4. Lifesaving Hacks: Whirring Hearts, Printed Organs, and Miraculous Medicine
At some point in your life, it’s a simple fact you’re going to get sick. It might be as simple as the common cold, in which case it’ll probably be best if you curl up with a bowl of delicious, genetically engineered chicken soup and a good personally customized nasal spray, loaded with a cold-killing payload of nanobots. That will be the trick in a few years.
Of course the number one killer of Americans today is heart disease. So you can be sure that people you know and love will likely deal with heart issues in their lives. You might be one of them. Let’s face it, there’s a good chance you might end up on an operating table with your chest splayed open getting your heart replaced by a jet engine.
Wait, what?
Yeah, that’s for real. We will get back to that in a bit.
As with many other areas of life, technology has inserted itself firmly into the world of medicine, a process going back thousands of years, back to the time when the first caveman dabbed some mud onto a bug bite and invented the health spa. Okay, that last fact might have been completely fabricated, but it is true that humans have made many breakthroughs in health technology along the way, including surgery, the invention of pharmaceuticals, and eventually designing new organs and body parts out of metal, plastic, and a meat-spraying inkjet printer.
I know we are probably freaking you out here, but it’s all about to come true. Go take bathroom break because this chapter will not work for you on a full bladder. And we don’t want you to tinkle on yourself.
When we considered what to include in this chapter, there was an almanac full of diseases and conditions that are being remedied by incredible new medical technologies that we could have included. Breakthroughs in cancer treatments and associated tumor fighting therapies alone could fill an entire book.
Instead, we looked at the number-one killer of Americans: Heart disease. And how an amazing team of researchers came together to develop an artificial heart that could save a half-million American lives every year. And millions worldwide.
We will tell how the “jet engine heart,” developed by a team that includes Australian researcher Daniel Timms and Americans Bud Frazier and Billy Cohn of the Texas Heart Institute, came to be.
It is just one miraculous story driven by accelerating technology improvement. But we also examine the macrotrends that are driving cancer therapies, organ replacement, and diseases that would otherwise kill the humans they plague. Those breakthroughs, within nanotechnology, genetics, and robotics, are revolutionizing medicine today.
First, let’s take a peek at the medical past.
A Brief History of Medicine
The basics with your health are generally pretty well understood today. If you are feeling sick, you pop into the pharmacy for some medicine, and if your illness is somewhat worse, you see your doctor for stronger measures (usually drugs). If you are really, really sick, a specialist is likely in your future. They will do their best to fix up anything going wrong inside you, usually using a surgical procedure.
There’s nothing new here. There is evidence people knew how to suture wounds all the way back into prehistoric times, and that humans were aware of surgical intervention as early as 12,000 b.c.e.
That ancient intervention, by the way, was called trepanation, which was the opening of a hole in your skull to relieve pressures inside the head caused by other injuries or illness. As you can imagine, surgical instruments in 12,000 b.c.e. weren’t exactly state-of-the-art, so opening a hole into the skull sometimes meant actually scraping a hole into the skull with a rock. We are no doctors, but common sense says you’d probably want to avoid a procedure like this.
Ancient procedures also included tooth drilling more than 10,000 years ago. There’s further evidence of dental surgery in Egypt 5,000 years ago. There’s even ancient evidence of splinting broken bones.
You are probably familiar with the Hippocratic Oath—especially the section that apparently says “above all, do no harm.” (As an aside, this actual quote doesn’t appear in the Ionic Greek version, and is attributed to a 19th century surgeon). Thematically, however, the oath and modern updates of it support its intention.
Still, Hippocrates, for whom the oath was named, is considered the father of western medicine. Born in Greece in 460 b.c.e., he formalized some of the rules and ethics of medicine—no longer was it acceptable to gouge someone’s head with a rock to relieve pressure in the skull.
Hippocrates espoused a theory that medical ailments were caused by your lifestyle and not because the gods had cursed you. This allowed doctors to treat patients using a diagnosis based on observation, rather than superstition.
“Hippocrates espoused a theory that medical ailments were caused by your lifestyle and not because the gods had cursed you.”
One of the major side effects of cutting holes into people is that it really, really hurts, so it’s no surprise that for the last few thousand years, people have been trying to find ways to dull the pain when undergoing such procedures. This meant herbal concoctions of varying effectiveness, and good old alcohol, opium, and related narcotics. There’s also the case of early medicine men in Peru spitting into wounds after chewing a mouthful of coca leaves. In the 1800s, this technique was refined somewhat by distilling the coca leaves into cocaine.
For major procedures, most people prefer to be rendered unconscious. Apparently, people agreed with this principle as far back as the 1100s, when Arab surgeons would knock their patients out with a sponge soaked in an opium cocktail (that’d be opium, hemlock, and mandrake with a twist of lime).
It was during the eighteenth and nineteenth centuries when general anesthesia started to gain traction. This happened with the refinement of nitrous oxide (aka laughing gas, the funniest general anesthetic), and the introduction of morphine and chloroform. Eventually, that led to the modern complement of gases and painkillers that knock us out before surgery today, and then keep us numb throughout the procedure.
In the late 1800s, morphine was one of the key pharmaceutical agents used to help people control pain during and after surgery. One problem: it was wickedly addictive. So scientists got to work on a new non-addictive painkiller to use in place of morphine. The result was a drug called diamorphine, which has since become better-known by the trademark name Bayer gave it: Heroin. Oops!
The funny thing, though, is that it’s not so much the surgery that’ll kill you as it is the germs. No matter how skilled your surgeon is, bacteria can get into your incisions and cause terrible infections that can kill you in an equally nasty way.
There have been some attempts to counteract infections through the ages, but it wasn’t until Alexander Fleming discovered penicillin in 1928 that there was a truly recognized pharmaceutical option. This was the real start of the antibiotic revolution, and shortly thereafter, there were specific formulations that would tackle post-surgery infections, tuberculosis, and other bugs that kept people from recovering from surgeries. Antiviral medicines followed, and rather than killing the viruses outright (as an antibiotic would kill bacteria), antivirals rather prevented viruses from reproducing themselves, halting their spread.
Now, of course, today there’s a wide variety of consumer products featuring antimicrobial properties, from over-the-counter medicines to hand soaps to footwear. In the past, if you got a tiny little cut on your finger, you could get a massive infection and lose your arm ... you could even die. Now, you head down the block to the pharmacy and buy a tube of Polysporin for a few dollars, and soon enough you’re back to chopping onions as if nothing happened.
Ultimately, keeping people from dying from complications due to small nicks, cuts, and large-scale incursions like modern surgery is what brought us into the medical modern age, allowing us to do even bigger and better things.
There’s a Future in Plastics
It’s hard to overstate the effect of the introduction of plastic on the world of medicine. For the longest time, most medical instruments were made out of metal or rubber. While that made them generally quite durable, their reusability meant they had to be constantly cleaned to avoid spreading infection from patient to patient. With the introduction of plastic in the operating room, it became more cost-effective for surgical tools to be switched over to single-use sterile equipment. Even for some of the devices that still came in metal, like lancets or needles, plastic packaging enabled these items to remain sterile right up until the moment of use, again helping prevent the spread of germs.
Beyond the operating room, plastic is becoming essential for some of the things left behind after surgery. In the past, hip replacement surgery might have involved joints where there was metal-on-metal contact. Now, with some of these parts cast in plastic, they’re lighter than before and there’s often less need for repeat surgery to replace worn parts. In one Canadian study, those with metal-on-metal hip joints were 1.6 times more likely to require a repeat surgery than those with metal-on-plastic joints.
Plastics have also taken a feature role in many prosthetics. Replacement limbs like legs and arms, previously made of wood or metal, are now custom-molded from plastic to better fit the recipient. For limbs with robotic components, plastic is also used to minimize weight, for better agility and lower cost. In fact, some enterprising do-it-yourselfers are even using 3D printers to make replacement hands out of Acrylonitrile Butadiene Styrene (ABS), which is a low-cost engineering plastic easy to machine, fabricate, paint, and glue.
Plastic will almost certainly play more of a role as people do more self-modification projects down the road, too. (We’ll take a closer look at how DIY biohackers are modding themselves in Chapter 6, “Franken-You: A Better Life Through Cyborg Technology”.)
