6
Searching for the Fountain of Health: Can We Match Healthspan to Lifespan?
MEDICAL SCIENCE IS making astounding progress with the diseases and conditions of aging. Robots are conducting eye surgeries. Robotic underwear can assist the hips and lower back to support mobility and posture. Smart pills can monitor gastrointestinal functioning, and genetic editing will be able to improve digestive health by altering the microbes in people's guts. Deep brain stimulation, including with the help of virtual reality, is helping patients regain motor function after being paralyzed by strokes. Genetically reengineered T cells are returned to a patient's body as part of an immunotherapy approach to cancer treatment. 3-D bioprinters can produce living tissue, bone, blood vessels, and soon entire organ systems.
Artificial intelligence is getting into the game. Canadian health-monitoring platform BlueDot alerted its customers to the Wuhan coronavirus outbreak a full nine days before the World Health Organization notified the public. BlueDot's AI algorithm combed through foreign-language news, information on disease networks, and official proclamations to pinpoint the outbreak. In addition, with its access to global airline data, BlueDot accurately predicted when and where the disease would spread.1
Just as notable is who's entering the business of health these days. As The Verge has reported,2 Amazon acquired PillPack and with it a medical records software platform. Apple, which has long partnered with medical and government institutions, continues to expand its Apple Health medical records app, and the Apple Watch can take one's EKG. Alphabet's Verily Life Sciences company pursues medical research collaborations, for example, with ResMed to tackle sleep apnea. And Google is consolidating its health industry initiatives, including AI assistance to physicians and health-monitoring technology for nursing homes.
Health providers can now book rides for patients or caregivers through Uber Health, and Lyft has partnerships with BlueCross BlueShield. Some early setbacks notwithstanding, IBM continues to make Watson artificial intelligence and natural language processing technology a centerpiece of its health division. Microsoft Azure is partnering with Epic Systems to provide cloud-based artificial intelligence and predictive analytics to health care organizations. And Stanley Healthcare, part of the Stanley Black & Decker tools empire, offers patient safety and security solutions to health care providers.
Why is everyone flocking to the health care space? Mary Furlong, EdD, author of Turning Silver into Gold: How to Profit in the New Boomer Marketplace and a leading pioneer on the longevity marketplace, puts it concisely: “Every dissonance of aging – from joint pain to diabesity – is a market opportunity.”
At $3.65 trillion annually, health care is one of the largest industries in the United States. It is also inefficient and fragmented, with many potential niches to fill. It's no wonder that major corporations in other industries, especially technology, are getting into the health care business. But for all these investments and advances in technology and techniques, staying healthy as we age remains a problematic proposition.
In the United States we spend over $10,000 annually per capita on health care, more than any other country and 25% more than Switzerland in second place. Over one-third of that spending is on people age 65 and older (who represent about 17% of the population). But, as we mentioned in Chapter 1, that spending does not necessarily buy results in terms of longevity, where the United States ranks 33rd (almost six years behind Japan), or overall health of the population, where it ranks 35th (Spain is first).3 Promising treatments are always on the horizon, but we await breakthroughs against the leading causes of death, starting with heart disease and cancer (Figure 6.1), and what has become the most debilitating and feared condition of age, Alzheimer's.
Retirement's Biggest Wild Card
Health is the biggest wild card in a happy and fulfilling retirement. It can make the difference between a retirement of activity, happiness, independence, and financial security – or of worry, unhappiness, constraint, and financial insecurity. Boomers are a very health-conscious cohort and, compared to past generations, they can look forward to longer and healthier retirements, perhaps extended by breakthroughs in disease prevention and medical care. But at the same time, more of them may spend more years later in retirement fighting the chronic and often debilitating diseases of aging.
Which will it be? Are we approaching Shangri-la, the fictional valley where people don't age, with longer and healthier lives and accessible and affordable care? Or are we headed to Geriassic Park, with tens of millions constantly beset by chronic and degenerative diseases, taking a toll on themselves, their families, and their finances? The fields of health science and health care may be moving fast, but the jury is still out.

Figure 6.1 Leading Causes of Death in the United States
Source: National Center for Health Statistics, Health United States, 2017
In the meantime, what do Boomer retirees say they want? To take charge of their health because they don't trust the system to take care of them. To prevent or manage their chronic conditions so they can live the active lifestyles they want. To avoid cognitive decline. And to stay healthy and look and feel their best without breaking the bank. Do they want to live to be 100 or more? It's an intriguing prospect, but only 22% of Americans say yes. Among those already 65 and older, twice as many say no (35%) as yes (17%). The most common response, of course, is “it depends on quality of life.”4
The real issue is not lifespan but healthspan – how long people live in “full health” without disabling illnesses or injuries. In ancient Greek mythology, Eos, the beautiful goddess of the dawn, falls deeply in love with the warrior Tithonus. Distraught over his mortality, she goes to Zeus to request a special favor: she wants to love Tithonus until the end of time and begs Zeus to grant her lover immortality. “Are you certain that is what you want for him?” Zeus challenges. “Yes,” Eos responds. But as she leaves Zeus's chamber, she realizes in shock that she forgot to ask that Tithonus also remain eternally young and healthy. With each passing year, she looks on with horror as he grows older and sicker. His skin withers and becomes cancerous. His organs rot, and his brain grows feeble. As the decades pass, Tithonus's aging body becomes increasingly frail, yet he cannot die. Ultimately, the once-proud warrior is reduced to a collection of pained, foul, and broken bones – but he continues to live forever.
Tithonus's story is a fitting allegory for what is occurring in health care today. Until recently, most people died swiftly and relatively young of infectious diseases, accidents, or in childbirth. During the past century, however, health care breakthroughs have eliminated many, but not all, of those threats. Today, rather than worrying about dying too young, many people worry about living too long without sufficient quality of life. In the United States and most of the industrialized world, the difference between life expectancy, or lifespan, and healthy life expectancy, or healthspan, is almost 10 years.5 Whether we're headed toward Shangri-la or Geriassic Park is a matter not just of extending life, but of better matching healthspan to lifespan. That requires progress against both the infectious and the often debilitating chronic conditions associated with aging, and progress toward the behaviors that protect our health and well-being.
The Health-Wealth Convergence
Retirees say the key ingredients for a happy retirement start with good health and financial security, with good health in the lead by a significant margin (Figure 6.2). But the two are closely related. Those with wealth can invest more in their health. And it's harder to enjoy wealth – and all the activities it enables – if you're in poor health. At the same time, unpredictable health care costs can quickly unravel financial preparations for retirement and deplete one's wealth. As more people spend more years in retirement, they'll need more care, and as health care costs continue their rise, health and wealth become more intricately intertwined.
Even with many people postponing retirement in order to build their nest eggs or simply because they enjoy their work, nearly four in ten (39%) retirees globally and nearly three-fifths (58%) in the United States retired sooner than planned, and the number-one reason is due to their own ill health (Figure 6.3). Early retirement is for some a sign of financial success, but today it's more often driven by health issues. That's a double whammy: a shorter career means less in earnings and retirement savings to start retirement with, especially for people who haven't saved enough and had hoped to plump up their nest egg by working longer. Then those savings must be tapped earlier than planned and health expenses may deplete them faster.
