Chapter 6
HOT ENVIRONMENTS*
David W. DeGroot and Laura A. Pacha**
Exposure to high ambient temperatures while working in hot indoor environments or while working outdoors in hot weather is a common and potentially fatal occupational hazard. Unlike cold exposure (Chapter 7), which can be almost completely mitigated with proper clothing and equipment, it is impossible to fully mitigate the effects of a hot environment. Normally, body core temperature is maintained within a very narrow range. In the occupational setting, heat stress from the combined effects of environmental heat, metabolic heat, and often the use of impervious clothing can strain the ability to maintain heat balance, and core temperature may begin to rise, potentially leading to an exertional heat illness. Workplace heat exposure, in addition to causing heat-related illness, has been found to decrease productivity and to increase job-related accidents.1
OCCUPATIONAL SETTING
No recent estimate of the number of workers exposed to hot environments has been published. In 1986, the National Institute for Occupational Safety and Health (NIOSH) estimated that 5–10 million Americans worked in jobs where heat stress was an occupational health hazard, and this range is probably still a reasonable estimate.2 Table 6.1 lists some common work sites where workers may be expected to experience heat stress.3 Heat-related deaths are common in the United States. From 1999 to 2009, there was an average of 658 heat-related deaths annually.4 Most of the heat-related deaths reported by the Centers for Disease Control and Prevention (CDC) were in nonworking populations. Occupational- or exertional-related heat deaths, while known to occur, are infrequently reported in the medical literature.5 Thirteen workplace heat-related deaths were cited for federal enforcement by the Occupational Safety and Health Administration (OSHA) in 2012–2013.5 On the other hand, heat-related hospitalizations are relatively common, with over 28 000 cases in a 10-year period.6 How many of these cases were associated with occupational exposure to heat stress is not known. A case series of heat-related casualties in the mining industry reported the incidence of heat exhaustion in the summer months as 43 cases/million man-hours worked.7 Military personnel, who are often required to achieve very high levels of work output in hot environments, have a long history of high risk for heat stress.8 Reports from the military continue to provide information on the occurrence of heat injury in healthy, young individuals.9,10
TABLE 6.1 Work sites with heat exposure.
Source: Department of Labor. OSHA Technical Manual In: OSHA, ed. Washington, DC 1999.
| Iron and steel foundries |
| Non-ferrous foundries |
| Brick-firing and ceramics plants |
| Glass products facilities |
| Rubber products factories |
| Electrical utilities |
| Bakeries |
| Confectioneries |
| Commercial kitchens |
| Laundries |
| Food canneries |
| Chemical plants |
| Mining sites |
| Smelters |
| Steam tunnels |
| Fires (firefighting) |
| Outdoor operations |
| Surface mines |
| Agriculture sites |
| Construction sites |
| Merchant marine ships |
| Hazardous waste sites |
| Military training sites |
| Athletic competitions |
In any hot environment, whether indoors or outdoors, high humidity or heavy manual labor increases the workers’ risk for heat strain. Specific occupational groups, such as firefighters, are at exceptionally high risk for heat stress. Not only are they exposed to extremely high temperatures while fighting fires but they also must perform demanding physical tasks while wearing fire-resistant protective clothing that attenuates heat dissipation to the environment. The hazardous waste cleanup industry is another field where heat strain is a potentially significant occupational hazard, due to required respiratory protection and full protective clothing. These requirements limit the use of conventional heat stress monitoring guidelines and place an additional stress on the hazardous waste cleanup worker.
MEASUREMENT ISSUES
Environmental heat
Ambient or environmental heat affecting the worker and the worker’s ability to transfer body heat to the environment is determined by four environmental factors: (i) air or dry-bulb temperature (Tdb), (ii) air moisture content or wet-bulb temperature (Twb), (iii) air velocity, and (iv) radiant heat (solar and infrared). Microwave radiation may also be a source of environmental heat in some work situations (see Chapter 15). Various measures of ambient heat load, reflecting the factors influencing heat transfer, are available for use in the industrial setting.11 The most commonly used instruments for quantifying the thermal environment are described in Table 6.2.
TABLE 6.2 Measures of external heat.2,11
| Measure | Device | Comments |
| Dry bulb | Liquid-in-glass thermometer; thermocouple; resistance thermometer | Measures ambient air temperature and is useful in determining comfort zone for lightly clothed sedentary workers. Does not measure effect of humidity, radiant heat, or air movement on temperature |
| Wet bulb | Thermometer bulb or sensor covered by a wet cotton wick that is exposed to air movement | Measures effect of humidity on evaporation and effect of air movement on ambient temperature. Natural wet-bulb temperature is the term used if the wet bulb is exposed to prevailing natural air movement; may be a useful guide in preventing heat stress in hot, humid, and still environments where radiant heat does not contribute to heat load, such as underground mines |
| Globe temperature | Black globe—temperature sensor in the center of a 15 cm hollow copper sphere painted flat black | Measures effect of radiant heat. Wet globe thermometer (Botsball) also reflects the effect of humidity and supposedly exchanges heat with the environment similarly to a nude man with totally wet skin |
| Wet globe—temperature sensor in the center of a 3 in. copper sphere covered by a wet black cloth | ||
| Air velocity | Vane and cup, hot-wire, pulsed-wire, ultrasonic, and Laser doppler anemometers | Vane and cup and hot-wire anemometers are directional devices, remaining anemometers are insensitive to flow direction and may be more suitable for use in locations with varying air flow direction |
Metabolic heat
Heat production in the body is the by-product of normal basal metabolism and occurs mostly in the liver, brain, heart, and skeletal muscles. During exercise or work, skeletal muscle activity greatly increases metabolic heat production. A measurement of metabolic heat production or, at least, an estimate of metabolic heat is essential in determining a worker’s total heat stress and in calculating workplace heat exposure limits. Direct or indirect measurement of each worker’s level of work and quantity of heat produced in the occupational setting is not practical. Therefore, tables of the workload or energy cost of various tasks have been developed and are used to estimate metabolic heat (Table 6.3).
TABLE 6.3 Metabolic rate categories and example activities.
| Category | Metabolic rate (W)* | Examples |
| Resting | 115 | Sitting |
| Light | 180 | Sitting with light manual work with hands or hands and arms, and driving. Standing with some light arm work and occasional walking. |
| Moderate | 300 | Sustained moderate hand and arm work, moderate arm and leg work, moderate arm and trunk work, or light pushing and pulling. Normal Walking. |
| Heavy | 415 | Intense arm and trunk work, carrying, shoveling, manual sawing; pushing and pulling heavy loads; and walking at a fast pace. |
| Very Heavy | 520 | Very intense activity at fast to maximum pace. |
* The effect of body weight on the estimated metabolic rate can be accounted for by multiplying the estimated rate by the ratio of actual body weight divided by 70 kg (154 lb). From ACGIH®, 2015 TLVs® and BEIs® Book. Copyright 2015. Reprinted with permission.