Taking a Peek Inside
While the birth of diagnosis-based modern medicine dates back to the time of Hippocrates, it’s worth noting that a lot of diagnoses through the ages have been sheer guesswork when it came to anything that was malfunctioning inside the body. In some cases, there were reasonably obvious signs that made their way to the outside of the body, such as swelling or discoloration, but some maladies without outward indications were a bit trickier to diagnose without surgery.
That changed at the end of the nineteenth century when Wilhelm Röntgen discovered the X-ray. As part of his experimentation, he directed a stream of X-rays through his wife’s hand toward a photographic plate, and noted that they were able to pass through flesh and other human tissues, but not through bone or metal. And so, radiography was born, and medical practitioners quickly adopted the technology. With this tool in their arsenals, doctors could confirm that bones were fractured, or locate a metal fragment caught under the skin. It was a pretty nifty invention.
While X-ray imaging continues to be used today, its use has tailed off dramatically, thanks to the discovery that radiation produced by X-ray equipment could actually harm human tissue, including the increased risk of cancer. Old-school single-shot X-ray exposures tend to be very short and very focused, and are only undertaken after determining that the benefit outweighs the risks of radiation exposure.
On the other hand, CAT scan usage has grown through the years, despite using X-rays as their method of looking inside the body. CAT is short for computerized axial tomography (sometimes referenced as a “CT scan”). It uses computers to create cross-sections of the body by stitching together information taken from different locations and angles, as the patient slides through a diagnostic ring on a moving platform. CAT scans allow doctors to look at the body in 3D, providing a much better view than the previously available flat version, where a lot more was left to interpretation.
Radiation exposure from a CAT scan is many times the exposure level of a single X-ray and there are concerns that the cancer risks might outweigh the medical and diagnosis benefit.
Magnetic resonance imaging scans, also known as MRIs, have also become popular. Because they use a combination of radio waves and magnetism to create a three-dimensional scan of the patient’s internal structure, they’re often preferred over CAT scans. However, they have limitations compared to CAT, including higher cost, and the fact that they can’t be used with patients that have cochlear implants, pacemakers, or some neurostimulator devices because of the metal in those implants. (The magnet in the MRI can tug on the metal pretty fiercely.) There’s also some concern that extensive MRI usage could cause a breakdown in the patient’s DNA itself, which is another reason that MRI hasn’t taken over completely from X-ray-based scanning.
All these advancements have gone a long way to increasing our lifespan in ways that would have seemed unnatural hundreds of years ago, when people were dying of old age at lifespans that would now be just edging us into midlife crisis territory. Average human life expectancy has actually increased dramatically over the last 60 years. In the mid-1950s, people in the developed world could expect to live until sometime into their 60s, but now expected lifespans are north of age 80. That’s because we are now able to catch a lot of the things that would have otherwise put us into an early grave, like random infections or tumors. (You’ll learn more about longevity in Chapter 8, “Hyper Longevity: How to Make Death Obsolete.”)
Have a Heart—Pacemakers, Transplants, and Artificial Hearts
Physicians have known since 1889 that the heart reacts to electrical stimulation, when John Alexander MacWilliam discovered that application of electricity could cause a heart’s ventricle to contract. Repeated application of electrical impulses through electrodes placed into the heart muscle could, in fact, cause a heart to “beat” at a more-or-less regular rate. Research continued on and off through the first half of the twentieth century, but it wasn’t until 1958 that Arne Larsson received the first implanted pacemaker designed to regulate his heartbeat, kicking in when his own heart stopped beating at a normal rate.
Larsson, a Swedish citizen, went through 26 more pacemakers during his life, and lasted to the ripe old age of 86. He succumbed to skin cancer in 2001.
The technology continued to change and improve: battery life improved; construction materials changed, facilitating longer life with less danger of corrosion or moisture damage. Also, newer pacemakers could adjust their rate based on the level of physical activity, oxygen and CO2 levels, temperature, and the respiration rate of the user.
One of the issues with pacemakers through the years was the fact they required wired leads between the pacemaker and the heart, and damage to those leads could cause the pacemaker to malfunction, or result in other medical complications such as infection.
In April 2016, the FDA approved Medtronic’s “vitamin-sized” Micra pacemaker, which “sits inside the ventricular cavity,” attaches to the muscles inside the heart using tiny little metal claws, and delivers pacing impulses by an electrode located at the end of the device. With a battery meant to last around ten years, younger patients can expect to replace it during their lifetime, or at least until we can replace the faulty heart with a jet-engine version or one grown in the lab.
The Micra can be installed or retrieved via the femoral artery, meaning the procedure is “minimally invasive.”
Sometimes, unfortunately, a pacemaker isn’t enough to kick-start the heart, it may need a heavy-duty device to help it pump, or it may need a full replacement.
The history of organ transplantation goes back a while, but just how long is a matter of some debate. Although there have been reports of leg and heart transplants dating back thousands of years, these accounts seem dubious at best; reports of skin grafting seem to be more credible, though it’s hard to say just how successful those operations were. In 1883, Swiss surgeon Theodor Kocher performed a thyroid transplant, widely regarded as the first human organ transplantation; since that point, we’ve learned to transplant corneas, kidneys, bone marrow, intestines, livers, lungs, spleens, and hearts, among other things. In fact, we’ve started to transplant hands and even faces with varying levels of success. One unfortunate man even had a penis transplant, but his wife rejected it.
“We’ve started to transplant hands and even faces with varying levels of success.”
And then there’s the experimental work that’s been done where it was shown to be somewhat feasible to transplant heads using animals. In 1970, Neurosurgeon Robert White, for example, successfully transplanted the head of a monkey onto a second monkey’s body. The procedure was successful to an extent, with the animal being able to smell, taste, hear, and see the world around it. It was also able to bite.
Italian neurosurgeon Sergio Canavero, has also said he has a 30-something Russian candidate selected for a possible human head transplant in 2017. The man has a progressive and incurable wasting disease called Werdnig-Hoffmann disease. Canavero says he needs $100 million for the operation and is calling on billionaires to help fund the project.
“I need your help and I need your assistance,” Canavero is quoted as saying. “Be Americans.”
Critics aren’t enthusiastic about the idea. The most difficult part of the transplant is restoring the spinal cord. White failed to do that resulting in the reheaded monkey’s eventual death. That should be resolved using stem cell therapies, which are in development, but not likely by 2017.
Let’s not get ahead of ourselves here, though, and get back to issues of the heart. They are a different story. While we’ve been able to successfully transplant hearts since 1965, the donor unfortunately has to be dead in order for the transplant to take place, and people with healthy hearts just don’t die in sufficient quantities to satisfy the needs of people waiting for a replacement heart.
Although a mechanical heart machine was first used as a temporary replacement for the patient’s own heart during surgery in the early 1950s, the bulky automobile-sized machine could barely be considered a suitable alternative for the heart. The patient was tethered to an operating room for the rest of his or her life.
Through the 1950s and 1960s, further research led to testing of more compact artificial hearts in calves, and even temporary artificial hearts in human patients waiting for a permanent human heart transplant.
The first truly promising replacement to gain international attention was the Jarvik 7 artificial heart implanted into Barney Clark in 1982. The Jarvik 7 had a component that was implanted right into Clark’s chest, but it had to be attached to a large, mobility-limiting and noisy external compressor unit.
Clark survived 112 days with the Jarvik 7 implanted, but died following a series of complications. Another Jarvik 7 recipient, William Schroeder, lasted 620 days, and was even able to leave the hospital with a portable compressor unit, but his remaining days were also plagued with complications, such as a series of strokes.
Since Clark and Schroeder, there have been a number of patients implanted with either artificial hearts, or what are called ventricular assist devices. The latter devices don’t replace the heart outright, but provide assistance to the patient’s own heart.
Until fairly recently, the problem with both these types of devices was that they were mechanical, so they had durability issues. They were designed to simulate the organic human heart. Their mechanical components allowed them to “beat” roughly 85,000 to 140,000 times a day—or tens of millions of times per year. The problem was that the components inside the pumps eventually wore out and failed.
If the device was assisting a weakened heart and it failed, there was a chance the patient could undergo surgery for urgent replacement of the device or for an emergency heart transplant. If the patient received an artificial heart and the device failed, death was inevitable.
Consequently, these artificial units were often regarded as what Cohn calls “bridges.” They give a patient time, until a human heart from a donor becomes available for transplant. Patients who can be supported with an assist pump alone generally have disease primarily involving the left ventricle, the main pumping chamber of the heart. The right ventricle, the one responsible for pumping the dark venous blood to the lungs to pick up oxygen, needs to continue to function; otherwise, the assist pump doesn’t function well.
