2
Neurorehabilitation Robots Review: Towards a Mechanized Process for Upper Limb
Yogini Dilip Borole*1 and Roshani Raut2
1Department of E&TC, G H Raisoni Institute of Engineering and Technology, SPPU, Pune University, Pune, India
2Department of Information Technology, Pimpari Chinchwad College of Engineering, SPPU, Pune University, Pune, India
Abstract
Restoration Robotics gives a presentation and outline of all zones of recovery mechanical technology, ideal for anybody new to the field. It likewise sums up accessible robot advancements and their application to various pathologies for talented scientists and clinicians. A few business gadgets for mechanical recovery have empowered to build up the ability and skill important to manage those looking for complete comprehension of the point. The usage of productive robot methodologies encourages the re-securing of engine abilities. This innovation fuses the results of social examinations on engine learning, and its neural relates into the plan, execution, and approval of robot specialists that act as “ideal” coaches, effectively abusing the construction and versatility of the human sensorimotor frameworks. In this specific situation, human–robot cooperation assumes a principal part, at both the physical and intellectual levels, toward accomplishing an advantageous connection where the human body and the robot can profit by one another’s elements.
Keywords: Exoskeleton, electromyograph, rehabilitation robots, stroke
2.1 Introduction
The proportion of adolescent patients with functional impairment of the upper appendages brought on by stroke has increased rapidly, as influenced by the speed of life, unhealthy lifestyle, and environmental factors [1, 2]. The issue of appendix development, brought on by hemiplegia after a stroke, not only reduces patient satisfaction but also carries excruciating pain in education and scientific expertise. Strong restorative adjustment can improve patients’ sensory function and maintain a level of joint action, and prevents reunion and improves patients’ “final recovery rate.”
The engine operates basically [3]. The most common remedy for recovery is moderate exercise of patients by a specialist. This strategy is difficult to build a compulsory treatment plan and is largely well managed [4]. With the advancement of robotic rehabilitation and drug rehabilitation, the regenerative robot has become a new therapeutic sensory therapy. It is very important to abuse the introduction of robots in order to recover the supplemental dose of patients with stroke [5]. Common treatment strategies, based on expert clinical knowledge, have problems with high staff utilization, long recovery cycles, side effects of restricted boundaries, etc. for the successful rehabilitation of clinical assets, and to improve personal satisfaction of patients with stroke [6, 7]. The advanced add-on robot can be divided into two types according to the original design: the last foot and the type of exoskeleton. The latter type actually provides a return that prepares for flight development. In addition, the exoskeleton type expands the range of retrieval adjustments from the plane to the third-dimensional (3D) space, which can help the affected appendix to complete the adjusted restoration in 3D space. The exoskeleton retrieval robot for the most part conducts the development of patient placement with the aid gadget (otherwise called the mechanical exoskeleton structure). The design of the auxiliary gadget is similar to the bone structure of a human implant. During the preparation, the patient appendages and comparing parts of the assistant gadget are merged together, and the merger bar of the auxiliary gadget rotates the associated member in order to deliver moving additions. It can make the appendages be trained especially in a variety of situations by controlling the gadget’s auxiliary power indicators. Currently, the basic strategy of the exoskeleton robot repositioning model is one of the hottest problems in robotic retrieval tests. Contributing to the construction of various equipment and recovery levels, various land reclamation robots are developed, e.g., unique exoskeleton ADEN-7 robot with 7 degrees [8], ARMIN robot with six levels of chance (four dynamic and two active) semi-exoskeleton structure [9], an ARMEO robot that provides arm weight depletion network that supports emotional preparation, enhancement of installation, and test instruments [10], etc. In addition, the air muscles are used as a pilot to receive four levels of stimulus potential for the RUPERT movement robot [11], a LIMPACT water-based robot [12], and a CAREX cord-based robot [13]. Since then, scientists have recreated and designed a superficial regenerative robot based on pneumatic muscle drive [2], a superficial regenerative retrieval robot, an over-the-top rescue robot, and a half-drive and under the upper exoskeleton drive retrieval robot [14–22]. The reciprocal robot takes care of the problem of controlling the adequacy of movement and the summary of each human body during the recovery time spent repairing and overcomes the burden of ultimately redirecting recovered robot, which can only make basic adjustment (direct or circular movement) enough for minimal movement. Currently a protected and productive robotic retrieval building available for different applications. In any case, in the system of exoskeleton prostheses, the integration of mechanical joint movement pivot and human joint movement hub is important. The exoskeleton produces a surprising effect on the patient’s joint under a deformed condition, which not only promotes pain associated with the patient’s injury but also further prevents the developmental space of the patient’s placement, and reduces the impact of prepared recovery. In line with these lines, the pivot of each travel pair is directed and focused on the reversal of each joint of the human body in the same way as can be considered in the external regenerative device system. The movement of each integration of the foreign exchange gadget is basically accepted by modifying or moving the couple, and obtained positive results [23, 24]. Compared with non-invasive treatment, the robotic rehabilitation framework has the advantages of high preparation, easy-to-measure performance measurement, and long-term systematic treatment of patient rehabilitation.
To meet the need for rehabilitation of patients with augmentation [21, 25] problem, a robotic over-the-counter replacement robot is being developed, primarily a powerful recovery and rehabilitation gadget for patients with stroke. The basic renewal process is shown in Figure 2.1.
Because of the understanding of common rehabilitation barriers and displays of regenerative robots, combined with the upper body appendage of vital signs structures and parameters, we determine the arm development for each integrated range from all bones and upper limbs to improve extension features; this document proposes a robotic regenerative robot design system. It is an over-the-top acquisition robot used for therapeutic restorative therapy for hemiplegic supplementation to maintain the range of motion of the appendix, prevent muscle degeneration of the appendix, improve system muscle strength, and promote functional recovery. As a result, it can provide a powerful recovery gear for patients with high appendage hemiplegia brought on by stroke [31, 47].
In this article, due to the investigation of life structures, the movement of metal, and the range of motion of the upper human appendix, the movement area of each joint is determined by the human arm, and part of the machine all levels designed. First, set the location link between each moving part and the ultimate high return robot wear; then model the navigation system set up on the Denavit-Hartenberg (DH) boundary plan, and the movement space is set up for an advanced wearable high-speed acquisition robot. The kinematics test is used to disperse the movement of the over-the-top wearable robot. Alternatively, to check if the return robot designed for top wear is able to understand the top assistant adjustable adjustment, working space is allocated to an over-the-counter wearable robot. Third, to investigate the harvesting potential of a more advanced retrieval robot, a powerful simulation of the robot has been completed. In conclusion, it is planned to control the robots for the acquisition of high-quality wearable, which received the following results of the adjustment of the robotic reversal.
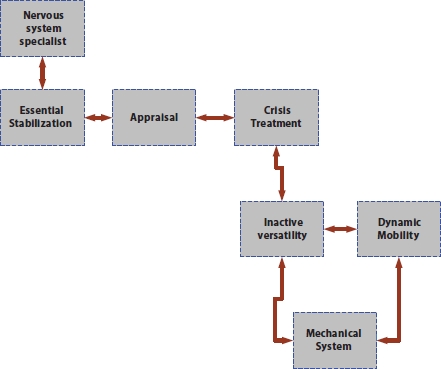
Figure 2.1 Basic rehabilitation process.