EXPOSURE GUIDELINES
Heat stress indexes
The guidelines currently used for worker exposure to heat stress are based on indexes developed through subjective and objective testing of workers or from combinations of external heat measurements. Earlier examples include the effective temperature index, resultant temperature, equivalent temperature, the Oxford index, the Botsball, the heat stress index, and the wet globe temperature index. It is important to note that some of these are indicators of subjective thermal comfort and not of heat stress.12 Today, the most commonly used index is the Wet-Bulb Globe Temperature (WBGT) index, which was originally developed in an effort to reduce the incidence of heat illness during Marine Corps basic training at Parris Island.13
The WBGT index is recommended by OSHA, NIOSH, and American Conference of Governmental Industrial Hygienists (ACGIH) and required by the US Armed Forces.14,15
The WBGT index is calculated from measurements of the natural wet-bulb (Twb), the black globe (Tg), and the dry-bulb (Tdb) temperatures.
For outdoor environments with a solar heat source, the WBGT formula is
For indoor use or for outdoor settings without a solar load, the formula is
The necessary measurements require relatively simple instrumentation and can be easily obtained in an industrial environment. Automated heat stress monitors that measure all three temperatures and calculate the WBGT index temperature are also available. An example of a manual WBGT monitor is shown in Figure 6.1. The WBGT index was developed for men exercising outdoors in military fatigues. Therefore, if different types of clothing are worn, correction factors are required. This index is not applicable in settings where sweat-impermeable clothing is required and may not be as effective as other indices in preventing heat casualties in extreme heat stress conditions.
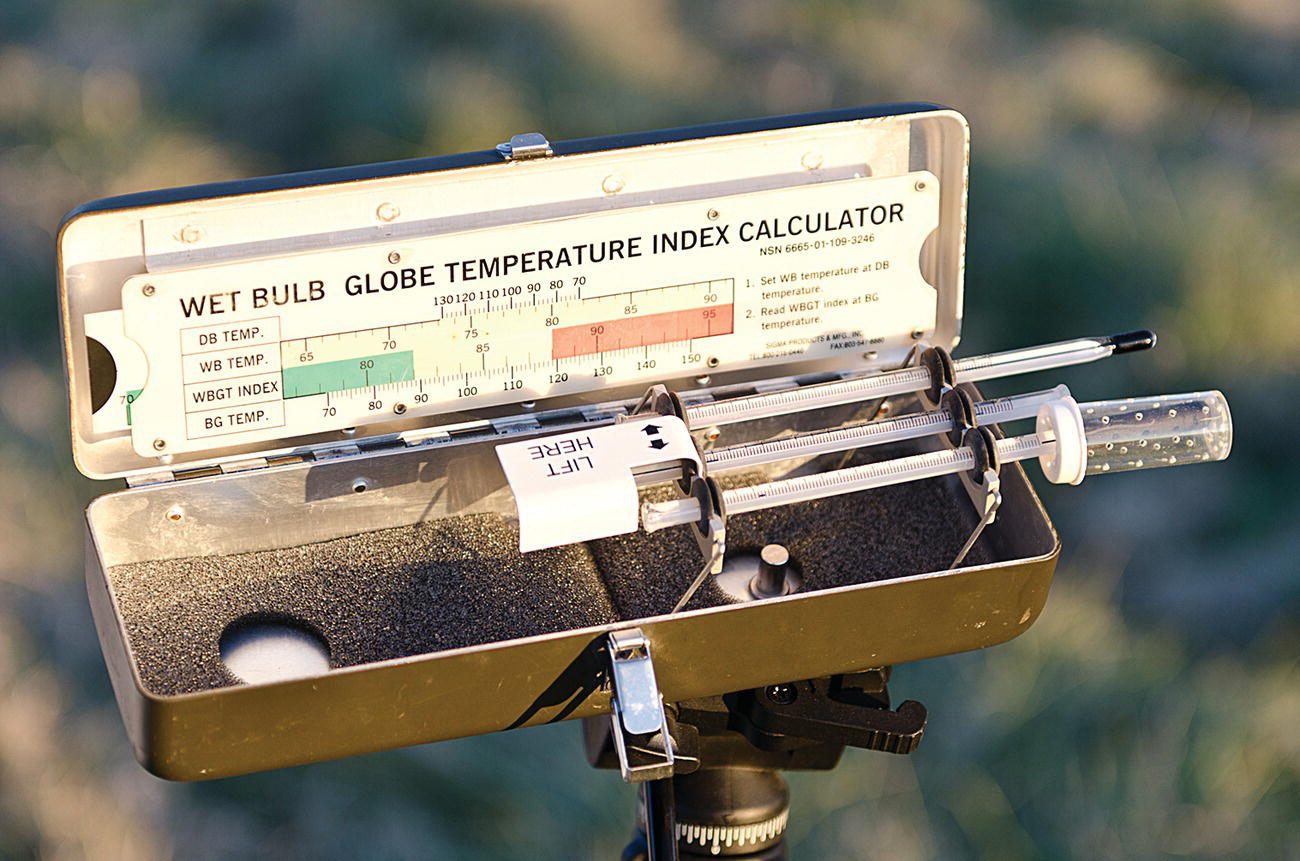
FIGURE 6.1 Manual, analog WBGT monitor; automated WBGT monitors are available from a variety of manufacturers.
Photo courtesy of the authors.
Heat strain indicators
Under identical heat stress conditions, the heat strain experienced by different individuals may vary widely, which may require estimation of the physiologic responses to environmental heat stress. Historically, the cumbersome nature of monitoring equipment and its lack of durability have limited our ability to make real-time measurements of a workers’ core temperature or heart rate. As technology improves and durable and convenient monitors and sensors become available, the physiologic measures of heat strain may take on increasing importance, especially for workers in heavy protective clothing.
Heart rate is easily measured and may be a reliable indicator of overall heat strain, rising with both increasing workload and increasing core temperature. Utilizing this physiologic response to heat, a method of measuring oral temperature, postwork heart rate, and recovery heart rate to monitor for heat strain has been developed. Heat stress exposure should be discontinued if (i) sustained heart rate is in excess of 180 bpm minus the individual’s age in years or (ii) recovery heart rate at 1 minute after peak work effort is greater than 120 bpm.14 The availability of inexpensive electronic pulse monitors and timers has made this method easier, and it can be a valuable indicator of heat strain in certain settings.