The older assist pumps (like the artificial hearts) would fail after a year or two as described above. But all that changed 15 years ago. In the 1980s, physician inventor Rich Wampler visited Egypt and witnessed local workers using a hand-turned Archimedes screw to pump water up a river bank for irrigation. (See video of the screw: http://www.superyou.link/archscrew.)
He realized that if a screw could move water against gravity, perhaps it could move blood against pressure. So he designed a prototype that used an external motor outside the body to spin a small screw the size of a pencil eraser 25,000 times per minute inside the body.
Perhaps, he reasoned, it could pull a meaningful amount of blood out of a weakened ventricle to get a patient through a short period of heart failure.
Wampler showed the device to O. H. “Bud” Frazier, chief of transplantation and assist devices at the Texas Heart Institute in Houston.
Frazier was initially concerned that the rapidly spinning screw would destroy fragile blood cells, but multiple animal experiments showed it wasn’t an issue. So, in 1988, the device was used successfully to save a dying patient.
Thanks to this innovation, and ongoing work by artificial heart researcher Rob Jarvik, a number of durable, permanent, screw-like assist pumps were developed over the next few years. Unlike the assist pumps that beat like the human heart, these rapidly spinning pumps were much smaller and much more durable.
“These continuous flow pumps have no flexible membranes, no cams, no cam followers, no high torque rotors,” said Frazier’s partner Billy Cohn. “The new pumps eliminate all that mechanical complexity ... they’re small, they’re quiet, and they’re very durable.”
In these earliest heart-assisting devices, the spinning screw, sometimes also called an “impeller,” was supported on each end with a mechanical bearing that was impervious to wear and was kept clean by the rapid flow of blood.
“There was one moving part, so nothing to fail,” explained Cohn.
With the newest generation of assist pump, the spinning impeller is suspended magnetically. Now, even the mechanical blood-washed bearings have been eliminated.
Enter the jet-engine heart.
One of the first of these spinning assist pumps, or continuous flow devices as they are commonly called, was the HeartMate II. This was designed to assist a patient’s weakened heart by pulling blood directly from the left ventricle through a metal tube inserted through the heart wall.
“HeartMate II assist pumps are now being implanted daily, just like the one Vice President (Dick) Cheney had,” Cohn told us in an interview.
There is also a version called a HeartWare HVAD pump. It is another continuous flow assist pump. Both are generally used in patients who have failure involving only the left ventricle. But what about patients with failure affecting both ventricles?
Many heart centers have tried to implant a pair of assist pumps; one in the left ventricle, and a second in the right ventricle.
“Putting two pumps in has proven to be challenging,” said Cohn, explaining that two controllers are needed, plus the enlarged diseased heart stays in place and interacts with the pumps. And, there is limited space inside the chest.
“We have tried to use this strategy in carefully selected patients, but results have been mixed,” said Cohn. “Other institutions have tried to use this two-pump strategy as well, but it is often not ideal.”
To address these challenges, Cohn and Frazier began using animal studies to investigate whether it would be possible to remove the heart completely and replace it with a pair of rapidly spinning pumps.
“Removing the enlarged heart certainly would free up a lot of space, and decreasing the different flow paths the blood could follow maybe would be beneficial,” said Cohn.
The idea of completely eliminating the heartbeat was not without precedent in Cohn and Frazier’s experience.
Although a significant percentage of patients implanted with continuous flow assist pumps lose their pulse, the pressure in the arteries still rises and falls with each heartbeat—just not enough that a doctor or nurse can feel it with their fingertips.
In contrast, if the heart is removed and replaced with spinning pumps, the arterial pressure waveform is a flat line—though this has been seen only on rare occasions.
In one case, Frazier was surprised to discover that a patient who had received the HeartMate II no longer had a pulse.
The patient’s heart had stopped beating altogether, yet blood was passively flowing through the lungs without help from the pumping action of the heart’s right ventricle.
That was a surprise to the doctors. Yet the unexpected result was duplicated in another patient from New York State, whose HeartMate II was providing the only blood pumping mechanism in her body. In each of these patients, the flow of blood was absolutely continuous, like water in a garden hose, without a hint of a pulse.
Who Needs a Pulse, Anyway?
Cohn and Frazier’s idea was validated through extensive research in the large animal facility at the Texas Heart institute. It showed conclusively that calves—there were more than 50 involved in the research—could be kept alive with continuous flow devices.
The animals would eat, sleep, and grow like normal calves, and would interact with caregivers and exercise on a treadmill, and yet they had no heartbeat, no EKG, and—that’s right—no pulse.
In 2011 Craig Lewis, a gravely ill man, arrived at the Texas Heart Institute. He was in profound shock. His heart, liver, and kidneys had been infiltrated with a substance called amyloid, which was produced by a rogue population of bone marrow cells. He was too sick for heart transplantation and his heart was too small and contracted to allow safe placement of assist pumps. The other challenge: He wasn’t a candidate for a temporary mechanical artificial heart, because he wasn’t a transplant candidate.
After extensive discussions with his family, Lewis’s diseased heart was replaced with a pair of HeartMate II pumps. The research at this point was solid. The team had been exploring the option for six years.
The device kept Lewis alive for more than five weeks, and it even allowed him to sit up and interact with his family after a prolonged pre-operative period, where he was in a coma.
Lewis died, however, because of progressive failure of some of his other organs. Still, the heart replacement showed it was possible to live without the original organ for longer periods.
Through all this work, Cohn and Frazier spent considerable time talking about their research at numerous professional society meetings and at many speaking engagements attended by the public, including a talk at TEDMED in 2012 (see video: http://superyou.link/tedmed2012). As a result of that exposure, they met Daniel Timms, a scientist living in Australia. Timms’ father had died of heart failure while he was working to earn his PhD.
“... the heart replacement showed it was possible to live without the original organ.”
Timms was motivated to try to find a technological solution for patients like his father, who would otherwise die without some sort of intervention.
He independently came upon the idea that a continuous-flow device was the way to go. His unique design addressed many of the challenges caused by a pair of spinning pumps. And it wasn’t unlike the technology being used by Frazier and Cohn.
The device Timms conceived contained a single moving part suspended in an electromagnetic field. The single spinning disc had impeller vanes on each of the two faces. One side took the bright red blood returning from the lungs and pumped it to the rest of the body. On the other side of the same spinning disk, an assembly of vanes drove the blood returning from the body to the lungs.
“This one spinning disk performed the function of both pumps,” explained Cohn.
Even better, Timms had designed the spinning disc to shift slightly from one side to the other, based on changes in pressure. This resulted in a change in the relative strength and efficiency of the left and right pumps.
“This device can respond to physiological changes faster than a natural human heart,” said Cohn. “Although the strength of the electromagnetic field is adjusted 20,000 times each second to keep the disc spinning in space, 20 times a second it says, ‘wow, the right side pressures are getting a little higher than the left, I need to move to the right.’ Or, move to the left to accommodate exercise or whatever. So at 20 times a second it’s re-evaluating the two pumps and adjusting for it.”
The only problem: Timms didn’t have the resources, institutional experience, and support to get it to work—and he was out of money. So, after seeing Frazier present at numerous conferences, and watching Cohn and Frazier’s TEDMED talk, he got on a plane with the intention of showing them the technology.
Cohn said they weren’t expecting much when he showed up in Houston. (He and Frazier had already seen a lot of unsolicited crackpot ideas.)
“He was unshaven, and had on blue jeans, but he seemed like a nice young man, so I was going to let him down softly when I figured out why his device was tragically flawed, as soon as I figured it out,” said Cohn, recounting the meeting.
But Timms’ pitch was brilliant. “He starts describing this device. I sort of cross examine him. I say ‘What about this? What about that?’ He had great responses to everything,” said Cohn. “We had scheduled a 30-minute meeting. And after talking to him for three hours, I realize this guy is one of the most brilliant men I’ve ever met, and his device addresses many of the challenges and shortcomings of our twin turbine concept.”
Specifically, it had the potential to be much smaller. It automatically balanced the left and right sides of the circulation. It would only require a single controller. And, most importantly, it wouldn’t wear out after a year.
“So I beg him to stay at Texas Heart and let us implant one,” recalled Cohn.
In the end, Timms’ team moved to Texas to work on the project. The Texas Heart team was able to leverage their network to help Daniel and his team raise the necessary money, and leveraged their experience with heart replacement and their large animal lab to help keep the project moving forward.