It also ensures the ingenuity of the return robot design for high wear. The main commitments for this article are summarized as follows:
- (1) Due to the speculative health features, partial movements, and scope of additional human appendages, a retrieval robot mounted with a pressure gauge is located directly on the fixed bat, then re-examined, interrupted by the above appendix depending on the patient relying on flexible transmission during recovery to prepare the scale. A joint operated by specially designed joints intended for the elbow/wrist and shoulder joint is driven by a dental band. All engines connected to the link have been reversed to achieve greater distance transmission and reduce driving delays for the last members. The material belt is rigged to drive the members of the return robot designed for high wear, which authorizes high balance.
- The design of an obsolete durable adhesive robot promotes the restoration of integration, adequately reduces the volume, weight, and delay of the actuators, and achieves a lightweight design of the standard design.
- (2) In addition, the paper proposes a parallel design for the wrist-operated. With a rope and kept in a spring pressure. With a rope and kept in a spring pressure, the fixed base and the moving base of the additional decorative return robot are connected to the three wires and the spring pressure involved. The fixed base and the moving base of the additional decorative return robot are connected to the three wires and the spring pressure involved. The springs are designed to mimic the human wrist and support the versatile section to complete the growth of the wrist, while the wires are formed by regenerating the wrist muscles to control the wearable retrieval robot. In this paper, the system approach will contribute to the ongoing investigation of equal instruments with flexible members. The results will play an important role in reversing the development of the human wrist and further in improving the retrieval robot, the cord that creates the drive.
- (3) The kinematics and performance of the retrieval robot designed for high wear are also confirmed, decreasing according to the DH plan and the Monte Carlo process. It shows that a removable retrieval robot that can be worn can meet recovery needs by preparing for kinematics/ element investigations as well as prepared tests. In this way, it also looks at the availability and adequacy of the planning strategy, which provides an important strategy for improving the robot recovery tool.
2.2 Recovery and the Robotics
The accompanying issues have consistently existed in recovery [1]:
- • Operational and useful redesign from a cerebral perspective and engine recuperation appear to require treatments that require a significant utilization of the appendage related with an imaginative kind of learning as well as capacity concerning new engine abilities.
- • Based on the past thought, it is apparent that straightforward developments do not lead to greatest recuperation of the restored appendage.
- • Based on the primary thought, it is additionally certain that even the utilization of uninvolved activities does not prompt ideal recuperation of the influenced appendage.
Thus, the thinking prompted the beginning and the first utilization of mechanical technology as commonsense and viable restoration devices [2, 3] in light of the fact that they can permit organization of recovery treatments that include:
- 1. Rousing and drawing in recovery work out.
- 2. Preparing that both upgrades and amplifies the usefulness of the appendage.
- 3. A climate brimming with rousing improvements.
Recovery upheld by the utilization of automated frameworks can have various points of interest [4]. Specifically, it permits more escalation and is custom-fitted to the patient recovery exercises and administrations (expanding the sum and nature of treatment that can be regulated); what’s more, it permits all the elaborate entertainers in the group (e.g., physiotherapists, doctors, bioengineers, and different figures) to set and deal with some work boundaries to make the recovery explicit and ideal for the patient (the kind of activity, the degree of help from the robot, the power and the kinematic that the patient should apply, following the exercise).
2.2.1 Automated Technological Tools Used in Rehabilitation
There are two distinct sorts of mechanical innovative instrument (RTT) in restoration for both the lower and upper appendages. The first depends on exoskeletal instruments. The second is of the end-effector type.
2.2.1.1 Exoskeletal-Type RTT
The exoskeletal robot, regardless of whether it is for the lower [5] or upper appendages [6], totally covers the appendage, following and imitating its anthropometric attributes and hence managing each portion associated with the recovery practice. The exoskeletons are frameworks with a combination of mechanical and electronic segments that comprise a mechatronic mechanical assembly that is worn and that plays out a similar sort of kinematic/dynamic action rehearsed by the patient who wears it. These frameworks cover the influenced appendage, or if nothing else the piece of the appendage influenced by the clinical viewpoints from a restoration perspective. In these frameworks, the quantity of levels of opportunity is equivalent to that of the joints on which the restoration treatment should mediate depending on the targets. As to recovery of the lower appendages [4], we allude to class 1 exoskeletal frameworks regarding nonportable mechanical frameworks. Class 1 has a place with those nonportable automated frameworks comprising of a mechanical exoskeleton. At times, there is likewise a body weight uphold (BWS) [4] type framework circulated over the entire body for weight alleviation, a transport line, and a control data framework including biofeedback reaction frameworks dependent on augmented experience. These frameworks are normally utilized uniquely in the facility and halfway establish a development of unadulterated BWS frameworks. We explicitly allude to Class 2 exoskeletal frameworks with explicit reference to versatile frameworks that can likewise be utilized remotely to the restoration clinical climate.
2.2.1.2 End-Effector-Type RTT
In a mechanical end-effector gadget, the contribution for completing the restoration work out comes straightforwardly from the distal piece of the appendage, permitting the characteristic kinematic initiation of the development without unnatural requirements. These frameworks are utilized for both lower [7] and also upper appendage [8, 9] restoration. The robot with the end-effector interconnects to the appendage in a solitary point, for the most part a handle or a grasp point for the restoration of the upper appendage or a pedal-like apparatus for the restoration of the lower appendages. As regard the restoration of the upper appendages regarding end-effector frameworks, now and again we talk about Cartesian frameworks because of certain imperatives that can be forced in the directions additionally joined with explicit activities (likewise gamified) given by programming.
2.2.2 Benefits of the RTTs
Both the two RTTs produce persistent advantages [4–9]. It is currently grounded that for the lower appendages, the RTT produces different advantages, counting:
Improved trunk control.
Improvement of the rest wake cadence and decrease of apparent weariness in conveying our everyday life exercises.
Pain alleviation.
Improvement in the condition of emotional well-being.
Improvement of general anthropometric attributes (decrease of fat mass, increment of lean mass).
Improvement of intestinal and bladder work.
A portion of these advantages are additionally gotten because of the blending with explicit programming additionally dependent on computergenerated simulation (VR) as well as enlarged reality (AR), and furthermore in characterized secured vivid virtual conditions where the recovery situations called Cave Programmed Virtual Environment (better known with the abbreviation CAVE) occur.
It is presently grounded that for the upper appendages, the utilization of an RTT shows a few benefits, including:
- • Neuromata improvement of appendage work.
- • Pain alleviation.
- • Improvement in the condition of psychological well-being
- • Improvement of general anthropometric attributes (decrease of fat mass, increment of lean mass).
- • Improvement of psychological capacities.
A portion of these advantages are additionally acquired thanks to blending with explicit programming that, for the most part, offers spurring GAME and as of late, at times, is likewise dependent on computer-generated reality or potentially enlarged reality.
2.3 New Directions to Explore and Open Problems: Aims of the Editorial
2.3.1 New Directions of Research and Development and First Aim of the Editorial
As of now, advanced mechanics for recovery are pushing a great deal of innovative work; what’s more, various new fascinating headings are opening both straightforwardly associated with the automated apparatuses referenced above and on the side of a considerably more extensive restoration measure.
A portion of these headings that all the more straightforwardly relate with movement recovery [4, 10, 11] are:
- 1. To evaluate the impacts of utilizing robots at various periods of recuperation.
- 2. To create wearable robots simple and viable to wear and eliminate.
- 3. To diminish the expenses likewise by methods for new models of care.
- 4. To improve and reevaluate the models of care dependent on advanced mechanics.
