk of also contracting that disease.
Z80 |
Family history of primary malignant neoplasm |
Z81 |
Family history of mental and behavioral disorders |
Z82 |
Family history of certain disabilities and chronic diseases |
Z83 |
Family history of other specific disorders |
Z84 |
Family history of other conditions |
Z85 |
Personal history of malignant neoplasm |
Z86 |
Personal history of certain other diseases |
Z87 |
Personal history of other diseases and conditions |
Z91.4_ |
Personal history of psychological trauma NEC |
Z91.5_ |
Personal history of self-harm |
Z91.8_ |
Other specified personal risk factors NEC (except Z91.83) |
Z92 |
Personal history of medical treatment (except contraception and tPa) |
Screening Screening is the testing for disease or disease precursors in seemingly well individuals so that early detection and treatment can be provided for those who test positive for the disease. The Z code indicates that a screening exam is planned. A Z code is not used if the patient already has a sign or symptom; this is a diagnostic exam, not a screening. In those cases, the sign or symptom is used to explain the reason for the test. Screening codes may be first listed if the reason for the visit is specifically the screening exam. It may be a secondary code if the screening is done during an office visit for other health problems.
Z11 |
Encounter for screening for infectious and parasitic diseases |
Z12 |
Encounter for screening for malignant neoplasm |
Z13 |
Encounter for screening for other diseases and disorders (except Z13.9) |
Z36 |
Encounter for antenatal screening for mother |
Observation Observation codes are only used in limited circumstances when the patient is being observed for a suspected condition that is ruled out. They should not be used if an injury or illness or any signs or symptoms related to the suspected condition are present. In those cases, the diagnosis or symptom code would be used. It is used as a principal diagnosis only (except for Z03.7, maternal and fetal conditions, which may be used as secondary if appropriate).
Z03 |
Encounter for medical observation for suspected diseases and conditions, ruled out |
Z04 |
Encounter for examination and observation for other reasons (except Z04.9) |
Aftercare Aftercare is when the initial treatment of a disease has been performed but the patient requires continued care during the healing or recovery phase or for the long-term consequences of the disease. The aftercare Z code is not used if the treatment is directed at a current, acute disease, in which case the diagnosis code would be used. Exceptions to this rule are chemotherapy, immunotherapy, and radiation therapy. If the purpose of the encounter is to receive one of these therapies, the appropriate Z51 code would be first, accompanied by the diagnosis code for the neoplasm being treated. The aftercare Z codes would not be used for aftercare for injuries. Instead, the acute injury code should be used with a seventh character for the subsequent encounter.
Z42 |
Encounter for plastic and reconstructive surgery following medical procedure or head injury |
Z43 |
Encounter for attention to artificial openings |
Z44 |
Encounter for fitting and adjustment of external prosthetic device |
Z45 |
Encounter for adjustment and management of implanted device |
Z46 |
Encounter for fitting and adjustment of other devices |
Z47 |
Orthopedic aftercare |
Z48 |
Encounter for other postprocedural aftercare |
Z49 |
Encounter for care involving renal dialysis |
Z51 |
Encounter for other aftercare |
Follow-up The follow-up codes are used to explain continuing surveillance following completed treatment of a disease, condition, or injury. They imply that the condition has been fully treated and no longer exists. Follow-up codes may be used with history codes to provide the full picture of the healed condition and its treatment. The follow-up code would be sequenced first. If the condition is found to have recurred, the diagnosis code should be used instead of the follow-up code. Do not confuse the follow-up codes with aftercare codes or injury codes with a subsequent seventh character; those codes are for a healing condition or its sequelae, not for a condition that no longer exists.
Z08 |
Encounter for follow-up exam after completed treatment for malignant neoplasm |
Z09 |
Encounter for follow-up examination after completed treatment for conditions other than malignant neoplasm |
Z39 |
Encounter for maternal postpartum care and examination |
Donor The donor code is used for living individuals who are donating blood or other body tissue to another person. Not for self-donation or cadaveric donations.
Z52 |
Donors of organs and tissues |
Counseling Counseling codes are used when the patient or family member receives assistance in the aftermath of an illness or injury or when support is required in coping with family or social problems.
