Adhesives for Medical and Dental Applications
This chapter focuses on adhesives used in direct physiological contact in dental and medical procedures. Activity in both areas has been quite extensive outside the United States for decades. In contrast, adhesive use in medical devices, patches, and plasters has been ongoing in the United States for a long time. In the case of medical devices, adhesion is concerned with the joining of materials such as plastics, elastomers, textiles, metals, and ceramics, which are examined in other chapters of the present volume. The coverage of this chapter is devoted to applications where to adhesives are in direct contact with tissues and other live organs.
Keywords
Adhesives; monomers; cyanoacrylates
This chapter focuses on adhesives used in direct physiological contact in dental and medical procedures. Activity in both areas has been quite extensive outside the United States for decades. In contrast, adhesive use in medical devices, patches, and plasters has been ongoing in the United States for a long time. In the case of medical devices, adhesion is concerned with the joining of materials such as plastics, elastomers, textiles, metals, and ceramics, which are examined in other chapters of the present volume and are covered in various references [1–7], The coverage of this chapter is devoted to applications where adhesives are in direct contact with tissues and other live organs.
10.1 Introduction
The use of adhesives in medicine and dentistry is often critical and functional and with little visibility to patients. Infant immunization, flu shots, restorative dental fillings, blood transfusions, heart bypass surgery, urological surgery, anesthetic administration, intravenous drug delivery, and numerous other medical procedures would not be possible today if not for advanced adhesives. Modern adhesives are used to assemble thousands of medical devices around the world, or they are used in direct physiological interactive modes [8].
There are different types of commercially available tissue adhesives, classified into three categories: natural or biological, synthetic and semisynthetic, and biomimetic. The biological tissue adhesives such as fibrin glues and collagen are quite effective in select applications. Their drawbacks are high cost and limited availability. The action of biomimetic adhesives is based on adhesion of algae to a wet surface and the Gecko’s ability “to stick” its paws on to surfaces [9].
10.2 Natural Adhesives
Surgical adhesives and sealants based on natural polymers, cross-linked via biochemical reactions, offer in general a more biocompatible alternative to synthetic glues. The main biological adhesives are based on fibrin and collagen. Gelatin and polysaccharide-based adhesives are newer adhesive classes which have attracted attention and research. Fibrin sealants are made from a number of components produced from pooled human plasma that enable the adhesive to mimic the final stages of blood clotting. The most basic fibrin sealants consist of combinations of thrombin and fibrinogen. Collagen-based adhesives adsorb blood and coagulation products on to their fibers, trapping them in the interstices and adhering well to the wound. This biopolymer also induces platelet adhesion and aggregation, and activates coagulation factors [10].
10.3 Synthetic and Semisynthetic Adhesives
Semisynthetic and synthetic surgical adhesives include gelatine–resorcinol–formaldehyde (GRF), urethane prepolymers, and cyanoacrylates. These adhesives have some shortcomings such as low bioabsortion and metabolic rates, cytotoxicity (low biocompatibility), low adherence to wet surfaces, and chronic inflammation induced by the release of formaldehyde from GRF and cyanoacrylate polymers and aromatic diamine from aromatic polyurethanes [11].
10.4 Cyanoacrylic Adhesives
These so-called wonder adhesives are marginally thermosetting materials and were first introduced commercially by Eastman Chemicals. They form strong thermosetting bonds between many materials without heat or an added catalyst. They are particularly useful in bonding metal to nonmetal. Lap-shear strengths of 13.7 MPa have been reported. However, the resistance capability of these adhesives to moisture is still somewhat low [12]. These materials set very quickly when squeezed out to thin film between many types of adherends.
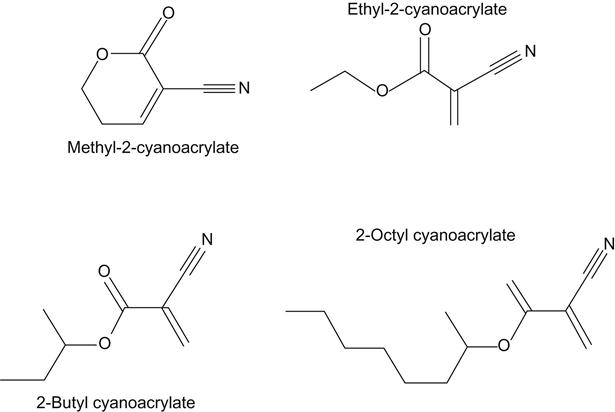
A cyanoacrylate adhesive is a relatively rapid curing adhesive also from the acrylic family tree, but has a completely different cure system. Cyanoacrylate monomer (Figure 10.1) is made using a complex chemical process. The monomer produces a very reactive polymerization. The reaction or polymerization process is stabilized and the monomer is kept in the liquid state by the addition of a small amount of an acid stabilizer material [13].
When a drop of cyanoacrylate adhesive is put on the surface of a part, the acid stabilizer molecules react with the water molecules present on the surface of the part from the relative humidity in the air. The reaction of the water and acid causes the acid stabilizer to be neutralized. The cyanoacrylate molecules then react with each other and form polymer chains without cross-linking [13].
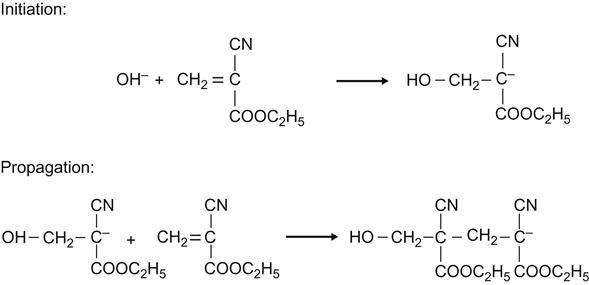
Cyanoacrylate adhesives undergo anionic polymerization in the presence of a weak base, such as water, and are stabilized through the addition of a weak acid. The stabilizer is usually in the form of a weak acidic gas such as SO2, NO, or BF3. An essential function of the stabilizer is to prevent polymerization in the container, which is usually made of polyethylene. When the adhesive contacts a slightly alkaline surface, trace amounts of adsorbed water or hydroxide ions (OH−) that are present on the substrate’s surface neutralize the acidic stabilizer in the adhesive, resulting in rapid polymerization as shown in Figure 10.2.
The amount of stabilizer molecules in cyanoacrylate is very small—measured in parts per million—and very little moisture molecules are required to cause rapid polymerization. Cyanoacrylates begin to form polymer chains immediately on contact with the water vapor on the surface of the part. If parts are moved during initial contact, the polymerization process and polymer chains are stopped. The process must start again at a new site of catalysis [13].
Cyanoacrylates are very rapid in curing and provide high bond strengths on plastic and rubber materials. These adhesives are versatile, which renders them highly useful in all industries. Some of the larger application areas are in electronics for printed circuit board wires and components, and in medical technology for disposable plastic medical devices. Other applications include toys, small and large appliances, automotives, and cosmetics packaging. Applications exist in all industries for repair of all rubber and plastic parts as well as some metal parts. The consumer market is a large volume user of cyanoacrylate adhesives for repairing everything in the home from wallpaper tears to broken toys to torn and false fingernails.
Cyanoacrylate adhesive can be made from different acrylate monomers, such as methyl, ethyl, butyl, and isopropyl. These molecules differ in size and adhesives made from them exhibit different physical properties. Methyl is the smallest molecule and seems to work best on metal and rubber parts, whereas ethyl works best on plastic parts. Many modifications can be made to the monomers to alter or improve their properties as adhesives. They can be toughened with rubber or formulated to have low odor, resistance to thermal cycling, or less sensitivity to surface conditions, which tend to stabilize the adhesive and slow down the cure [13].
As with other acrylics, the monomers are liquids of low viscosity that polymerize very easily in the presence of a slightly basic surface containing adsorbed water. Polymerization is ionic. The resulting polymers have different properties, depending on the alkyl group. The methyl ester (methyl-2-cyanoacrylate) is the most commonly used compound. This material is formulated with a thickener (to prevent starved joints from being formed) and a plasticizer to make it more resistant to shock loading. The thickener can be a polymer of the same monomer. An essential feature is a stabilizer to prevent polymerization in the adhesive container, which is usually made of polyethylene [15].
The polymerization of cyanoacrylates is inhibited by low pH (high acidity), and thus it does not proceed satisfactorily on acid surfaces such as wood. The suggested incorporation of poly-N-vinyl pyridine or polyethyleneamine, or even simple amines, presumably serves the dual purpose of thickening the liquid and increasing the pH.
Adhesives based on higher homologs than the methyl form have been in use for a number of years. These include the ethyl, propyl, and butyl esters of cyanoacrylic acid. Moisture resistance of the methyl-2-cyanoacrylate is only fair. Ethyl cyanoacrylate has been shown to form stronger bonds than the methyl form between several different types of plastic surfaces. The higher homologs, however, generally do not form bonds as strongly as the methyl form. The most important step in the successful application of a cyanoacrylate adhesive is the application of a thin adhesive film between two well-mated surfaces. The thinner the film is, the faster the rate of bond formation, and the higher the bond strength. Bond strength is dependent on proper surface preparation.
In general, aging properties of the cyanoacrylates are good. Rubber-to-rubber and rubber-to-metal bonds typically have endured outdoor weathering for over 7 years. These bonds have also passed stringent water-immersion and salt-spray tests. Plastic-to-plastic and plastic-to-rubber bonds have aged satisfactorily for 3–5 years. Metal-to-metal bonds generally age rather poorly, except under special conditions where the minimal glue line is exposed to moisture. Solvent resistance is also generally satisfactory. Dilute alkaline solutions weaken the bond considerably, while dilute acid solutions weaken it to a lesser degree. Impact resistance is generally poor because of the thin, inflexible bond.
This is especially true with two rigid substrates, such as metals. The methyl cyanoacrylate bond melts at approximately 165°C. Prolonged exposure to temperatures in this range results in a gradual but permanent breakdown of the bond. Generally, the upper temperature limit for continuous exposure is about 77°C. At low temperatures, bonds remain intact at least down to –54°C. Grades of cyanoacrylates with specialized improved properties are available. For example, one grade has improved heat resistance to 246°C, high viscosity, and very fast setting ability [16].