Body core temperature appears to be a more reliable indicator of heat stress than heart rate. The World Health Organization recommends that body core temperature should not, under circumstances of prolonged daily work and heat, be permitted to exceed 38°C (100.4°F) rectally or 37.5°C (99.5°F) orally.2 Though this heat strain index may seem ideal, monitoring internal or core body temperature with rectal or esophageal probes is not acceptable to many workers. Oral temperatures, while easy to obtain, may be inaccurate measures of core temperatures because of mouth breathing or drinking hot or cold liquids immediately before using a thermometer. An ingestible capsule containing a temperature sensor and a device producing a telemetry signal is available to monitor real-time internal temperatures as the capsule passes through the gastrointestinal tract. Validation studies suggest that given appropriate time to exit the stomach, this method is an acceptable surrogate for rectal or esophageal temperature.16,17 Tympanic membrane temperature monitors may also provide an acceptable measurement of core temperature, but use of these monitors is uncommon because of ear discomfort and the need for a good seal in the ear canal. Mathematical models to predict core temperature and/or heat strain risk from noninvasive inputs have been developed; further validation and packaging in an end-user-friendly interface are necessary before they can be utilized in the occupational setting.18
Estimation of fluid loss or hydration status by regular weight measurements prior to work and throughout the day has also been proposed as an indicator of heat strain. Based upon weight measurements (assuming that the worker was fully hydrated before beginning work), the heat-exposed worker can be encouraged to drink liquids to maintain hydration and constant body weight throughout the day. Urine specific gravity measurements before, during, and after work have also been used to assess hydration status in workers. Weight loss of greater than 1.5% of body weight over the course of a normal shift may indicate that an individual is at greater risk of heat illness.14
ACGIH GUIDELINES
In the United States, the ACGIH guidelines are frequently used by industry to determine acceptable heat exposure for employees. These guidelines or threshold limit values (TLVs®) permit working conditions “that nearly all adequately hydrated, unmedicated, healthy workers may be repeatedly exposed without adverse health effects”.14 The International Organization for Standardization also provides guidance for use of the WBGT index and for estimating thermal strain using physiological measurements.19,20
The 2006 revision of the ACGIH heat stress and strain guidelines includes a decision tree for the assessment of a worker’s risk of heat stress (Figure 6.2). The previous ACGIH guidelines were similar to the NIOSH guidelines and recommended that workers in hot environments rest for a portion of each hour, with the amount of rest based upon WBGT index, level of activity, and acclimation status of the worker. The current ACGIH recommendations still use a “work–rest regimen” but expand the guidelines for work situations where heat stress conditions (e.g., use of encapsulating clothing) exceed the typical work–rest cycle recommendations.

FIGURE 6.2 Heat stress decision tree.
From American Conference of Governmental Industrial Hygienists, (ACGIH®), 2015 Threshold Limit Values (TLVs®) for Chemical Substances and Physical Agents and Biological Exposure Indices (BEIs®). Reprinted with permission.
In general, the ACGIH decision tree incorporates an assessment of the type of clothing worn, the level of environmental heat or WBGT index, an estimate of the worker’s physical activity, and an analysis of the work and work site. Table 6.4 provides work–rest cycles based upon the worksite WBGT index, work intensity, and worker acclimatization status. If the temperature index or work exceeds the limits outlined in Table 6.4, a detailed analysis of the heat stress potential of the work site, using a rationale model of core temperature, is required.20 If the detailed analysis reveals excessive heat stress, physiologic monitoring of the workers is needed. The reader should consult an experienced health professional and review the specific guideline documentation before attempting to implement these guidelines in the workplace.14
TABLE 6.4 Examples of permissible heat exposure threshold limit values: screening criteria for TLV and action limit for heat stress exposure.
| Allocation of work in a cycle or work and recovery | TLV (WBGT values in °C) | Action limit (WBGT values in °C) | ||||||
| Light | Moderate | Heavy | Very heavy | Light | Moderate | Heavy | Very heavy | |
| 75–100% | 31.0 | 28.0 | – | – | 28.0 | 25.0 | – | – |
| 50–75% | 31.0 | 29.0 | 27.5 | – | 28.5 | 26.0 | 24.0 | – |
| 25–50% | 32.0 | 30.0 | 29.0 | 28.0 | 29.5 | 27.0 | 25.5 | 24.5 |
| 0–25% | 32.5 | 31.5 | 30.5 | 30.0 | 30.0 | 29.0 | 28.0 | 27.0 |
See Table 6.3 for work demand categories.
WBGT values are expressed in °C and represent thresholds near the upper limit of the metabolic rate category.
If work and rest environments are different, hourly time-weighted averages (TWA) should be calculated and used. TWAs for work rates should also be used when the work demands vary within the hour.
Because of the physiologic strain associated with heavy and heavy work among less fit workers regardless of WBGT, criteria values are not provided for continuous work and for up to 25% rest in an hour. The screening criteria are not recommended, and a detailed analysis and/or physiologic monitoring should be used. From ACGIH®, 2015 TLVs® and BEIs® Book. Copyright 2015. Reprinted with permission.
NIOSH GUIDELINES
NIOSH has published a draft update to the 1986 “Criteria for a Recommended Standard Occupational Exposure to Hot Environments”.2 A system of work–rest cycles, similar to the ACGIH guidelines in Table 6.4, to prevent heat-related illnesses are presented. Work–rest time curves based upon WBGT index measurements and metabolic heat estimates were developed for unacclimatized and acclimatized workers; they are called recommended alert limits (RALs) and recommended exposure limits (RELs), respectively (Figures 6.3 and 6.4). The NIOSH RALs and RELs were developed for healthy workers who are physically and medically fit for their level of activity and who are wearing customary work clothes (i.e., a long-sleeved shirt and trousers).

FIGURE 6.3 Recommended heat stress alert limits for heat-unacclimatized workers. C = ceiling limit; RAL = Recommended Alert Limit. Calculations are for a standard worker of 70 kg (154 lb) body weight and 1.8 m2 (19.4 ft2) body surface.
Reproduced from National Institute for Occupational Safety and Health. Criteria for a recommended standard. Occupational exposure to hot environments. Revised criteria. DHHS (NIOSH) publication no. 86-113. Washington, DC: US Government Printing Office, 1986.
FIGURE 6.4 Recommended heat stress exposure limit for heat-acclimatized workers. C = ceiling limit; REL = Recommended Exposure Limit. Calculations are for a standard worker of 70 kg (154 lb) body weight and 1.8 m2 (19.4 ft2) body surface.
Reproduced from National Institute for Occupational Safety and Health. Criteria for a recommended standard. Occupational exposure to hot environments. Revised criteria. DHHS (NIOSH) publication no. 86–113. Washington, DC: US Government Printing Office, 1986.
NORMAL PHYSIOLOGY
Body core temperature is normally maintained in the range of 36.7–37°C (98–98.6°F) by oral measurement and 37.3–37.6°C (99–99.6°F) by rectal measurement. This narrow range of temperature control is maintained through the balance of heat production and conservation of metabolic heat in cold ambient conditions or the dissipation of metabolic heat to the environment in hot ambient conditions. When core temperature is elevated, active vasodilation of the cutaneous blood vessels and thermoregulatory sweating are initiated in order to facilitate heat dissipation. In humans, neurons in the preoptic area of the anterior hypothalamus, along with deep body temperature sensors, detect small changes in blood temperature. As the blood temperature rises, neurons in the hypothalamus activate the autonomic nervous system, which initiates circulatory, endocrine, and eccrine or sweat gland, responses to rid the body of excess heat.