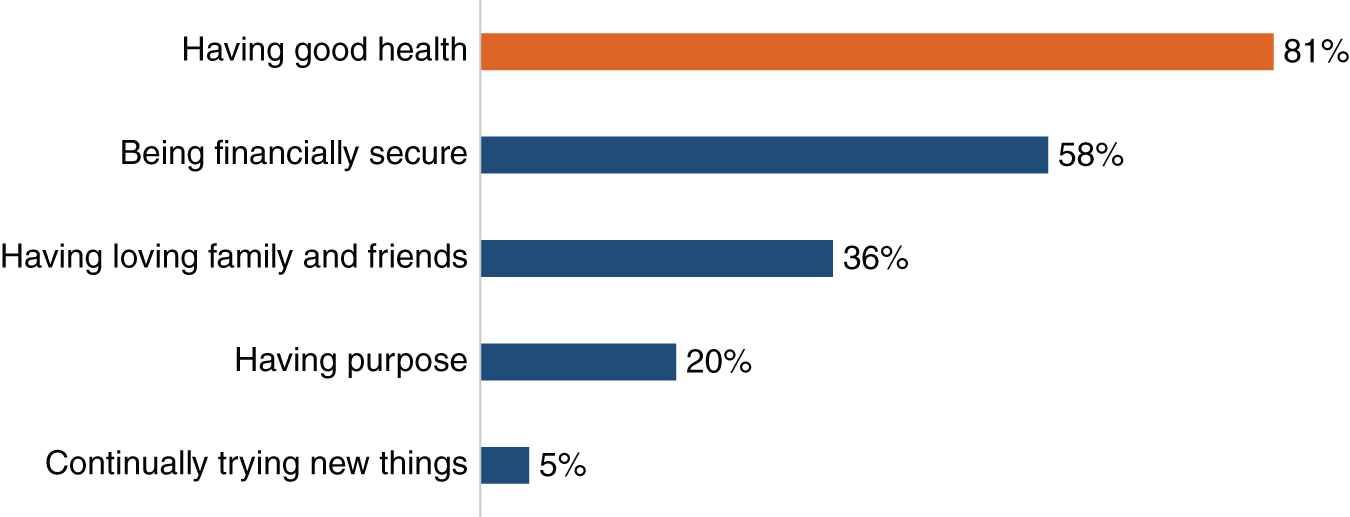
Figure 6.2 Most Important Ingredients to a Happy Retirement
Source: Age Wave / Merrill Lynch, Health in Retirement: Planning for the Great Unknown
What catches many people off guard are the out-of-pocket health-related costs they'll face throughout their retirement. The longer they or their partner live, the higher the accumulated cost. So it's no wonder that health care costs, unpredictable and potentially high, are retirees' greatest financial worry.6 And those financial concerns are a family affair. Spouses and partners naturally worry about each other's health, and women, who are likely to live longer, often after having spent savings on the spouse's care, are more worried than men about the long-term financial impact of health care expenses. One retiree expressed the concerns shared by many: “My husband and I have always tried to do the right things – save money, maximize our 401(k)s, even delay retirement a bit. But who knows how long we'll live and what might happen to our health? Will that make us outlive our savings? It's a scary thought.”
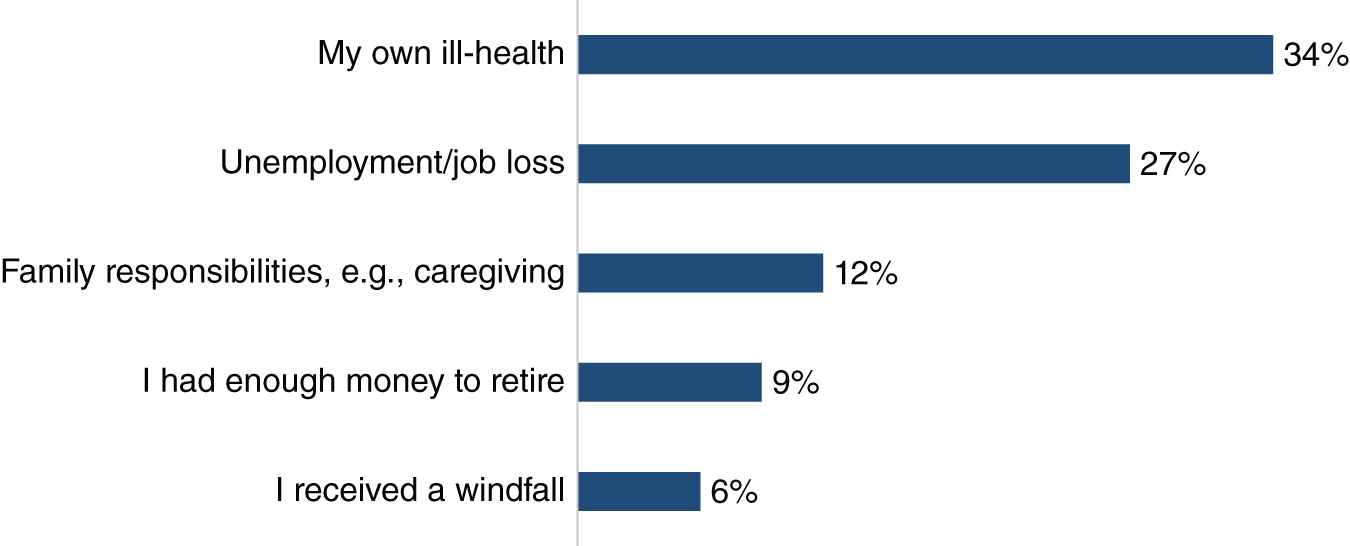
Figure 6.3 Reasons for Early Retirement Globally
Source: Aegon Center for Longevity and Retirement, The New Social Contract: Empowering Individuals in a Transitioning World, 2019
Ken Cella, who leads the Client Strategies Group for Edward Jones, describes the growing role of health in retirement preparation:
Longevity planning is so much more than simply an investment discussion. So many of our clients talk about health as a key focus in their retirement, so we are having more and more conversations about how our clients want to age with dignity, using long-term care solutions that allow them to receive in-home care. We also train our financial advisors to recognize the 10 warning signs of Alzheimer's, for example. And we have a responsibility to have trusted contacts named for our clients, so we can reach out to those contacts if we are concerned about issues such as elder abuse or fraud. We have to go beyond helping our clients create wealth to helping them navigate the often complex journey to and through retirement – so they can experience meaning and purpose during this third phase of life.
Taking Charge of Health: The Self-Care Revolution
Their approach to health is one of the pronounced differences between Boomers and their parents. Boomers were behind the fitness movement that saw the proportion of adults who exercise regularly more than double between the 1960s (25%) and the 1980s (60%).7 They have helped drive the growth of health club memberships from 53 million to 71 million over the last decade.8 And they are driving the current growth of alternative, complementary, and holistic medicine. But as singer Al Jolson famously said, “You ain't heard nothing yet.”
Americans over 50 account for 64% of all expenditures on vitamins.9 Boomers are more open than older generations to alternative treatments to beat cancer. Nearly 80% of Boomers say they support medical marijuana use.10 The global complementary and alternative medicine market, which includes botanicals, acupuncture, and mind/body/yoga therapies, is expected to grow from $60 billion in 2018 to $211 billion in 2026.11
Precision Medicine
Boomers want more precise and holistic care of body and mind, not just treatment of their symptoms. So integrative and precision medicine are gaining traction fast. An early pioneer is Dr. Andrew Weil, author of Healthy Aging and founder and director of Center for Integrative Medicine at the University of Arizona. Integrative medicine is a healing-oriented approach that takes account of the whole person (body, mind, and spirit), including all aspects of lifestyle. Dr. Weil created an anti-inflammatory diet to ward off diseases like heart disease, Alzheimer's, and some cancers. Its principles include maximizing intake of fresh fruits and vegetables and minimizing processed and fast foods. True Food Kitchen, a restaurant chain based on the anti-inflammatory diet, plans to have close to 40 locations by 2022.
One of the most courageous pioneers in the field of preventive medicine for healthy aging is Ken's longtime friend Dr. Dean Ornish. President and founder of the nonprofit Preventive Medicine Research Institute in Sausalito, California, and a Clinical Professor of Medicine at the University of California, San Francisco, Ornish disrupted the nutrition and medical fields in 1995 with the publication of his bestselling book Dr. Dean Ornish's Program for Reversing Heart Disease: The Only System Scientifically Proven to Reverse Heart Disease Without Drugs or Surgery. Over the decades, he has been an unrelenting advocate for using diet and lifestyle changes to treat and prevent heart disease. Ornish's approach, which he now recommends for a wide range of chronic conditions from heart health to prostate cancer to dementia to aging itself, incorporates a primarily plant-based diet, smoking cessation, moderate exercise, stress management techniques, including yoga and meditation, and holistic psychosocial support.
Another influential figure in the Boomers' quest for the fountain of health is Dr. Mark Hyman, author of Food: What the Heck Should I Eat and many other popular books. He is the Medical Director of the Cleveland Clinic's Center for Functional Medicine, which seeks to identify and address the root causes of disease, and views the body as one integrated system, not a collection of independent organs divided up by medical specialties. Functional medicine treats the whole system, not just the symptoms. Programs include functional-based approaches to weight loss and blood sugar control that incorporate lifestyle changes, dietary guidelines, and a specific supplement regimen.
The SHA Wellness center may provide a glimpse into the spa of the future. Located in Alicante, Spain, SHA positions itself as a pioneering clinic, focused on improving people's health and well-being “through the fusion of natural therapies, mainly originated from millenarian Eastern wisdom with Western techniques.” In addition to what a typical spa would offer – massage, facials, manicures, and body wraps – SHA offers cutting-edge treatments including cryotherapy, pressotheraphy, oxygen bars, and electro-lymphatic drainage. Offerings now include a seven-day program on healthy aging. Participants begin the week with a multitude of tests to create a biological health profile based on 88 determinants. Throughout the week, they have consultations with various specialists including in anti-aging medicine; they receive acupuncture, hydrotherapy, massage, or other treatments; and they follow personalized macrobiotic nutrition plans and supplement regimens aimed at optimizing cell function and strengthening the immune system.
