Chapter 1
Introduction
Pain Points
One thing that many of us SAS employees have in common, aside from our love for free M&M's and Zumba class at lunch, is something a little less glamorous. It's unfortunately pain: back pain, shoulder pain, neck pain, you name it. But it isn't unique to SAS. Many corporations, especially large software companies like us, share the same challenge. With over 5,000 people on our Cary, NC, campus, we definitely have our fair share of hunched-over-their-computer-screen employees.
Don't take me wrong, though; SAS isn't one of Fortune's top places to work for nothing. While we have world-class healthcare, a wonderful fitness center, and an ergonomics department all onsite, we, however, can't escape the fact that some jobs require long periods of sitting. Well, it turns out that sitting is really bad for you and can evolve into some serious chronic pain. And unfortunately, the M&M's don't relieve pain.
Chronic pain has become so widespread that one out of three Americans suffers from it and it costs our nation over $600 billion a year, which is more than the yearly costs for cancer, heart disease, and diabetes.1 That's probably the least alarming statistic. Lower back pain, for example, affects 80 percent of the adult population and is the number-one cause of lost workdays in the United States.2 And often, that's just the beginning of the vicious pain cycle; chronic pain can lead to obesity and chronic diseases such as diabetes, and to injuries and employment disabilities, not to mention the loss of productivity and costs to individuals and employers like SAS. But it's not just the adult population who's in pain. Have you ever heard of “text neck”? The younger generations—whose lives revolve around mobile and tech—are experiencing pain as young as in their teenage years; so much so that it's estimated that 25 percent of today's young adults will become disabled before they retire.3
Pain is tricky and confusing in so many ways, which makes it a really difficult problem to tackle. It can fluctuate a lot in intensity, occur in multiple places at once, and it doesn't always appear where the problem originates from. It really doesn't help solve the mystery when the pain in your right knee is contributing to a problem in your left gluteus. (Yes, that's how strange it is.) In a nutshell, it's a hard thing to get to the bottom of. Listening to so many pain stories over the years, I found that people often accept pain as a regular part of their lives. There was my friend Leigh, who was visiting a chiropractor biweekly for five years straight—it was a part of his Friday routine; my colleague John, who was in so much pain for two years that he one day found himself lying on his office floor unable to get up; and Melissa, whose lower back pain that she kept avoiding eventually led to severe knee pain. And there was my own experience in which my long nights of sitting (thank you, grad school) led to pain all over my right side. It was beyond physical, though; the emotional toll it took on all of us was draining. Managing the consequences of pain was tough. Tracking it was tough. Finding a solution was tough. I really wanted to do something about it.
Sometime last year I had an idea that could possibly help people manage their pain better. And after seeing some of the outrageous statistics, I was convinced that there was a way to curb some of the $600 billion in costs. So about 30 seconds after my brainwave moment (I admit I briefly felt as if I'd solved all the world's problems), I called my friend Lance, who's the CEO of DXLab—a local design consultancy that creates remarkable products and services. Following an hour-long phone conversation about the pains of pain, Lance and I mapped out a plan for incubating my idea and we were on our way.
Birth of a Start-up
Lance and his team at DXLab use a process called design thinking to take ideas to implementation in a short period of time. Design thinking is a human-centered approach to innovation that translates observations into insights and insights into products and services that improve lives.4 I've been a fan of the methodology since I was introduced to it during my days at NC State University, because of the way it converges creativity with business innovation. Its emphasis on human needs is what drives the approach and is what makes it ideal for solving healthcare challenges.
The process that Lance described to me was simple and refreshing. It looked like Figure 1.1.
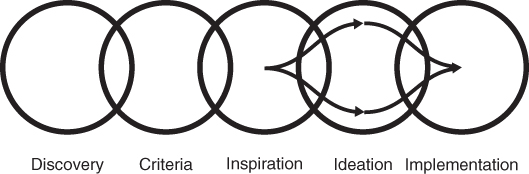
Figure 1.1 Design Thinking Process
Design thinking is unique because it gets people involved from the get-go. The very first thing we'd do is customer discovery—to understand the real issues of managing pain from the customer's point of view, rather than my point of view. Is managing pain really a problem for people? Connecting with people and hearing their stories lets us gain empathy for the individuals, and also helps us define and validate our problems.
So that's what I did. Luckily, I had already expedited this step through many previous conversations around pain, but to put the structure I needed around it, I spoke with several individuals, through workshops and one-on-one interviews, to dive deeper into their pain stories and experiences. I wanted to understand both their obvious needs and their latent needs—needs that may be more difficult to articulate. But my customers weren't only those individuals experiencing pain. It was important to extend my understanding to their network of interactions and to hear how the issues affected them as well. So I connected with those who treat and manage pain; medical professionals such as physical therapists, pain medicine specialists, and chiropractors play an important role in the management of pain.