Heat stress places demands on many body systems, primarily the cardiovascular and thermoregulatory systems, though the pulmonary, renal, and endocrine systems are also involved in the heat stress response. The cardiovascular system plays a prominent role in heat dissipation. As core temperature rises, the cutaneous active vasodilator mechanism initiates an increase in skin blood flow, which necessitates an increase in cardiac output. Cardiac output is redistributed so that less blood flow goes to internal organs and reducing the overall cardiovascular strain.21 To maintain blood pressure and blood flow to exercising muscles and vital organs while blood is being shunted to the skin, adequate hydration is essential. Sweat evaporation is the body’s primary method of heat loss. For each gram of sweat that evaporates from the skin, 0.58 kcal of heat is lost.22 Under heat strain conditions, the sweat glands can be stimulated to produce up to 2 liters per hour (L/h) in an acclimatized individual, and sweat rates of 1 L/h would not be unusual in industrial workers.2 Sweat rates this high cause significant loss of body water. Sweat rate is reduced in proportion to the magnitude of hypohydration, illustrating the importance of adequate fluid replacement during heat stress.23 Sweat also contains sodium, chloride, and potassium and can account for measurable losses of these electrolytes from the body.24
After repeated exposures to heat, physiological adaptations occur that improve heat dissipation and tolerance. This adaptation to heat stress, or heat acclimatization, occurs over 5–14 days with daily exercise in hot ambient conditions and of sufficient duration and level of exertion to raise body temperature and initiate vigorous sweating.22 Once acclimatized, a worker exposed to the same levels of heat will have a lower core temperature, a lower heart rate, and an increased volume of sweat that contains a lower concentration of sodium. The reduced sweat sodium concentration is the result of aldosterone-mediated reabsorption of sodium and chloride ions in the sweat glands. With acclimatization, sweat rates can increase from 0.6 to 2 L/h, and sodium chloride loss can decrease from 15–30 grams per day (g/day) to 3–5 g/day.22 Overall, the sodium loss is reduced to <5 g/day after acclimatization. The average American diet provides 8–14 g of salt each day, which is adequate for the acclimatized worker. Before acclimatization, while salt deficits may occur in heavily sweating workers, increasing dietary salt is rarely required.
Generally, physically fit workers are better able to tolerate heat, and they achieve acclimatization more rapidly than nonphysically fit workers. Physical fitness, independent of heat acclimatization status, enhances sweat secretion. The adaptations of heat acclimatization are rapidly lost when the worker leaves the heat stress environment. Workers who return to hot environments after more than a few days away from the job—especially those who return after an illness—should be allowed to reacclimatize to the hot environment before resuming full-time work, though evidence suggests that reacclimatization occurs more rapidly than the initial acclimatization.
Heat exchange
Heat exchange between the body and the environment is influenced by air temperature and humidity, skin temperature, air velocity, evaporation of sweat, radiant temperature, and the clothing worn.25 The heat balance equation describes the major modes of heat exchange or loss by the body (Table 6.5).
TABLE 6.5 Heat balance equation.
| S = (M ± W) ± (R + C) ± K − E |
| where: |
| S = storage, the amount of heat gained or lost by the body |
| (M ± W) = metabolism ± external mechanical work performed |
| (R + C) = combined radiative and convective heat gain or loss between the skin and the ambient air |
| K = heat gain or loss from conductive heat transfer |
| E = evaporative heat loss as sweat evaporates from the skin surface |
Calculated heat loss by radiation and convection is typically estimated from the skin-air thermal gradient. Consequently as Tdb approaches skin temperature, heat loss via R + C is diminished, and there is an increased reliance on evaporative heat loss. If Tdb exceeds skin temperature, heat will be gained rather than lost. Conductive heat exchange, where there is direct transfer of heat to air or objects in contact with the body, is rarely an important source of heat gain or loss in clothed workers in most occupational settings. However, conductive heat exchange may be an important mode of heat transfer for some workers, such as divers working in hot or cold water.
In addition to elevated ambient temperature, an increase in the water vapor content of the air and clothing will limit heat dissipation to the environment. Relative humidity is the most common way of expressing water vapor content of the air, but comparisons between different levels of humidity are appropriate only when the air temperature is the same. The evaporation of sweat is dependent on the vapor pressure gradient between the skin and the air, which is temperature dependent. As an example, the vapor pressure of air at 30°C, 40%RH, is approximately equal to that at 40°C, 20%RH. Clothing insulates the body from heat loss via radiation, and convection will also serve as a barrier to the evaporation of sweat. Protective clothing, especially sweat-impermeable clothing, which effectively eliminates any body cooling from sweat evaporation, places workers at significantly greater risk for heat strain and heat-related illnesses.
Numerous acute and chronic medical conditions, medications, and individual characteristics may diminish the body’s ability to tolerate heat stress and dissipate internal heat (Table 6.6).26 Dehydration from any cause, whether due to increased sweating or associated with underlying illness, fever, vomiting, or diarrhea, increases the risk of hyperthermia. Many medications, especially antihypertensive or cardiac medications that affect the cardiovascular or renal systems or medications with anticholinergic effects on sweat glands, may alter a worker’s physiologic responses to heat and therefore increase the risk of heat illness. Previous heat-related illness, especially heatstroke, has historically been considered an indicator of both heat intolerance and a possible underlying defect in the individual’s thermoregulatory system. One investigation of 10 individuals with previous exertional heatstroke found that nine of them readily acclimatized to heat while one displayed evidence of persistent heat intolerance for almost 1 year following heatstroke. The investigators concluded that a small percentage of individuals with previous heatstroke may be heat intolerant.27
TABLE 6.6 Risk factors predisposing to heat disorders.
| Individual factors |
| Increased age |
| Obesity |
| Lack of acclimatization |
| Use of water-impermeable/heavy clothing |
| Fatigue/sleep deprivation |
| Underlying medical conditions/states |
| Dehydration |
| Infection/fever/recent immunization |
| Overuse of ethanol |
| Diseases |
| Cardiovascular disease |
| Renal disease |
| Hyperthyroidism |
| Diabetes mellitus |
| Parkinson’s disease |
| Skin conditions limiting sweating, including sunburn |
| Previous heat disorder |
| Pesticide poisoning |
| Drugs |
| Medications with anticholinergic effects |
| Antispasmodics |
| Tricyclic antidepressants |
| Psychotropics |
| Antihistamines |
| Antihypertensive medications |
| Diuretics |
| Stimulants (decongestants, amphetamine, cocaine) |
PATHOPHYSIOLOGY OF ILLNESS AND TREATMENT
The spectrum of heat-related disorders ranges from relatively harmless illnesses such as various skin conditions and heat cramps to serious heat illnesses, which represent a continuum of severity from heat exhaustion to potentially fatal heatstroke.26
Heat-related skin conditions
Heat rash, or miliaria, is caused by sweat duct obstruction and resultant sweat retention within the sweat gland. Obstruction of the sweat duct leads to duct rupture and an inflammatory reaction surrounding the duct. Because the rupture of the sweat ducts may occur within different layers of the skin, three forms of miliaria—crystalline, rubra, and profunda—are described.28
Miliaria crystallina is a mild, asymptomatic skin condition consisting of small, clear vesicles resulting from sweat duct rupture within the surface layers of skin. Small erythematous macules resulting from sweat duct rupture within the middle layers of the skin and associated with burning and itching is known as miliaria rubra or “prickly heat.” Miliaria rubra commonly affects the skin of the trunk and intertriginous areas of the body. Extensive cases of miliaria rubra involving large numbers of sweat glands can impede body heat dissipation and contribute to more severe heat-related illness.29 Miliaria profunda results from sweat duct rupture deep within the skin. The lesions, which usually appear only after prolonged periods of miliaria rubra, are small, white to flesh-colored papules and occur most commonly on the trunk. Sunburned skin and occlusive clothing that precludes the free evaporation of sweat increase the risk of all forms of miliaria. Treatment involves reducing sweating in the affected individual and keeping the skin cool and dry. In workers whose jobs require sweat-impermeable protective clothing, the treatment of miliaria may include a temporary transfer to a job not requiring protective clothing or into an air-conditioned workspace. Miliaria rubra usually resolves within a week. Complete resolution of miliaria profunda may take several weeks in a cool environment.