They won't spread like McDonald's restaurants starting when the Boomers were teenagers, but can we imagine a worldwide chain of health and rejuvenation clinics? Definitely.
Within a few short years, through advancements in artificial intelligence, we believe there will be a transformation from today's somewhat chaotic state of health diagnosis and treatment to an era of “precision medicine.” We're going to see scientific breakthroughs that will enable us to arrive at a far deeper and richer understanding of the interactions among our genes, nutrients, and molecular activity – indeed, our brain-body interactions – so that we'll be able to holistically track thousands of biomarkers. And if the AI is informed by a wide range of potential solution paths – allopathic, naturopathic, homeopathic, ayurvedic, and others (always evolving based on outcomes research) – it could be far more effective at precisely diagnosing what's not working right – even novel coronavirus – and then proposing the ideal constellation of solutions for each individual. This will create an entirely new science and practice of medicine, geared to optimizing physical and mental health, enhancing well-being and happiness, and maybe even forestalling aging.
These breakthroughs may also present us with a serious market-driven ethical issue. If precise and optimal health is available to everyone, that would be grand, but if it's only available to Silicon Valley billionaires, that doesn't seem fair. Access to quality care and the best that medicine has to offer has been and remains tied to wealth and social factors. However, in the years ahead, the disparities could multiply. If we think “income inequality” is a big deal (and we do), just imagine how folks will feel about “longevity inequality.”
Personalized Care and Customer Service
Boomers have also taken charge of how they consume health care services. They expect, and often demand, plenty of information and explanation from their doctors, not just a diagnosis and instructions. They expect doctors to go beyond the physical and ask them about their feelings and concerns, something most doctors are still shy of doing. And those who can afford it are driving the growth of concierge medicine.
With concierge or direct-pay medicine, individuals pay a retainer for more direct and personalized access to physicians and services. Most of the medical costs may still be covered by insurers or Medicare, but patients pay extra for a different kind of relationship with their physicians. Founded in 2000, MDVIP is one of the oldest and largest medical concierge companies in the United States, a network of more than 900 physicians in more than 40 states. A typical MDVIP practice has 600 patients, compared to 2,300 for an average group practice. Patients pay an annual fee from $1,650 to $1,800. Membership benefits usually include no-wait, same-day, or next-day appointments, on-time visitations, and after-hours direct access to one's doctor. Even what can turn out to be minor medical issues may seem big at first, and concierge medicine ensures that treatment happens in the patient's time frame, not the medical establishment's.
Concierge medicine can add value to any traditional medical services model. Concierge Choice Physicians is expanding from the United States into the U.K., which already has universal health coverage. Patients will pay roughly 100 pounds per month to have better access to their physicians.
Individual Responsibility
Boomers' approach to health and health care are rooted in the fact that, rightly or wrongly, they now place more faith in themselves than in the health care system. In our study Health and Retirement: Planning for the Great Unknown, we were surprised to see that Boomers believe their lifestyles – starting with diet, exercise, and activity in general – have far more influence on their health in retirement than having a great doctor (Figure 6.4). They also believe that retirement is enhanced if they can take excellent care of their health, and they're correct. Surveyed retirees who reported being in good health are more likely to be exercising, eating nutritiously, watching their weight, and staying connected socially.12
When asked to compare themselves to their parents, Boomers say they are more than twice as likely to be proactive about their health, to question their doctors' orders, and to view their doctors as partners in managing their health. And, thanks in large part to the internet, they are four times more likely to do their own research on health matters (Figure 6.5). As one retiree summarized for us: “My parents believed that the doctor's word was gospel. You didn't question it. Now you need to be your own health expert and advocate.”
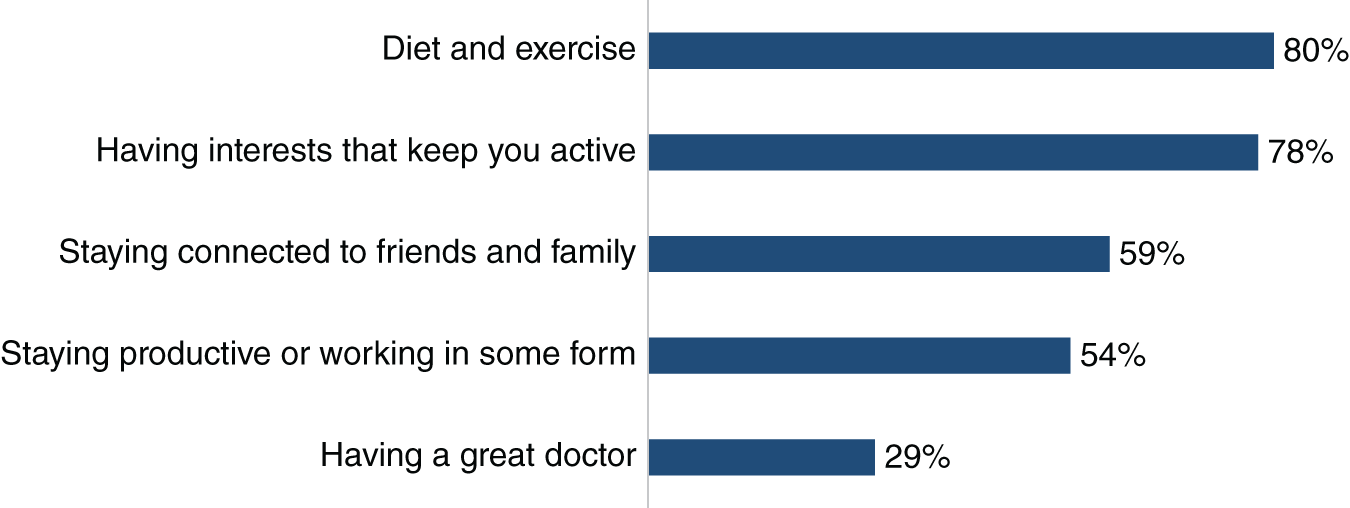
Figure 6.4 Boomers' View on How to Maintain Health in Retirement
Source: Age Wave / Merrill Lynch, Health in Retirement: Planning for the Great Unknown
It turns out that health is a matter of personal attitude as well as individual responsibility. One of the keys to better health is a positive attitude toward oneself and the process of aging. As Dr. Charlotte Yeh, Chief Medical Officer at AARP Services, Inc., told us, “Studies have shown that if you have a positive view of aging, you live seven-and-a-half years longer, and you're 44% more likely to fully recover from a disability. These are correlations, not causal. But those who view aging positively have 55% lower risk of hospitalization and fewer plaques and tangles at autopsy indicative of dementia. One study calculated that the stress of negativity around aging costs the United States $63 billion a year in health care costs.”
Four Boomer Health Styles
Knowing what it takes to promote good health does not, of course, always translate into good practice. While some Boomers are very health conscious, many are not. For example, Boomers have higher rates of obesity than older generations.13 Our survey found four basic health styles among Boomers, based on their condition and approaches to health itself, getting health care, and preparing for health expenses in retirement.14 Providers of health products and services may benefit from engaging these segments differently.

Figure 6.5 Boomers' View of Their Generation versus Their Parents'
Source: Age Wave / Merrill Lynch, Health in Retirement: Planning for the Great Unknown
- Healthy on Purpose Boomers consistently do what's good for their health, both physically and financially. They engage in healthy behaviors, including exercise and eating well, and don't let things interfere with their discipline. They take pride in their health. Half say they are nonetheless concerned about the financial impact of an illness, and they learn what they can about costs and insurance.
- Course Correctors are motivated to take better care of their health, often by the onset of a condition that is not yet a serious impairment. The wake-up call has them paying more attention and learning more. More than half are diligent about their health behaviors, but the majority also say they still let things get in the way of attending to their health. They are very concerned about potential health costs and very interested in technology that can help them manage their health.
- Health Challenged Boomers have conditions, often chronic, that keep them from doing many things they enjoy. They are the most concerned about their health and how to pay for it, yet only two in five are actively attending to their health. A majority say that other responsibilities and worries interfere with taking care of their health. They express greatest concern about health care costs, and the majority say that they are confused by costs and insurance options.
- Lax but Lucky do not take great care of themselves but manage to remain somewhat healthy. They likely have their genes to thank, not their behaviors. Only about a third try to engage in healthy behaviors or to seek out information on improving their health. Like everyone else, they are concerned about the financial impact of health problems, but they are doing little to prepare financially.
Roughly 30% of Boomers fall into each of the first three categories, leaving 10% Lax but Lucky. Women are in the majority in the first three categories, men among the Lax but Lucky.