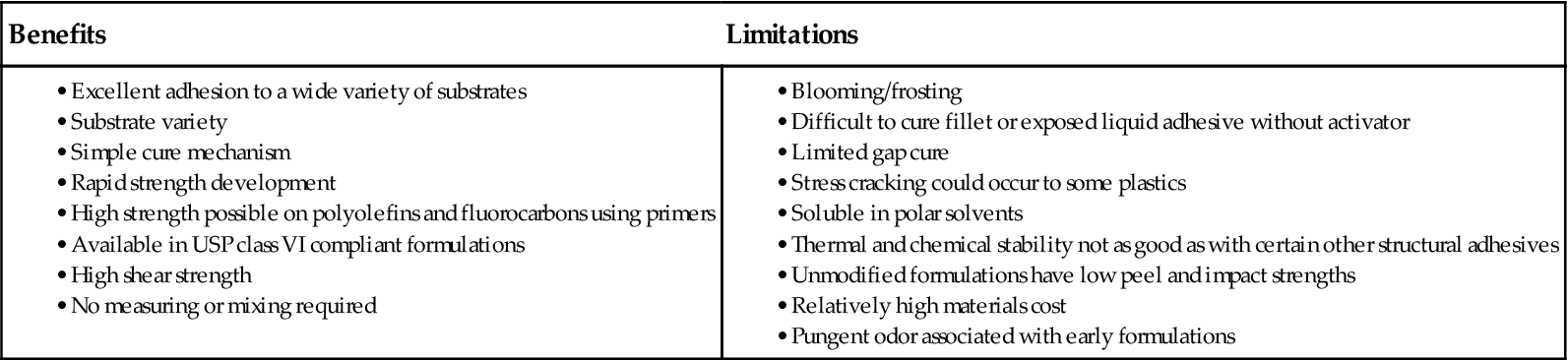
Among the advantages of the cyanoacrylates are the following (see also Table 10.1):
• High bond strength with thin glue line
• No added catalyst or mixing needed
• No solvent to evaporate during bond formation
• Contact pressure is usually sufficient
• Economical because of minute quantities needed, although relatively expensive.
Table 10.1
Benefits and Limitations of Cyanoacrylate Adhesives [14]
| Benefits | Limitations |
The Loctite Corporation offers a rubber-toughened cyanoacrylate adhesive, such as 380 Black Max®, which is reported to achieve improved strength, resiliency, and fast fixturing at the expense of a rather limited shelf life (about 4 months) [17]. This adhesive cures to fixturing strength in 2 min in the case of most substrates. It reaches 80% strength in 24 h and full strength in 72 h (Table 10.2). On aluminum, its average strength is 16.6 MPa after full room temperature cure, versus 6.2 MPa for a typical epoxy adhesive and 3.8 MPa for “instant” adhesives. After 240 h of tensile-shear thermal-cycling tests, this adhesive improved its strength to 21.3 MPa for “instant” adhesive. Loctite claims that it is consistently 20 times stronger than epoxies on aluminum, 10 times stronger on neoprene, 4 times stronger on steel, and 2 times stronger on epoxy/glass after the tests. This adhesive is designed for assembly-line cure (Table 10.3) [18].
Table 10.2
Typical Performance of Cured Loctite 380 Cyanoacrylate Adhesive [17]
| Adhesive properties | ||
| After 24 h at 22°C | ||
| Lap shear strength, ISO 4587 | ||
| Steel (grit-blasted) | N/mm2 (psi) | 26 (3,770) |
| Aluminum (etched) | N/mm2 (psi) | 18 (2,610) |
| ABS | N/mm2 (psi) | >6 (>870) |
| PVC | N/mm2 (psi) | >4 (>580) |
| Polycarbonate | N/mm2 (psi) | >5 (>725) |
| Phenolic | N/mm2 (psi) | 10 (1,450) |
| Neoprene | N/mm2 (psi) | >10 (>1,450) |
| Nitrile | N/mm2 (psi) | >10 (>1,450) |
| Tensile strength, ISO 6922 | ||
| Steel (grit-blasted) | N/mm2 (psi) | 18.5 (2,700) |
| After 48 h at 22°C | ||
| Lap shear strength, ISO 4587 | ||
| Steel (grit-blasted) | N/mm2 (psi) | ≥17.2LMS (≥2,495) |
| Cured for 24 h at 22°C, followed by 24 h at 121°C, tested at 121°C | ||
| Lap shear strength, ISO 4587 | ||
| Steel (grit-blasted) | N/mm2 (psi) | ≥6.9LMS (≥1,000) |
| Cured for 24 h at 22°C, followed by 24 h at 121°C, tested at 22°C | ||
| Lap shear strength, ISO 4587 | ||
| Steel (grit-blasted) | N/mm2 (psi) | ≥19.3LMS (≥2,800) |
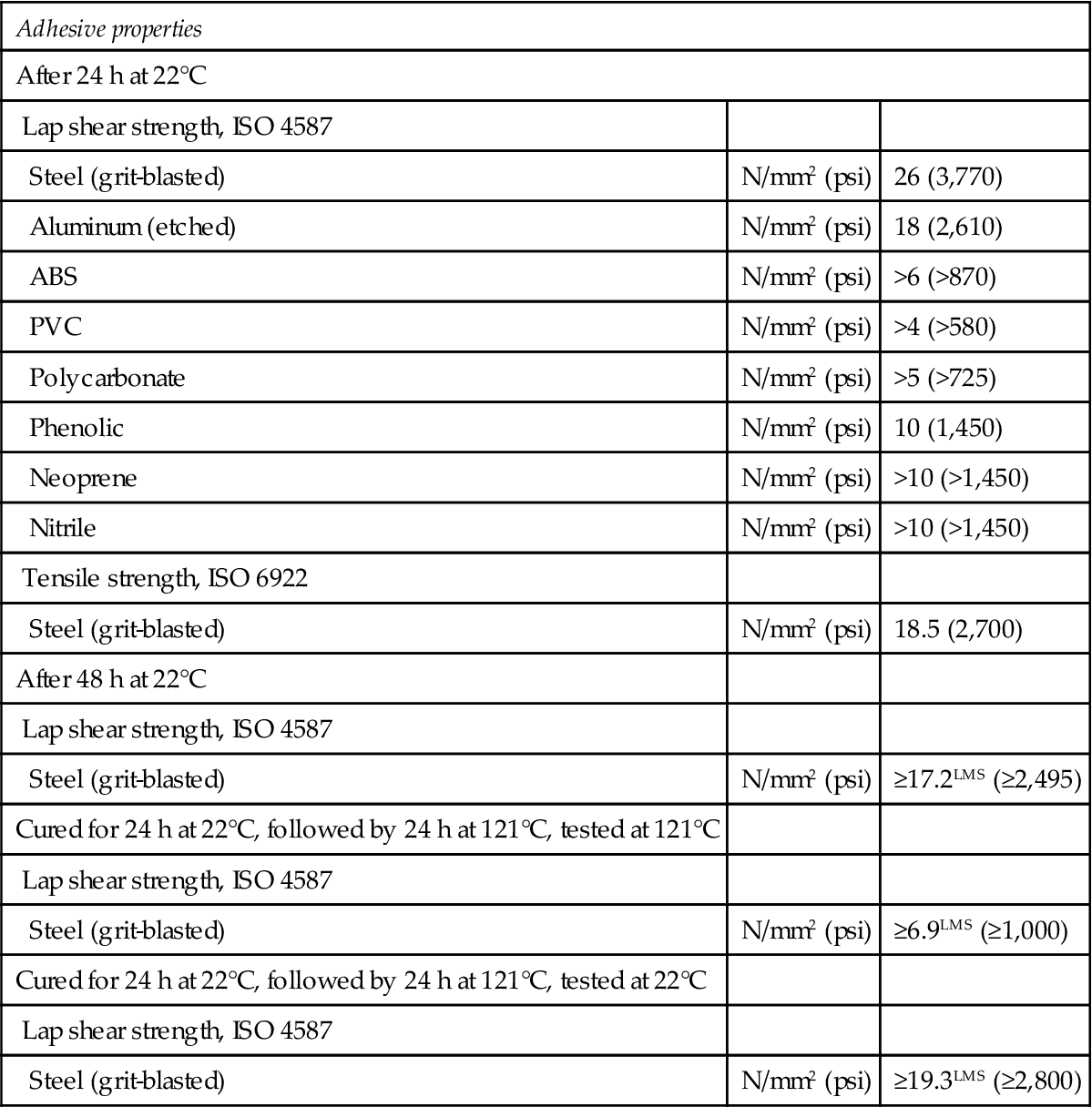
Table 10.3
Bond Strength of Methyl or Ethyl Cyanoacrylate Adhesive as a Function of Substrate and Time [14]
| Joint Substrates | Age of Bond | Shear Strength, psi |
| Steel–steel | 10 min | 1,920 |
| 48 h | 3,300 | |
| Aluminum–aluminum | 10 min | 1,480 |
| 48 h | 2,270 | |
| Butyl rubber–butyl rubber | 10 min | 150a |
| SBR rubber–SBR rubber | 10 min | 130 |
| Neoprene–neoprene | 10 min | 100a |
| SBR rubber–phenolic | 10 min | 110a |
| Phenolic–phenolic | 10 min | 930a |
| 48 h | 940a | |
| Phenolic–aluminum | 10 min | 650 |
| 48 h | 920a | |
| Aluminum–nylon | 10 min | 500 |
| 48 h | 950 | |
| Nylon–nylon | 10 min | 330 |
| 48 h | 600 | |
| Acrylic–acrylic | 10 min | 810a |
| 48 h | 790a | |
| ABS–ABS | 10 min | 640a |
| 48 h | 710a | |
| Polystyrene–polystyrene | 10 min | 330a |
| Polycarbonate–polycarbonate | 10 min | 790 |
| 48 h | 950a | |
| Polyester glass–polyester glass | 10 min | 680 |
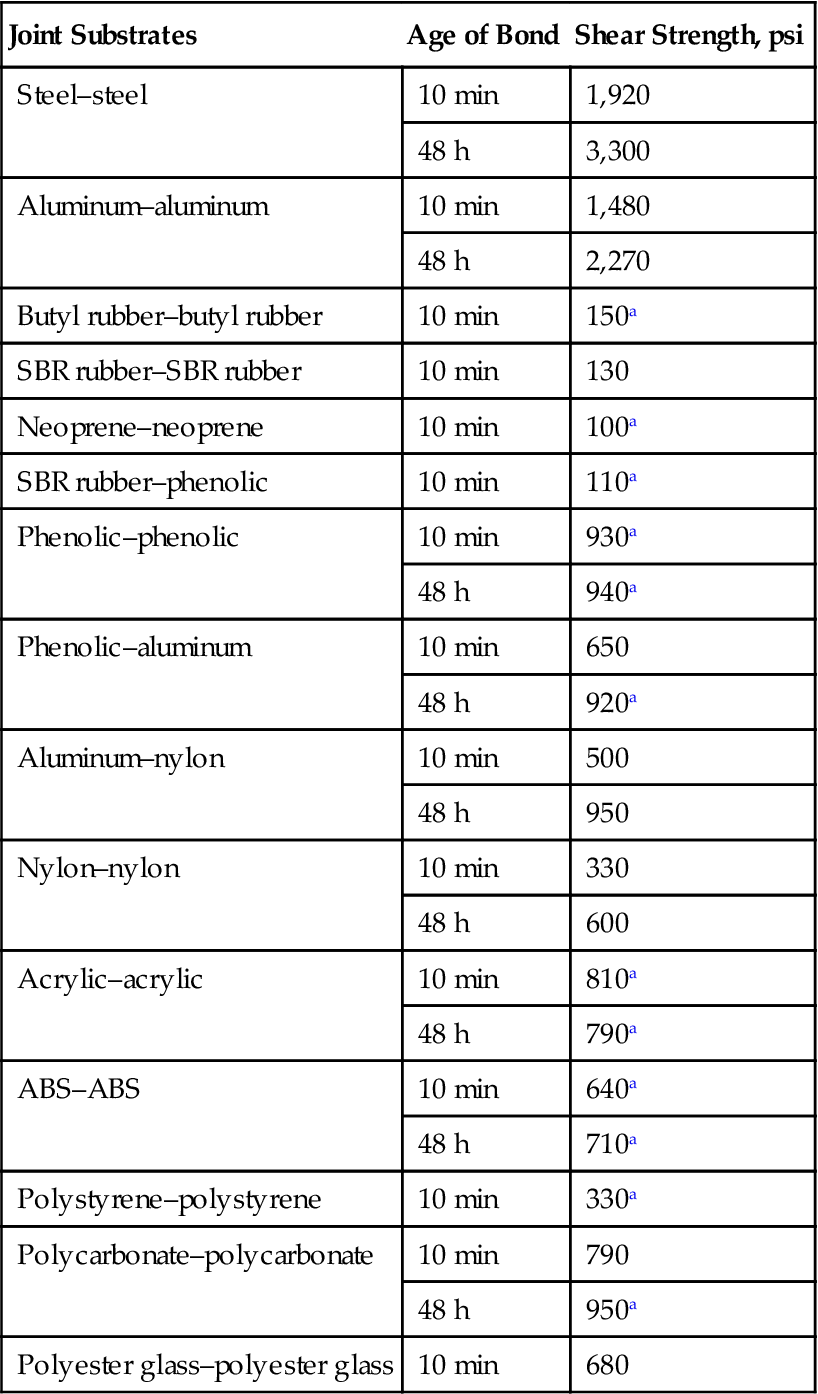
aSubstrate failure.