Heat edema
Heat edema is often not considered a true heat-related disorder. It is a rather a common condition in which the extremities swell during the first 7–10 days of exposure to higher temperatures. Typically it is found in unacclimatized individuals, often women or military trainees, who stand or sit for long periods during hot weather and is not associated with cardiac or renal impairment. The etiology of heat edema is uncertain, but it may involve local vasomotor changes or be associated with changes in aldosterone activity.24 It is sometimes prominent in pregnancy, when heat can aggravate the underlying condition of pregnancy-associated edema. Heat edema usually resolves spontaneously within a few days as the individual acclimatizes. Diuretic therapy does not provide significant relief and is not indicated. Symptomatic treatment—elevation of the legs, compression stockings, and gradual exposure to heat—is generally all that is required.
Heat cramps
Heat cramps are painful muscle spasms that occur during or following intense physical exercise in hot environments. The affected individual is usually acclimatized to heat and gives a history of heavy exertion in the heat, profuse sweating, drinking large quantities of water, and minimal salt or electrolyte replacement. Inadequate electrolyte replacement is probably associated with the underlying mechanism responsible for the muscle spasm.24,30
The muscles involved in the spasm are usually the same muscles used during the preceding exercise, such as the abdominal muscles or the large muscles of the thigh. Heat cramps may be heralded by fasciculations, and while multiple muscle spasms may occur simultaneously, usually only a small section of the muscle is involved. Individual heat-induced muscle spasms last less than a minute; but if untreated, attacks of intermittent heat cramps may last for 4–8 hours.
Heat cramps respond to rest in a cool place and ingestion of 0.1% saline solution (one teaspoon of salt in a quart of water) or fluids containing electrolytes. Salt tablets should not be given. If nausea and vomiting preclude administration of oral solutions, intravenous electrolyte solutions may be necessary. Heat cramps can be prevented by ensuring that workers, especially acclimatized workers, maintain adequate dietary salt intake in addition to adequate fluid replacement.
Heat syncope
Heat syncope occurs in individuals who stand for prolonged periods, who make sudden postural changes, or who exercise strenuously in the heat. The underlying mechanism of heat syncope is similar to that of orthostatic syncope. Venous return to the heart is reduced by pooling of blood in dependent extremities or in dilated peripheral vessels, and cardiac output is inadequate to maintain cerebral circulation and consciousness. Heat syncope is not associated with elevated body temperature, and the syncope victim may remember a typical prodrome of nausea, sweating, and dimming of vision before loss of consciousness. Following syncope and falling to a recumbent position, consciousness returns rapidly. Heat syncope is generally a benign “faint.” The primary health concern is the potential for falling and injury, especially for workers on roofs and scaffolding.
Following an episode of heat syncope, the worker should be allowed to recover in a cool area. To ensure that he or she has not been injured by the fall, a medical examination should be performed. The employer should make sure that the worker is properly hydrated and acclimatized before returning to a job that requires heavy exertion or standing in a hot environment.
Heat exhaustion
Heat exhaustion is a mild to moderate illness characterized by an inability to sustain cardiac output during strenuous work or exercise in the heat that is necessary to meet the combined demands of blood flow for metabolic and thermoregulatory requirements.15 The signs and symptoms include weakness, ataxia, fatigue, headache, nausea, hypotension, tachycardia, and transient alterations in mental status. Since the symptoms of heat exhaustion are similar to those of early heatstroke, all heat exhaustion victims must be evaluated to eliminate the diagnosis of heatstroke (see Heat Stroke below). Heat exhaustion occurs more commonly in workers who are unacclimatized to heat and who are without adequate water and salt replacement. Treatment of heat exhaustion must be individualized based upon the severity of the presenting symptoms and the underlying cause. Mild heat exhaustion may be treated by having the worker rest in a cool area and providing oral fluid and salt replacement. Severe cases of heat exhaustion—especially severe water-depletion type requiring intravenous fluids—need to be referred to an emergency room for careful replacement of body water. Timing of return to work after heat exhaustion has not been fully studied, but it seems prudent to allow at least 24–72 hours for full rehydration and correction of electrolyte abnormalities before the individual returns to work.
Hyponatremia occurs when electrolyte replacement is insufficient and/or fluid replacement is overly aggressive and can lead to potentially serious and sometimes fatal outcomes. Exercise- or work-related hyponatremia is due to overdrinking, both in absolute (related to total volume consumed) and relative (related to sodium loss via sweating) terms.31 In the occupational setting, as hyponatremia rarely occurs, specific prevention measures beyond encouraging appropriate fluid replacement and consumption of salt-containing foods are not necessary.
Heat injury and heatstroke
Heat injury is a moderate to severe illness characterized by tissue (muscle and gut) and organ (liver, renal) injury resulting from work or exercise during heat exposure.26 Individuals with exertional heat injury do not demonstrate sufficient neurological abnormalities to meet the usual definition of heatstroke. Organ and tissue damage may not manifest early in the presentation of heat injury, making it difficult to distinguish it from heat exhaustion, and a thorough clinical evaluation, including assessment of possible organ damage, is necessary.15
Heatstroke is a life-threatening medical condition. Symptoms include altered mental status and rectal temperatures are often but not always >40°C (104°F).26 However, core temperature >40°C should not be used as a universal diagnostic criteria, as well-conditioned individuals can have core temperatures above this threshold yet remain asymptomatic of heat illness.32,33 During physical work in the heat, skin blood flow is high, reducing perfusion of the intestines and other viscera, which can result in ischemia, endotoxemia, systemic inflammatory response, and multiorgan damage.