Helping Boomers Look and Feel Their Best
Today's retirees want to stay healthy, with all the parts in working order. They also want to look good and feel comfortable in their own skin. Unlike their parents who were relatively stoic, most Boomers want their comforts to continue indefinitely. They want to age agelessly, reasonably free of aches and pains and robust enough to live the lifestyles they want. And they'll spend money to try to bring this about. Health-related products and services that have framed a positive attitude toward aging and deliver aspirational messages will reap the marketplace rewards.
The number-one ad campaign of this century is Dove's Campaign for Real Beauty. As Advertising Age introduces it, “Many ad campaigns over the years have sold soap. Fewer have tried to change societal notions about beauty.”15 The worldwide campaign, launched by Unilever working with Ogilvy & Mather in 2004, included advertisements, videos, workshops, events, a book, and a play. The first forays of the campaign were billboards at busy intersections in London and Canada with photos of women of all shapes, colors, and ages and the invitation for motorists to vote on whether they were “fat or fit” or “wrinkled or wonderful.” That turned heads and started conversations. The campaign really took off with the 2006 “Evolution of Beauty” video showing at accelerated speed the complete makeover, photography, and photoshopping of a young woman to turn her into a billboard image. The concluding message: “No wonder our perception of beauty is distorted.” The video went rapidly and globally viral, also generating extensive coverage by the traditional media. The ongoing campaign has continued to thrive on social media.
The campaign had a strong foundation. Dove had always used a variety of “real” women in its ads, and the brand identity included honesty and transparency. The welcome message on dove.com says, “For over a decade, we've been working to make beauty a source of confidence, not anxiety…. Beauty is not defined by shape, size or color – it's feeling like the best version of yourself.”
The campaign's impact has been both commercial and cultural. Sales increased from $2.5 billion to well over $4 billion, and not just in soap and shampoo. Nancy Vonk of Ogilvy explains, “We found out that the women and men exposed to [the campaign] became much more interested in buying anything the brand was selling. That was about, ‘I really appreciate what the brand is doing in the world.’”16
The Dove campaign succeeds in large part because it fits the modern ambitions, purchasing patterns, and attitudes of Boomer women. They are most interested in achieving a healthy, authentic look. And they are experienced and realistic as consumers of personal care and beauty products. They know what they're looking for, and they don't believe most product claims. Today's women over 50 say they feel more beautiful in midlife than they felt when they were in their twenties. They object to use of younger models or phony celebrities in advertising targeting them. And, interestingly, they define beauty in terms of confidence.17
Finances expert Kerry Hannon, author of Never Too Old to Get Rich, reflects, “The Dove campaign gave a message to the rest of us that, you know what, you're attractive just the way you are.” Colin Milner, founder of the International Council on Active Aging, said, “They were looking at the inner spirit of these older women as opposed to the outer look.” And Karyne Jones, CEO of the National Caucus and Center on Black Aging, told us, “Too many marketers are saying to avoid your age. Improving my look is appealing, but trying to make myself look younger isn't. They should all be appealing to people's individuality to make them feel good about who they are.”
Unfortunately, plenty of brands have stuck with the formula of serving up guilt and shame with an ageist spin. Contrast Dove's stance with a Dior campaign, widely and rightly criticized, that used an unblemished 25-year-old model in ads for an anti-aging cream called “Capture Youth.” Much of the criticism flew on Instagram with the hashtag #ThatsNotMe. Like many gerontophobic ads in that product category, it created anxiety by stressing what's wrong with the consumer. And it set an impossible ideal standard of beauty rather than encouraging consumers to be their own version of beautiful. Then there are the ubiquitous – and ageist and sexist – ads for Peloton exercise equipment. Featured exercisers are young and already in perfect condition. As USA Today reported, “Every person portrayed in Peloton ads is in great shape, lives in a lavish home, and chooses to make the Peloton workout bike the centerpiece of said home. Sure, it's a commercial, but it might as well be parody.”18 Older exercisers need not apply.
A wide range of health products and services can engage older consumers by helping them look and feel their best – beauty and personal care, fashion and everyday attire, pharmaceuticals and medical services, food and nutrition, fitness and wellness. Some campaigns use generational anchors sharing their need for care, just like the rest of us. The Novartis “See Me” campaign places Cyndi Lauper amid a variety of everyday people showing how their skin has improved as they manage the chronic condition of psoriasis. Bon Jovi's “Advil Story,” declares that there's no room for pain in his busy schedule as singer, songwriter, philanthropist, and father because “life's a juggling act.”
Coming Breakthroughs in Longevity?
Will we see practical and affordable medical protocols to slow, or even partially reverse, the aging process? Many scientists believe it's a question of when, not if. A big breakthrough may come too late for most Boomers, but some experts predict that a majority of the children born today will live past 100, thanks to advances in chronic disease prevention, precision medicine, and new biotechnologies.
CRISPR (pronounced “crisper”) stands for Clustered Regularly Interspaced Short Palindromic Repeats, which are the hallmark of a bacterial defense system. It forms the basis for a revolution in genome editing that could change every aspect of our lives in the decades ahead. Some experts believe that we're heading toward an era when revolutionary gene-editing methods may be able to correct almost 90% of disease-causing genetic variations, and the global CRISPR market is projected to reach over $7.6 billion by 2026.19 The cost of sequencing an individual's DNA will soon be down to around $100. That will open floodgates of diagnosis, preventive treatment, and customization of wellness plans: the diets, supplements, exercises, and behaviors that work best for individuals.
The field of anti-aging medicine is coalescing and expanding rapidly. The American Academy of Anti-Aging Medicine (A4M), co-founded by physician and sports medicine author Bob Goldman, and physician/researcher/inventor Ronald Klatz, is dedicated to the advancement of tools, technology, and transformations in health care that can detect, treat, and prevent diseases associated with aging. The organization has more than 26,000 members, primarily MDs, and hosts educational events all over the world.
Some promising protocols aim for rapid recovery. For example, platelet-rich plasma therapy (PRP) uses injections of a concentration of a patient's own platelets to accelerate the healing of injured tendons, ligaments, muscles, and joints. A blood sample from the patient is centrifuged to section out the platelet-rich plasma, which is then delivered to the targeted area of the body. Other protocols try to influence the aging process itself. Senolytics is an emerging class of drugs that targets senescent cells, those which in the natural aging process have ceased to divide. Unity Biotechnology, backed by Amazon founder and billionaire Jeff Bezos, is developing therapies intended to selectively eliminate senescent cells to slow age-associated disease and restore tissue to healthier states. Diseases being addressed include osteoarthritis, macular degeneration, COPD, and glaucoma.
Living Longer in Blue Zones
At the opposite end of the technological spectrum are decidedly low-tech ways to increase lifespan. A 2005 National Geographic story by Dan Buettner profiled five “Blue Zones,” geographic regions with three times higher than average rates of living centenarians. The zones were in Greece, Sardinia, Japan, Costa Rica, and California. Researchers talked with centenarians and identified the common key practices which make for a longer and healthier life.
In Blue Zones, people's daily activities keep them moving naturally; they don't make special trips to the gym. They eat in moderation, heavy on various types of beans and greens and light on meat, and they drink alcohol moderately. They are closely connected to family, faith, and friends who reinforce each other's healthy behaviors. And they have a strong sense of purpose, worth up to seven years of life expectancy. In Okinawa, the key word is “Ikigai,” which translates generally as “purpose” and specifically as “why I get up in the morning.”
The value of this approach is being put to the test today. The organization Blue Zones has partnered with 48 cities to improve health metrics and life expectancy for residents. Their ten years of work in Albert Lea, Minnesota, is projected to have collectively increased individual life expectancy by 2.9 years and saved employers $8.6 million in health care cost, in large part by reducing the number of smokers.
The Blue Zones highlight healthy behaviors that we're all familiar with. Regular exercise helps fend off chronic disease, depression, and physical and cognitive impairment. Healthy diet and weight improve heart and bone health, and reduce the risks of stroke, type 2 diabetes, and cancer. Quitting smoking at 65 adds an average of two to four years to life.20 Failure to take medications consistently and correctly correlates with increased hospital and nursing care admissions.21 Lack of social interaction is as bad for health as lack of exercise.22 Even small improvements in health behaviors in later life can contribute to a more active and fulfilling retirement.
Battling and Coping with Chronic Conditions
Many health problems are acute – brief illnesses like the flu or injuries like broken bones that can heal fairly quickly. However, the conditions that tend to arise with age are chronic – arthritis, hypertension, COPD, heart disease, diabetes, cancer, and Alzheimer's. As the term “chronic” implies, there's no complete cure, but rather an ongoing process of trying to manage the underlying causes and mitigate the symptoms. Conditions like Alzheimer's, Parkinson's, and ALS cause steady and often prolonged decline.