- 5. To engage the cooperative energy and coordinated effort between experts of the recovery group and architects through shared and appropriately planned undertakings.
- 6. To make computer-generated reality, expanded reality, at home advancements, exoskeleton, and counterfeit insight accessible for the treatment of psychological as well as degenerative conditions.
Different bearings, more engaged to mental help, in a more extensive way to deal with recovery measure are the accompanying [12]:
- 1. To put resources into social robots explicitly intended to help during the recovery stages (concerning model being taken care of by the older).
- 2. To put resources into social robots explicitly planned as social middle people to help during correspondence/treatment movement (as being taken care of by the chemical imbalance).
- 3. To deal with the issue of the sympathy in mechanical technology particularly according to communication with the social robots. Considering the abovementioned, the publication intends to invigorate researchers to report their encounters identifying with different parts of advancement on the turn of events and utilization of mechanical technology in recovery both from a mechanical and clinical perspective.
2.3.2 Open Problems and Second Aim of the Editorial
In spite of the incredible improvement of advanced mechanics in the restoration field, we are helping to a few unique methodologies in the utilization and in the pertinent models of care. For instance, both the recovery treatments and the results in the global display are frequently evaluated in an alternate manner. As in different areas, for example, telemedicine, mechanical technology is regularly utilized exceptionally restricted to direct as well as examination projects. Much the same as in telemedicine, all angles that can fortify the utilization of mechanical technology in routine clinical exercises should be tended to in the global display with solid committed activities. Through this methodology, restoration advanced mechanics will actually want to be important for the arrangement of proposed medical care offers in each state with an unmistakable repayment of the demonstrated administrations. Considering the abovementioned, the article points likewise to animate researchers to report their encounters identified with these different parts of the utilization of mechanical advances utilized in the recovery habitats and research facilities. From this assortment acquired with heterogeneous strategies, which probably will go from the audit to the mass overview, we hope to have significant reactions and boosts for the global academic local area.
2.4 Overview
As the findings regarding the Global Activity on Neurology and Public Health developed by the World Health Organization, a large number of vascular disorders continue and are reversible, contain a global medical issue [1], and have a particular impact on individual adults. Also, a high future makes society of more than 60 people progressively higher [2]. Persistent gatherings for rehabilitation administrators in the Commonwealth are designed for neurological disorders, as outlined in the general view [3]. 70% of respondents provided recovery management for people with stroke, multiple sclerosis, severe cerebrum injury, neurological disorders, and, in addition, other neuromuscular conditions. The different treatments mentioned were those that provided recovery for people with a single brain injury (10%), spinal cord injury (9%), amputees (5%), muscle paralysis (4%), learning disabilities (1%), and suffering (1%). In Spain, a similar situation appears where muscle and bone failure (half), neurological disorders (15%), severe injuries (29%), and others (6%) are treated in the management of recovery [4]. The current situation, along with the need for further recovery, assistance for people with disabilities, means that automatic care and rehabilitation can play a significant role in the long run. Nowadays, research on the use of automated frameworks in various fields identified by healthcare is extensive [5–7].
In the field of recovery, logical writing demonstrates the different order of such structures as indicated by their level of communication [8], the most important points treated [9–12], the release of rescue robots [13, 14], control strategies [15, 16], and therapeutic efficacy [17–20]. In any case, no experiments were performed on the method of appropriate recovery, and the commitment of mechanical technology to the various stages of the recovery or communication cycle was not examined. In this article, an efficient writing survey is directed to distinguish the commitment of mechanical technology for upper appendage neuro rehabilitation featuring its connection with the restoration cycle and to explain the planned examination headings in the advancement of a self-sufficient recovery measure.
2.5 Renewal Process
A World Disability Report by WHO and the World Bank [21] provides the definition of recovery: “a number of measures that help people who experience, or are likely to experience, inability to achieve and continue to function effectively in communication with their surroundings.” in various definitions in a world characterized by social diversity. UMeyer et al. [22] provided the calculated visual recovery:
“The social process is based on the WHO integration model of performance, inefficiency and efficiency, with the aim of empowering people with medical problems they experience or tend to cope with inability to achieve and maintain good co-operation with the climate” of the patient’s well-being throughout the recovery cycle. These interactions include tangible evidence of human problems and needs, related to issues in human priorities and climate, setting goals for recovery, planning and action, and impact assessments [21]. This approach is called the recovery cycle (see Figure 2.1), adapted from the World Report on Disability [21], and recently developed by Stucki and Sangha [23] and modified by Steiner et al. [24].
By the way it works, the recovery cycle consists of four steps: testing, operation, mediation, and testing. The interaction occurs at two levels: the first is about the direction given by the continuation of care, and the second is about the provision of specific care [25]. From a practical point of view, the test program contains an ID of individual issues and needs, an investigation of the ability to rescue and guess, a description of the assistance provided, and the objectives of the plea program. Work refers to the placement of a person in the most appropriate intercession assistance program in treating their needs. From the direction of the guide, no decisions appear on the roll. Assessment refers to the help and accomplishment of the purpose of intercession. From the point of view of providing specific assistance, the assessment includes tangible evidence of issues, audits, and expected changes in assistance or mediation program objectives, a description of the main objectives of the recovery cycle, and objectives to address. The action phase refers to the professional side, and social advocacy is essential to achieving the goals of mediation. Dependence includes the determination of methods, measures, and a description of the target measures to be achieved within a predetermined timeframe. Ultimately, testing determines spatial achievements related to specific symptoms, recovery cycle objectives, and, finally, the goals of the mediation program. It also includes selections in relation to the requirement for another mediation cycle based on other tests.
2.5.1 Renovation Team
Rehabilitation requires the management of many medical care providers with novel skills, preparation, and skills that are used to fully restore patients’ strengths and their positive recovery in all areas of life [26]. Rehabilitation experts have chosen the concept of “continuous focused treatment.” This is not intended to alleviate the needs of the patient but rather to strengthen the patient as the head and judge of the mediation as indicated by the wishes implanted by the patient [27]. The inclusion of different clinical approaches can be done with three functional models [26, 28]: (a) a multigroup model—in which colleagues interact and transmit between them, knowing that they are composed of all components and provide testing and equal but free operation; (b) a multisectoral group model—in which group members share a common source of information (intended to encourage the advancement of nonfiction), and selections are made in one or a few general circuits (hence, drugs developed by independent experts); and (c) a multidisciplinary team model—not only promoting communication within the group but also gaining information from other related scholars and joining them in training [29]. Since the segmentation model is specific to promote early communication, it is extremely appropriate for retrieval groups [28].
2.5.2 Renewal Methods and Results
Recovery techniques are a myriad of recovery activities that reflect more physical strength, structure, exercise and coordination, natural flexibility, and other factors. The effects of restorative benefits and changes in human performance over the long term cannot be measured by a single measure or set of measures [30]. These results can be tested in three terms measurements of the Worldwide Classification of Functioning, Disability and Wellbeing (ICF) [31]: body capacities and designs, exercises, and, furthermore, interest.
2.6 Neurological Rehabilitation
One example of recovery points to the treatment of neurological problems that affect the nervous system and the neuromuscular system, known as neuro regeneration. These types of problems can bring about mental or physical disability or recurrence of both and persist or may change again. Rehabilitation can be seen as a cycle that aims to improve one’s social cohesion in the public eye and a sense of prosperity. This description includes a few highlights: recovery is by no means a form of mediation; emphasis is placed on the patient himself; objectives indicate social functioning, as well as welfare or prosperity; and nothing but a closed cycle in patients who can recover, especially or completely, but applies to all remaining patients with long-term withdrawal problems [32]. This will be followed by shortages, travel limits, and investment restrictions, which include a comprehensive approach to assistance [33].