Heatstroke requires immediate, aggressive cooling of the affected individual. Classic heatstroke occurs during summer heat waves predominantly in infants or elderly individuals. The condition is most common in poor and/or elderly individuals who take medications for underlying medical conditions and live in poorly ventilated housing without air conditioning. After days of hot, humid environmental conditions, their ability to maintain body heat balance fails, and heatstroke occurs. A second form of heatstroke, exertional heatstroke, occurs in workers, athletes, or military recruits who perform vigorous exercise in hot, humid conditions and is the focus of this section. Mental status changes are the predominant initial presenting symptom. Heatstroke victims may present with any form of mental status change ranging from irrational behavior, poor judgment, and confusion to delirium, seizures, and coma. Sweating, characteristically absent in classic heatstroke, may be present in exertional heatstroke. The rectal temperature is often >40°C (104°F) and may be much higher; the pulse is elevated; the blood pressure is normal or low; and hyperventilation is common. Nausea, vomiting, and diarrhea may be present.
Initial laboratory findings often include proteinuria, with red blood cells and granular casts also present in the urine, an elevated white blood cell count, and a decreased platelet count. Serum electrolyte levels will vary with level of hydration, acid–base status, and underlying tissue damage. Serum enzymes—lactic dehydrogenase, creatinine phosphokinase, aspartate aminotransferase, and alanine aminotransferase are characteristically elevated. With hyperventilation, respiratory alkalosis may be present; but in exertional heatstroke, lactic acidosis may be the presenting acid–base abnormality. Abnormalities of blood clotting consistent with disseminated intravascular coagulation—including decreased fibrinogen, prolonged prothrombin time and partial thromboplastin time, and elevated levels of fibrin split products—may be present on initial evaluation.
The treatment for all heatstroke victims is immediate initiation of cooling and appropriate resuscitation. The method of cooling used in military settings is immersion of the victim in ice water or wrapping the victim in wet sheets. Even though this type of cooling will cause cutaneous vasoconstriction and shivering, thereby decreasing conductive heat loss and increasing metabolic heat formation, it is still probably the most effective method of cooling outside of a healthcare facility. Rapid cooling to a core temperature <38.3°C (101°F) has been associated with no mortality and an attenuation of organ damage.34,35 Other rapid cooling methods used for heatstroke include packing the individual in ice or applying ice packs and/or spraying with cold water. Once cooling has been initiated, the victim should be transferred immediately to a hospital for continuous monitoring of core temperature and definitive care. Endotracheal intubation and invasive cardiovascular monitoring are often needed during resuscitation and follow-up care.
The severity of sequelae and mortality in heatstroke is determined by the degree and duration of the elevated temperature. After initial resuscitation of an individual with heatstroke, failure or disruption of the function of multiple organ systems is common and should be expected. Frequent sequelae to heatstroke include liver function abnormalities, disseminated intravascular coagulation, rhabdomyolysis, and acute renal failure.24 Other reported complications of heatstroke include pancreatitis, pulmonary edema, myocardial infarction, and central and peripheral nervous system damage.
MEDICAL SURVEILLANCE
Medical surveillance of heat-exposed workers is one aspect of the overall prevention of heat-related illness. Preplacement and periodic medical examinations of heat-exposed workers should ensure that they can meet the total demands and stresses of the hot job environment without putting their safety and health or that of fellow workers in jeopardy.2 The components of the preplacement and periodic medical examinations recommended by NIOSH are provided in Table 6.7. There are no strict guidelines to identify which heat-exposed workers require medical surveillance. An initial medical history may be taken on all heat-exposed workers to identify those at risk for heat illness. The initial history should elicit information about underlying medical conditions, use of prescription and over-the-counter medications, and previous episodes of heat-related illness. Workers may not require regular medical surveillance if they (i) do not have medical conditions that increase their risk of heat injury, (ii) are not exposed to heat above recommended guidelines, and (iii) are properly trained in the prevention of heat-related illness. Special categories of workers likely to be exposed to extreme heat stress conditions, such as hazardous waste site workers who wear heavy protective clothing and respirators, should be screened carefully before placement and should receive periodic medical surveillance.
TABLE 6.7 NIOSH recommended medical surveillance for heat-exposed workers.
Source: National Institute for Occupational Safety and Health. Criteria for a Recommended Standard: Occupational Exposure to Heat and Hot Environments: Revised Criteria 2013. Centers for Disease Control and Prevention; 2013:1–184.
| Pre-placement medical evaluation | Periodic medical evaluation | ||
| Component | Special emphasis on | Component | Special emphasis on |
| History | History | ||
| Occupational | Previous heat exposure jobs | Occupational | Changes in job or personal protective equipment |
| Use of personal protective equipment | |||
| Medical | Diseases of the following systems: cardiovascular, respiratory, endocrine, gastrointestinal, dermatologic, renal, neurologic, hematologic, reproductive | Medical | Change in health status |
| Symptoms of heat strain | |||
| Personal habits | Alcohol and drug use | Personal habits | Update |
| Medications | Prescription and over the counter | Medications | Update |
| Characteristics | Height, weight, gender, age | Characteristics | Update |
| Direct evaluation | Direct evaluation | ||
| Physical examination | Cardiovascular, respiratory, nervous and musculoskeletal systems | Physical examination | Systems emphasized in pre-placement examination |
| Skin | |||
| Blood pressure | Blood pressure | ||
| Clinical chemistry tests | Fasting blood glucose | Clinical chemistry tests | Fasting blood glucose |
| Blood urea | Blood urea | ||
| Serum creatinine Serum electrolytes | Serum creatinine Serum electrolytes | ||
| Hemoglobin | Hemoglobin | ||
| Urinary sugar and protein | Urinary sugar and protein | ||
| Mental status | Assessment of worker’s ability to understand heat, | Mental status | Reassessment of ability to understand heat |
| Communicate and respond to emergencies | |||
| Detailed medical evaluation | Cardiovascular disease | Detailed medical evaluation | Based upon changes in health |
| Pulmonary disease | |||
| Medication use which might interfere with heat tolerance or acclimatization | |||
| Hypertension | |||
| Need to use respiratory protection | |||
| History of skin disease that may impair sweating | |||
| Obesity | |||
| Women with childbearing potential | |||
Return to Work Considerations
Return to work/play guidelines are often “common sense” recommendations based on a return to normal laboratory parameters and an asymptomatic state.36 Recent data indicates that these criteria may not be appropriate, as tissue damage and/or impaired organ function may persist after the individual appears to have recovered. Biological markers of exertion heat illness (EHI) severity are lacking; however, recent evidence from a rat model of heatstroke suggests that there are novel patterns of core temperature responses to mild, moderate, and severe pathophysiology that may assist in the differential diagnosis. Additionally, associations between hemodynamic changes during heat exposure, high circulating cardiac troponin I levels, and histopathological changes in cardiac muscle during recovery were identified.37 Whether similar or other biomarkers of EHI severity and/or recovery exist in humans remains to be determined.
The return-to-play recommendations from the American College of Sports Medicine are to refrain from exercise for 1 week after release from medical care, with follow-up examination, testing, and imaging as appropriate prior to resuming exercise. Work intensity, duration, and heat stress should be gradually increased until tolerance to vigorous exercise in the heat has been demonstrated. Development of clinical aids and/or biomarkers of EHI injury severity and recovery are necessary, as well as determination of the long-term health consequences, if any, of exertional heatstroke.