Between 2013 and 2016, a number of calves had been implanted with the devices, and after the surgeries, some were able to exercise on a treadmill.
The results so far have been extremely encouraging, so much so that Frazier and Cohn are fairly convinced that the device will be the first practical permanent mechanical replacement for the failing human heart.
The first few generations of this new heart module will be powered by a large driveline exiting through the skin to a vest that holds a computer controller and several large batteries.
Ultimately, the device will be powered by technology called Transcutaneous Energy Transfer System, or TETS.
It is essentially a short-range wireless power transmitter. TETS uses external batteries that generate a high-intensity oscillating magnetic field, which is beamed into the body by an external coil-shaped antenna, attached to the patient’s skin. Inside the patient’s body a second antenna receives the transmitted energy. And this setup powers the heart-replacement device in the patient’s chest.
The implant has minimal moving parts, for increased reliability, and it is powered by a vest that can be swapped out as easily as you might change jackets.
Each year 500,000 people die of heart failure in the United States alone. And yet, surgeons only have access to 2200 donor hearts.
For authors Kay and Andy, this hit pretty close to home. As we finalized this chapter, Kay’s dad Kris, who did substantial research for us in several of this book’s chapters, suffered a heart condition that almost took his life. It required a valve replacement and triple bypass to save his life.
“Each year 500,000 people die of heart failure in the United States alone. And yet, surgeons only have access to 200 donor hearts.”
So a permanent mechanical heart replacement that has only one moving part is a miracle of science and technology. It has no flexible membranes or complex mechanisms that could fail, and it is small enough to implant in most patients, including, perhaps one day, Kay’s dad. It will truly change the way end stage heart failure is managed.
As you can see, the accelerating improvement of technology saves lives. Just think about the technologies at play in this one story. Scientists building on each other’s breakthroughs over several decades using evolving tools, multi-disciplinary expertise, and the power and reach of the Internet, to produce a device that can replace a human heart—for a lifetime.
And the technology goes from helping extend a few people’s lives to dozens, then hundreds of lives. And today, as it nears production, it has the potential to save a half million lives a year. It’s quite incredible. Especially, when one of those people is someone you love.
It’s Now, and It’s New: The Future Frontiers of Medicine
If you think medical advances in the last 100 years have been amazing, wait until you see what’s coming next. Let’s peer into the future of medicine.
Nano, Nano
Nanotechnology is something people have been talking about for a long time, but what does it actually mean, especially when it comes to medicine? Essentially, nanomedicine involves targeting illness at extremely small scales. This can be anything from extremely small medicine-delivery methods to tiny little robots swimming through the bloodstream.
Biomedical engineer Mark Kendall has been working on a new technology called the Nanopatch, which uses nanotechnology to get around the fear many people have of the needle (see it here: http://superyou.link/nanopatch).
While many people have no particular love of injections from a needle and syringe—a technology that’s been around for more than 160 years—there have been precious few alternatives. That is until now. Enter the Nanopatch, a spring-loaded applicator that shoots a small vaccine-loaded patch measuring roughly 0.4 square inches (1 square centimeter) at the skin.
When the patch hits the skin, roughly 4,000 tiny projections breach the skin, and vaccines located on each of the projections make their way into the bloodstream. After a short period, the Nanopatch can then be peeled off and discarded.
Even better, argues Kendall, the Nanopatch offers a better level of protection than the standard needle-and-syringe combo, allowing effective levels of protection at a fraction of the cost.
The Nanopatch can also potentially boost the efficacy of vaccines that don’t currently work all that well when delivered by needle. It also allows the vaccines to stay viable without the same level of refrigeration required by standard methods. That makes them useful in areas where refrigeration isn’t available or widespread. Consequently, the Nanopatch can be useful in parts of Africa where traditional vaccination methods currently don’t work.
Nanotechnology has already made its way into the world of pharmaceuticals, with a number of drugs in the marketplace making use of nanoparticles, most notably for targeting cancer cells. Nanotech can also repair tissue, do genetic detection, and purify blood.
Some see an even larger role for nanotechnology in the world of medicine. Take medical futurist Dr. Bertalan Meskó, who refers to himself in his LinkedIn profile as “a geek physician with a PhD in genomics.”
Meskó looks forward to a day when tiny robots course through your bloodstream waiting to spring into action at the first sign of trouble. For example, they could “release oxygen during a heart attack,” or collect information and then provide alerts when we are at risk of developing a disease.
“I’ve had a bunch of genomic tests just to see how they work in action,” Meskó told us. “They say that, ‘I have this kind or increased risk for this kind of medical condition,’ which, based on my genetic profile tells me I might develop a disease within the next five to ten years, but with nanorobots we might be able to get the notification even before the first symptom arrives.”
In his book The Guide to the Future of Medicine, Meskó notes, “These microscopic robots would send alerts to our smartphones or digital contact lenses before disease could develop in our body.” He even foresees a future where blood-borne microbots could identify and treat cancer cells.
But Meskó is cautious about the time frame for this type of technology entering the mainstream. When asked how soon he believes it will be commercially viable, he said “The nanorobot technology? Not ten years. At least 15 to 20. And I’m considered an optimistic futurist.”
There’s nothing wrong with that prediction. It’s pretty much on par with Ray Kurzweil’s forecast. Kurzweil told the Wall Street Journal in early 2014, “We’ll have millions—billions of blood cell-sized computers in our bloodstream in the 2030s keeping us healthy, augmenting our immune system, also going into our brain, putting our neocortex on the Cloud.”
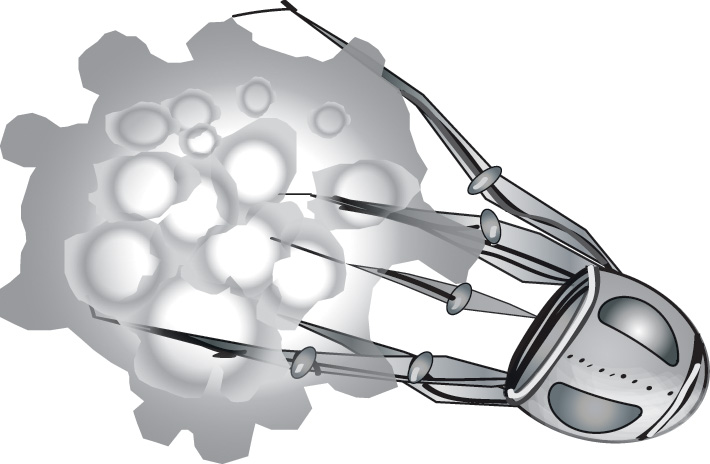
These tiny robots will also attack cancer cells (see Figure 4.1), cleanse the bloodstream, and scrub the plaque from our arteries.
(Illustration by Cornelia Svela.)
Figure 4.1 Our artist’s rendition of a microscopic nano-robot attacking a cancer cell.
That said, If you think nanobots in your bloodstream is a way out concept, watch this short interview with Metin Sitti, a roboticist and Professor of Electrical Engineering at Carnegie Mellon University: http://superyou.link/nanobots.
I Sing the Body Electronic!
Electronics have been part of medicine for a long time now. For decades patients have had monitoring equipment of varying shapes and sizes sitting beside their hospital beds. They automatically measure heart rate, blood pressure, and other vital statistics. Electronically controlled medication drips automatically delivering doses at precise intervals. These devices, as well as more specialized equipment, are used in operating theaters around the world to help surgeons and their assistants keep an eye on the progress of an operation.
These days they include tiny cameras that can be inserted directly into the body through the stomach, through arteries, or other passageways that would have been impossible in years gone by. Surgeons are now able to see what’s actually going on inside the body so they can provide precise treatment. Procedures that once required opening a patient’s sternum can now potentially be performed using small cameras inserted alongside tiny robotically operated surgical tools, through a small incision. As you’d imagine, these procedures are less traumatic to the patient and they also speed up recovery times greatly.
Other technologies have started to make their way into operating theater, including tablet computers, augmented reality headsets, and heads-up displays.
In one application from Germany’s Fraunhofer Institute for Medical Image Computing MEVIS, a patient’s liver was scanned using a CT scan. The information was imported into an iPad app. In the operating theater, doctors were then able to point the iPad’s camera toward the patient’s exposed liver and the app then overlaid the image of the liver with a virtual image of the patient’s blood vessels, using information collected during the CT scan. The idea: Give the medical team quick access to as much info as possible, reducing the possibility of inadvertently cutting into vital blood vessels, while removing a tumor.