The complexity of the issues brought on by traumatic brain injury underscores the need for a team working on its own treatment, a model of the most widely used multidisciplinary framework [34]. The organization of a multifaceted group in the renewal of the neuro is not entirely clear, but there is agreement on the key people who should be in the group. According to the Union of European Clinical Specialists (UEMS), the multidisciplinary team must include complementary medical professionals: real-time specialists, returning paramedics, rehabilitation doctors, terminology counselors, speech therapists, therapists, social workers, muscle therapists, and specialists diet [35].
The recovery cycle that appears in Figure 2.2 works in the case of the emotional recovery of some of the underlying substances examined below.
2.6.1 Evaluation
The recovery interaction begins with gathering information from the patient and others to set up the issues; the reasons for, and factors affecting, every issue; and, furthermore, the desires and assumptions for every invested individual. It is also important to consider expectations that depend on analysis, general history, broadcast, and autonomy and the nature of impedance, as well as other individual, social, and environmental factors [36].

Figure 2.2 Restoration cycle.
To date, the development of targeted scales has been developed to assess the level of freedom of patients. Three basic ICF sites can be used at this point as a clinical device [37, 38].
- (i) Disability: The general physical functions that need to be assessed in a neurosurgeon are those identified by genetic makeup, muscle, development, and hearing and cognitive ability.
After that, the few most important growths are muscle, developmental size, concentration, memory, and balance.
There are traditional scales included at this level similar to the Beck Depression Inventory, Behavioral Disruption Test, Canadian Neurological Scale, Clock Drawing Test, French Aphasia Test, Fugl-Meyer Trial Recovery after Stroke, General Health Questionnaire-28, Geriatric Depression Scale and Despondency Anxiety Scale, Mini-Mental State Examination, Altered Ashworth Scale, Montreal Visual Comprehension Test, Invisible Visual Vision Test, Community Health Center Stroke Scale, and Orrington Prognostic Scale.
- (ii) Function: while evaluating a patient’s exercise, the specialist will check whether they are competent as it was the assignment yet and the quality with which it is performed. According to a study by Lennon [39], one of the most widely used scales in the recovery process was the Barthel Index, followed by the Rivermead Motor Assessment and Useful Independence Measuring. More than a quarter of counselors (28%) used the results tools they were pregnant with, which could not be tested for static quality or legitimacy. The various types of scales at this level are: Test Action Test, Berg Balance Scale, Box and Square Test, Chedoke-McMaster Stroke Assessment Scale, Variety of Clinical Outcomes, Active Activity Phases, Country Renewal Revealing System, Frenchay Activities Index, Modified Rankin Handicap Scale, Motor Assessment Scale, Nine-Hole Peg Test, Rivermead Mobility File, Timed “Up and Go” Test, and the Wolf Motor Capacity Test.
- (iii) Participation: this is a more complex concept than the challenges and exercise, but it is the key in understanding patients and their health and helping to plan treatment. Collaborative physiotherapy testing thus focuses on exercise or activities and when patients participate in them, patients are excluded, and patients wish to cut more than that, which can be improved and will definitely be weakened. The standard scales used are the following:
Canadian Performance Measure, EuroQol Quality of Life Scale, London Handicap Scale, Medical Results Short Form 36, Nottingham Health Profile, General Health Index Recovery, Stroke Impact Scale Profile, Stroke Impact Scale, and Stroke Specific Quality of Life Scale.
2.6.2 Treatment Planning
As indicated by the pathology, the rescue team plans specific arrangements based on the conclusion (issuing ID) and the patient’s inability. It is important to note the clear terms identified for usage issues. Restoration purposes often follow SMART standard as it should be clear, measurable, feasible, efficient, and time-limited [32]. There are three key areas in which restorative communication is divided: (1) it moves towards that disability reduction; (2) methods aimed at acquiring new skills and programs, which will enhance action; and (3) is approaching that assistance to address the climate, physical, and social, and therefore inefficiency transmits a series of minor setbacks. The design of a sensory recovery program should take into account the previous three approaches, including SMART level.
2.6.3 Mediation
Specific Methods. Explicit restoration mediations incorporate those identified with actual medication, word-related treatment, discourse and language treatment, dysphagia, the executives, neurophysiological mediations, mental evaluation and intercessions, healthful treatment, and, furthermore, different intercessions [25]. A wide scope of explicit methods is utilized in the act of recovery [40]. These strategies are used to treat various patients who differ extensively across various topographical areas.
As of now, the proof recommends that to be powerful, restoration requires the act of exercises in the most important potential conditions, as opposed to undertaking logical activities pointed toward changing weaknesses [41]. This is once in a while alluded to as assignment that is explicit to the preparation. Notwithstanding, different methodologies are referred to like help procedures (like Bobath idea, Brunnstrom strategy, Kabat strategy, or Rood strategy), present-day procedures (such as treadmill preparing with body weight uphold, requirement induced development treatment, or useful electrical incitement), or, on the other hand, remuneration procedures.
2.6.4 Assessment
In this stage, the state of being of the tolerant is reconsidered to decide the adequacy of the treatment, in view of the SMART goals [32] at first raised. The contemplations for release on account of the neurological patient are extremely differed, since the clinician should decide if the improvement accomplished is adequate from the clinical perspective of the patient (patient-centered practice). Past quantitative examinations and contextual analyses have shown that the utilization of patient-focused objective arranged with grown-ups going through neurological restoration can improve self-saw and noticed objective execution and fulfillment [42]. A patient-focused methodology includes objectives that are set by the patients based on their own definition of the issues. This methodology empowers a more noteworthy self-determination; what’s more, it controls and upgrades the individual’s latent capacity for dynamic investment.
Furthermore, one should consider the basic obsessive cycle, the constant idea of specific pathologies, the requirement for oversight as well as the congruity in the nonappearance of an expressive up close and personal restoration treatment, or, on the other hand, the degenerative and reformist character of a few neurological pathologies [44, 45], like Parkinson’s illness, different sclerosis, or Alzheimer’s illness.
2.7 State-of-the-Art Healthcare Equipment
2.7.1 Neuro Renewal of Upper Limb
In this phase, this test will include parts of the recovery cycle used to regenerate the high neuro appendage created with the help of any type of repair framework. The robot system for the upper limb regeneration is shown in Figure 2.3.
2.7.1.1 Things and Method
2.7.1.1.1 Methods of Search
The creators welcomed the October 2017 writing review on the discovery of high-resolution neurotransmitter robots using visual terms such as robot, emotions, recovery, high, augmentation, point of resilience, arm, hand, neuro regeneration, mediation, medical aid, treatment program, and different combinations. The data sets were from Brain, Science Direct, PubMed/Medline, and IEEE. Only papers written in English were considered to the pursuit that stretches all the details of the information. Studies are included for the following reasons: (1) high-quality (direct) add-on frames; (2) frames depend on the end user and exoskeleton gadgets (economically available or not); (3) clinical communication was led; and (4) the effects of robotic-assisted treatment were evaluated.