10.4.1 Medical Grade Cyanoacrylate Adhesives
Butyl cyanoacrylate is an intermediate-length cyanoacrylate (Figure 10.1) adhesive and was the first product to be broadly used for closing cutaneous wounds. This compound has been approved for use in Europe and Canada as Histoacryl® Blue (trademark of Aesculap, Inc.) and GluStitch® (trademark of GluStitch, Inc.) for nearly 40 years. It had not been approved by the US Food and Drug Administration (FDA) for use in the United States for a long time (see later). In Europe, Canada, and Japan, it has been used for middle ear procedures, to close cerebrospinal leaks, to repair incisions and lacerations, and to affix skin since the 1970s [19–25].
Short-chain cyanoacrylates (methyl, ethyl) are toxic to tissue; this is not the case with butyl cyanoacrylate when applied topically. In an experimental model of incision wound healing in hamsters, butyl cyanoacrylate resulted in less inflammation than that caused by 4.0 silk sutures on histologic assessment [20]. Randomized clinical trials were conducted in a study of just under 100 patients with facial lacerations suitable for tissue adhesive closure. The patients underwent closure using either butyl cyanoacrylate or octyl-2-cyanoacrylate (2-OCA), and results failed to reveal a difference in cosmetic results after 3 months. The ratings were based on assessment of photographs by a plastic surgeon using a visual analog scale [26]. A toxic reaction was prevented by taking precautions to prevent the adhesive from being trapped in the wound itself [27]. Because of these concerns, n-butyl cyanoacrylate was approved by FDA in 2000 for use in the United States. In 2010, B. Braun manufactured Histoacryl®, which consists of n-butyl-2-cyanoacrylate. This sterile, liquid topical skin adhesive is available in two formulations: Histoacryl and Histoacryl Blue [28].
2-OCA has a longer side chain than butyl cyanoacrylate. It was approved by the FDA for use in the United States in August 1998 for certain types of laceration. Its applications have been expanded and it is now marketed as Dermabond® (a trademark of Ethicon, Inc., a Johnson & Johnson Company) topical skin adhesive for closure of lacerations and incisions in place of sutures or staples. Later on, a 2-OCA formulated for greater flexibility, Liquid Bandage, was approved for use in the over-the-counter market in the United States for the treatment of minor cuts and abrasions [29].
The longer side chain gives 2-OCA several potential advantages over shorter chain cyanoacrylates. 2-OCA, for instance, produces a stronger bond and is more flexible than butyl cyanoacrylate. It has four times higher volumetric break strength than the latter [30]. Owing to the increased strength and flexibility and reduced risk of tissue toxicity, 2-OCA is now widely used in the United States for closure of wounds. It is currently one of the best selling bandage brands in the United States.
The following is an excerpt of a useful review, albeit made in 2004, of tissue adhesives, by Singer and Thode [31]: “Octylcyanoacrylate is a medical grade topical tissue adhesive that has been approved for closing surgical incisions and traumatic lacerations. We reviewed animal and human studies that evaluated its use for a variety of surgical indications and specialties. We also performed a metaanalysis of all clinical trials using octylcyanoacrylate. Data sources: Animal and human studies published in peer-reviewed articles as well as published abstracts. A search of Medline was performed using the MESH terms tissue adhesives, cyanoacrylates, and octylcyanoacrylate. Conclusions: The current review and metaanalysis demonstrate that octylcyanoacrylate can be used successfully in a wide variety of clinical and surgical settings for multiple types of wounds covering most of the surface of the human body. Prior knowledge of the limitations and technical aspects specific to wound closure with octylcyanoacrylate as well as appropriate wound selection and preparation will help ensure optimal results.”
10.4.2 Commercial Grades of Cyanoacrylate Tissue Adhesives
Some of the manufacturers of cyanoacrylate tissue adhesives are listed below:
Proprietary Device Name: HISTOACRYL® & HISTOACRYL BLUE® TOPICAL SKIN ADHESIVE
Web site: www.aesculapusa.com
Company Name: CLOSURE MEDICAL CORP.
Address: 5250 GREENS DAIRY RD.
Product: TOPICAL TISSUE ADHESIVE
Proprietary Device Name: DERMABOND® TOPICAL SKIN ADHESIVE
Website: www.closuremed.com
Proprietary Device Name: DERMABOND® TOPICAL SKIN ADHESIVE
Website: www.impactfs.com
Address: Via dei Campi, 2—PO Box 427
Proprietary Device Name: GLUBRAN2®
Website: www.gemitaly.it/web/en/glubran2.html
Company Name: HENKEL IRELAND LIMITED
ELECTRONIC AND BIOMEDICAL FACILITY
Address: Whitestown, Dublin, 24 EI
Proprietary Device Name: INDERMIL® TISSUE ADHESIVE
Website: www.henkel.com/cps/rde/xchg/henkel_com/hs.xsl/indermil-17865.htm?automaticTransfer=3
Company Name: MEDISAV SERVICES, INC.
Product: TISSUE ADHESIVE FOR REPAIR OF MINOR CUTS & LACERATIONS
Proprietary Device Name: EPIDERMGLU®
Website: http://www.ethicon.com
Company Name: SKINSTITCH CORP.
Product: TISSUE ADHESIVE FOR REPAIR OF MINOR CUTS & LACERATIONS
Proprietary Device Name: SKINSTITCH™
Website: www.skinstitch.com
Cyanoacrylate tissue adhesives can be used in lieu of sutures in a number of surgical procedures contributing to make the recovery easier and more comfortable [32]. They include:
1. OB/GYN surgeries, such as C-sections where excellent cosmetic outcomes are desired [33], as well as the ability for new mothers to shower immediately and move about without the discomfort of staples or sutures [34].
2. General surgeries, such as many abdominal surgeries, back surgeries, and routine surgeries of the face, neck, arms, and legs [35].
3. Cardiovascular surgeries that may involve incisions in the arm or leg as well as the chest [35].
4. Cosmetic surgery, particularly facial incisions, on areas such as the eyelid and the nose where suture removal can be painful. No stitches means no “suture marks” [36].
5. Sports surgery, involving lacerations that may need immediate attention, to help players to return to the game [37].
Dermabond® (2-octylcyanoacrylate by Ethicon, a Johnson & Johnson Company), the latest in cyanoacrylate technology, has less toxicity and almost four times the strength of n-butyl-2-cyanoacrylate. Special plasticizers have been added to the formula to provide flexibility. It is marketed to replace sutures that are 5-0 or smaller in diameter for incision or laceration repair. Patients, especially children, readily accept the idea of being “glued” over traditional methods of repair [38]. This adhesive reaches maximum bonding strength within 2.5 min and is equivalent in strength to healed tissue at 7 days post-repair [38].
Dermabond has been found to create [39] a microbial barrier over the wound and protect against the penetration of the following bacteria, commonly associated with surgical site infections:
Dermabond adhesives [39]:
1. Provide the strength of healed tissue at 7 days in less than 3 min
2. Offer three-dimensional strength that is at least three times greater than that of n-butyl cyanoacrylate, another leading type of adhesive
3. Help protect and seal out bacteria that can lead to infection
4. Promote a moist wound-healing environment that has been shown to speed the rate of epithelialization
5. Cause less pain and relieve anxiety over sutures, particularly important for pediatric patients; have been found to be as safe and effective as conventional sutures with equivalent cosmetic results
6. Save valuable clinical time in that they can be applied more quickly than sutures, eliminating the need for the following process:
a. Injecting a local anesthetic into the wound
b. Waiting for the anesthetic to numb the area
c. Closing the wound with sutures
d. Placing a dressing over the wound
7. Slough off naturally over time (usually 5–10 days), eliminating the need for a follow-up visit to remove stitches.
10.5 Test Methods to Characterize Strength of Tissue Adhesives
The following four test methods are used [40] to provide a means for comparison of the adhesive strengths of tissue adhesives for use as surgical adhesives or sealants on soft tissue. These or equivalent methods may be used in support of the bench testing outlined above:
ASTM F2255-05 Standard Test Method for Strength Properties of Tissue Adhesives in Lap-Shear by Tension Loading
ASTM F2256-05 Standard Test Method for Strength Properties of Tissue Adhesives in T-Peel by Tension Loading
ASTM F2258-05 Standard Test Method for Strength Properties of Tissue Adhesives in Tension
ASTM F2458-05 Standard Test Method for Wound Closure Strength in Tissue Adhesives and Sealants.