If you think you haven’t had any experience with technology from the Fraunhofer Institute, you’re probably wrong: It’s also where the MP3 was invented. Pump up those beats!
Of course, slipping an iPad into the middle of surgery may not be ideal; the tablet requires two hands to use, and generally has to be packed up in a protective coating to make it suitable for use in a sterile medical environment. Instead, heads-up displays have a more promising future.
It’s probably not surprising that one of the technologies already making its way into the operating theater is Google Glass. Not only does it have an eyepiece to allow surgeons to view charts, medical scans, or other relevant information, the device’s voice control can enable a surgeon to get information immediately without the need to put down tools in their hands. The built-in camera can enable surgeons to livestream video of their surgery to off-site experts—or simply to provide a record for later analysis.
Dr. Rafael Grossmann, based in Maine, was the first to use Glass inside the operating room, and the experience has made him a fan of the technology. During an initial trial, he used it to livestream his point-of-view to an iPad located elsewhere in the surgery room, which then sent it to a Google Hangout. In a blog post following the announcement from Google that there would be a new generation of Glass, Grossmann wrote that his wish list envisioned a version of Glass that could be used for remote consultations, which could stand up to “field-conditions no matter the type of field! (think of doctors from Doctors Without Borders using them in disaster zones or in the middle of a conflict.”
“... the [Google Glass] built-in camera can enable surgeons to livestream video of their surgery to off-site experts. ...”
Grossmann noted during one of his TED Talks that heads-up technology like Glass can play a big part in increasing safety in the operating room, by reducing the possibilities of sometimes-fatal medical mistakes, such as wrong-site surgery (i.e. amputating the wrong leg). Coupled with modern apps that replace the old-school pen-and-paper checklist, surgeons can minimize the risk of entirely preventable errors which can cost patients their lives.
Meskó thinks this type of technology is going to continue to play a big part in surgeries of the future. He was one of the remote viewers of Grossmann’s livestreamed operations.
“I told [Grossmann] that it’s great and I believe all these operations will be recorded and that all the recorded videos will not be checked for errors by humans, but actually by the IBM Watson supercomputer,” said Meskó.
But he also sees a future where the device can be controlled through the power of thought, using technology similar to that found in the Muse brainwave-sensing headband, and then have results delivered to next-generation heads-up displays: “I’ve worn Google Glass a few times but I had to communicate with the device by using my hand or by voice: ‘OK Glass, take a picture,’ and it does. But with EEG, we actually think about doing things and we’ll get the same information through the digital contact lenses.”
The future of electronics in medicine is going to go well beyond what surgeons strap onto their heads during an operation.
Some researchers are already starting to use electronics as a stand-in for actual human organs in prototyping both medications and health outcomes.
In a 2013 TED Talk, Geraldine Hamilton of Harvard University’s Wyss Institute showed an “organ-on-a-chip” device that that simulated the function of a “breathing, living human lung.”
The chip contains human lung cells arranged in a layer that can then be manipulated in a way that simulates the way an actual lung would behave.
The device also features a channel that behaves like blood. That is combined with channels that can simulate some of the forces real organs would experience in the body. Foreign material, such as bacteria, can also be introduced to see how the lung will react.
The organ-on-a-chip could also simulate the function of a human intestine, which could help model a disease such as irritable bowel syndrome (IBS). Other models have simulated liver, heart, and bone marrow tissues.
Each organ-on-a-chip structure is important in and of itself, but it’s when you link them to each other that is when the magic starts to happen. It can show what happens when each system interacts with other systems.
This becomes important when prototyping new drugs. It’s all well and good to know how a drug might affect the specific organ it was intended to treat, but if it has an adverse reaction on one of the other important body systems, it can be problematic. By linking these chips designed to simulate body parts, you can tell that a drug designed to treat asthma might actually have an adverse effect on the heart or liver (or vice versa), all without having to test the drugs on living, breathing humans that may have malpractice attorneys on speed dial.
Or, for example, it can be used to test reactions to chemical exposure (such as that found in a household cleanser, for example) on human skin.
Ithaca University’s Michael Shuler has also worked with similarly linked biological systems; in the article “Honey, I Shrunk the Lungs” in the March 2015 issue of Nature magazine, Shuler details a test his group conducted on the effects of naphthalene, a chemical in mothballs.
In the group’s testing, introduction of naphthalene into the linked system caused the death of lung cells, but that cell-death disappeared when the liver module was removed from the linked system, indicating that the lungs were affected not by the chemical itself but by a byproduct of the liver’s attempts to neutralize the chemical in the linked system. How cool is that?
Hamilton noted in her TED Talk that the most important application that organ-on-a-chip might provide is individualized response. You provide your own cells for inclusion in one of these chips and doctors can start personalizing treatments that avoid some of the pitfalls or current one-size-fits-all treatments.
“Individual differences mean that we could react very differently and sometimes in unpredictable ways to drugs. I myself, a couple of years back, had a really bad headache, just couldn’t shake it, thought, ‘Well, I’ll try something different.’ I took some Advil. Fifteen minutes later, I was on my way to the emergency room with a full-blown asthma attack.”
With the organ-on-a-chip setup, you can tailor new individual treatments without risking sending anyone to the hospital.
“We can simulate how organs work,” said Meskó. “And, if we can do that now with a lung, that means in five or ten years time we can do that with other organs,” he said.
“With the organ-on-a-chip setup, you can tailor new individual treatments without risking sending anyone to the hospital.”
Drugs will not be administered to patients without knowing the outcomes. Instead, drugs can be administered to the simulators, and the results will show what would happen if they were given to real patients.
This will have a profound effect on the speed of clinical trials. “Now you have tens of thousands of people and half of them will be on placebos. But you will be able to do the same thing with simulations. You will get the same quality. It frightens the pharma industry because they’re not ready for these kind of changes. But they will have to change their business models for sure,” Meskó explained.
Up Close and Personal with Your Genome
The thing that determines a huge chunk of who we are, what we will become, and the maladies that will ultimately afflict us is our DNA, which is a fairly unique sequence of nucleic acids that determines our genetic makeup.
When a daddy and a mommy make a baby, their DNA mixes together to produce a new person, which means that one offspring might be very different from his or her sibling. Consequently, each person has a different genetic signature that might make them prone to different diseases or conditions, and might make them react to chemicals or treatment in differing ways.
Researchers believe that understanding an individual’s DNA makeup will provide valuable information for keeping them healthy, including preventative treatment, individually tailored medicines, and custom therapies. For the longest time, that was easier said than done, as the ability to decode DNA remained elusive, containing as it did some 3.3 billion chemical “base pairs.” A project to decode the human genome started in 1990, but didn’t yield an effectively complete sequence until 2003.
Following the completion of the project, the big factor preventing people from blasting ahead at full speed in decoding the genome was cost. In 2007, the cost to sequence a single genome was somewhere around $10 million. Now, the cost for sequencing an individual’s genome is down to four digits, a drop that a chart from Genome.gov notes is well ahead of the curve Moore’s Law might have predicted. In 2017, it will likely drop into the three digits, below $1,000. (See the chart at http://superyou.link/1kgenome.)
Extrapolating out from this existing price curve, no doubt some people are looking forward to a time in the very near future where you can simply send a DNA sample away in the mail with $20 and receive your complete genome by return mail a few short weeks later. Or someone might make a kit akin to the pee-on-a-stick pregnancy test but for DNA profiling. Remember, once upon a time, a rabbit’s ovaries were injected with a potential mother-to-be’s urine to test for pregnancy. So the idea of a drug store DNA test isn’t that far-fetched.
With this type of information on hand, people can start to understand what types of conditions they might be genetically predisposed to develop.
During a 2012-released Stanford University study detailed in the book The Cure in the Code, geneticist Michael Snyder discovered that his genetic profile indicated that he might develop type II diabetes, despite the lack of any family history of the disease. Consequently, he was able to track the progress of the disease in his body, and how it responded to treatment. Following the study (where he was a project leader), he speculated on what this could mean for people as the price of testing drops. “I think people who are at risk for certain diseases could do a simple home test. You could probably monitor yourself every month so you can catch diseases early,” said Snyder.