2.7.2 Advanced Equipment for Neuro Revival of the Upper Limb
In line with the Strategic Research Agenda for Robotics in Europe [43], medical services are considered to be a combination of three domains: (1) high-quality clinical equipment—care support structures (determination) and remedial measures (medical procedure); (2) recovery—which includes postoperative care or post-traumatic stress disorder where direct contact with the robot’s frame will promote recovery or continue as a exchange of lost energy; and (3) assistive technology—incorporating various components of operational technology within the range of medical care where the essential capacity of the service delivery framework is either to provide assistive care or services or directly to patients in a medical clinic or specialist research office.
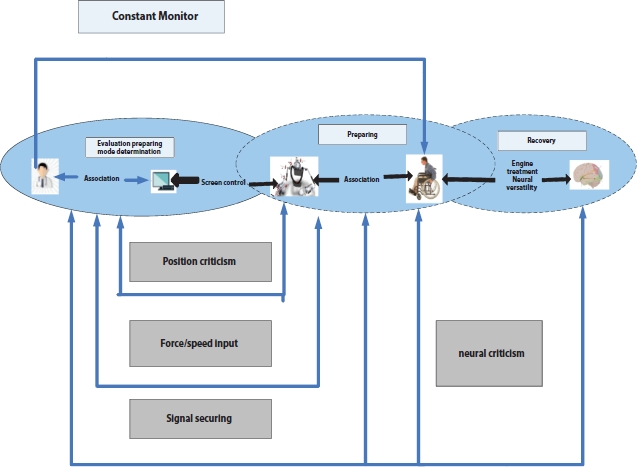
Figure 2.3 Robot system: upper limb rehabilitation.
In this way, gadgets [61–70] that need to be prepared (robotic-assisted treatments), supportive (exoskeletons), or implanted (prosthesis) disability tests or, on the other hand, impaired physical strength and construction are limited to restoring high-quality equipment. Therefore, robots are included as an important tool in the recovery cycle in neurological therapy.
Such structures are effective and help the professional to perform a high recovery rate. However, it is unclear how long the default entities provide this assistance in the recovery cycle. To improve the type of assistance provided, it should be divided into how the guide is administered and when.
2.7.2.1 Methods of Testing
As recently shown, the first and final part of the recovery cycle is an active test. It is important to note that most of the tests performed by mechanical components are not functional tests (indicated on the bench and in the follow-up treatment categories), and their results provided indications for patient presentation. Currently, useful tests are performed with custom tests and scales given by experts. The basic highlights of the robotic-assisted study framework relating to the experimental cycle are as follows:
(1) Test Mode. Patient demonstration tests can be completed in two ways: scheduled or nonscheduled. Scheduled mode compares the online information test, that is, during the turn of events or at the end of a meeting. In fact, the nondefault mode compares to a broken information investigation (after the end of the meeting). Progress data are available for the entire work group, as indicated by the segmentation model. Data management is one of the boring activities that promote the flexibility of the consultant. As of now, there are a number of systems for the electronic clinical recording (EMR) system for patient information management [46], including by looking at man-made assumptions [47]. After all, one of the useful features integrated into the robotic aided structures is the organization, and the power of knowledge as a result allows for years of renewable energy reports.
The results of the study show that an additional 45% of entities (business) offer some form of assistance in expanding treatment. The most popular help is by offering a wide range of activities, games (REOGO, DIEGO, and ARMEO), or medical meetings (INMOTION framework) that can be developed or coordinated by a consultant. The other framework (REHAROB) similarly allows for the selection of practices based on the most commonly used coping strategies in real recovery, such as the Bobath or Kabat strategy. Then again, the internal and external investigation of the record-based treatment of robotic aids, as it allows for rapid deployment testing, fills in as a selection aid tool to determine patient discharge. The INMOTION [71–80] framework allows the release sites to be built based on a five-test exhibition that registers kinematics knowledge and energy knowledge. To the creators’ information, there are no business frameworks ready to naturally produce a total recovery procedure from the underlying practical evaluation information, and along these lines, the advisor actually needs to appropriately distinguish the patient’s issues by methods for a dependable analysis and the correct decision of clinical measures to assess the adequacy of the treatment.
2.7.2.2 Renewal Methods and Results
Normally, rehabilitation takes place over a period of time but may involve one or more individual interventions delivered by a person or, on the other hand, a team of rehabilitation staff and may be required from a strong or early stage immediately following admission of illness in post-acute condition and final stages. Recovery reduces the effect of a wide range of diseases. In addition, neuro regeneration often relies on expert control, competing between different ways of thinking and exposing the greatest risk to what the neuro regenerative robot should do [48].
The robotic aided structures allow for the repair of a disabled appendage in many assemblies and effectively, without loss of functionality. In the case of a targeted treatment district, the number of members in the appropriate treatment unit has been indicated. No gadgets covering the construction of all the upper appendage members were found, i.e., shoulder, elbow, wrist, and hand (including finger joints). ARMEOSPRING, INMOTION, and ARMEOPOWER structures learn how to connect the joints of the shoulder and elbow and in addition prepare for the expansion of the flexo wrist and hand grip, without the finger joints.
The therapeutic performance of specific tasks prepared for prayer assisted by robots is demonstrated. It is therefore reasonable that 86% of audit entities look at this approach. It is evident that the structures have more than one mode of operation (pride, flexibility, strong support, or strong restraint). This speaks to the amazing preferred position when considering treatment options in a flexible and well-planned way for the type of injury. A few frameworks are developing robotic applications, which can provide assistance in the development or remuneration of gravity through transmissions based on connectors or pneumatic actuator components.
The pneumatic actuator [81, 90, 98] frames offer the advantage of building high power with low weight added to the gadget, while the transmission modes have more stunting input, perfection, and greater flexibility in their input by members.
Finally, all of the restorative components of the tested technology can detect and naturally maintain biomechanical measurements during treatment. To each set of machines, one is able to measure workplace, levels of shared development, more energy expenditure, such as quality in terms of greater accuracy, and completeness of directions. Various steps were obtained in the past at a given speed to perform and fulfill assignments, and as response times. The security and power of these parameters are accelerated due to the natural sensitivity of the automatic frame (encoders, power sensors, current sensors, etc.). These are paid records due to the physical properties of the equipment.
2.8 Towards Autonomous Restoration Processes?
The advancement of independent frameworks is a functioning line in mechanical technology by and large, and with expanding presence in medical services applications, it is as of now producing valuable outcomes as it has done in industry [49]. That is the situation of careful robots in insignificantly intrusive systems for executing independently straightforward careful assignments, in view of the exactness of robot developments, picture handling calculations, and psychological frameworks [82–89].
There are numerous different models than careful advanced mechanics of translational exploration applied to medical care. The regular comprehension in the mechanical local area is that the objective of automated restoration gadgets ought to be to help specialists in playing out the sorts of exercises and practices they accept to give their patients the most obvious opportunity with regards to a useful recuperation. Be that as it may, a few boundaries have been recognized, for the specific instance of recovery advanced mechanics. The first recognized hindrance is the absence of viable correspondence in the arranging phase of planning mechanical technology helps, between engineers and also specialists. Second, large numbers of gadgets are extraordinarily confounded, from both a designing and an ease of use perspective. Indeed, “easy to-utilize” gadgets are more probable to be embraced by the clinical local area than those that have since quite a while ago been set up on occasions or require numerous advisors and additionally help to utilize [50]. Other major obstacles are the cost and accessibility, its relevance and adequacy of treatment, and the duration of mechanical therapy. Many works address these issues. The back models are those of Acosta et al., which show that while computer games can provide a convincing interface, it is much better whenever it is intended to identify obvious weaknesses [51]. Burgar et al. incorporate the importance of providing high administrative power (long duration of treatment each day) in a powerful side study using the MIME robot [52]. Telemedicine and telephone rehabilitation are promising features for remote construction for a superficial, easy-to-use restorative framework that can allow for patient counseling work at home. Real games and tangible portable gadgets are emerging as the most inspiring devices to break this limit. The last limit, however not the smallest one in the view of the creators, is the lack of equipment, which greatly creates the total cost of medicine. Is there a great deal of power to capture medical interactions?