10.6 Medical and Dental Applications of Adhesives
The use of adhesives in medical applications has been restricted, for some time, to the manufacture of self-adhesive bandages (plasters, self-adhesive strips of fabric, etc.). The first pressure sensitive adhesives used for this were based on natural rubber, decades ago. This first usage was later partially superseded by synthetic rubbers (e.g., polyisoprene, polyisobutylene). In the mid-twentieth century, pressure sensitive adhesives based on polyacrylic acid esters gained significance in general use and in the composition of bandage materials [41].
Today, adhesives are used in various areas of medicine, replacing traditional methods with “friendlier” processes. Often, stitches can be avoided by applying special cyanoacrylate adhesives to quickly close skin wounds. An advantage of this method is that the whole wound can be covered, thereby largely suppressing secondary bleeding and the risk of infection. Cyanoacrylic acid butyl ester is normally preferred over the methyl and ethyl esters because it cures more slowly and the polymerization produces less heat. Cyanoacrylic also causes less tissue irritation. By and large, this adhesive is only used for relatively small wounds, and it is occasionally used in vascular surgery.
Consider the transdermal patches where the drug delivery mechanism to the bloodstream is through the skin: adhesives enable a more efficient method of drug delivery, rather than prescribing a high-ingestion dosage (which is subsequently flushed out of the body by the liver). Transdermal patch technology is highly effective because the adhesive that sticks the patch to the skin—made of products of chemistry like acrylic, acrylic-rubber hybrid, polyisobutylene, and styrenic rubber solution—actually controls the rate at which the drug enters the body. This mechanism ensures that the drug dosage is continuously and evenly administered throughout the day, without the spikes and falls associated with medicines administered orally [41].
The applications of these patches are numerous, including smoke cessation and hormone replacement; and cardiovascular aid, such as nitroglycerin delivery, is commonplace. New transdermal patches hit the market every day, with more applications like pain cessation becoming a reality. Other innovative products, such as foot care and cosmetic patches, and nasal dilator strips, have come onto the market in recent years. Their existence is possible because of the unique functional properties of the pressure sensitive adhesives integral to the product [41].
One of the newest bio-adhesives on the market enables drugs to be delivered through the inside of the mouth, nasal passages, and other mucous membranes, rather than only being administered through skin. The newest bio-adhesives adhere extremely well to the soft, wet mucous membranes of the body because the adhesives are made from starch-polyacrylic acid blends, which then completely erode and disappear. Drug makers are able to put their medicine into tablet, film, or powder form, and the patient is able to attach the product directly to a mucous membrane, providing a means for controlled delivery of drugs to specific areas of the body or systemically (throughout the body) [41].
Fibrin, which is made from fibrinogen, a soluble protein recovered from blood, is a key sealing agent in heart surgery. It has a hemostatic effect, meaning that it is an antihemorrhagic agent: a substance that promotes hemostasis, the halting of blood flow. Fibrin is much gentler on the body tissues when compared to cyanoacrylates. The disadvantage of fibrin is that before use it must undergo a special treatment in order to prevent microbial infection.
The use of methacrylate-based adhesives has been a great success in orthopedics for the purpose of anchoring hip socket implants to the bone. There are currently no other types of adhesive used for this application. The adhesive products comprise (i) a powder component (a mixture of polymethyl methacrylate (PMMA) and a polymerization initiator) and (ii) a liquid component (whose main components are methyl methacrylate (MMA) and a polymerization accelerator). In spite of the considerable stress that these adhesives exert on bone and tissue due to intense heat development, hip and knee implants anchored using this adhesive are in 90% of cases functional for upwards of 15 years [41].
In dentistry, restorative fillings based on UV curing acrylates have largely replaced traditional filling materials such as amalgams. The products have a long pot life or open time (the period during which they can be used after mixing) and bond in just a minute or so when exposed to UV light.
There are numerous orthodontic appliances or devices that are used to correct dental conditions in minor and adult patients. Most of these appliances involve use of adhesives. The advent of adhesive dentistry and direct bonding of orthodontic brackets is a dramatic event that has changed the course of clinical orthodontics. Product development and technological advances have occurred quite rapidly. This rapidity has, at times, complicated the decision-making process for practitioners [42].
10.6.1 Adhesives for Skin Closure
This section reviews the use of adhesives as an alternative to stitches. The key advantage of supplanting stitches with an adhesive is that the adhesive overlays the entire wound as a continuum. The global coverage prevents secondary bleeding and reduces the risk of infection by creating a temporary barrier while healing takes place. Other advantages of gluing the skin are that it is quick, saves surgery time, is inexpensive, does not involve stitch removal, and is waterproof. The disadvantage of gluing is that doing so can be messy if the adhesive is applied incorrectly.
One of the adhesive options is copolymeric hydrogels, comprised [43] of aminated star polyethylene glycol and dextran aldehyde (PEG:dextran). These materials exhibit physicochemical properties that can be modified to achieve organ- and tissue-specific adhesion performance. The investigators reported that resistance to failure under specific loading conditions, as well as tissue response at the adhesive material–tissue interface, can be modulated through regulation of number and density of adhesive aldehyde groups.
There are two common adhesive choices: cyanoacrylic and methyl metacrylic. Cyanoacrylic acid butyl ester is usually preferred over the methyl and ethyl esters because of its slower cure (polymerization) rate. Consequently, the polymerization produces less heat; it also causes less tissue irritation. Cyanoacrylate glue is commonly used for approximation of skin after various surgical procedures [44], and is occasionally used to embolize blood vessels [45,46] and to occlude fistulas [47].
There is no need to apply a dressing to cover the wound after gluing the skin. Apart from eyes and mucous membranes, adhesive may be used to close various clean wounds of the skin, including covering wounds of the face if there is no contraindication. However, glue application has some disadvantages: some glue applications are messy, may not hold oozing wound edges, and may stick to the instruments and gloves. Meticulous attention to different techniques in various situations may avoid most of the disadvantages. Gluing is common in surgery, but it is not formally taught. This illustrated chapter has been written to educate junior doctors without any practical experience in using tissue glue.
FDA approved cyanoacrylate adhesives are considered comparable to 5-0 sutures but are not recommended to be used alone in high tension areas.
10.6.2 Case Studies of Tissue Adhesives
In this section, examples of the use of tissue adhesives, namely cyanoacrylates, in the closure of different types of lacerations and surgical incisions, are discussed. In vitro and in vivo animal and human studies have been conducted to assess the efficacy and outcome of tissue adhesives as compared to traditional stitching.
10.6.2.1 Comparison of Effects of Suture and Tissue Adhesive on Bacterial Counts
In this study [48], the effects of closing lacerations with suture or cyanoacrylate tissue adhesive on staphylococcal counts in inoculated guinea pig lacerations were investigated. Wounds closed with adhesive alone had lower counts than did wounds containing suture material (P <0.05). The results of a time-kill study were consistent with a bacteriostatic adhesive effect of the adhesive against S. aureus.
Another study used a well diffusion method to conclude that cyanoacrylate adhesive is bacteriostatic for Gram-positive organisms [49]. It is also known that suture material increases the risk of wound sepsis by serving as an adherent foreign body [49,50]. In contrast, S. epidermidis adheres to cyanoacrylate adhesive, which may thus promote wound infection [51]. The authors studied the difference in wound bacterial counts among the following wound closure methods (the terms are given in parentheses): use of a cyanoacrylate adhesive alone (glue), adhesive and subcutaneous suture (glue/SQ), skin suture alone (suture), and skin suture with subcutaneous suture (suture/SQ).
Four lacerations each, with a length of 3 cm, were made parallel to the spine to deep fascia. The lacerations were inoculated with S. aureus (ATCC 11632) and adjusted to a spectrophotometric absorbance of 0.138–0.139. Inocula were quantified at approximately 108 CFU/ml by standard microbiological methods. After inoculating the lacerations, the four wounds on each animal were approximated in one of four ways: (1) with Nexaband Liquid (n-butyl-2-cyanoacrylate and D and C violet number six dye) (glue), (2) with subcutaneous suture (i.e., intradermal stitches buried beneath the skin) followed by application of Nexaband Liquid (glue/SQ), (3) with simple skin suture (suture), or (4) with intradermal subcutaneous suture followed by simple skin suture (suture/SQ).
Table 10.4 summarizes the wound data. Any lacerations subject to protocol abrogations were excluded. Wound bacterial counts for glue were significantly lower than those for glue/SQ, suture, and suture/SQ. A time-kill study of Nexaband with S. aureus was also performed according to National Committee for Clinical Laboratory Standards guidelines [52]. Four drops of Nexaband, the approximate amount used to close each laceration, were suspended in Trypticase™ soy broth before vortexing. The results of the kill study are summarized in Figure 10.3. Broth containing cyanoacrylate exhibited bacterial growth levels significantly lower than those of the control.
Table 10.4
Bacterial Counts for Contaminated Lacerations Treated with Tissue Adhesive and Suturea [48]
| Treatment Method | Mean Bacterial Count±SDb | 95% Confidence Interval |
| Glue | 1.78±1.9 | 0.5–3.06 |
| Glue/SQ | 4.42±1.92 | 3.1–5.7 |
| Suture | 3.72±1.4 | 2.83–4.62 |
| Suture/SQ | 4.58±1.43 | 3.67–5.49 |
aThe adhesive used was n-butyl-2-cyanoacrylate tissue adhesive; skin sutures were done with monofilament nylon, and subcutaneous sutures were done with braided absorbable suture.
bValues are log10 conversions of CFU per gram of tissue.