Meskó believes this scenario could come sooner than you’d think. “The Oxford Nanapore genomic company came up with a device, a USB-based device which I can connect to my laptop, and with a blood drop I can actually sequence parts of my DNA. With a laptop! So it’s actually quite cheap based on the whole genome sequencing. So maybe in a few years’ time we will be able to sequence our whole genome just with a USB stick and a laptop. It’s not so futurist anymore.”
See, we told you! Though we won’t bet on the “laptop and USB stick.” By then your “computing” device will likely be something completely different.
The device Meskó references is known as the MinION. It can identify DNA, RNA, micro RNA, and proteins, and at the time of this writing (mid-2016) is available from Oxford Nanopore for an “access fee” of $1,000 (see: http://superyou.link/minion). It’s about the size of a compact remote control, and sits beside your computer to process material you put onto its sensor.
Here’s how it works, for those of you that want to show off to your mom at brunch next weekend: It measures how molecules disrupt a current flowing through a protein micropore inserted into an electrically resistant membrane. As different types of materials flow through the pore, the signal that’s generated can help analyze the different types of material—for example, different types of RNA strands—and in what concentration they appear in the sample.
It’s not exactly a complete genomic sequencing, but for those who want to keep an eye out for certain genetic markers, it’s certainly less expensive than building a complete genetics lab.
As the technology for peering into your own genetic makeup continues to become more available and less expensive, Meskó sees it becoming a part of your life right from the start.
“In a few years—three, four, or five years’ time—every newborn will get their genome sequenced,” he told us. “So, they will start their life with this information. We might not be able to do much about this information from a medical perspective. But at least they will have it. Their genome will not change throughout their life.”
That can prove extremely valuable down the road when it comes time to develop treatments for any diseases or conditions that might transition from simple predisposition into hard, cruel reality.
We already know that drugs that might be effective for one person might do nothing at all for another person with the same condition, and might even have life-threatening consequences. That’s largely because everyone has a slightly different genome, and as a result, different types of drugs have the potential to interact slightly different for different people.
That’s one key reason why there are so many different drugs (and drug types) for a fairly common condition like hypertension. Some patients respond perfectly fine to the old-school diuretics, while others might see no effect. Still others might benefit from beta blockers while others might find they cause lung problems. In the end, treating even relatively well-understood conditions can involve a lot of trial-and-error when trying to pin down an effective pharmaceutical treatment.
Patients should be able to bring the power of their own genetic information to this process. After getting your genome sequenced, doctors can use modeling to have a better understanding of how your specific system works, and would then potentially have the ability to reverse-engineer a medicine that will be fantastically efficient for your specific condition, rather than throwing a series of pharma options into your system just to see what sticks ... or what sticks long enough to be considered “good enough.”
We bet the role of your pharmacist at your local Walgreens or Duane Reade will become increasingly important in the near term and then super tech-savvy, and then suddenly redundant. Sort of like the guy that used to develop the film from your camera at your local Photomat 15 years ago.
With your genomic information in hand, it’s easier to see how to hit the bullseye, especially if you start to pair the design of the custom pharmaceutical with the organ-on-a-chip modules detailed earlier in this chapter. Or, as author Peter W. Huber puts it in The Cure in the Code, “We are moving swiftly toward systems that can design an anti-molecule to match any molecule found in the vast, complex, diverse, mutable library of biochemical code that defines humanity and all the rest of life on earth.”
DIY Body Parts
If you’ve walked through a mall in the last decade, you might have seen one of those storefronts where you can build your own teddy bear using various custom parts.
If you’ve ever lamented the fact that you can’t get replacement parts for your own body that easily, you might be surprised to know that this is coming. (Whether it makes its way to a mall storefront is another question entirely.)
One way technology and biology have come together during the last decade is in the hot field of 3D printing (see Figure 4.2).
(Illustration by Cornelia Svela.)
Figure 4.2 A 3D object is designed on a computer (left) and then is printed out by a machine (right) that layers materials slice by slice to form an actual three-dimensional object.
In addition to 3D-printing custom pharmaceuticals, this technology can also be used to create replacement biological body parts.
Using information gleaned from CAT and MRI scans, labs are now able to use industrial 3D printers to create replacement parts, such as titanium hip joints custom-designed to fit seamlessly into the patient’s own existing bone structure. Other teams have been using 3D printing to replace lost bone, enabling both facial and skull reconstruction customized specifically to the patient.
The technology can also prove extremely useful for diagnostic purposes. In one case at Brigham and Women’s Hospital in Boston, a scan of a patient’s heart was turned into a full-sized three-dimensional model. After examining it, a cardiologist preparing for a surgery on the patient realized the procedure would not work. In another case, following an ultrasound scan, a blind woman was able to “see” her unborn child with the aid of a 3D print made from the scan information.
Anthony Atala, Director of Wake Forest Baptist Medical Center’s Institute for Regenerative Medicine, is looking for ways to regrow organs that might have already become nonviable, or as he refers to them in his 2011 TED Talk, “deceased.”
After procuring a tissue sample from the expired organ, Atala’s team was able to grow tissue that would function in the same way as the original tissue. He noted that these newly created heart cells would even “beat” the way original cells would have beaten. Atala also noted that his team was able to grow a new bladder from a section of the patient’s own cells taken from the original organ that was “less than half the size of a postage stamp.”
But Atala isn’t content with simply regrowing the patient’s own organs in a lab environment. He wants to 3D-print new organs using cells instead of ink. (See 3D bioprinting technology here: http://superyou.link/3dprinting.)
While some of this can already be done using a standard desktop printer—equipped with special cartridges, of course—Atala envisions a future where specialized equipment can scan a patient’s wound and print new cells directly onto the patient in the proper layers of tissue that would have occurred in the original, uninjured form.
“Ninety percent of the patients on the transplant list are actually waiting for a kidney,” Atala said in his 2011 TED Talk. “Patients are dying every day because we don’t have enough of those organs to go around.”
The solution? Scanning the patient’s body to get the detailed dimensions of their kidneys, layer-by-layer, and then print a new one, layer-by-layer, using actual cell tissue. At the time of his talk, the equipment they had could print a prototype kidney—not a fully functional kidney replacement, mind you—in about 7 hours.
In early 2016, Atala and his team announced they had successfully printed an ear, along with bone and muscle structures. When implanted under the skin of rats and mice, the living printed tissue maintained its shape, grew, and developed blood vessels.
One researcher has even found a way to print tiny blood vessels using a $40 cotton candy machine (see http://www.superyou.link/cottoncandy).
As the technology exponentially improves, we can expect printing speed to improve (as well as the accuracy), leading to a viable kidney replacement within reasonable time frames. Within ten years? We are betting on it.
It’s not just organs that we’re creating from scratch, though. Researchers in South Korea have also recently developed what they’re calling “smart skin.” The skin, which features sensors embedded into a soft material known as polydimethylsiloxane (PDMS), can measure pressure when stretched or when pressure is applied, providing some of the same feedback that would have been provided by actual human skin. That includes feedback you don’t really think much about, such as measuring heat and cold, or whether an object is wet.
You’d know when your dog is licking you, or when you are resting your prosthetic arm on a hot stove so you would be able avoid this scenario.
“Funny smell. Hmm. What’s burning in the kitchen?”
“Oh crap, it’s you, honey!”
This artificial skin can theoretically be applied over artificial limbs such as hands and legs, including artificial limbs with articulating robotic parts such as wrists and ankles, allowing an amputee to regain some of the sense information lost with the removal of the original limb. The big hurdle, as you might expect, is somehow interfacing the information being gathered by this synthetic skin and transmitting it to the brain in a way that makes sense.
The synthetic skin might not be immediately viable because there is still the problem of wiring the recipients’ brains with the sensors. However, the British National Health Service has also been working on synthetic blood that might become useful faster. The artificial blood gets its start from either the umbilical stem cells of newborns or from bone marrow from adults. These cells are then cultured in the lab until they become full-fledged red blood cells. The process so far has resulted in modest success, but not quite enough to be a practical replacement just yet. However, the National Health Service (NHS) hopes to do full clinical trials in 2017 using the lab-grown synthetic blood. Again, provided this technology proves viable, it’s possible that someone could have a few bags of their own blood grown before surgery, or dip into a pool of synthetic blood when donations are running low.
Then again, you know that donor blood as we know it won’t really be needed for much longer. In (and probably within) ten years, we’ll grow our own supply through a mass production synthesizer of some sort. It’s not hard to imagine with the NHS breakthrough.