Z30.0_ |
Encounter for general counseling and advice on contraception |
Z31.5 |
Encounter for genetic counseling |
Z31.6_ |
Encounter for general counseling and advice on procreation |
Z32.2 |
Encounter for childbirth instruction |
Z32.3 |
Encounter for childcare instruction |
Z69 |
Encounter for mental health services for victim or perpetrator of abuse |
Z70 |
Counseling related to sexual attitude, behavior, and orientation |
Z71 |
Persons encountering health services for other counseling and medical advice NEC |
Z76.81 |
Expectant mother prebirth pediatrician visit |
Encounters for Obstetrical and Reproductive Services A Z code may be used for routine visits if none of the problems or complications included in the codes from the obstetrics chapter exist.
Z30 |
Encounter for contraceptive management |
Z31 |
Encounter for procreative management |
Z32.2 |
Encounter for childbirth instruction |
Z32.3 |
Encounter for childcare instruction |
Z33 |
Pregnant state (includes code for elective termination of pregnancy) |
Z34 |
Encounter for supervision of normal pregnancy |
Encounter for antenatal screening of mother | |
Z3A |
Weeks of gestation (use the date of admission to determine weeks of gestation for inpatient admissions that encompass more than one gestational week) |
Z37 |
Outcome of delivery (use on all maternal records; always secondary) |
Z39 |
Encounter for maternal postpartum care and examination |
Z76.81 |
Expectant mother prebirth pediatrician visit |
Newborns and Infants The following Z codes apply to newborns and infants:
Z00.1_ |
Encounter for routine child health examination |
Z38 |
Liveborn infants according to place of birth and type of delivery (principal only) |
Z76.1 |
Encounter for health supervision and care of foundling |
Routine and Administrative Examinations These include general check-ups or exams such as pre-employment physicals. These codes are not used if the exam is for diagnosis of a suspected condition or for treatment purposes. During a routine exam, if a diagnosis or condition should be discovered, it should be coded as an additional code. Pre-op exam codes are for clearance only, not the treatment given.
Z00 |
Encounter for general examination without complaint, suspected or reported diagnosis |
Z01 |
Encounter for other special examination without complaint, suspected or reported diagnosis |
Z02 |
Encounter for administrative examination (except Z02.9) |
Z32.0_ |
Encounter for pregnancy test |
Miscellaneous Z Codes These capture a number of other healthcare encounters that do not fall into another category.
Immunization not carried out (except Z28.3) | |
Z40 |
Encounter for prophylactic surgery (use additional code to identify the associated risk factor) |
Z41 |
Encounters for procedures for purposes other than remedying health state (cosmetic, piercing) |
Z53 |
Persons encountering health services for specific procedures and treatment, not carried out (contraindicated, patient’s decision) |
Z55 |
Problems related to education and literacy |
Z56 |
Problems related to employment and unemployment |
Z57 |
Occupational exposure to risk factors |
Z58 |
Problems related to physical environment |
Z59 |
Problems related to housing and economic circumstances |
Z60 |
Problems related to social environment |
Z62 |
Problems related to upbringing |
Z63 |
Other problems related to primary support group, including family circumstances |
Z64 |
Problems related to certain psychosocial circumstances |
Z65 |
Problems related to other psychosocial circumstances |
Z72 |
Problems related to lifestyle |
Z73 |
Problems related to life management difficulty |
Z74 |
Problems related to care provider dependency (except Z74.01) |
Z75 |
Problems related to medical facilities and other health care |
Z76.0 |
Encounter for issue of repeat prescription |
Z76.3 |
Health person accompanying sick person |
Z76.4 |
Other boarder to healthcare facility |
Z76.5 |
Malingerer (conscious simulation) |
Z91.1_ |
Patient’s noncompliance with medical treatment and regimen |
Z91.83 |
Wandering in diseases classified elsewhere |
Z91.89 |
Other specified personal risk factors, NEC |
Nonspecific Z Codes These codes are so nonspecific that there can be little justification for their use in the inpatient setting and they should only be used in the outpatient setting when there is no further documentation to permit more precise coding.