Fernando Torres-Gil, PhD, is director of the Center for Policy Research on Aging at the Luskin School of Public Affairs at the University of California, Los Angeles. In 1993, he was appointed by President Clinton as the first Assistant Secretary for Aging in the Department of Health and Human Services. In 2010, President Obama appointed him vice chair on the National Council on Disability. He is a board member of AARP. He is also a Latino Boomer who contracted polio as a child. His personal and professional experience gives him a unique perspective on what Boomers face as their health declines:
I'm really happy to talk about my personal story because I'm thrilled I made it this long. I have a huge advantage over all our Baby Boomer friends who are now discovering a variety of chronic conditions and disabilities, whether it's a stroke, or high blood pressure, or a knee replacement. I've had a lifetime to go through the psychological and emotional transitions to accepting and adapting to my limitations. Now at 71 I'm very happy, even though my polio is going to lead me to be in a motorized scooter or a wheelchair. I've been practicing for this all my life, as I've been aging with a disability.
Our generation is going to go through a major collective crisis as they move into their 70s, 80s, and 90s and are suddenly confronted with the vicissitudes of aging. They're not all going to grow to be 85 and hiking and doing marathons and essentially acting like they're 25. The Baby Boomer cohort is going to have the largest number of individuals who will grow older on their own, either divorced, never married, or estranged from others. We're going to have a real social crisis with a large portion of our generation at risk of isolation and depression, with all the consequences for mental and physical health.
Organizations would be wise to pause and reflect on Torres-Gil's thoughtful concerns and try to imagine products or services that can help assuage either the physical or psychological challenges of what's ahead for so many.
Chronic conditions among older adults are very common (Figure 6.6). Atop the list is hypertension, commonly known as high blood pressure. Nearly six in ten Americans age 65+, over 33 million in total, have hypertension, and it is one of the most common health conditions among older adults globally.23 Hypertension is called a “silent killer” because it usually goes unnoticed unless blood pressure is measured. Two in five Americans with hypertension are not aware they have it,24 even though it can lead to heart failure, stroke, and kidney failure, three common causes of death. The risks can be reduced by diet and exercise, specifically more fruit and vegetables, less salt, fats, and alcohol, and avoiding tobacco.
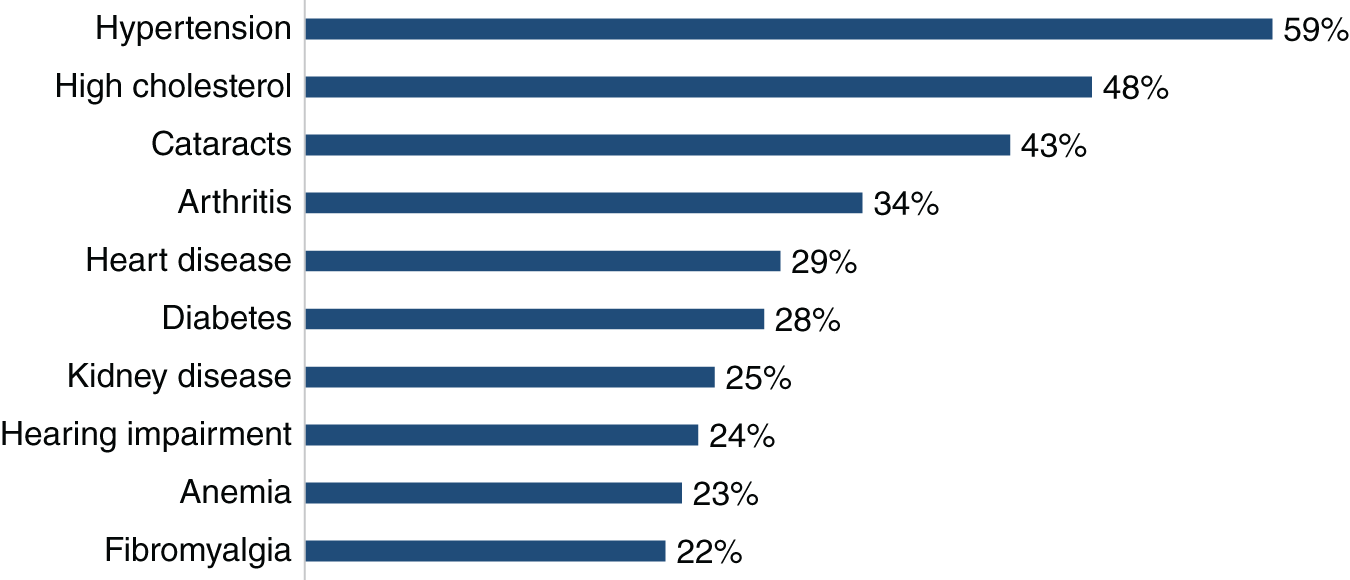
Figure 6.6 Most Common Health Problems Among 65+
Source: National Center for Health Statistics, Health United States, 2017
Those with hypertension should monitor their blood pressure regularly, and sales in the United States of smart devices for doing so are projected to grow from $85 million in 2018 to $122 million in 2022.25 Omron Health released the first monitor built into a wristwatch. HeartGuide uses an inflatable cuff in the watchband to take an actual blood pressure reading (where other wearables provide only an estimate). HeartGuide's smartwatch functionality tracks activity levels (steps, aerobic steps, distance covered, and calories burned), monitors sleep (bed time, sleep time, and deep versus light sleep), and communicates (email and call and text notifications). The companion app tracks health data and provides customized coaching. Users have a more continuous and comprehensive picture of their heart health.
You can look at Figure 6.6 and do the math. If 59% of those 65+ have hypertension, and more than one in three has high cholesterol, cataracts, or arthritis, then a lot of older Americans must have multiple chronic conditions. In fact, 81% have two or more (Figure 6.7). That's unpleasant news if you are a sufferer, but for the nutraceutical, vitamin, pharmaceutical, diagnostics, and biotech sectors, it presents a world of opportunity.

Figure 6.7 People with Multiple Chronic Conditions by Age
Source: Rand Corporation, Multiple Chronic Conditions in the United States, 2017
Maintaining Brain Health for Life
Retirees' greatest fear regarding living a long life is losing physical and cognitive abilities.26 Presented with a forced choice, 75% say that functioning well mentally in retirement is more important than functioning well physically.27 And Alzheimer's has become the most feared condition of old age. Cancer, stroke, and heart disease are frightening for sure, but more Boomers now fear Alzheimer's than all the other major diseases combined (Figure 6.8). What they really fear are the specific repercussions of the disease – losing independence, losing personal dignity, and most of all losing their minds and becoming a burden on their families.
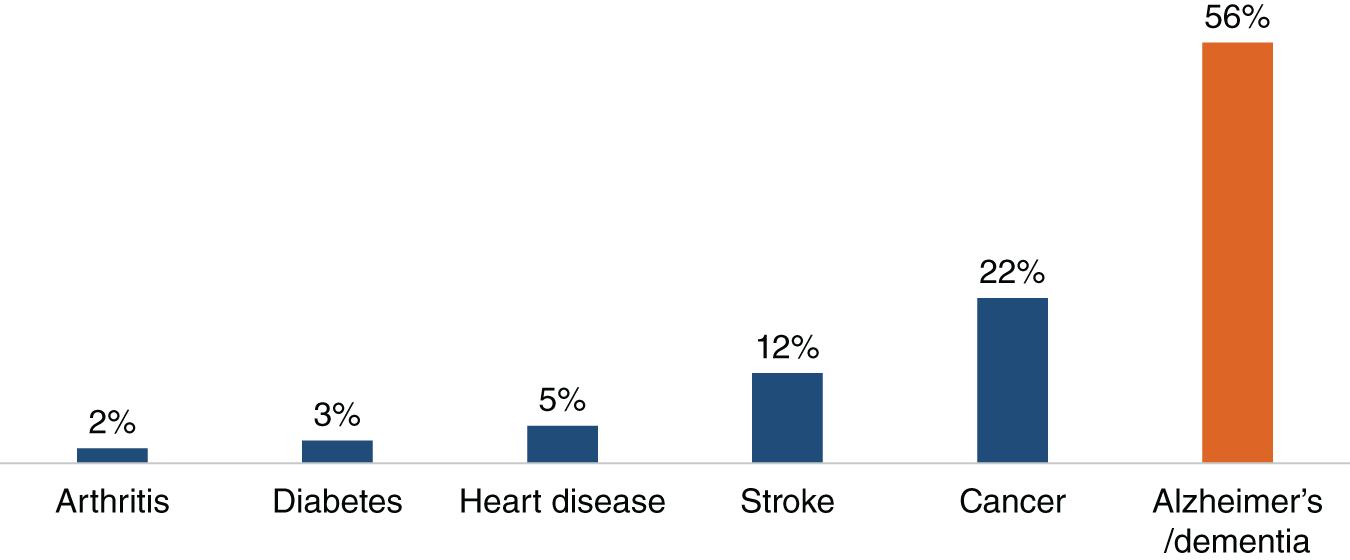
Figure 6.8 The Scariest Disabling Condition of Later Life
Source: Age Wave / Merrill Lynch, Finances in Retirement: New Challenges, New Solutions
The World Health Organization estimates that 50 million people worldwide are living with dementia, and due to the age wave, that's projected to increase to 82 million in 2030 and 152 million in 2050. Over 10% of Americans over age 65 are living with Alzheimer's. The percentage of people with Alzheimer's increases with age: 3% of people age 65–74, 17% of people age 75–84, and one-third of people age 85 and older. Since so many people will be living well into their 80s, Alzheimer's will become a challenge that most families – and nations – will face. Women are far more likely to develop Alzheimer's at some point – a one-in-five chance (21%) for a 65-year-old woman, but closer to a one-in-ten (12%) chance for a 65-year-old man – partly due to their longer lives. The projected number of people with Alzheimer's in the United States is expected to grow from 5.8 million in 2020 to 15 million in 2050.28 Unless there's a true breakthrough, and we are surely hoping there will be, it could become the mental, physical, social, and economic sinkhole of the twenty-first century.