While we’re becoming good at building replacement parts out of metal and plastic (hips, artificial limbs), and transplanting others (hearts, lungs), we might be on the verge of being able to plug someone’s genome into a vending machine in the operating room and printing out a new kidney, knitting some sensors into a roll of replacement skin, and dispensing a jug of blood (lids and straws are located to the right of the machine). Compare this to the agony of sitting around on a waiting list (weirdly) hoping the right organs become available from some unfortunate motorcycle driver who miscalculates an eighteen-wheeler’s trajectory.
Stop the Bleeding
Speaking of blood, it can be a huge problem when you suffer a deep wound that results in a rapid bleed-out that kills you.
If you’ve ever watched one of TV’s many medical dramas, you’ve no doubt seen one of the show’s heroes barking something along the lines of, “We’ve got to stop the bleeding, dammit!” or “If he loses any more blood, he’ll die!” It doesn’t matter now much artificial blood you have at the ready, if the patient is making like a fire hose, they are pretty much a goner.
Naturally, blood contains agents that will start to coagulate from a liquid into a gel when you receive a cut. This coagulation, or clotting, allows a scab to form, creating a protective layer that keeps the rest of your blood inside your body, allowing the tissue underneath to heal.
Generally speaking, this process works pretty well, with most cuts needing little more than a bit of pressure or a light bandage to aid the process. For patients with more extreme wounds, two recent technologies will likely make rapid bleeding a thing of the past.
An Oregon company, called RevMedx, has a solution designed for fast treatment of “gunshot and shrapnel wounds on the battlefield.” Called the XStat, it’s a syringe-style applicator with a 30-millimeter diameter (about 1.2 inches) that gets inserted directly into the wound. When the plunger is depressed, the XStat releases a number of tiny sponges which quickly expand into all available space, stopping the blood from flowing out of the wound until it can be properly attended to. Each sponge is tagged with an X-ray marker, enabling all the inserted material to be properly scanned and removed when the foreign object that caused the original wound is removed. The XStat was shipped to the United States military early in 2015 for use in the field after receiving FDA approval.
Joe Landolina, who is 17 years old, discovered another effective alternative as a freshman at New York University, which he now offers via his company Suneris. Also delivered to a wound using a syringe-style applicator, Veti-gel is comprised of algae-derived polymers which reconfigure their structure when they are applied to tissue, essentially super-gluing a wound shut by creating a structure that’s similar to flesh, an organ, or skin.
According to the Suneris website, “Immediately after application, our gel stimulates the clotting process by physically holding pressure in the damaged blood vessel. The gel then rapidly activates the accumulation of platelets, which bind to the site of the injury to create a platelet mesh. Our gel completes hemostasis by accelerating the binding of the clotting protein, fibrin, to the platelet mesh, resulting in blood coagulation and a stable clot.” Veti-gel is now in trials with veterinarians and could be applied to human wounds in the near future.
A Sensor of Wonder
Before you can begin medical intervention, you need to know that something is wrong. A bleeding wound is a pretty good indication, but a lot of the conditions that plague us have less obvious indicators. We already have a lot of technology that can help diagnose problems without a lot of inconvenience. A basic oral thermometer can show if our internal temperature is out of whack. An automated cuff can quickly show that someone’s blood pressure is dangerously high. But these tools can’t diagnose all ills.
As flexible electronics become more commonplace, we’re starting to see new types of devices that can wrap around other objects—objects such as body parts. That opens up a new generation of health-related devices taking forms that were previously inconceivable, such as the heat-sensing synthetic skin that we covered earlier in this chapter.
Flexible electronics also enabled the creation of one of Alphabet’s new wonder gizmos, the glucose-sensing contact lens prototype.
![]() The ABCs of Google
The ABCs of Google
Alphabet is the new parent of Google, as of the summer of 2015, and holds all the non-search engine technology parts of the company.
A condition such as diabetes requires constant monitoring, including regularly pricking the skin to take a small blood sample. Unfortunately, a lot of people prefer to avoid the ouchy pinprick and consequently a lot of people self-monitor less regularly than they should.
Also, blood sugar can vary wildly through the day, and even those who regularly test their own blood might find themselves with dangerous blood sugar levels as they eat or exercise, and they might not always know that they’re about to pass out from low blood sugar until it’s too late. That’s where the glucose-sensing lens comes in.
The contact lens prototype is striking to look at. Even though it otherwise looks like any other contact lens on the market, tiny antennae run rings around the outside of the lens (See video: http://superyou.link/superlens). They are connected to a tiny sensor that can measure glucose levels found in the wearer’s tears once every second. That information can then be transmitted to a receiver, such as the wearer’s smartphone. It enables monitoring in more-or-less real time. According to the blog post on the lens, the company is even exploring such options as tiny lights that would illuminate if the wearer’s blood glucose level trended too high or too low. That gives them more warning that something is wrong. It would also make them look like a cool cyborg in the process.
We can see it now: “Hey dad, you’ve got glowy monster eyes. Do you want a sugar cookie?”
While the project was simply a prototype at the beginning of 2014, Verily (the new name for Google Life Sciences) continues to reach out to partners to bring a final product to the market. Stay tuned.
At the engineering labs of UCLA, Aydogan Ozcan is also working on a sensor of the future, or rather a series of attachments that can turn your smartphone into a series of powerful sensing devices. Using a 3D printer to create housings that can snap to the back of a smartphone, Ozcan’s team pops in various electronics designed to measure biometric parameters, often leveraging the phone’s own built-in camera. These sensor modules can scan for viruses in a blood sample, measure toxins in water, or detect trace amounts of a known allergen inside a bit of food, and then send information to an app installed on the phone.
While a Smithsonian magazine article recently compared Ozcan’s creations to Star Trek’s mythic tricorder device, the comparison isn’t yet 100 percent. For one thing, doctors on Star Trek would simply wave the tricorder in the air in front of the patient and instantly diagnose them, but Ozcan’s creations still require the user to place a physical sample onto a sensor or in front of a camera lens. On the other hand, a tool that can identify a virus in the field is still pretty damned powerful, even if you have to insert a blood sample into the device. Combined with the smartphone’s connectivity to the Internet, it’s more like a portable bio-lab than a tricorder, a fact that only becomes more impressive when you consider that running a full lab can cost millions of dollars, while one of Ozcan’s prototypes cost something like $10.
That low cost of entry theoretically puts the capabilities of a full lab into the hands of anyone with a smartphone. Locals could test the quality of their water supply with their own phones instead of having to call in the government, or doctors in the field could immediately detect the presence of a pathogen without having to send a sample to the lab.
Such tools could have huge democratizing power, even in locations where local infrastructure is weak to nonexistent, allowing people across the world to take better control of their own destinies.
Just think how this could have helped the residents of Flint, Michigan with their fight against a government who insisted that tapwater that looked like root beer was okay to drink.
Hi, I’m Your Robot Doctor ... Wait! Come back!
Robots have been in the operating room for quite some time now, as assistive devices for actual surgeons. These specialized pieces of equipment have several advantages:
• They are more accurate, reducing the need for extensive cutting and minimizing blood loss.
• They allow doctors to sit down while working, reducing fatigue.
• They contain corrective algorithms that would remove tremors found in the surgeon’s hands, preventing it from being transferred to work done on the patient.
• And, the robotic tools and cameras can be positioned in ways that were just not possible for a human surgeon to accomplish using old methods.
Robotic devices in surgery can also perform automatic tasks quickly and precisely, such as certain types of incisions or in-surgery bone manipulation, using a prestored algorithm and feedback provided by the tools as they do their work. They’ve also been much-used in certain types of procedures where a miniaturized touch would be more appropriate, such as heart surgery or certain types of catheterization.
The one thing robots have not been able to accomplish, though, is completely autonomous diagnosis followed by delivery of the appropriate corrective procedure. Human input is still always required. It’s also a pretty good bet that if you asked most people out there if they’d be comfortable with a robot performing surgery without any human input whatsoever, most would be reluctant.
Maybe that’s an odd position to take, considering the trust we are now putting in autonomous cars to make their way through traffic without hurting or killing anyone. At the time of writing, the majority of accidents that have occurred involving self-driving automobiles have been the fault of human drivers in other vehicles. Taken to its logical conclusion, handing the wheel over to your robot driver seems like the safest course, leaving you free to catch up on your reading, knitting, or yoga.
On the other hand, the stakes seem low if a self-driving car were to malfunction. You might be hurt if a car drives into a guardrail or even into the back of another car, but hopefully the car’s other safety functions (such as airbags and seatbelts) will prevent any truly serious injuries. And, theoretically, if you notice something going wrong, you can take manual control of the vehicle.