To incorporate this method of mechanization to deal with the rate of retrieval, it is first important to differentiate how connections are created and to classify the ones that are less useful. Computer programming, such as the needs and controls to achieving this goal.
In the literature review presented in this document, we have divided the three main regions into a recovery cycle in which key technicians add to the use of equipment: treatment planning conferences, mediation, and evaluation of therapeutic efficacy. This cycle of recovery, from Figure 2.1, has been transformed into a computerized cycle as shown in Figure 2.2. In this figure, entertainers (patient and professional) are supported by a few computer resources, as will be explained below.
2.8.1 Default Renewal Cycle
This document suggests the formation of a continuous cycle of recovery that is more explicit as to which components of interaction will be installed on a computer, just as the processors and components are installed. The autonomous cycle will be constructed in this way with five elements directly related to the squares of the first cycle. In line with this trend, three forms of entertainment have been categorized: client, clinic (grouped), and computer systems. Although a few frames with robots can be accessed, as shown in Figure 2.2, we expect that the ones used are better suited for each case. Proper joint effort between the medical team and the robotic structures is essential in achieving a well-established recovery rate.
The association between the three members during the mechanical rehabilitation process will be shown in Figure 2.4. Initially, a basic examination (performed by a meeting and investigation) is performed by a physician to distinguish the patient’s issues and needs and select the most appropriate treatment options. Similarly, appropriate scales for practical testing are taken to measure the impedance level of usefulness brought on by nerve injury. Here, where the first robotic-to-robin framework is present, the standardized test framework plays a practical test using the same clinically approved scales. The results obtained with AAS are naturally renewed in the patient’s clinical history. Moreover, these effects are effective as a limitation of knowledge in the second structured framework, a network of spiritual selection. DSS [91–96] aims to organize the most appropriate treatment session for the patient, creating specific interventions. This figure is based on the requirements identified in the recently launched writing survey.

Figure 2.4 Automated restoration cycle.
The specialist talks about the patient to evaluate and change goals, choosing which treatment plans proposed by the DSS will be available. At that point, automated rescue agencies play communication. After pleading with RRS, a feasibility test similar to the one below was performed, measuring the adequacy of the recovery measures. With this, AAS is also used. Finally, when all identified issues are considered to have been resolved or accepted by both physicians and the patient, the recovery cycle is over. Alternatively, important cycles will be made to try to deal with excessive problems.
It can be well documented that the proposed mechanical frameworks operate independently and freely but that they are naturally related and dependent on each other for productive work, with concerted effort by the clinic and the patient. Strategies for issuing measurements and providing them and their level of acceptance by both clients and social workers should be supported and evaluated, such as the right to achieve computer use. Planning to help recovery frameworks, although it is emphasized that no obligation is to be met, it is important to plan for the understanding of the requirements requested by counselors to enable easy reconciliation of innovation in their daily activities [53].
By making it easier and easier to access resources to make this cycle of recovery, the power to extend the recovery cycle can be expanded not only as a permanent action but also in addition as a fixed recovery, for example, finding appropriate energy-saving treatment in destructive cases.
In this way, in the test of the creators, the requirements for the components of the recovery cycle be met in order to be self-sufficient are depicted next.
2.8.1.1 Computerized Testing Programs
With the discovery of experimental strategies in neuro regeneration [97–111], the use of a standard engine and practical scales is a key approach to determining the adequacy of the reversal rate. Therefore, the development of strategies based on the standard commonly used test and known expert in retrieval is one of the research lines developed to achieve a self-sufficient cycle.
There is now an investigation into this work, looking at two structures: process and measurement. In terms of techniques, controlled experiments without direct consultation with a specialist are best suited for robotics. With respect to measurements, it is important to examine which provides the most important and least disruptive data for the study to be evaluated [54].
It is commonly seen that FMA may be the most widely used scales used in engine testing in early clinical trials for this included study. It therefore makes sense that these types of experimental strategies may be explored. The use of RGB-D sensors, internal balance sensors, and various sensors allows beating a piece of FMA to be made into a robot [55]. Besides, perhaps the biggest problem related to testing using a culture test is the time they take the counselor to control us.
The address of the various activities sets out the design of the test strategies, for example, the BBT model [56]. All assumptions, a large number of scales, and a combination of strategies (based on sensors, global positioning frames, PC based, etc.) make the topic of computerized testing a promising line of testing.
In this regard, writing in addition reveals a few activities that focus on using machines on a very high level and “advanced” scale. As cultural scales are widely used in clinical preliminaries in retrieval, as found in this article, and since the experimental organization is tedious, it seems reasonable that robotization of these species of assessment strategies be considered. There is a significant difference in focus between clinical evaluation and evaluation. Custom scales include a few things.
However, the estimates are based on feature tests and a few investigations [57], which show that multi-item measures require fewer selectively selected products to produce reliable and legal standards.
Following the recovery cycle model, most of the tested components (depending on the end result or exoskeletons) are clearly found within the mediation stages of the recovery cycle. In any case, their level (46% of final performance, more than 43% exoskeleton) adjusted the test phase, based on the estimates available for use.
These tests complement as a “quick test” procedure to assist the counselor and educate the patient about the effectiveness of recovery interactions; however, there are not many activities that report near trials or clinical initiatives for acknowledging nonclinical ratings.
2.8.1.2 Choice Support System
Choice emotionally supportive networks in view of computerized reasoning (AI-fueled DSS) are quite possibly the most dynamic fields as of late, and it is normal that they will before long add to the dynamic measure. In medical services, an assortment of programming for EMR, the board is as of now accessible to help the specialist in dynamic. Notwithstanding, the conclusion of infections still presents genuine restrictions. We can discover various cell phone applications that permit an online determination, yet the dependability of the finding is not yet predictable with that of a specialist [58]. Plus, scientists in the man-made brainpower local area have begun to plan robot-helped recovery gadgets that execute man-made reasoning strategies to enhance the dynamic help procedures found in Section 2.2. Clinical choices are a significant part of the restoration cycle, since they include the assurance of the goals and plan of the restoration treatment. As can be found in this survey, the help given via mechanized frameworks for this sort of errand is through more solid target data about the engine execution of the client during the mediation, just as permitting the execution of various sorts of mediation techniques that can be designed by the clinician.
With respect to the task phase of the recovery cycle, there are two stages that could be robotized by utilizing computerized reasoning procedures: the arranging of mediation medicines and the task of fitting RRS for intercession.
Identified by the classification of antibodies, the age of these conferences depends on the various components depending on the type of wound and what it means in the evolution of events of exercise for the daily life of the patient. Many interventions are designed to manage a particular effect (strong measures of obvious problems); however, there is no reason to accept that good treatment.
In addition, meeting planning should consider the resources available to hold such a meeting to remove the appropriate RRS from the type of injury (e.g., hand injuries cannot be repaired by a elbow designed gadget).