HEAT EXPOSURE AND REPRODUCTION
Physiologic and hormonal changes during early pregnancy are associated with a slight increase in maternal resting core temperature; however, there is no evidence that a pregnant woman’s ability to eliminate excess heat is diminished. In fact, physiologic adaptations during pregnancy—increase in blood volume, increase in cardiac output and resting pulse rate, and increase in cutaneous blood flow—appear to offset the increased metabolic heat load associated with pregnancy.38,39 In one study, physically fit pregnant women appeared to maintain thermoregulation during exercise throughout their pregnancy at least as well as nonpregnant women.38 During the late third trimester of pregnancy, decreased venous return, due to the size of the uterus, may compromise cardiac output in the pregnant worker and impair heat tolerance.
In experimental animal studies on a variety of species, hyperthermia has been found to be teratogenic.2 Early in the gestation, excessive heat exposure in animals is associated with structural defects, predominantly of the central nervous system and skeleton, and embryo death. Heat stress in animals later in gestation has been associated with retarded fetal growth and postnatal neurobehavioral defects. Studies of the effect of hyperthermia on the developing human fetus have been primarily concerned with the effect of illness-related fever during pregnancy. The results of these studies have been inconsistent. Some investigators have reported an association between maternal fevers of 38.9°C (102°F) and abnormal fetal development, whereas others found no association between maternal hyperthermia and adverse pregnancy outcomes. Heat exposure, in addition to its possible effects on female reproduction, is associated with decreases in sperm count and motility in male workers.40 Considering the potential for reproductive effects due to heat in men and women, preventive measures to limit excessive heat exposures are essential for all workers.
PREVENTION
The prevention of heat-related illnesses and conditions of unacceptable heat stress can be categorized into four basic areas of control: (i) engineering controls, (ii) administrative controls, (iii) work practices controls, and (iv) protective clothing and devices.2 Table 6.8 summarizes these prevention measures. Engineering controls, such as shielding and increased air movement, are the most desirable preventive measures. However, they are not effective in many outdoor work sites or work sites requiring full protective clothing. In these cases, administrative and work practices controls—such as reducing heat exposure, reducing work rates, enhancing fitness and heat tolerance, and offering special heat safety training—should be utilized to the fullest extent possible. Adequate fluid replacement in the heat-exposed worker is critical. The sensation of thirst has been proven to be inadequate to prevent hypohydration in heavily sweating individuals. Therefore, workers need to be encouraged to drink adequate amounts of liquid to replace sweat losses. Any water or beverage provided for workers should be cool (10–15°C or 50–59°F) and should be consumed in small volumes. In the acclimatized worker, sweat rates of 1 L/h are possible, and fluid replacement with approximately 5–7 oz every 15–20 minutes approximates fluid losses. Maximum gastric emptying in exercising individuals is 1–1.5 L/h; therefore, larger volumes of fluid are not effective.41 Overhydration and resultant hyponatremia, while rare, have been reported in marathon runners.42 Numerous carbohydrate and electrolyte solutions are marketed for fluid replacement in athletes and workers. Studies have shown that the addition of carbohydrates and electrolytes to fluids may be beneficial for athletes who exercise strenuously for long periods.41 For acclimatized workers whose diet includes sufficient calories and salt, water alone should provide adequate fluid replacement. Because of their diuretic effect, caffeinated beverages should be discouraged as a primary source of fluid replacement.
TABLE 6.8 Heat strain/heat-related illness prevention.
Source: National Institute for Occupational Safety and Health. Criteria for a Recommended Standard: Occupational Exposure to Heat and Hot Environments: Revised Criteria 2013. Centers for Disease Control and Prevention; 2013:1-184.
| Engineering controls |
| Decrease convection heat gain by worker |
| Cool air temperature to below mean skin temperature |
| Increase air movement (if ambient temperature ≤ skin temperature) |
| Decrease radiant heat gain by worker |
| Insulate hot surfaces |
| Use shielding between worker and heat source |
| Increase evaporative heat loss by worker |
| Eliminate humidity sources (steam leaks, standing water) |
| Decrease air humidity (ambient water vapor pressure) |
| Increase air movement |
| Administrative and work practices controls |
| Limit workers’ exposure to hot working environment |
| Use appropriate environmental monitoring |
| Work during cool parts of day or in the shade |
| Schedule hot work for cool seasons |
| Provide cool rest areas |
| Increase the number of workers for a given job |
| Use recommended work/rest regimens |
| Decrease the metabolic heat load |
| Mechanize heavy work when possible |
| Rotate heavy work over entire workforce or increase workforce |
| Decrease shift time; allow liberal work breaks; restrict overtime |
| Enhance tolerance to heat |
| Encourage physical fitness in workers |
| Require minimum level of fitness in certain jobs |
| Use heat acclimatization program for new workers or |
| workers returning from vacations, layoffs, or illness |
| Encourage regular fluid and salt replacement |
| Avoid conditions increasing risk to heat strain |
| Health and safety training for supervisors and workers |
| Recognize signs and symptoms of heat intolerance |
| Emphasize acclimatization, fluid and salt replacement |
| Avoid conditions increasing risk of heat strain |
| Use control methods to prevent heat strain |
| Use protective clothing |
| Use buddy system, if applicable |
| Medical screening of workers with heat intolerance |
| Establish heat alert program |
| Establish heat alert committee |
| Reverse plant winterization measures |
| Ensure water sources, fans and air conditioners are working |
| Ensure that medical department is prepared to treat heat casualties |
| Establish criteria for heat alerts |
| Take all appropriate preventive measures during heat alerts |
| Post signs identifying heat hazard areas |
| Protective clothing and auxiliary body cooling |
| Water-cooled garments |
| Air-cooled garments |
| Ice-packet vests |
| Wetted overgarments |
| Aluminized overgarments |
Personal protective equipment can be very effective in prolonging intervals of heat exposure. Ice-packet vests are the least cumbersome items to wear because they require no connection to an external device to provide cooling air or water. At work sites where radiant heat sources are the primary exposure problem, aluminized suits are a good choice because they reflect heat.
References
- 1. Dukes-Dobos FN. Hazards of heat exposure: a review. Scand J Work Environ Health 1981;7(2):73–83.
- 2. Jacklitsch B, Williams WJ, Musolin K, et al. 2016. NIOSH criteria for a recommended standard: occupational exposure to heat and hot environments. Cincinnati, OH: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, DHHS (NIOSH) Publication 2016-106. Available at: https://www.cdc.gov/niosh/docs/2016-106/pdfs/2016-106.pdf (accessed on June 28, 2016).
- 3. Department of Labor. OSHA Technical Manual OSHA, ed. Washington, DC: Occupational Safety & Health Administration; 1999.
- 4. Centers for Disease Control and Prevention. Heat-related deaths after an extreme heat event—four states, 2012, and United States, 1999–2009. Morb Mortal Wkly Rep 2013;62(22):433–6.