At the end of these conversations, I had defined and validated multiple problems from the patients' and the providers' points of view. It turned out that there were just as many problems on the provider side in managing pain as there were on the patient's side, and this shed light on what some of the barriers in pain management are. Most important, though, I gained a sense of empathy for both the patients and providers—the first and foundational component of human-centered design. It's something we don't do in healthcare as much as we should, even though we strive to be a patient-centric system. Taking this step before any discussion of the technology or design of the product was eye-opening and put me in a much better position to create something that met both the functional and emotional needs of individuals.
What I learned when I began to see the issues through their eyes was invaluable. I heard about many patient experiences, both good and bad (mostly bad), as they dealt with their pain. Some people had seen dozens of providers for their pain; some of them blamed their provider for their continuous pain; many were frustrated with trying to keep up with their evolving pain and trying to explain it to their providers; many thought they'd find a cure quicker if they weren't having to go from provider to provider to find the best treatment. And everyone said their pain might be healed quicker if the experience was better, more seamless, and easier. What they wanted was meaningful conversations, to get more value out of their doctor's visit, to share their pain story more effectively, and most important, to find a remedy to their pain. One thing was absolutely certain—managing pain needed to be a better experience.
A huge untapped market began to take shape before my eyes, and thus, Remedy was born.
Experience Is the Teacher of All Things
About a year ago, I finally got around to reading Change by Design, by Tim Brown, CEO and president of the highly talented design firm IDEO. The book had been on my reading list for quite some time, and I found it so stimulating that I read it from cover to cover on a six-hour flight to Seattle. The book describes the concepts of design thinking in a simple but enriching way, and the applications Brown draws to our daily lives had me unfolding idea after idea of how it could be applied to healthcare. At the time, I had already begun writing The Patient Revolution, but was so inspired by Brown that I scratched my initial drafts and constructed an entirely different approach.
I used the design thinking process as a framework for this book and to organize my thoughts. I also wanted to shed light on how the human-centered approach can be applied to the healthcare system, both broadly and to individual healthcare issues. Needless to say, this book is very much inspired by Brown's ideas. And while that may have been the best thing that happened to it, I did take a mini-vacation from my reading list to spare myself the possibility of starting over again.
What's Your Healthcare Experience?
In his book, Brown says that whether we're sitting on an airplane, shopping for groceries, or checking into a hotel, we aren't just carrying out a function, but having an experience. The same is true when we engage with the healthcare system, but despite our attempts to be patient-centric, we don't always consider the experiences of individuals as they move through the system. Moreover, our approach to health, arguably the most important aspect of our lives, still lacks personalized experiences that create opportunities for active participation.
Creating those experiences is, of course, not easy. Healthcare, unlike many other systems, isn't a single stream of predictable and regular events. It's uniquely personal to each individual, and that's what makes it so difficult to personalize. Like Dr. Marty Kohn, chief medical scientist at Sentrian, says, unlike Jeopardy, healthcare is not deterministic; there's often no one right answer since many patients have multiple comorbidities. Each individual undergoes a unique health journey; hence there's no one story that characterizes the healthcare experience.
Take a moment to think about some of your experiences with the healthcare system, perhaps a simple event, like your annual physical exam, or something more complex, such as a surgery that required extensive pre-op and post-op care. What series of events occurred throughout the process? Do you think that those activities catered to what's desirable to you? Did you find yourself actively participating or passively consuming?
The Experience Economy
Joseph Pine and James Gilmore say we're now living in what they call the “experience economy,” in which people shift from passive consumption to active participation.5 Services across most industries have fully shifted toward delivering experiences, and most have gone beyond that to provide personalized and customized experiences. This is what Pine calls the transformation economy, which is the final stage in his chain of economic value. In the transformation economy, services are designed so specifically for a person that they are life-transforming for the individual.6 In other words, the experience changes us in some way.
If you're an online shopper like me, you're very aware of how the growth of the experience economy and the emergence of the transformation economy have revamped the online shopping experience. Not only is your shopping personalized to your likes and dislikes, but your experience is your unique experience. That means a retailer learns things about you like your lifestyle, preferences, and shopping habits, so that they can be proactive in giving you a truly personalized experience. And with new innovations like smart watches and one-click shopping, the mobile shopping experience is becoming an increasingly fun and engaging part of our lives. For example, products like the Google Ventures–backed Spring (www.shopspring.com) are attempting to re-create the shopping experience with a “one-click-to-buy” feature. And other industries, like financial services and hospitality, are making similar transformations; with services like Mint (www.mint.com), you can manage your financial health through personal budget and goal-setting, and receive custom recommendations for saving money. Even hotels are tailoring each part of the experience for guests, from entertainment and technology to pricing and communications.
These services are focusing on the total experience for their customers, which makes the experience continuous and all-inclusive. It's no longer about a one-night hotel stay or your one sporadic shopping spree; hotels and retailers are now customizing experiences for you before, during, and after your service. So now you may be checking into your room early on your mobile device, preordering television programs and snacks before you even arrive, and receiving personalized recommendations of places to eat near your hotel. And after you leave, you may receive promotions and offers catering to your preferences, encouraging you to plan another stay at the hotel. It's a continuous relationship that keeps you actively participating while blending into your daily rituals, like texting or perusing your Twitter feed.