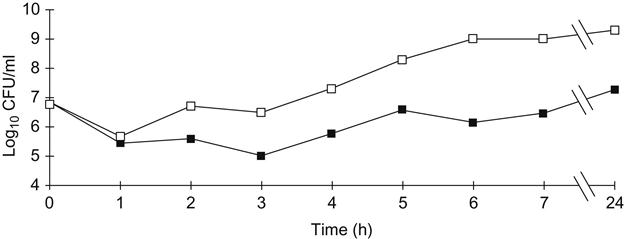
The study concluded that contaminated wounds sealed with cyanoacrylate alone have appreciably lower staphylococcus counts than do lacerations containing suture material. The presence of suture material in some wounds may be the reason for this effect. Bacteriostatic behavior of the products containing cyanoacrylate may also be at work. No study has, however, found any adhesive present in the wound after closure.
The microbiological permeability of cyanoacrylate compounds, using Liquiseal (MedLogic Global Ltd, Plymouth, UK) as an example, was studied [53] to verify its reported primary attribute as a compound that remains impervious to microorganisms and water for 1 week following application. The occlusive dressing used was OpSite (Smith & Nephew, London, UK), commonly used in surgical procedures. The methods used in the study are well established in the investigation of bacterial penetration through various materials [54]. The organisms selected were S. aureus and E. coli, both known to be common pathogens causing surgical site infections.
This study [54] demonstrated that, as a barrier to microbiological penetration, cyanoacrylates are as effective as standard occlusive dressings. The limitations of the two types of dressing are similar: both have the potential to allow bacteria to travel around the edges of the dressing and potentially infect the wound. However, as suggested by Bady and Wongworawat, the adhesion that the cyanoacrylate compounds have with the skin is effective in preventing the translocation of microorganisms across the skin [55].
10.6.2.2 Sutureless Anastomoses of Small and Medium Vessels
In a study in China [56], an animal model was used to assess the efficacy of sutureless anastomoses using tissue adhesives. The two cut ends of the rabbit common carotid artery were sutured by three stitches with a 1208 interval circumferentially. Then two optional threads were pulled horizontally and 0.1 ml cyanoacrylate adhesive was smeared on the attached surfaces of the two ends. The three stitches were removed after completion of anastomosis. The burst pressure of the anastomosis was measured and compared with that of a traditional sutured artery. The glued anastomosis was associated with a shorter completion time (8.25±6.34 min vs. 20.67±14.24 min, P<0.01), less bleeding (3.17±9.04 ml vs. 11.04±16.28 ml, P<0.01), and equivalent patency (93.8 vs. 87.5%, P<0.05). The sutureless anastomosis was associated with less intimal thickening (decreased by 31.4, 24.5, 23.9, and 31.9%, P<0.01 compared with the traditional suture group at 1, 2, 4, and 12 weeks, respectively). The study concluded that glued anastomoses provide an effective, simple, and feasible way for anastomosing small or medium caliber vessels. This technique can also reduce intimal injury (i.e., to the inner lining of the vessels).
Another paper [57] presents the results of an experimental study of small arterial anastomosis, combining suture with the cyanoacrylate tissue adhesive. At the distal end of the vessel, two parallel incisions were made, 180° apart from each other, and two sutures were placed passing from the proximal end to exit from the most distal part of the longitudinal incisions. The tissue adhesive was then applied to the proximal vessel, and the full-thickness vascular “lid” flap was closed over it on anterior and posterior surfaces. Eighty anastomoses were carried out on the left and the right femoral arteries of 40 Wistar rats. For all of the animals, conventional end-to-end anastomosis was carried out on the left side, and the lid technique was used on the right side. There was no statistically significant difference between the patency rates of the groups (two non-patent in the control and two in the study group) (P>0.05), whereas significantly reduced operation time (mean 16.2 and 10.7 min in control and study groups, respectively) (P<0.0001) and bleeding time (median 1.5 and 0.5 min in control and study groups, respectively) (P<0.0001) were documented in the study group. Histopathological evaluation of both the patent and non-patent vessels at day 21 revealed no signs of tissue toxicity or intraluminal adhesive leakage. In view of these data, the investigators concluded that using cyanoacrylate tissue adhesive provides an effective and simple method for end-to-end anastomosis of small-size arteries.
Akhtar [58] has put forth contradictory studies regarding the toxicity and long-term effects of cyanoacrylate. He cites that Barbalinardo et al. [59] compared relative effectiveness of isobutyl 2-cyanoacrylate, fibrin adhesive, and oxidized regenerated cellulose, which was determined by application of these hemostatic agents to sources of point bleeding. They found, in the meantime, that hemostasis was shorter in the cyanoacrylate group, but the reported inflammatory response that it induced, and its possible carcinogenicity, limited its availability for clinical use. Ellman et al. [60], also using oxidized cellulose (Surgicel) as control, assessed two formulations of a new cyanoacrylate compound. Long-term graft patency was assessed angiographically at 4, 6, and 18 months. Tissue reaction at 2 weeks, and at 1, 6, and 18 months, was assessed grossly by vascular surgeons and microscopically by a blinded pathologist. There were no significant differences between groups with regard to graft patency. Histopathology showed mild to moderate tissue reaction at 2 weeks and 1 month in the cyanoacrylate groups compared with controls at 1 month (ANOVA P=0.004). Mild tissue reaction was seen at 6 and 18 months, with no significant differences between groups (ANOVA P=0.08, 0.62, respectively). Their conclusion was that the cyanoacrylate compound was an effective suture line sealant.
10.6.2.3 Tissue Adhesive as Dressing after Open Pediatric Urological Procedures [61]
In 2003, an effectiveness study of 2-OCA (Dermabond by Ethicon, Inc.) tissue adhesive as a sole dressing after open pediatric urological procedures, was carried out. For a period of 6 months, February to August 2003, the investigators prospectively evaluated patients undergoing extragenital open and laparoscopic pediatric urological procedures at the Children’s Hospital, University of Colorado School of Medicine in Denver, Colorado. All open incisions were closed in layers using a final layer of self-absorbing subcuticular stitches for the skin before applying Dermabond cyanoacrylate adhesive at the skin level alone. In laparoscopic cases, Dermabond alone was applied to the port sites (3 mm or less in diameter) and instrument sites without any sutures beneath the skin. No adjuvant occlusive dressings were applied to any of these wounds. All patients were allowed to bathe and return to normal lifestyle activities immediately postoperatively.
A total of 146 patients participated in the study with a total of 200 incisions (open 146, laparoscopy 54). Of these children, 103 who had had 142 incisions returned for follow-up visits during the period of study. Only one complication was identified. The subject, a 6-month-old infant, presented in the evening of surgery with omental prolapse through the umbilical port (3 mm port) requiring urgent closure. There were no cases in which appreciable healing problems were identified by surgeon or parent examinations. No wound infection occurred. It was concluded that Dermabond alone provides a simple coverage for a vast range of pediatric urological surgical wounds, and that immediate bathing and return to normal lifestyle activities do not seem to affect the wound healing adversely as long as a simple skin barrier, in place of standard dressings, is applied to the wound site [61].
10.6.2.4 Tissue Adhesive Applications in Gastrointestinal Endoscopic Procedures [62]
This section is based on a 2006 review paper by Ryou and Thompson. Cyanoacrylates and other tissue adhesives can be applied locally for a variety of indications, including hemostatic, wound closure, and fistula repair. The main classes of tissue adhesives currently used in gastrointestinal (GI) endoscopy include cyanoacrylates, fibrin glues, and thrombin. The focus of this section is on applications of cyanoacrylates.
Gastric Variceal Bleeding
Injection therapy with cyanoacrylates is now the first line of endoscopic intervention for bleeding gastric varices as well as secondary prevention of gastric variceal bleeds outside of the United States [63].
In a randomized controlled trial of 59 patients, cyanoacrylate injection of bleeding gastric varices was reported to be more effective and safer than band ligation. Both initial hemostatic rate and rebleeding rates were lower in the cyanoacrylate group compared with the band ligation group. Initial hemostatic rates were 87% in the cyanoacrylate group compared with 45% in the band ligation group (P=0.03); rebleeding rates in the cyanoacrylate group were 31% compared with 54% in the band ligation group (P=0.0005). Treatment-induced ulcer bleeding occurred in two patients (7%) in the cyanoacrylate group and eight patients (28%) in the band ligation group (P=0.03). The amount of blood transfusions required was also higher in the band ligation group than in the cyanoacrylate group (4.2±1.3 vs. 2.6±0.9 units, respectively) (P<0.01) [64].
Esophageal Variceal Bleeding
Several randomized controlled studies have demonstrated that injection of cyanoacrylate is comparable to sclerotherapy in the endoscopic hemostasis of acute variceal bleeding and prevention of rebleeding [65–67].
Peptic Ulcer Bleeding
In a randomized controlled trial comparing injection of cyanoacrylate and hypertonic saline for bleeding gastroduodenal ulcers, initial hemostasis was similar in both groups and the rebleeding rate was lower after cyanoacrylate injection [68]. There are no studies comparing glue injection to a combination of injection and cautery or application of clips, which are considered more effective than saline injection alone for the treatment of bleeding ulcers.
Bleeding from Other Sources
Cyanoacrylate injection has been used successfully in the management of a few patients with Dieulafoy’s lesions and bleeding tumors [69–70].
Closure of Fistula
Cyanoacrylates have been shown to be successful in the closure of pancreatic fistulas, biliary fistulas [71], and GI fistulas [72] (Seewald and coworkers reported successful closure of pancreatic fistulas in 8 of 12 patients using endoscopic injection of Histoacryl into the fistulous tract and endoscopic drainage) [73]. Seven of the eight successful patients required only one treatment over a median follow-up period of 21 months. Closure was temporary in two patients, unsuccessful in one patient, and there was one death within 24 h of treatment from pulmonary embolism.
Some complications have been described with the use of cyanoacrylates such as systemic inflammatory reaction to foreign body (pain and fever, local tissue necrosis) and inflammatory reaction to foreign body (mediastinitis, esophageal pleural fistula, duodenal ulcer perforation, pancreaticoduodenal necrosis, inflammatory pseudotumor of pancreatic tail) [74–78]. Other types of complications have also been reported [79–83].
10.6.2.5 Tissue Adhesives in Topical Skin Wounds [84]
There are over 7 million traumatic lacerations each year in the USA [85] in addition to tens of millions of surgical incisions. All require closure by surgeons, emergency physicians, and primary care practitioners [86]. These wounds and incisions have been traditionally closed with sutures, staples, or surgical tapes, and more recently, tissue adhesives. An ideal wound closure device should be user friendly, quick, pain free and result in excellent cosmesis, without device removal requirement, and of course be cost-effective [87]. None of the current closure devices possesses all of these requirements. Topical cyanoacrylate tissue adhesives, however, have a number of the characteristics of an ideal wound closure device.