In this way, we have identified a number of requirements that must be met to establish strategic frameworks for treatment planning: (1) the enjoyment between outcome measures and standardized approaches, with the aim of ending innovative-based interventions and critical thinking processes; (2) classify these measures according to the level of impact (mild, moderate, and sensitive); (3) by looking at the models, distinguishing the boundaries that reflect the sufficiency of the socio-economic status of the patient and the sound profiles; (4) having the opportunity to measure the client’s status against a reliable government assistance model; and (5) create a meeting that can be used with accessible mediation structures.
These requirements suggest that the integration of DSS-controlled intelligence into a computer cycle is required as the information affects the results of the testing frameworks (AAS) and, as a result, introduces an advanced medical conference that can be used by structured communication frameworks (RRS). This is why unconventional considerations are expected in the development of strategies that allow for integration and social inclination in the manufacture of these mechanical structures.
2.8.1.3 Mechanical Rehabilitation Systems
The evolution of events in the medical technology fields and the RRS are areas that have aroused great interest in research in mechanical technology. Because of the rapid interaction in the communication phase, the various strategies used for recovery (work planning, motivation demand, etc.), and the understanding of these most involved, appropriate treatment can be a powerful topic for testing [59].
Two key issues have been identified: the RRS’s ability to obtain a variety of patient performance information during the turn of events and that from this information a patient’s performance assessment is obtained, or for the same type of points as cultural scales.
However, the type and amount of data available depend largely on the framework of the default framework (end-to-end or otherwise exoskeleton) and physical visual framework. In addition, the parameters obtained in the measurement, such as value marks (precision, completeness, etc.), may vary significantly. In this way, the key issue is to integrate the ratings obtained by the RRS, so they provide as much data as possible for a quick test by a consultant and not just raw data. In line with this, among these types of measurements, we have compliance: scope of improvement, speed, accuracy, and efficiency.
The level of patient activity and the level of robot activity, and the level of consideration in the delivery of items should be absolutely equal. All the experimental activities are related to the acquisition of kinematic information; however, they do not look for important level marks, for example, robot levels and patient activity (other than NeRe-Bot offers you as a level) or level of consideration.
Another important issue is to promote client adherence to treatment. It is important to provide adequate input to convince the patient. Using realms that are unpopular with consumers is the most widely used answer for this reason. However, it is important not just how the current criticism is given in addition to the data provided to the client. In this sense, counselors agree that a visual input that informs the client of the possibility of improving his or her score during treatment may be helpful. Other markers at an undeniable level, for example, robot and patient activity levels, control signal, or additional kinematic information, may be helpful to the client if they are likely to help show the importance of patient development.
RRS-type structures are currently integrated into the recovery cycle due to their proximity to mediation; in any case, looking at the questions mentioned earlier will allow the rest of the computer components shown in this article (AAS and DSS) to use the specified data obtained through RRS.
2.9 Conclusion
Another segment of PC recovery is proposed depending on a composed review of computerized recuperation modes for cutting-edge treatment, which incorporates its connection with the recuperation cycle. This construction has been acquainted in connection with the utilization of a specific free reclamation strategy. Three mechanical parts are shown to frame the proposed framework: mechanized testing frameworks, discretionary assistance structures, and computerized recuperation systems. The advancement of AAS ought to be founded on standard demonstrative methods, since standard scales are right now the “best quality” for estimating results and deciding treatment ampleness. Furthermore, the outcomes given by AAS are acquired in an objective scoring way, creating extra information on customer execution.
Those systems ought to be enhanced with DSS books to help with clinical arranging and treatment arranging. The board is right now inclined to use patient information for the utilization of unequivocal frameworks dependent on verifiable levels and notwithstanding man-made abilities. Progressed treatment meetings adjusted to the patient’s condition rely upon them being made normally by the DSS. Hence, AI is presently a promising device. Dealing with an assortment of goals in picking insightful arranging and supporting learning measurements [60] may consider fitting gatherings to be built. Along these lines, treatment gatherings may require just approval or change by the facility. Taking everything into account, the execution of the proposed plan should address a couple of issues summed up as follows:
- (i) For the advancement of instruments to consider further correspondence, socialization of these PC frameworks is required. One should have thought of data pertinent to administrators to permit AAS and DSS to focus on information acquired through RRS. In accordance with these lines, a book channel, for example, the different segments of PC parts will be empowered.
- (ii) For the situation of the advancement of AAS, the arranged testing association ought to be thought of and not simply a replication of results. Customer data are similarly just about as significant as system usage, on the grounds that without the customer’s collaboration and endorsement, structure may not work.
- (iii) The seriousness of the neurological issues and their impact regularly lead to extra illnesses at the same time with a huge issue (comorbidity) that may thwart the patient’s recuperation.
- (iv) The disclosure of utilizing AI to create positive remedial gatherings is as yet youthful; anyway, considering these non-logical advances as of now being created, it is feasible to add to the proposed utilization of DSS to engage you.
- (v) Clinical meetings are affirmed by the act of randomized controlled preliminaries when countless patients get a similar treatment. Accordingly, more significant models ought to be selected RCTs that evaluate the immediate impact of characteristic neurological issues. Robots are at present seen as forefront gadgets under the direction of an advisor. Regardless, the utilization of the previously mentioned structures can make an ever increasing number of free, sharp cycles in neuro recovery.
References
1. Janca, A., Aarli, J.A., Prilipko, L., Dua, T., Saxena, S., Saraceno, B., WHO/WFN survey of neurological services: a worldwide perspective. J. Neurol. Sci., 247, 1, 29–34, 2006.
2. United Nations, World Population Ageing 2017 Report, 2017, October, 2017 http://www.un.org/en/development/desa/population/publications/index.html.
3. Holliday, R.C., Antoun, M., Play ford, E.D., A survey of goal-setting methods used in rehabilitation. Neuro Rehabil. Neural Repair, 19, 3, 227–231, 2005, 16093413.
4. Climent Barbera, J. and Sanchez-Paya, J., Indicadores desalud y medicina de rehabilitacion: estimadores de incapacidad en la poblacion. Rehabilitacion, 30, 277–286, 1996.
5. Chua, K.S.G. and Kuah, C.W.K., Innovating with rehabilitation technology in the real world: promises, potentials, and perspectives. Am. J. Phys. Med. Rehabil., 96, 10, S150–S156, 2017.
6. Van der Loos, H.M., Reinkensmeyer, D.J., Guglielmelli, E., Rehabilitation and healthcare robotics, in: Springer Handbook of Robotics, B. Siciliano and O. Khatib (Eds.), pp. 1685–1728, Springer International Publishing, Cham, 2016.
7. Gomes, P., Surgical robotics: reviewing the past, analyzing the present, imagining the future. Robot. Comput.- Integr. Manuf., 27, 2, 261–266, 2011, Translational Research – Where Engineering Meets Medicine.
8. Huang, H., Wolf, S.L., He, J., Recent developments in biofeedback for neuro motor rehabilitation. J. Neuro Eng. Rehabil., 3, 1, 11, 2006.
9. Poli, P., Morone, G., Rosati, G., Masiero, S., Robotic technologies and rehabilitation: new tools for stroke patients’ therapy. BioMed. Res. Int., 2013, 8 pages, 2013.
10. Timmermans, A.A., Seelen, H.A., Willmann, R.D., Kingman, H., Technology-assisted training of arm-hand skills in stroke: concepts on reacquisition of motor control and therapist guidelines for rehabilitation technology design. J. Neuro Eng. Rehabil., 6, 1, 1, 2009.