Now think back to your healthcare experiences from earlier. Do they feel as seamless and continuous as these others? Do you feel like an active participator in your healthcare before, during, and after services?
Experiences are important to products, services, and systems because, simply put, they create happier customers. The key to excellent experiences is to focus on totality and consider every element across people, process, and place. By creating an unwavering consistency in delivering value, experiences result in more engaged and more satisfied customers. It's not an easy thing to do, but is entirely possible with the right understanding of your end-users and the right tools. I'll talk more about this later, but first, let's take note of what's going on today with the healthcare system.
#healthcaretrends
The Affordable Care Act (ACA), also known as Obamacare, has since its inauguration in 2010 prompted a variety of transformations throughout the healthcare system. And while it's been a topic of ongoing debate since its inception, the ACA has brought forth many innovations toward a new health economy focused on consumer value. Healthcare payers, providers, and policymakers are exploring new initiatives to improve the health of individuals while managing the escalation of costs, including new service and payment models. Marketplaces are being created for consumers to purchase healthcare insurance, researchers are examining novel datasets to advance the field of precision medicine, and much, much more. Lots of unprecedented activity is taking place at all levels of the health ecosystem.
Volume to Value
If you're in the healthcare industry, you've likely heard by now of the paradigm shift that's happening from volume-based care to value-based care. The traditional “fee-for-service” model of healthcare reimbursement is well on its way out, as value-based payment is quickly becoming the new norm. This means that instead of being paid by the number of visits, procedures, or tests, providers are now being paid on the value of care they deliver to individuals. The switch has really turned the traditional model of healthcare reimbursement on its head, causing providers to change the way they bill for care. Providers are taking on more of the risk, as new payment models that reward outcomes and penalize poor performance, such as high rates of readmission and hospital-acquired conditions, are proliferating. These models require teamwork and collaboration between physicians, and many provider groups are establishing accountable care organizations (ACOs) to facilitate this. ACOs are teams of care that are accountable to the patients they serve and focus on the complete care delivery of patients and of populations. They require a high level of coordination among providers and the use of data and technology to succeed.
Insurance Marketplaces
The Health Insurance Marketplaces is one of the flagship components of the ACA, which is underpinned by the goal of improving access to healthcare across the nation. Each state was required to establish an insurance marketplace or participate in a federal exchange by January 1, 2014. By establishing marketplaces and mandating that insurers must sell coverage to all people with no price variation based on health status, the ACA has boosted the creation of retail-style health insurance. The exchanges encourage individuals to shop, compare pricing and coverage options, and select a health plan as an informed consumer. It's exciting to think that people who may have never had health coverage before now can at an affordable rate. The second year of open enrollment closed with about 11.7 million people signing up for coverage on the state and federal marketplaces.7
As health insurance moves from a business-to-business (B2B) model to a business-to-consumer (B2C) model, PricewaterhouseCoopers predicts that insurers will continue to zero in on the notion of consumer-directed health, as plans focus on the consumer experience across all lines of business and not just the individual market.8
Interoperability
Interoperability describes the extent to which systems and devices can exchange data and interpret that shared data. In 2009 came the big launch of interoperability efforts as healthcare reform began to push heavily for the digitization of health records through electronic medical records (EMRs)/electronic health records (EHRs), and patient portals. An incentive program called Meaningful Use was put in place by the federal government to encourage providers to meaningfully use EHRs. Meaningful Use sets specific objectives that providers must achieve to qualify for the incentives, and the objectives include things like improving quality, safety, and efficiency; reducing health disparities; engaging patients and families; improving care coordination; and maintaining privacy and security of patient health information.9 Providers have certainly got on board, as Centers for Medicare and Medicaid Services had delivered payment incentives to more than 468,000 healthcare providers as of July 2015.10
The year 2009 also saw the State Health Information Exchange (HIE) Cooperative Agreement Program (State HIE Program), which offered states and territories $564 million in funding and guidance to enable secure electronic information exchange. According to the federal government, the purpose of the State HIE Program is to “facilitate and expand the secure, electronic movement and use of health information among organizations according to nationally recognized standards.”11 While each state now currently has some sort of exchange in place for the sharing of healthcare data, there's still significant progress to be made in interoperability. The ultimate goal is to create a national health information network, and that's why the Office of the National Coordinator of Health IT (ONC) released a ten-year roadmap for nationwide interoperability in January 2015. It's a wonderful vision to work toward and definitely puts forth the awareness that interoperability is a key priority over the next decade.
Other Trends
Aside from value-based care, insurance marketplaces, and interoperability, trends like transparency, focus on prevention and wellness, and reduction in fraud, waste, and abuse have all surfaced due to healthcare reform. Additionally, state governments have taken on a lead role in healthcare reform, through Medicaid expansions, by leading payment reform initiatives, and by creating new healthcare exchange models and databases like all-payer claims databases.
While many may argue that these changes are long overdue, it's still very inspiring, as it's setting the groundwork for creating better healthcare experiences and improvements to the delivery of care.