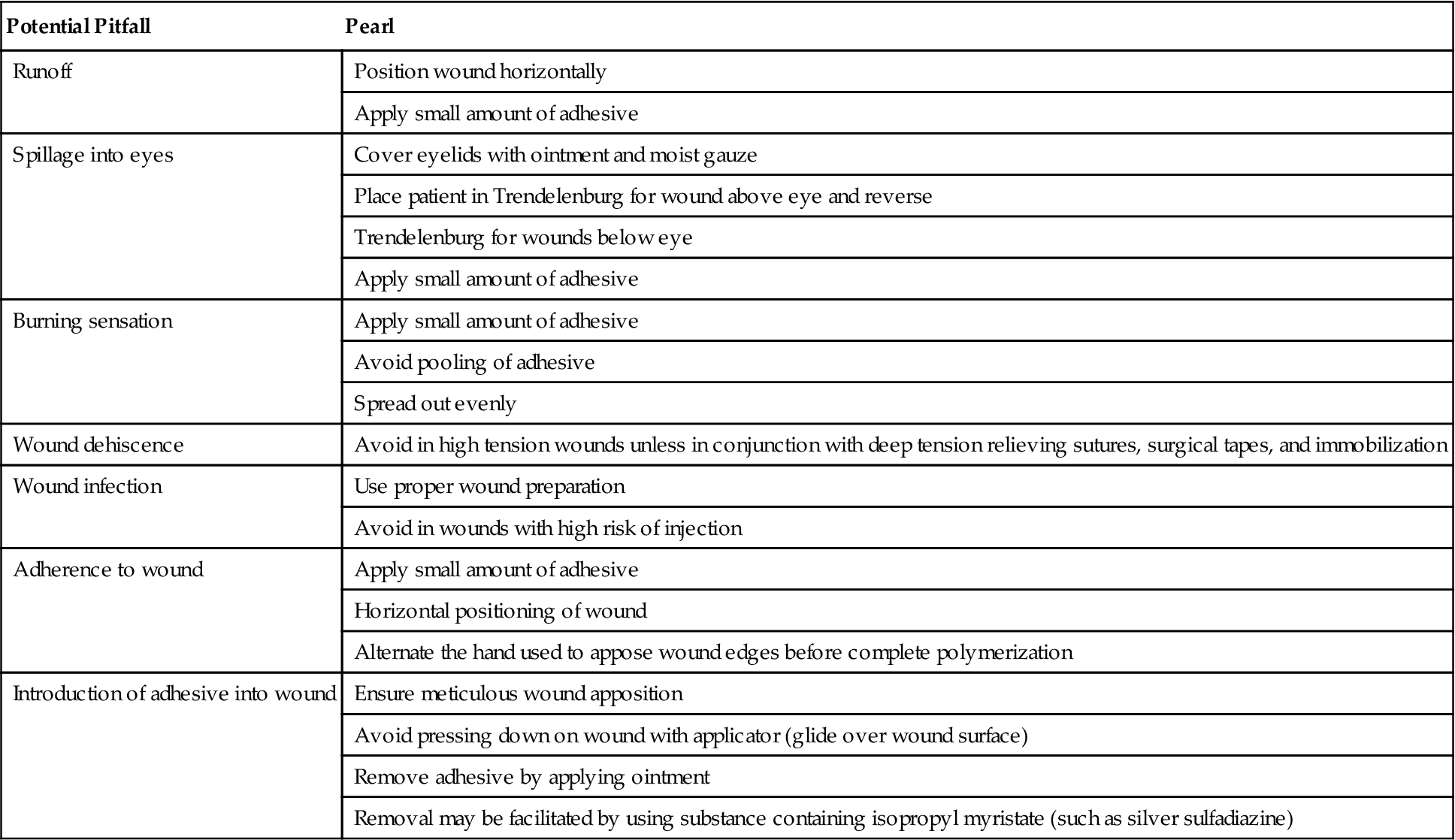
Cyanoacrylate topical adhesives have some obvious advantages over sutures such as ease of use and pain-free application of the adhesive. Consequently, local anesthetics are unnecessary. In addition, because the cyanoacrylate adhesives slough off spontaneously within 5–10 days, no removal is required—a procedure that may be painful and threatening, especially to children. Although the cost of the cyanoacrylate adhesives is higher than that of most sutures, a formal cost-effective analysis conducted several years ago that included the costs of the suture kits, suture removal kits, and dressing materials, demonstrated that use of the adhesives actually reduces the costs [88]. The use of the topical cyanoacrylate adhesives also reduces the risks of needle sticks [89] and prevents the formation of suture marks on either side of the wound. Unlike suturing that has a learning curve of up to 2 years [90], proficiency at using the cyanoacrylate adhesives is rapidly attained [91]. They also have the potential to save operative time, especially with longer incisions and lacerations. In surveys, most surgical patients prefer topical adhesives to sutures or staples [92–94]. In contrast, in a study of 724 emergency department patients, of which two-thirds had a prior or current laceration, more patients preferred sutures to adhesives [53]. The surgical tapes offer many of the same advantages that the topical skin adhesives offer and are a reasonable alternative for closure of appropriate wounds [26,33]. Surgical tapes are easy to use, rapid, painless, and comfortable, do not require removal, and are less costly than any of the wound closure devices. However, because of their low bursting strength and tendency to fall off, the use of surgical tapes is limited to simple very-low-tension wounds. Furthermore, surgical tapes do not have microbial barrier properties. A summary of the advantages, disadvantages, and common indications for the various wound closure devices is presented in Table 10.5. A summary of potential pitfalls associated with the cyanoacrylates together with possible solutions is presented in Table 10.6.
Table 10.5
Comparison of Wound Closure Devices [84]
| Sutures | Staple | Tapes | Adhesives | |
| Advantages | Most meticulous approximation | Fast | Fast | Fast |
| Great tensile strength | Good tensile strength | Simple | Simple | |
| Low dehiscence rate | Simple | Inexpensive | No risk of needle stick | |
| Time honored | Lower tissue reactivity | Minimal reactivity | No need for removal | |
| Lower risk of needle stick | No risk of needle stick | Microbial barrier | ||
| No need for removal Comfortable | Occlusive dressing Comfortable | |||
| Disadvantages | Painful | Less meticulous approximation | Lowest tensile strength | Lower tensile strength than sutures |
| Prolonged learning curve | Painful | Highest risk of dehiscence | Limited moisture resistance | |
| Require removal | Require removal | No moisture resistance | ||
| May leave suture marks | ||||
| Risk of needle stick | ||||
| Most reactive | ||||
| Indications | Most incisions and lacerations | Long linear incisions and lacerations | Linear low tension wounds and lacerations | Linear low tension wounds and lacerations |
| Scalp wounds | Fragile skin (flaps and skin tears) | Fragile skin | ||
| Wound support after suture/staple removal | Under splints/casts | |||
| Under splints/casts | ||||
| Contraindications | Infected or heavily contaminated wounds | Inadequate hemostasis | Inadequate hemostasis | Inadequate hemostasis |
| Complex irregular wounds | High tension | High tension | ||
| Hair bearing area Uncooperative patients Circumferential use around digits Proximity to moist areas |
Hair bearing area Proximity to moist areas |
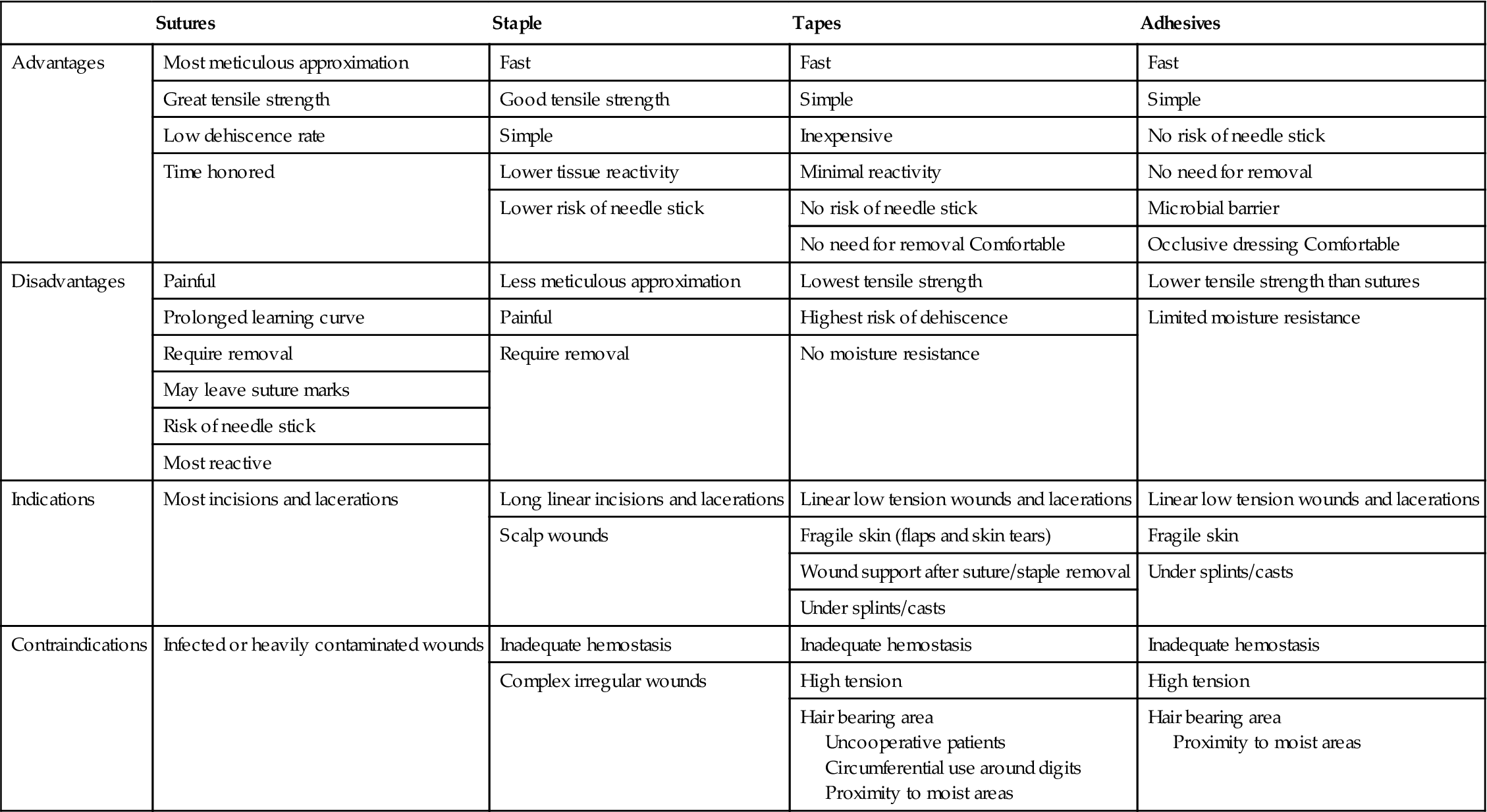
Table 10.6
Potential Cyanoacrylate Pitfalls and Pearls [84]
| Potential Pitfall | Pearl |
| Runoff | Position wound horizontally |
| Apply small amount of adhesive | |
| Spillage into eyes | Cover eyelids with ointment and moist gauze |
| Place patient in Trendelenburg for wound above eye and reverse | |
| Trendelenburg for wounds below eye | |
| Apply small amount of adhesive | |
| Burning sensation | Apply small amount of adhesive |
| Avoid pooling of adhesive | |
| Spread out evenly | |
| Wound dehiscence | Avoid in high tension wounds unless in conjunction with deep tension relieving sutures, surgical tapes, and immobilization |
| Wound infection | Use proper wound preparation |
| Avoid in wounds with high risk of injection | |
| Adherence to wound | Apply small amount of adhesive |
| Horizontal positioning of wound | |
| Alternate the hand used to appose wound edges before complete polymerization | |
| Introduction of adhesive into wound | Ensure meticulous wound apposition |
| Avoid pressing down on wound with applicator (glide over wound surface) | |
| Remove adhesive by applying ointment | |
| Removal may be facilitated by using substance containing isopropyl myristate (such as silver sulfadiazine) |
10.6.2.6 Tissue Adhesive for Closure of Hernia Incisions
The study in Ref. [95] intended to elucidate that suture-based permanent mesh fixation can be replaced by fixation with n-butyl-2-cyanoacrylate glue (Glubran® 2 by GEM S. r. l., Italy) for surgical repair of abdominal wall hernias. The aim of this study was to investigate in a rat animal model the efficacy of the use of a small amount of modified n-butyl-2-cyanoacrylate (Glubran 2) in abdominal mesh fixation as a feasible alternative to sutures and staples. Glubran 2 is a class III medical-surgical product (for internal and external surgical use) which has outstanding hemostatic and adhesive properties and, once set, produces an effective antiseptic barrier against infectious agents or pathogens commonly found in surgical settings. At the present time, it is used in open and laparoscopic surgery, digestive tract endoscopy, interventional radiology, and vascular neuroradiology.