Dale Bredesen, MD, author of The End of Alzheimer's, is an optimistic voice in the fight against Alzheimer's while acknowledging the complexity of the challenge. He explained to us that a person with Alzheimer's and other related dementias may have 10 to 25 different factors contributing to their condition, and those all need to be understood at the individual level to come up with an effective treatment: “It's not going to be a one-pill, silver bullet solution that ends Alzheimer's. It's got to be a much more comprehensive approach.” He is hopeful and believes that with continued scientific and clinical progress worldwide, rates of Alzheimer's and other dementias will start to decline within the lifetime of the Boomer generation.
Bredesen currently serves as Chief Science Officer at AHNP Precision Health. The firm trains practitioners in the ReCODE protocol. After a series of lab and genetic tests on the individual, practitioners customize a program including dietary guidelines, sleep goals, stress reduction techniques, cognitive training, hormone therapy, and other actions that work together to fend off cognitive decline. To date, more than 100 patients have seen documented improvements in cognitive functioning based on Bredesen's ReCODE Protocol.
Others are also taking multidimensional approaches. Based on the work of psychiatrist and self-help guru Dr. Daniel Amen, Amen Clinics opened their doors in 1991, and are now popping up all over the country. They look at the biological, psychological, social, and spiritual aspects of their patients' lives in order to come up with a comprehensive approach to lifelong mental wellness. One of their signature tests is a SPECT (single-photon emission computed tomography) to analyze blood flow inside one's brain. They work with a multitude of mental conditions including Alzheimer's, ADD, bipolar disorder, depression, and PTSD. Their website claims that 85% of their patients report improvements from their treatments and prescribed supplements.
Lisa Genova, PhD, a Harvard-trained neuroscientist, speaker, author, and yogi, broke away from her scientific background and wrote the bestselling novel Still Alice, which has now been published in 37 languages. It also won Julianne Moore an Academy Award for her portrayal of Alice in the popular movie. Genova told us, “I think people have become very comfortable with the idea that they can influence their health and their future health from the neck down. So people wear Fitbits, they know their blood pressure, they know their cholesterol level, and they are managing those numbers by what they eat and how they conduct their lifestyle. But most have the sense that there's nothing they can do about their health from the neck up. And in truth, there's a lot we can do.”
When we asked for some examples, she shared, “We know that exercise does so many important, healthy things for everyday brain function and memory and has been shown to reduce the risk of dementia by as much as fifty percent. In addition, getting enough sleep, reducing stress, and supporting a healthy heart are all going to help fight off the accumulation of amyloid that could lead to Alzheimer's. All of these also help keep the brain running really well. But it's more than that,” she added. “Having a sense of belonging, staying cognitively active, and learning new things also help your brain develop new neural pathways. It's a way of taking advantage of neuroplasticity. Every time you learn something new, you're actually building a bigger, more elaborately connected, Alzheimer's-resistant, healthier brain.”
One of the other common mental difficulties among older Americans is depression, which is often linked to social isolation and loneliness. Social isolation also raises the risks of hypertension, heart disease, obesity, weakened immune system, and cognitive decline. Conversely, people who engage in activities with others tend to feel better, have greater sense of purpose, and live longer. Steve Cole, director of the Social Genomics Core Laboratory at the University of California, Los Angeles, said, “Loneliness acts as a fertilizer for other diseases. The biology of loneliness can accelerate the buildup of plaque in arteries, help cancer cells grow and spread, and promote inflammation in the brain leading to Alzheimer's disease. Loneliness promotes several different types of wear and tear on the body.”29
Living with Everyday Health Problems
Some of the most common health problems of older people cause everyday discomfort or impairment. While remedies exist today, we expect that market forces will bring many more on the way, some effective and others snake oil. We're concerned that for most consumers, since so much of what's coming will emerge on the outskirts of traditional medicine and nutrition, it will be hard to know the difference.
Pain
One in three Americans over 55 has a diagnosed pain condition, commonly associated with arthritis. The majority of Americans rely only on over-the-counter medications to treat it, about 20% on prescription drugs.30 The fast-emerging trend in self-managed pain treatment is CBD (cannabidiol), which is said to have anti-inflammatory and pain-relieving effects. CBD was legalized across the United States in 2018. The global CBD market, roughly half of which represents medical uses, was estimated at $4.6 billion in 2018 and is expected to grow to $23.6 billion in 2025.31
We're finally aware that far too many people have been prescribed opioids for their pain, and many have become tragically addicted or died. Increased awareness of the opioid epidemic is driving a decline in prescription pain medication use. Among Americans with reported pain, 21% used a prescription in 2017 compared to 35% in 2013.
Sleep
Regular and adequate deep, restful sleep is vital to physical and mental health, and lack of sleep is associated with a variety of chronic medical conditions including hypertension and diabetes.32 In Sleep Revolution, Arianna Huffington writes: “Scientists are resoundingly confirming what our ancestors knew instinctively: that our sleep is not empty time. Sleep is a time of intense neurological activity…. Getting the right amount of sleep enhances the quality of every minute we spend with our eyes open.” However, nearly half of Americans 65–80 report that they regularly have trouble falling asleep. And an estimated 22 million Americans suffer from sleep apnea. Its prevalence increases with age, and an estimated 80% of cases are undiagnosed.33
More older Americans means more sleepless Americans. The market for OTC sleep remedies nearly doubled between 2011 ($217 million) and 2015 ($420 million).34 Global sales of sleep aids and technology, including smart beds and pillows, are expected to grow from $60 billion in 2018 to $95 billion in 2025.35
Hearing Impairment
Nearly 25% of those aged 65 to 74, and 50% of those 75 and older, have disabling hearing loss. Although many could benefit from hearing aids, fewer than one in three (30%) has ever used them, as they feel they'll be stigmatized as old.36 However, hearing aids have come a long way from the big clunkers that debuted in 1956. Thanks to advances in miniaturization, some of today's options are virtually undetectable because they're positioned largely or completely in the ear canal or hidden away right behind the ear. And they'll soon do more than assist hearing. Valencell, with a wearable biometric sensor technology, and Sonion, with a new micro-acoustics and micro-mechanics technology, are partnering on a biometric sensor hearing aid. In addition to improving hearing, it will measure heart rate, electrocardiogram RR interval, activity levels, and energy expenditure – and provide a platform for future innovations in health monitoring. All that sounds promising, but Medicare doesn't cover hearing aids, and Supplement plans are unlikely to cover the most advanced and expensive kind.