- 5. Arbury S, Jacklitsch B, Farquah O, et al. Heat illness and death among workers—United States, 2012–2013. Morb Mortal Wkly Rep 2014;63(31):661–5.
- 6. Choudhary E, Vaidyanathan A. Heat stress illness hospitalizations: environmental public health tracking program, 20 states, 2001–2010. MMWR Surveill Summ 2014;63(13):1–10.
- 7. Donoghue AM, Sinclair MJ, Bates GP. Heat exhaustion in a deep underground metalliferous mine. Occup Environ Med 2000;57(3):165–74.
- 8. Minard D, Belding HS, Kingston JR. Prevention of heat casualties. J Am Med Assoc 1957;165(14):1813–8.
- 9. Carter R, III, Cheuvront SN, Williams JO, et al. Epidemiology of hospitalizations and deaths from heat illness in soldiers. Med Sci Sports Exerc 2005;37(8):1338–44.
- 10. Wallace RF, Kriebel D, Punnett L, et al. Risk factors for recruit exertional heat illness by gender and training period. Aviat Space Environ Med 2006;77(4):415–21.
- 11. International Organization for Standardization (ISO). ISO 7726, 1998 Ergonomics of the Thermal Environment: Instruments for Measuring Physical Quantities. Geneva: ISO; 1998.
- 12. Parsons K. Human Thermal Environments. London and New York: Taylor & Francis; 2003.
- 13. Yaglou CP, Minard D. Control of heat casualties at military training centers. AMA Arch Ind Health 1957;16(4):302–16.
- 14. American Conference of Governmental Industrial Hygienists. 2014 Threshold Limit Values for Chemical Substances and Physical Agents and Biological Exposure Indices. Cincinnati, OH: American Conference of Governmental Industrial Hygienists; 2014:206–24.
- 15. Department of the Army. TB MED 507 Heat stress control and heat casualty management. Washington, DC: Department of the Army and Air Force; 2003. TB MED 507/AFPAM 48–152.
- 16. Byrne C, Lim CL. The ingestible telemetric body core temperature sensor: a review of validity and exercise applications. Br J Sports Med 2007;41:126–33.
- 17. Goodman DA, Kenefick RW, Cadarette BS, et al. Influence of sensor ingestion timing on consistency of temperature measures. Med Sci Sports Exerc 2009;41(3):597–602.
- 18. Buller MJ, Latzka WA, Yokota M, et al. A real-time heat strain risk classifier using heart rate and skin temperature. Physiol Meas 2008;29(12):N79–85.
- 19. International Organization for Standardization (ISO). ISO 7243, 2003, Hot Environments: Estimation of the Heat Stress on Working Man, Based on the WBGT-Index (Wet Bulb Globe Temperature). Geneva: ISO; 2003.
- 20. International Organization for Standardization (ISO). ISO 9886, 2004, Ergonomics: Evaluation of Thermal Strain by Physiological Measurements. Geneva: ISO; 2004.
- 21. Rowell LB. Human Circulation: Regulation During Physical Stress. New York: Oxford University Press; 1986.
- 22. Sawka MN, Young AJ. Physiological systems and their responses to conditions of heat and cold. In: Tipton CM, ed. ACSM’s Advanced Exercise Physiology. Baltimore, MD: Lippincott Williams and Wilkins; 2006:535–63.
- 23. Sawka MN, Young AJ, Francesconi RP, et al. Thermoregulatory and blood responses during exercise at graded hypohydration levels. J Appl Physiol 1985;59(5):1394–401.
- 24. Knochel JP. Heat stroke and related heat stress disorders. Dis Mon 1989;35(5):301–77.
- 25. Gagge AP, Gonzalez RR. Mechanisms of heat exchange: biophysics and physiology. In: Handbook of Physiology: Environmental Physiology. Vol 1. New York: Oxford University Press; 1996:45–84.
- 26. Winkenwerder W, Sawka MN, Goldman L, et al. Disorders due to heat and cold. In: Cecil Medicine. Vol 2, 3rd ed. Philadelphia, PA: Saunders Elsevier; 2007:763–7.
- 27. Armstrong LE, De Luca JP, Hubbard RW. Time course of recovery and heat acclimation ability of prior exertional heatstroke patients. Med Sci Sports Exerc 1990;22(1):36–48.
- 28. Kanerva L. Physical causes and radiation effects. In: Adams R, ed. Occupational Skin Diseases. 3rd ed. Philadelphia, PA: WB Saunders; 1999:47–8.
- 29. Pandolf KB, Griffin TB, Munro EH, et al. Heat intolerance as a function of percent of body surface involved in miliaria rubra. Am J Physiol Regul Integr Comp Physiol 1980;239:R233–40.
- 30. Eichner ER. Heat cramps in sports. Curr Sports Med Rep 2008;7(4):178–9.
- 31. Sawka MN, Leon LR, Montain SJ, et al. Integrated physiological mechanisms of exercise performance, adaptation, and maladaptation to heat stress. Compr Physiol 2011;1:1883–928.
- 32. Ely BR, Ely MR, Cheuvront SN, et al. Evidence against a 40°C core temperature threshold for fatigue in humans. J Appl Physiol 2009;107(5):1519–25.
- 33. Byrne C, Lee JK, Chew SA, et al. Continuous thermoregulatory responses to mass-participation distance running in heat. Med Sci Sports Exerc 2006;38(5):803–10.
- 34. O’Brien KK. Case studies of exertional heat injury/stroke in military populations. Med Sci Sports Exerc 2003;35:S3.
- 35. Gaffin SL, Gardner JW, Flinn SD. Cooling methods for heatstroke victims. Ann Intern Med 2000;132(8):678.
- 36. O’Connor FG, Casa DJ, Bergeron MF, et al. American College of Sports Medicine Roundtable on exertional heat stroke–return to duty/return to play: conference proceedings. Curr Sports Med Rep 2010;9(5):314–21.
- 37. Quinn CM, Duran RM, Audet GN, et al. Cardiovascular and thermoregulatory biomarkers of heat stroke severity in a conscious rat model. J Appl Physiol (1985) 2014;117(9):971–8.
- 38. Jones RL, Botti JJ, Anderson WM, et al. Thermoregulation during aerobic exercise in pregnancy. Obstet Gynecol 1985;65(3):340–5.
- 39. Vaha-Eskeli K, Erkkola R, Seppanen A. Is the heat dissipating ability enhanced during pregnancy? Eur J Obstet Gynecol Reprod Biol 1991;39(3):169–74.
- 40. Thonneau P, Bujan L, Multigner L, et al. Occupational heat exposure and male fertility: a review. Hum Reprod 1998;13(8):2122–5.
- 41. Gisolfi CV, Duchman SM. Guidelines for optimal replacement beverages for different athletic events. Med Sci Sports Exerc 1992;24(6):679–87.
- 42. Frizzell RT, Lang GH, Lowance DC, et al. Hyponatremia and ultramarathon running. JAMA 1986;255(6):772–4.