In 25 Wistar rats, two hernia defects (1.5 cm in diameter) per animal were created bilaterally in the midline of the abdominal wall. The peritoneum was spared. The lesions were left untreated for 10 days to achieve a chronic condition. Then the defects were covered with TiMESH extra light and fixed by 30 μL of Glubran 2 or traditional suture. The time points of sacrifice were 17 and 28 days, and 3, 4, and 5 months. At autopsy, histology and immunohistochemistry were performed to evaluate the inflammatory response and the presence of apoptotic cells, respectively. Mesh fixation was excellent in all samples at each time point. At application sites, the inflammatory reaction was mild with a small number of macrophages and vascularized connective tissue presence around glue and mesh threads. Glue residues were observed in histologic sections at each time point. No presence of apoptotic cells was found. This study demonstrated that Glubran 2 can effectively replace traditional sutures in mesh fixation without affecting tissue healing and determining a physiological inflammatory reaction at the abdominal wall site.
In conclusion, on the basis of these experimental results, the use of an appropriate amount of Glubran 2 can effectively replace traditional suture threads in fixing abdominal mesh, guaranteeing long-term, firm adhesion without increasing inflammation.
In another study [96], the investigators compared the skin adhesive 2-octylcyanoacrylate to subcuticular suture for closure of pediatric inguinal hernia incisions to determine if skin adhesive improves wound cosmesis, shortens skin closure time, and lowers operative costs. They prospectively randomized 134 children undergoing inguinal herniorrhaphy at the Children’s Hospital of the University of Michigan to have skin closure with either skin adhesive (n=64) or subcuticular closure (n=70). Data collected included age, sex, weight, type of operation, total operative time, and skin closure time. Digital photographs of healing incisions were taken at the 6-week postoperative visit. The operating surgeon assessed cosmetic outcome of incisions using a previously validated visual analog scale, as well as an ordinate scale. A blinded assessment of cosmetic outcome was then performed by an independent surgeon comparing these photographs to the visual analog scale. Operating room time and resource use (i.e., costs) relative to the skin closure were assessed. Comparisons between groups were done using Student’s t tests and χ2 tests.
Children that enrolled in the study had a mean age of 3.7±0.3 years and weighed 16±0.8 kg. Patients were predominantly male (82%). Patients underwent one of three types of open hernia repair as follows: unilateral herniorrhaphy without peritoneoscopy (n=41; 31%), unilateral herniorrhaphy with peritoneoscopy (n=55; 41%), and bilateral herniorrhaphy (n=38; 28%). Skin closure time was significantly shorter in the skin adhesive group (adhesive=1.4±0.8 min vs. suture=2.4±1.1 min; P=0.001). Mean wound cosmesis scores based on the visual analog scale were similar between groups (adhesive=78±21; suture=78±18; P=0.50). Material costs related to herniorrhaphy were higher for skin adhesive (adhesive = $22.63 vs. suture = $11.70; P=0.001), whereas operating room time costs for adhesive skin closure were lower (adhesive=$9.33±5.33 vs. suture=$16.00±7.33; P=0.001). Except for a 7% incidence of erythema in both groups, there were no complications encountered. In the meantime, the data from this trial suggest that skin adhesive wound closure in inguinal hernia repair is associated with a small reduction in operative time without effect upon total cost, complication rate, or cosmesis.
10.6.2.7 Use of Tissue Adhesive for Skin Closure in Plastic Surgery [97]
Abdominoplasty and mammoplasty are cosmetic surgeries that demand relatively more time for skin closure. Methods: Skin closure with 4.0 Mononylon (Ethicon) continuous subcuticular suture and with Dermabond (Ethicon) (octylcyanoacrylate) was compared among 37 patients who had undergone body contouring surgery (23 abdominoplasties and 14 mammoplasties). Each side of the scar, randomly selected, was closed either with adhesive or suture. The time required for skin closure and the aesthetic aspect of these scars were compared. Three observers evaluated the scars at 3, 6, and 12 months postoperatively using a categorical and a modified visual analog scale. Results: The average time for closure using suture was 7 min and 45 s for the abdominoplasty and 4 min and 25 s for the vertical incision of the mammoplasty. This was significantly different statistically, as compared with the 2 min required for polymerization of the skin adhesive. The mammoplasty and abdominoplasty scars showed no statistical difference at 3, 6, and 12 months according to both scales. Conclusions: The esthetic aspects of the mammoplasty and abdominoplasty scars were similar on both sides at 3, 6, and 12 months. However, the adhesive allowed a shorter surgical time.
10.7 Bone Adhesives
One of the unmet clinical needs of orthopedic trauma surgeons is a ‘‘bone glue’’ or an adhesive to fix a broken bone instead of the conventional metal plates, nails, pins, and screws. Simplicity, quickness, and preservation of joint function, especially when fixing fractures with many small fragments, are the main benefits of a bone adhesive. An additional benefit is elimination of metal removal from fractures fixed solely with a biodegradable adhesive.
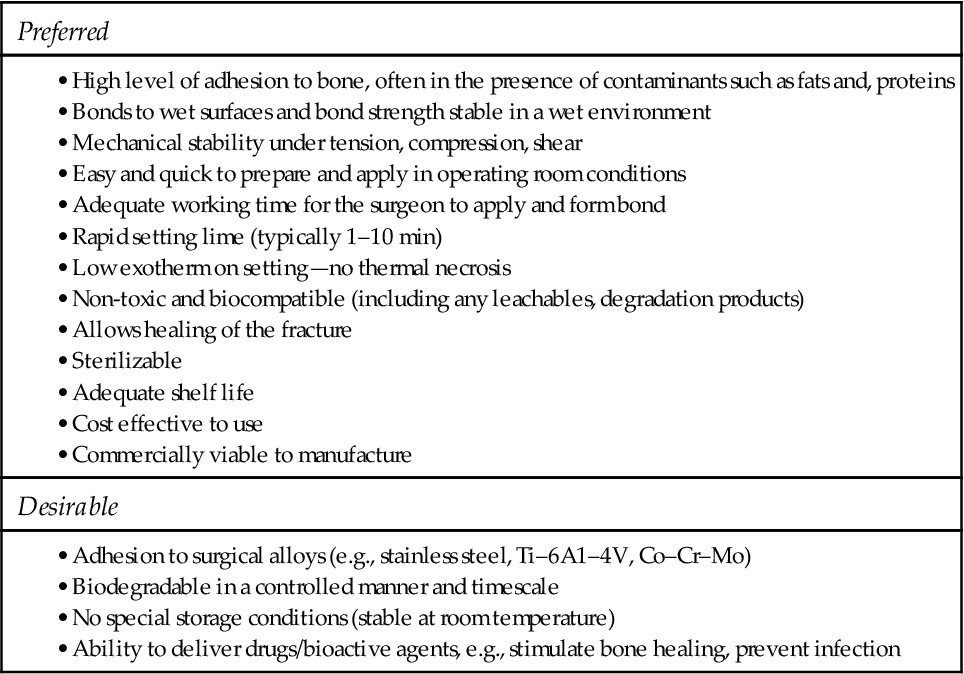
The development of bone adhesives has been underway since the 1950s. This is still in the relatively early stages in terms of not having resulted in adhesives which meet the many requirements of a successful product (Table 10.7). There are a number of bone cements and bone void fillers on the market though none claims any adhesive properties. Probably the best known of these products is PMMA bone cement that has long been used for the fixation of implants such as hip and knee replacements into bone. However, this material acts merely as a grout between the implant and bone and any attempts to use it to glue bones have generally been unsuccessful [98].
Table 10.7
Characteristics of a Successful Bone Adhesive [98]
10.8 Dental Applications of Adhesives [99]
Dental adhesives are basically intended to provide retention to composite fillings or composite cements. A good adhesive not only should withstand mechanical forces, particularly shrinkage stress from the lining composite, but should be able to prevent leakage along the restoration’s margins. Clinically, failure of restorations occurs more often due to inadequate sealing, with subsequent discoloration of the cavity margins, than due to loss of retention [100,101].