That’s not the case when you’re going in for surgery, of course. While it’s true that a malfunctioning robot doctor can result in little or no actual damage before a trained surgeon steps in, it’s easy enough to imagine a nightmare scenario where a scalpel started cutting a number of things that weren’t really meant to be cut. But what’s the likelihood of something like that happening? Given the record of self-driving cars, it seems that autonomous robot surgeons could well be the safest option—after all, it’s more likely that you’ll get sliced and diced by a bleary-eyed doctor with a hangover and an unsteady hand.
And if you are still unsure, most of you let robots handle your money. ATMs are robots. And tellers can have hangovers, a bad day, or sociopathic tendencies.
“... most of you let robots handle your money. ATMs are robots.”
For the record, your authors discussed this very topic on one of our official Weekly Author Conferences Online (yes, WACOs) as we developed this chapter.
Andy says he would feel perfectly happy trusting his vasectomy operation to a robot, and has no worries whatsoever that his manly bits could be snipped off and turned into a coin purse by a renegade robo-surgeon with a wonky algorithm. (Programmers have bad days too.)
For the record Sean is not so confident. While he’s pretty sure that the latter scenario wouldn’t happen, he’s still not convinced that he wants a robot digging around “down there” without any type of human supervision.
Kay, when she heard the other two talking about such things, rolled her eyes.
Perhaps there’s a middle ground.
While Meskó doesn’t believe that robots will be performing autonomous surgeries any time soon, he believes that computers and robots could well work in concert with human beings, with human doctors having the final say. And the reason? Computer technology can provide a much greater wealth of information about the surgical procedure immediately at hand than any human surgeon ever could.
“If you take the best professor in the world in a specific medical specialty, he or she might have 40 to 50 medical papers in mind at once. IBM’s Watson can check 200 million of these in 1 second. So we cannot compete with that. But that’s all right,” he said, noting that doctors could always use Watson in the decision-making process. That’s something that has already been going on at Memorial Sloan Kettering Cancer Center. “Based on textbooks and the 200 million papers in the world and the patient’s medical history, IBM Watson makes a few suggestions to a doctor and based on this, says ‘you might want to think of this test or this treatment or this diagnostic’. And doctors, they love this method because they felt more sure. For humans it’s impossible to keep in mind all these millions of papers.”
“This collaboration could also be used in concert with information about the patient’s genomic information to provide a more informed direction for treatment,” says Meskó. “Imagine, as a doctor, I can do a search because I have a 40-year-old male patient (with these types of symptoms) and data points and biomarkers in their blood, and what can I expect? What if I can look at 10,000 same-gender, same-age, same-population people with the same health parameters and lifestyle and I could see what happened to them after using this treatment? So, I could make the best-informed decision in the world because I would have all the information I would possibly need.”
In the short term, robot assistants are starting to perform some tasks around the hospital that are less productive for some human staff members. Vecna has created a mobile robot called the QC Bot. The staff at France’s Centre Hospitalier de Beauvais, where the robot was deployed, refer to it by the much friendlier name “Diane.”
“Diane” and her QC Bot relatives can serve multiple functions. Like the robotic mail carts that roll around many large office buildings, QC Bots can carry supplies from point-to-point around the hospital (see it in action here: http://superyou.link/qcbot). It also comes with a large screen and an onboard camera, enabling it to serve as a self-serve station for patients—people can check in for their appointment and follow the QC Bot right to the proper room where they’ll be seen by the doctor. The robots also come with the capability to kick into telepresence mode with a remote health provider when required, allowing health providers to consult with experts in other parts of the hospital, or for patients to talk to doctors.
“Robot assistants are starting to perform some tasks around the hospital that are less productive for some human staff members.”
All these tasks can help free up doctors and nurses, according to Daniel Theobold, Chief Technology Officer of Vecna, who explained this in an interview on the Healthcare Tech Talk podcast.
“In the pharmacy, when they prepare a cart full of medications that needs to get to a particular patient ward, it is literally a 15-minute walk from the pharmacy to that ward to just deliver that medication. That’s 15 minutes that a nurse is spending not providing care to patients. So when they can load those medications up in the robot with confidence, know that the robot is not going to lose them along the way, know that nobody is going to get into the robot and take them, and know that that medication is going to get to where it needs to be, when it needs to be, and now I can turn my attention to actually doing what I was trained to do as a nurse, and that is provide care to patients. That’s a win-win for everybody.”
This type of interaction requires a lot of research, he notes, as robots don’t see the world the same way we do—it’s all just a bunch of pixels to them. They also need to be trained in the kind of social cues humans use with each other when they intend to interact with one another, such as eye contact or gestures, because there are many variables to track. While the QC Bot has mastered some of that type of interaction, there’s still a long way to go before it would be even remotely capable of rolling into an operating theater and performing Andy’s vasectomy.
“... there’s still a long way to go before [the QC Bot] would be even remotely capable of rolling into an operating theater and performing Andy’s vasectomy.”
DIY Health
We know what you’re thinking. With all these medical technologies rolling out, we might be entering an era where you can finally take full control of your health right from the comfort of your own home. Almost certainly that last sentence causes some panicky moments for anyone who’s had to deal with a loved one who’s freaked out after taking a look at WebMD, and then become convinced that they had the rarest disease ever known to mankind.
“Honey, I think I’ve got ataxia telangiectasia. I read up on it on WebMD. I’ve got the shakes and little bumps on my skin.”
“Umm, I don’t think so. You have a hangover and you drank pomegranate-tinis when we ran out of cranberry last night. You’re allergic, remember?”
The good news—the future is a bit rosier than that. That’s thanks to inexpensive new options such as the $1,000 genome sequencing module we looked at a earlier in this chapter. With the ability to scan your own DNA at a reasonable cost—the immutable law of diminishing technology prices are in play here—you’re entering a world where you can get actual readings of what’s going on in your genetic makeup, rather than simply misreading a list and running around in circles thinking you’re going to succumb to a rare childhood disease.
Now imagine, with your genomic information in hand, having the ability to calculate what pharmaceuticals you should be taking for conditions such as hypertension or hypothyroidism, and then printing the drugs out on your home 3D printer as you need them. There’s no need to haul your carcass down to the clinic just to convince your doctor to renew your only semi-effective prescription yet again. All that information would be gathered by your home scanner and, potentially, verified by a giant remote computer in the Cloud—such as a descendant of IBM’s Watson—to be sure there aren’t any errors in the formula of your new home-brew drugs.
Or, imagine that you have a robot at home that can put you under with a dose of sedatives, open you up, and 3D print a healthy new kidney right into you. No more waiting around for some poor sap (who was otherwise healthy) to die in an unfortunate car accident.
We’ve already heard of people who have started to 3D print their own prosthetic limbs at home, complete with robotic servos inside to move fingers with the proper muscle input where the prosthetic attaches to the body, but this will almost certainly become more commonplace.
It’s relatively inexpensive now to buy 3D scanning equipment to create a three-dimensional model of your body, but it’s easy enough to envision a future where an amputee can scan the end of their arm or leg to get exact specifications, and then 3D print a prosthetic that fits perfectly onto the end of a limb that was partially amputated. All of this could happen at a fraction of the cost of having a new prosthetic limb cast at a medical lab, especially a limb containing robotics.
The whole DIY ethic is nothing new to a whole new generation of tech-savvy people who are trying to take control of their health. A growing number of people are starting to track their daily step-count and their heart rate through wearables such as the Fitbit or the Apple Watch. With the use of these easily available devices, combined with manual tracking of diet, sleep, weight, and other specialized exercise, people can build up a pretty robust profile of their general state of fitness.
And then there are people who are willing to go a step further and implant themselves with diagnostic devices such as temperature sensors or radio-frequency identification (RFID) chips that could contain medical information for emergency use. In the future, these implants could well expand to devices that measure your heart rate, breathing, or neural activity. At that point, people could do self-diagnostics with a wand they wave over various parts of their body, and if they receive errant readings, book an appointment with the doctor for a tune-up. We’ll take a further look at these self-implanting maniacs in Chapter 6, “Franken-You: A Better Life Through Cyborg Technology”.
Whether you end up going to futuristic new hospitals, or end up taking care of all your health needs from the comfort of your own Barcalounger, one thing is exceptionally clear. The future of medicine will be extremely personalized.