Z02.9 |
Encounter for administrative examinations, unspecified |
Z04.9 |
Encounter for examination and observation for unspecified reason |
Z13.9 |
Encounter for screening, unspecified |
Z41.9 |
Encounter for procedure for purposes other than remedying health state, unspecified |
Z52.9 |
Donor of unspecified organ or tissue |
Z86.59 |
Personal history of other mental and behavioral disorders |
Z88.9 |
Allergy status to unspecified drugs, medicaments, and biological substances status |
Z92.0 |
Personal history of contraception |
Z Codes That May Only Be Principal/First-Listed Diagnosis The following Z codes/categories may only be reported as the principal or first-listed diagnosis, unless there are multiple encounters on the same day and the records are combined.
Z00 |
Encounter for general examination without complaint, suspected or reported diagnosis |
Z01 |
Encounter for other special examination without complaint, suspected or reported diagnosis |
Z02 |
Encounter for administrative examination |
Z03 |
Encounter for medical observation for suspected diseases and conditions ruled out |
Z04 |
Encounter for examination and observation for other reasons |
Z31.81 |
Encounter for male factor infertility in female patient |
Z31.82 |
Encounter for Rh incompatibility status |
Z31.83 |
Encounter for assisted reproductive fertility procedure cycle |
Z31.84 |
Encounter for fertility preservation procedure |
Z33.2 |
Encounter for elective termination of pregnancy |
Z34 |
Encounter for supervision of normal pregnancy |
Liveborn infants according to place of birth and type of delivery | |
Z39 |
Encounter for maternal postpartum care and examination |
Z42 |
Encounter for plastic and reconstructive surgery following medical procedure or healed injury |
Z51.0 |
Encounter for antineoplastic radiation therapy |
Z51.1_ |
Encounter for antineoplastic chemotherapy and immunotherapy |
Z52 |
Donors of organs and tissues |
Z76.1 |
Encounter for health supervision and care of foundling |
Z76.2 |
Encounter for health supervision and care of other healthy infant and child |
Z99.12 |
Encounter for respirator (ventilator) dependence during power failure |
How Can You Code Your Conditions?
If you have a sign, symptom, or diagnosis that you want to code, follow these steps:
1. Look for the condition in the alphabetical index. You may have to look in more than one place. If you don’t find it listed under one of the terms, look under the others.
2. Once you have found the term, look at everything indented beneath it to see if there are other words from your diagnosis statement that apply.
3. After you have located what seems to be the correct term in the alphabetical index, look up the number in the tabular list.
4. Make sure you read all of the notes associated with your numeric code. Some of the notes may be at the top of the heading under which your number is listed. Some of the notes are “includes” that tell you what is included under this number, whereas others are “excludes” that may point you to another chapter and diagnosis code.
ICD-10-CM is updated once a year, effective October 1 of that year. Diagnosis codes are added to cover newly identified disease states. CMS and the NCHS publish these agenda in the United States with the approval of the World Health Organization. The diagnosis section of ICD-10-CM is the responsibility of NCHS, and the CMS handles the PCS (Procedure Coding System) procedure section. The other two cooperating parties on ICD-10-CM are AHIMA and the AHA. The central office on ICD-10-CM, housed at the AHA headquarters in Chicago, publishes Coding Clinic, a quarterly publication covering updates, coding guidelines, and readers’ questions.
It is imperative that you use the currently implemented version of ICD-9-CM or ICD-10-CM to research or solve personal coding-related concerns. When codes are revised, the code used is based on the date of service of your procedure. There is no longer any grace period during which it is okay to use either old or new codes.
Misdiagnosis: The Wrong Path
The patient was a 39-year-old male previously in good health. He was on summer vacation near the ocean, and over a 2-day period he participated in several strenuous activities, such as swimming, sailing, jogging, even putting out a small forest fire. He later experienced chills and was so tired that he went to bed early. By the next morning, one leg was weak. It became paralyzed by the afternoon, and by evening the other leg was weakened. He had a temperature of 102 degrees Fahrenheit. The family physician who examined the patient decided he had a cold.