Falls
Slipping and falling is not, of course, a medical condition. But it's a major cause of serious injury among older people, as well as a cause of general decline when the aftereffect is decreased mobility. Three million older Americans are treated in emergency departments for fall injuries each year,37 and falls are contributing to the steady rise in hip and knee replacement surgeries around the world.38
A 2018 Centers for Disease Control study estimated the medical cost of falls at $50 billion annually, including $38 billion paid by Medicare and Medicaid. Yet basic interventions – home modifications like handrails in the shower, better medications management, or doing Tai Chi exercises – could prevent falls and avert medical costs.39 The U.S. market for “ambient assisted living technology,” primarily fall detection and emergency alert systems, is expected to grow from about $450 million in 2017 to nearly $2 billion by 2022.40
Age-Related Tech Is Ramping Up
The migration of health care processes into the home, and onto or even into the body, has unleashed a torrent of technological innovation. We're just at the beginning of this revolution, but here is a sampler of relatively new tech solutions. 23andme can test DNA for health predispositions, ancestry, carrier status, and other DNA traits for $199. Habit, a California start-up, is creating custom nutrition plans based on an individual's genetic makeup. Pillo is a home health robot for medication management. It can use facial recognition technology to interact with and dispense the correct pills for different individuals at the appropriate times, as well as order refills and connect with health care professionals. Mixfit is an app and a drink dispenser, producing a drink that is personalized to a user's nutritional and vitamin needs. Triple W has a wearable to help people with incontinence by using ultrasound to notify them when the bladder is getting full.
The Apple 4 Watch can detect irregular heartbeats and falls. ReSound controls hearing aid settings via an iPhone or Apple Watch. Xandar Kardian offers a contact-free (via radar technology) monitoring device that can keep track of a user's vital signs, detect a fall, and measure for sleep apnea. WiseWear jewelry does much the same, plus GPS location, with a fashionable bracelet connected to a smartphone. Care Predict Home is a wearable that uses kinematics to quantify daily activities, including eating, walking, drinking, toileting, and bathing, as well as predicting health issues. Healium tracks a user's brain patterns and heart rate, and then transfers the patterns into a visual mindfulness and stress-reduction app that is compatible with Oculus Go, Gear VR, and Google Daydream headsets.
Finally, general-purpose voice assistants, starting with Amazon Echo and Google Home, can perform or assist with tasks and issue reminders. Reminder Rosie gives reminders in the recorded voice of a family member, friend, or caregiver.
In one of our studies, we asked people of all ages how interested they were in new health technologies. Their responses (Figure 6.9) reveal high interest in everything from anti-aging therapies to replacement organs to home care robots. We expect that these will all be lively markets in the near future.
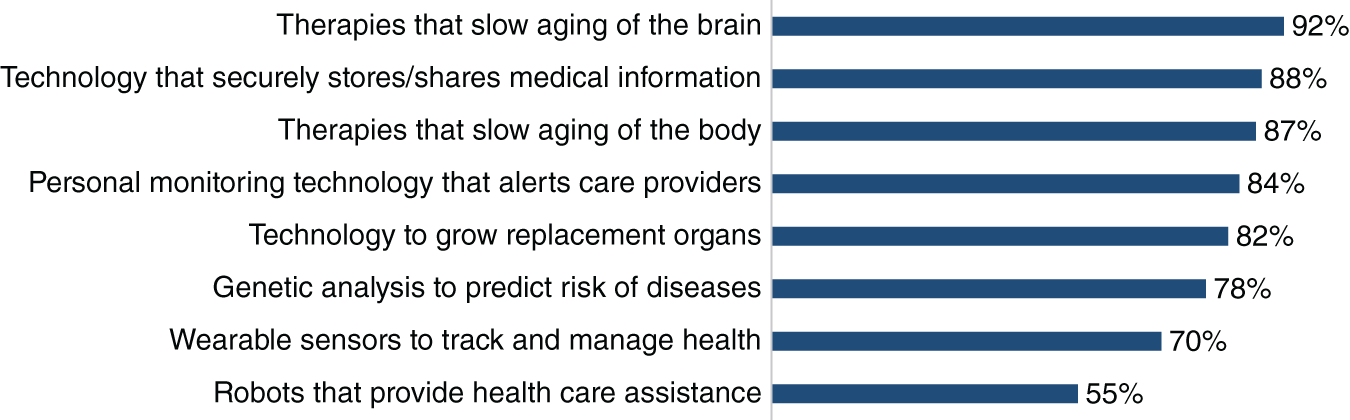
Figure 6.9 Interest in New Health Technology
Source: Age Wave / Merrill Lynch, Health in Retirement: Planning for the Great Unknown
Waze to Help People Out of the Maze?
The U.S. health care system is a maze. Worse, it's a 3D maze. A maze that is costly in terms of expense, time, efficiency, patient outcomes, and public health. It is in no way user-friendly.
One dimension is the provisioning and receiving of care. Physicians and facilities are specialized and clinic and remote care options are multiplying. This fragmentation of services is hardest on older patients because they need more care, they have more combinations of conditions, and they are more likely to be receiving care from multiple organizations.
The second dimension is paying for services. Given the cost of health care, maximizing insurance coverage and minimizing out-of-pocket expenses are necessities. Yet insurance options and processes are complicated, to put it mildly. Retirees may be dealing with three parts of Medicare, widely variable supplemental plans, and a lucky few with employer-sponsored retiree health plans. Only a small fraction of today's retirees (19%) say they feel knowledgeable about Medicare and its options. That's unconscionable.
Even the small stuff can cause confusion. Ken recently received a note from Medicare about his coverage. In the upper left of the document, in large letters, it proclaimed, “This Is Your Medicare Premium Bill.” However, in the upper right, also in large letters, it proclaimed, “This Is Not a Bill.” Hello? Is anybody there?
A third dimension is the often-overlooked challenge of accessing – and making sense of – supportive and social services at the local, state, and national levels. Agencies are separate organizations with often overlapping missions and little by way of coordination. Housing doesn't talk to home care. Fernando Torres-Gil told us, “As a 71-year-old with a disability, there are at least 20 different offices for 20 programs I could potentially qualify for. I'm smart enough to work most of them as needed, but for a 71-year-old without that kind of education, support, or advocacy, it becomes impossible.”
The Waze app helps people navigate to where they want to go – by car, on a bike, or on foot. It negotiates traffic, avoids roadblocks, and helps us reach destinations in the shortest time over a minimally complicated route. Perhaps it's time for a retiree “Health Waze.” On the care dimension, it could assess one's condition quickly, determine and recommend the right provider or service, identify the best nutrition and exercise protocols for every individual, and thereby help people stay healthier and get better sooner. Such a technology could help avoid roadblocks like competing diagnoses or prescriptions as well as confusion regarding all of the lifestyle modification possibilities. On the insurance and payment dimension, it could submit complete and correct claims quickly, thereby causing faster payment processing while minimizing out-of-pocket expense.
Although we're still a far cry from Health Waze, we do see and applaud steps toward easier navigation. Major hospitals and health systems have website portals to patients' health information, appointments and physician communications, billing, and other resources. Insurance companies have increasingly clever mobile apps. Aetna helps customers find services and manage benefits, and it integrates with the health and activity monitoring functions of an Apple Watch. UnitedHealthcare's app offers video chat with a doctor 24/7. These services are local to the institution, and they tend to be task-based, not objective-based. The user still puts the pieces together and does most of the navigating.
AI will probably need to advance for a few more years before there's a smart and user-friendly app to rule them all. But there are opportunities everywhere for providers, insurers, and agencies to deliver more of what retirees want – and sometimes desperately need – by way of navigating the system. And there may be opportunities for organizations to band together on technological capabilities without running afoul of patient data privacy regulations.
Once again, Fernando Torres-Gil helps us look at the big picture:
America has evolved a health system based on a categorical approach as opposed to a universal approach, a system with many categories of providers, insurers, and patients. Most other nations have created or are creating public policy approaches to their aging populations based first on a set of universal principles. These may be simply saying that everyone has the right to health care, everyone has the right to long-term care, everyone has the right to grow old without having to be on the street. From those principles, they move forward and create systems of services and benefits that are more universal – and can have one access point.
We agree 100%, and we're hoping that folks in the government sector will bring in a few skilled marketers and communicators to help them make Medicare and other services far more understandable and user-friendly. The long-term solution may be to simplify and better integrate the system, but for now retirees need a lot of help just navigating it.
A Looming Geriatric Medical Crisis
Two-thirds of Americans age 50+ believe that today's health care system isn't ready for an aging population.41 They're correct.
Even as the demand for geriatric medicine is growing rapidly with an aging population, geriatrics remains a relatively obscure medical specialty. By way of contrast, trained pediatricians outnumber trained geriatricians by more than ten to one. There is one active pediatrician providing patient care for every 1,393 children age 18 and under, but just one geriatrician for every 10,732 adults age 65 and over.42 The American Geriatrics Society projects that we will need more than 33,000 geriatricians by 2025. As of 2018, there were only 7,300 board-certified geriatricians. It's highly doubtful that supply will catch up to demand, since only 66 of the 5,349 medical school graduates in 2018 went into a geriatrics program.43 The reason is largely economic. In an era of highly specialized medicine, the disciplines that attend to people's health across the lifespan – pediatrics, family medicine, and geriatrics – are the least compensated (Figure 6.10). Plastic surgeons and orthopedic specialists earn about 2.5 times what geriatricians do. The incentives have got to change – this is an institutional failure. Many people today are speaking out about how our economy is “rigged.” We believe that our health care system is “rigged” to favor the rich, the young, and the connected.