The effectiveness of dental adhesives is dependent on two factors. First, the adhesive must bond to enamel and dentin, and second, the adhesive adheres to the lining composite. The second factor has been shown to be due to a process of copolymerization of residual double bonds (![]() C
C![]() C
C![]() ) in the oxygen inhibition layer. Bonding to enamel and dentin is believed to be by micromechanical adhesion as the main adhesion mechanism [102]. This takes place through an exchange process where inorganic tooth material is replaced by resin monomers that become interlocked in the retentions after polymerization [103,104]. Diffusion and capillarity are the primary mechanisms of micro-mechanical retention. Microscopically, this process is called “hybridization” [105]. Comprised of simple interlocking resin in etch-pits in enamel, entanglement of resin within the exposed collagen lattice occurs in dentin. Self-etch adhesives with a mild (relatively high) pH do not, however, completely expose collagen. An additional mechanism of ionic bonding of acidic monomers and calcium in hydroxyapatite was established in 2004 [106] that might explain the successful clinical performance of some of these mild self-etch adhesives [107].
) in the oxygen inhibition layer. Bonding to enamel and dentin is believed to be by micromechanical adhesion as the main adhesion mechanism [102]. This takes place through an exchange process where inorganic tooth material is replaced by resin monomers that become interlocked in the retentions after polymerization [103,104]. Diffusion and capillarity are the primary mechanisms of micro-mechanical retention. Microscopically, this process is called “hybridization” [105]. Comprised of simple interlocking resin in etch-pits in enamel, entanglement of resin within the exposed collagen lattice occurs in dentin. Self-etch adhesives with a mild (relatively high) pH do not, however, completely expose collagen. An additional mechanism of ionic bonding of acidic monomers and calcium in hydroxyapatite was established in 2004 [106] that might explain the successful clinical performance of some of these mild self-etch adhesives [107].
Some of the requirements of adhesive systems can be defined [99] using the knowledge of bonding mechanisms. Micromechanical interlocking occurs after consecutive demineralization, resin infiltration, and polymer setting. Consequently, adequately removing the smear layer together with demineralizing enamel and dentin to a small extent, good wetting, diffusion, penetration, and good polymerization of the resin components are all important. Chemical bonding can be achieved by adding specific monomers with affinity for hydroxyapatite. Finally, sufficient copolymerization between the adhesive and the lining composite will provide good adhesion to the composite.
Chemical composition of adhesives should be (is) selectively defined [99] such that the above mechanistic requirements may successfully be fulfilled. Even though dental adhesives can be classified into two main groups, i.e., etch and rinse (E&Rs) and self-etch adhesives (SEAs) (Figure 10.4), they all contain similar ingredients, irrespective of the number of bottles of which an adhesive consists. Nevertheless, the proportional composition differs between the different classes of adhesives. Traditionally, adhesives contain acrylic resin monomers, organic solvents, initiators and inhibitors, and sometimes filler particles. It is obvious that every component has a specific function. Good insights in to the chemical properties of the adhesives’ components are paramount to understand or even predict their behavior. Table 10.8 gives a list of the various ingredients of dental adhesives.
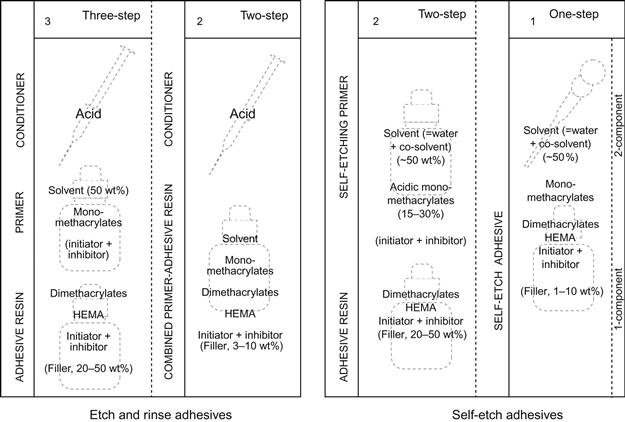
Table 10.8
Ingredients of Dental Adhesives [99]

Resin monomers in dental adhesives play a similar role to those of composites. Just as in the composites, the cured resin in the adhesive forms a matrix which functions as a backbone providing structural continuity and thus physico-mechanical properties such as strength. Monomers are the most essential ingredient of the adhesive because they are the key constituents of adhesives. There are two classes of monomers: cross-linking and functional monomers. Typically, the functional monomers only have one polymerizable group while cross-linking monomers have two or more polymerizable groups such as vinyl linkages (![]() C
C![]() C
C![]() ) [108]. Functional monomers, in addition to the polymerizable group, exhibit a particular chemical group which the functional species that embodies the monomer-specific functions imparted to the polymer.
) [108]. Functional monomers, in addition to the polymerizable group, exhibit a particular chemical group which the functional species that embodies the monomer-specific functions imparted to the polymer.
Functional monomers form linear polymers upon polymerization, contrary to the cross-linkers which supply the linkages for cross-linked polymers. Compared to linear polymers, the latter have proven to exhibit better mechanical strength, and cross-linking monomers are therefore important to the reinforcement of the adhesive resin [109–112]. Important characteristics of more common dental adhesive monomers are briefly covered in the followings sections [99].
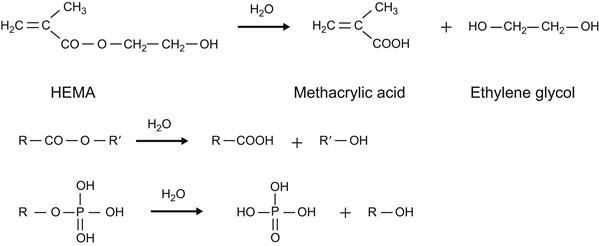
10.8.1 Methacrylic Acid
Methacrylic acid (MA) is a strong irritant and corrosive because of its strongly acidity. It can also rapidly penetrate gloves and skin, causing allergic reactions. This monomer is, therefore, seldom added to adhesives. It is, however, most likely to be present to different extents in the majority of adhesive resins, thanks to the hydrolysis of the ester group in other monomers as seen in Figure 10.5. Hydroxy ethyl methacrylate (HEMA) hydrolyzes and generates MA. Hydrolysis of methacrylate monomers is a problem associated with self-etching adhesives which routinely contain water and have fairly low pH, both of which result in easy hydrolysis [113].
10.8.2 Methyl Methacrylate
MMA, similar to MA, is one of the oldest monomers and is rarely sporadically added to adhesives because of the risk of allergic reactions [114]. It is no longer used for cosmetic applications because of a ban. Its role in adhesives is limited to dissolution of other monomers.
10.8.3 Hydroxy Ethyl Methacrylate
HEMA is a small monomer with widespread use, not only in dentistry but also in medical applications because of its relatively good biocompatibility [115] even though the uncured monomer is notorious for its high allergenic potential [116,117]. Unpolymerized HEMA appears as a fluid that is quite soluble in water, ethanol, and acetone. HEMA is purported to evaporate from adhesive solutions, although only in small amounts [118]. A key characteristic of HEMA is its hydrophilicity. Even though this monomer cannot be used as a demineralizing agent, its hydrophilicity makes it an excellent adhesion-promoting monomer [119–123]. By enhancing wetting of dentin, HEMA significantly improves bond strengths [124,125]. In monomeric and polymerized states, HEMA will readily absorb water. Water uptake adversely influences the mechanical strength of the HEMA copolymers; high amounts of HEMA will result in flexible copolymers with inferior qualities. The homopolymer of HEMA is a flexible porous polymer [126,127]. As such, high concentrations of HEMA in an adhesive may have deteriorative effects on the mechanical properties of the resulting polymer.
10.8.4 4-Methacryloyloxyethyl Trimellitic Acid
4-Methacryloyloxyethyl trimellitic acid (4-MET) is used both as an adhesion promoter and demineralizing monomer [128,129]. 4-MET is known to improve wetting to metals, such as amalgam [130] or gold [131]. Its popularity is partially due to its easy synthesizing method and broad availability. 4-MET is available in anhydride form (4-META), which is a crystalline powder. After addition of water to 4-META powder, hydrolysis occurs rapidly with 4-MET being formed. The two carboxylic groups bonded to the aromatic ring increase acidity and thus demineralizing properties as well as wetting. The aromatic group, however, is hydrophobic and will moderate the acidity and the hydrophilicity of the carboxyl groups [77].
10.8.5 4-Acryloyloxyethyl Trimellitate Anhydride
The structure of 4-acryloyloxyethyl trimellitate anhydride (4-AETA) differs from that of 4-META slightly, having an acrylate polymerizable group instead of a methacrylate group. The acrylate group is regarded as an advantage for polymerization because of higher reactivity [132]. Apart from facilitating resin penetration into dentin, the highly reactive acrylate group of 4-AETA is regarded as an advantage for better polymerization.
10.8.6 10-Methacryloyloxydecyl Dihydrogen Phosphate
10-Methacryloyloxydecyl dihydrogen phosphate (10-MDP) is a monomer that was originally synthesized by Kuraray (Osaka, Japan). Its main use is as an etching monomer, due to the dihydrogen phosphate group, which can dissociate in water to form two protons [113]. Structurally, the long carbonyl chain renders this monomer quite hydrophobic. Consequently, ethanol and acetone are most suitable solvents for this monomer. It is clear that 10-MDP is relatively hydrolysis stable. Yoshida et al. [106] demonstrated this monomer is capable of forming strong ionic bonds with calcium because of the low dissolution rate of its Ca salt in its own solution.
10.8.7 Other Monomers
These monomers include 11-methacryloyloxy-1,10-undecanedicarboxylic acid (MAC-10). This monomer is hydrophobic, which may reflect in limited dissolution in water. Another compound is 2-(methacryloyloxyethyl) phenyl hydrogen phosphate (phenyl-P) [133,134] which was used as one of the first acidic monomers in self-etching primers. It seldom finds contemporary use. Two other monomers are phosphates: di-2-hydroxyethyl methacryl hydrogen phosphate (di-HEMA-phosphate) and 2-hydroxyethyl methacryl dihydrogen phosphate (HEMA-phosphate) [135]. Dimethacrylates are cross-linking agents, and methacrylamide is an interesting matrix monomer because of its similarity to amino acids of which collagen consists [136], thus promoting the formation of hydrogen bonds between the carboxyl and amide groups of the monomer with the carboxyl groups of collagen.