By the second day, the paralysis had spread to all body areas below the chest. A specialist examined the patient and decided the problem was a blood clot in the lower spinal cord. Not until the 15th day of the illness was another diagnosis made. The patient was Franklin Delano Roosevelt, and the diagnosis was poliomyelitis.
Even long after Roosevelt’s death, the debate about the cause of his paralytic illness continues. At the time, the diagnosis of polio seemed appropriate because it was the most common cause of paralysis in the United States, it was contracted during the summer, and it was accompanied by fever. Researchers looking at the diagnosis retrospectively point to the patient’s age of 39 and the lack of physician knowledge about other potential causes as indicative of the fact that the actual culprit was Guillain-Barre syndrome, an autoimmune condition (Goldman et al., 2003).
Misdiagnosis can occur when:
![]() Doctors lack sufficient time to analyze a problem thoroughly
Doctors lack sufficient time to analyze a problem thoroughly
![]() Testing is not performed in order to save money
Testing is not performed in order to save money
![]() Knowledge about less common diseases is lacking
Knowledge about less common diseases is lacking
![]() Patients do not communicate complete information
Patients do not communicate complete information
![]() Tests are not completed due to patient noncompliance
Tests are not completed due to patient noncompliance
![]() Testing errors occur (equipment failure, human error)
Testing errors occur (equipment failure, human error)
![]() Objective testing is not possible
Objective testing is not possible
![]() Diagnosis is difficult to confirm
Diagnosis is difficult to confirm
Diagnosis is required for desired treatment implementation. If you obtain information that indicates to you that the wrong diagnosis has been made, it is important that you discuss the matter with your physician. He can review the facts with you and, if necessary, change his opinion. It is important that the incorrect diagnosis does not remain on your medical record, because it could affect your future treatment and well-being.
References
1984 Revision of the Uniform Hospital Discharge Data Set. (1985, July 31). Federal Register, 50(147), 31038–31040.
Center for Medicare and Medicaid Services. (n.d.). Documentation guidelines—evaluation and management services. Retrieved January 20, 2014, from http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/Downloads/97Docguidelines.pdf
Centers for Disease Control and Prevention. (n.d.). Facts about birth defects. Retrieved January 21, 2014, from http://www.cdc.gov/ncbddd/birthdefects/facts.html
Department of Health and Human Services, Centers for Medicare and Medicaid Services. (2001, September 26). Transmittal AB-01-144. Retrieved January 20, 2014, from http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/AB01144.pdf
Goldman, A. S., Schmalstieg, E. J., Freeman, D. H. Jr., Goldman, D. A., & Schmalstieg, F. C. Jr. (2003). What was the cause of Franklin Delano Roosevelt’s paralytic illness? Journal of Medical Biography, 11(4), 232–240.
Kim, P., & Leopold, S. (2012). Gustilo-Anderson classification. Clinical Orthopaedic Related Research, 470(11), 3270–3274.
National Center for Health Statistics. (2014). ICD-10-CM official guidelines for coding and reporting. Retrieved January 20, 2014, from http://www.cdc.gov/nchs/data/icd/icd10cm_guidelines_2014.pdf
National Library of Medicine. (2013, May). Genetics home reference. Retrieved January 21, 2014, from http://ghr.nlm.nih.gov/condition/partington-syndrome
National Pressure Ulcer Advisory Panel. (n.d.). Pressure ulcer stages/categories. Retrieved January 7, 2014, from http://www.npuap.org/resources/educational-and-clinical-resources/npuap-pressure-ulcer-stagescategories/
Maisel, E. (2013, July 23). The new definition of a mental disorder. Psychology Today. Retrieved January 5, 2014, from http://psychologytoday.com/blog/rethinking-psychology/201307/the-new-definition-mental-disorder
U.S. Department of Health and Human Services, National Institutes of Health, National Heart Lung and Blood Institute. (2012, September). Asthma care quick reference. Publication 12-5075. Retrieved January 6, 2014, from http://www.nhlbi.nih.gov/guidelines/asthma/asthma_qrg.pdf