Compounding the problems of health care delivery at large is the retirement wave of Boomer physicians. As of 2016, 52% of the one million professionally active physicians in the United States were over the age of 50, and 29% were in their 60s or older. More than one-third of currently active physicians will be 65 or older within the next decade, and 17% plan to retire within the next three years. That would remove approximately 136,000 physicians from the workforce during a period when about 85,000 physicians will complete residency and enter it. Overall, the supply of U.S. physicians is expected to grow by about 8% over the next 15 years, while the 65+ population is projected to grow by 53%.44
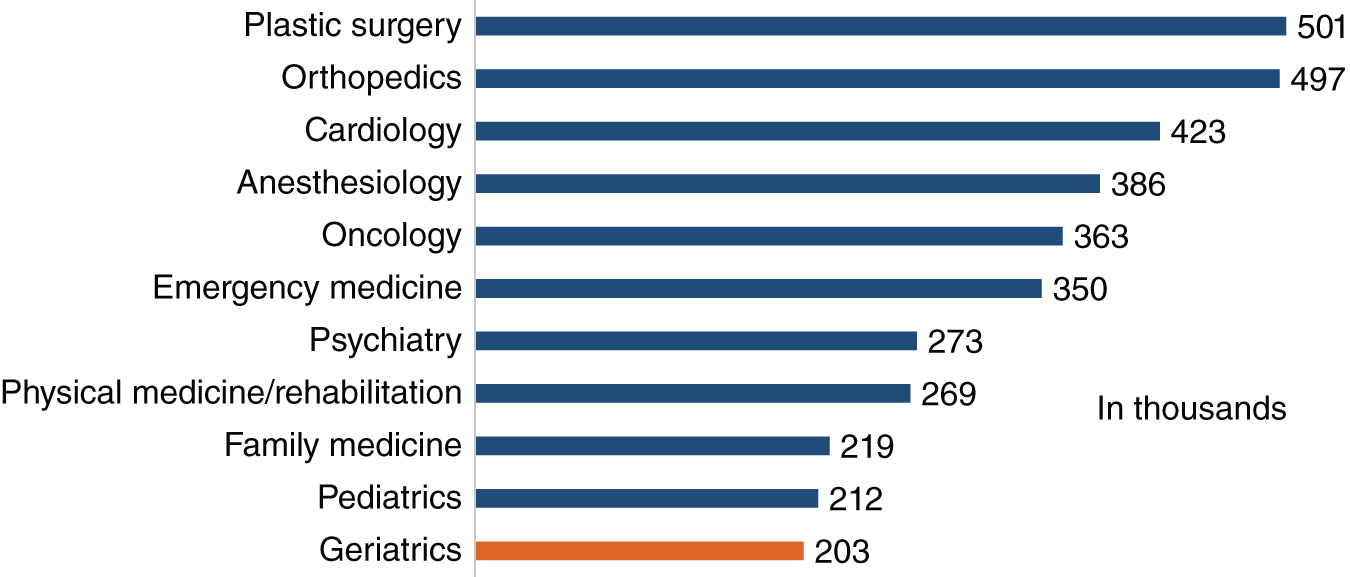
Figure 6.10 Annual Physician Compensation by Specialty
Source: Medscape, Physician Compensation Report, 2018; Medpage Today, 2018 Geriatrics Salary Survey
What will compensate for a severe shortage of physicians, especially geriatricians? Some medical schools are piloting tuition-free programs, funded by donations and grants, to attract students into lower-paying specialties. Kaiser Permanente opens its own medical school this year and is waiving tuition for the first five classes of students (but has no apparent focus on geriatrics). Those are laudable efforts but small steps. Against the backdrop of the demographic increase in older Americans, overall demand is not going to shrink, even if we see breakthroughs in the treatment of chronic conditions or in anti-aging medicine. Instead, the gap will need to be filled by more and better information, technology, and self-care.
Taking charge of one's health may not be just a generational trait of Boomers, but everyone's imperative. We believe we're in the first inning of a revolution in science, health, medicine, and self-care that could possibly transform the future of retirement more than any other factor.
Notes
- 1. Eric Niiler, “An AI Epidemiologist Sent The First Warnings of the Wuhan Virus,” Wired, January 25, 2020.
- 2. Angela Chen, “As tech companies move into health care, here's what to watch in 2019,” The Verge, January 3, 2019.
- 3. World Population Review, Heathiest Countries 2020.
- 4. Axios, “Poll: How many people want to live to 100,” May 9, 2019.
- 5. World Health Organization, World Health Statistics 2018.
- 6. Age Wave / Merrill Lynch, Health in Retirement: Planning for the Great Unknown, 2014.
- 7. Gallup, “Trends Show Bathing and Exercise Up, TV Watching Down,” 2000.
- 8. International Health, Racquet & Sportsclub Association, 2019 IHRSA Health Club Consumer Report.
- 9. U.S. Bureau of Labor Statistics, Consumer Expenditure Survey, 2017.
- 10. The Harris Poll, ASCO 2018 Cancer Opinions Survey, 2018.
- 11. Grand View Research, Complementary and Alternative Medicine Market Size, Share & Trends Analysis Report by Intervention, 2018.
- 12. Age Wave / Merrill Lynch, Health in Retirement.
- 13. Population Reference Bureau, “Are Baby Boomers Healthy Enough to Keep Working?” 2018.
- 14. Age Wave / Merrill Lynch, Health in Retirement.
- 15. “Top 15 Ad Campaigns of the 21st Century,” Advertising Age, 2015.
- 16. Ibid.
- 17. “Baby Boomer Beauty: Marketing to Female Boomers,” Medium Infographic, April 4, 2017.
- 18. Andrew Joseph, “A hilarious Twitter thread roasted peloton's absurd commercials,” USA Today, January 29, 2019.
- 19. Coherent Market Insights, CRISPR & CAS Gene Market Size Research Report 2026.
- 20. Donald H. Taylor et al., “Benefits of Smoking Cessation for Longevity,” American Journal of Public Health, 2002.
- 21. K. L. Pellegrin et al., “Potentially preventable medication-related hospitalizations,” Journal of the American Pharmacists Association, 2017.
- 22. National Institute on Aging, “Social isolation, loneliness in older people pose health risks,” April 23, 2019.
- 23. National Center for Health Statistics, Health United States, 2017; World Health Organization, “Hypertension Fact Sheet,” 2019.
- 24. National Health and Nutrition Examination Survey (NHANES) 2003–2010.
- 25. Statista, eHealth Report U.S., 2018.
- 26. Age Wave / Merrill Lynch, Finances in Retirement: New Challenges, New Solutions, 2017.
- 27. Age Wave / Merrill Lynch, Health in Retirement.
- 28. Alzheimer's Association, 2019 Alzheimer's Disease Facts and Figures.
- 29. National Institute on Aging, “Social isolation, loneliness in older people pose health risks,” April 23, 2019.
- 30. Kantar Health, The Global Health and Wellness Report 2018.
- 31. Grand View Research, Cannabidiol Market Size, Share & Trends Analysis Report 2019–2025.
- 32. Harvard Medical School Division of Sleep Medicine, “Healthy Sleep: Sleep and Disease Risk,” 2007.
- 33. American Sleep Apnea Association, “Sleep Apnea Information for Clinicians.”
- 34. Statista, “Sleeping aid OTC revenue in the United States from 2011 to 2018.”
- 35. Brand Essence Research, “Sleep Aids Market: Global Size, Trends, Competitive, Historical and Forecast Analysis, 2019–2025,” 2019.
- 36. National Institute on Deafness and Other Communication Disorders.
- 37. C. S. Florence et al., “Medical Costs of Fatal and Nonfatal Falls in Older Adults,” Journal of the American Geriatrics Society, 2018.
- 38. OECD, Health at a Glance 2017.
- 39. Judy A. Stevens and Robin Lee, “The Potential to Reduce Falls and Avert Costs by Clinically Managing Fall Risk,” American Journal of Preventative Medicine, 2018.
- 40. Statista, eHealth Report U.S., 2018.
- 41. Age Wave / Merrill Lynch, Health in Retirement.
- 42. U.S. Census Bureau, American FactFinder, 2018.
- 43. National Resident Matching Program, Results and Data: Specialties Matching Service 2018 Appointment Year.
- 44. Association of American Medical Colleges, The Complexities of Physician Supply and Demand: Projections from 2015 to 2030, 2017; Physician's Foundation, 2018 Survey of America's Physicians.