11. Dıaz, I., Gil, J.J., Sanchez, E., Lower-limb robotic rehabilitation: literature review and challenges. J. Rob., 2011, Article ID 759764, 11 pages, 2011.
12. Lv, X. and Wu, Z., Review of robot-assisted gait rehabilitation after stroke. J. Rehabil. Robot., 2013, 3–8, 2013.
13. Qian, Z. and Bi, Z., Recent development of rehabilitation robots. Adv. Mech. Eng., 7, 2, 14–23, Article ID 563062, 2014.
14. Rodrıguez-Prunotto, L., Cano-de la Cuerda, R., Cuesta- Gomez, A., Alguacil-Diego, I.M., Molina-Rueda, F., Terapia robótica para la rehabilitation del miembro superior en patología neurological. Rehabilitation, 48, 2, 104–128, 2014.
15. Marchal-Crespo, L. and Reinkensmeyer, D.J., Review of control strategies for robotic movement training after neurologic injury. J. Neuro Eng. Rehabil., 6, 1, 20, 2009.
16. Yan, T., Cempini, M., Oddo, C.M., Vitiello, N., Review of assistive strategies in powered lower-limb orthoses and exoskeletons. Rob. Auton. Syst., 64, 120–136, 2015.
17. Please note that Figures 2.4 and 2.3 citation was unsequence thus change it to be in sequence. Edit OK? Note that figures should be cited sequentially.
18. Kwakkel, G., Kollen, B.J., Krebs, H.I., Effects of robot-assisted therapy on upper limb recovery after stroke: a systematic review. Neuro Rehabil. Neural Repair, 22, 2, 111–121, 2008.
19. Norouzi-Gheidari, N., Archambault, P.S., Fung, J., Effects of robot-assisted therapy on stroke rehabilitation in upper limbs: systematic review and meta-analysis of the literature. J. Rehabil. Res. Dev., 49, 4, 479–496, 2012.
20. Veerbeek, J.M., Langbroek-Amersfoort, A.C., van Wegen, E.E.H., Meskers, C.G.M., Kwakkel, G., Effects of robot-assisted therapy for the upper limb after stroke: a systematic review and meta-analysis. Neuro Rehabil. Neural Repair, 31, 2, 107–121, 2017.
21. World Health Organization, World Report on Disability, 2011, October 2017, http://www.who.int/en/.
22. Meyer, T., Gutenbrunner, C., Bickenbach, J., Cieza, A., Melvin, J., Stucki, G., Towards a conceptual description of rehabilitation as a health strategy. J. Rehabil. Med., 43, 769, 765–769, 2011.
23. Stucki, G. and Sangha, O., Principles of rehabilitation. Rheumatology, 1, 517–530, 1998.
24. Steiner, W.A., Ryser, L., Huber, E., Uebelhart, D., Aeschlimann, A., Stucki, G., Use of the icf model as a clinical problem-solving tool in physical therapy and rehabilitation medicine. Phys. Ther., 82, 111, 1098–1107, 2002.
25. World Health Organization, Neurological Disorders: Public Health Challenges, 2006, October 2017, http://www.who.int/mental_health/neurology/neurodiso/en/.
26. King, J., Nelson, T., Blankenship, K., Turturro, T., Beck, A., Rehabilitation Team Function and Prescriptions, Referrals, and Order Writing, Rehabilitation Medicine: Principles and Practice, 4th edition, J.A. Delisa (Ed.), Lippincott Williams & Wilkins, Philadelphia, PA, USA, 2005.
27. McColl, M., Gerein, N., Valentine, F., Meeting the challenges of disability: models for enabling function and wellbeing, in: Occupational Therapy: Enabling Function and Well-Being, pp. 509–528, Slack, Thorofare, NJ, USA, 1997.
28. Ramiro-Gonzalez, M. and Gonzalez Alted, C., El equipo de trabajo en neurorrehabilitacion, in: Neurorehabilitacion, R. Cano-de la Cuerda and S. Collado Vazquez (Eds.), pp. 61–72, Medica Panamericana, Madrid, Spain, 2012.
29. Reilly, C., Transdisciplinary approach: an atypical strategy for improving outcomes in rehabilitative and long-term acute care settings. Rehabil. Nurs., 26, 6, 216–244, 2001.
30. Finch, E., Physical Rehabilitation Outcome Measures: A Guide to Enhanced Clinical Decision Making, 2nd edition, Canadian Physiotherapy Association, Hamilton, ON, Canada, 2002.
31. World Health Organization, International Classification of Functioning, Disability and Health (ICF), 2001, October 2017, http://www.who.int/classifications/icf/en/.
32. Barnes, M.P., Principles of neurological rehabilitation. J. Neurol. Eurosurg. Psychiatry, 74, 90004, 3iv–3iv7, 2003.
33. Thompson, A.J., Neurological rehabilitation: from mechanisms to management. J. Neurol. Neurosurg. Psychiatry, 69, 6, 718–722, 2000.
34. Miller, E.L., Murray, L., Richards, L. et al., Comprehensive overview of nursing and interdisciplinary rehabilitation care of the stroke patient: a scientific statement from the American Heart Association. Stroke, 41, 10, 2402–2448, 2010.
35. Neumann, V., Gutenbrunner, C., Fialka-Moser, V. et al., Interdisciplinary team working in physical and rehabilitation medicine. J. Rehabil. Med., 42, 1, 4–8, 2010.
36. Katz, D., Mills, V., Cassidy, J., Neurological rehabilitation: a guide to diagnosis, prognosis and treatment planning, in: The Neurological Rehabilitation Model in Clinical Practice, pp. 1–27, Blackwell Science, Oxford, UK, 2018.
37. Kersten, P., Principles of physiotherapy assessment and outcome measures, in: Physical Management in Neurological Rehabilitation, vol. 2, pp. 29–46, 2004.
38. Salter, K., Campbell, N., Richardson, M. et al., Outcome measures in stroke rehabilitation, in: Evidence-Based Review of Stroke Rehabilitation, Heart and Stroke Foundation, Canadian Partnership for Stroke Recovery, Ontario, Canada, 2014.
39. Lennon, S., Physiotherapy practice in stroke rehabilitation: a survey. Disabil. Rehabil., 25, 9, 455–461, 2003, 12745940.
40. Pomeroy, V., Aglioti, S.M., Mark, V.W. et al., Neurological principles and rehabilitation of action disorders: rehabilitation interventions. Neuro Rehabil. Neural Repair, 25, 5, 33S–43S, 2011.
41. Donaghy, M., Principles of neurological rehabilitation, in: Brain’s Diseases of the Nervous System, 12 editions, M. Donaghy (Ed.), pp. 165–179, Oxford University Press, Oxford, UK, 2011.
42. Doig, E., Fleming, J., Cornwell, P.L., Kuipers, P., Qualitative exploration of a client-centered, goal-directed approach to community-based occupational therapy for adults with traumatic brain injury. Am. J. Occup. Ther., 63, 5, 559–568, 2009.
43. The Partnership for Robotics in Europe SPARC, Robotics 2020 Multi Annual Roadmap, Call 2 ICT24 (2015) – Horizon 2020, Hindawi Publication, Brussels, Belgium, 2015.
44. Davis, A., Davis, S., Moss, N. et al., First steps towards an interdisciplinary approach to rehabilitation. Clin. Rehabil., 6, 3, 237–244, 1992.
45. Bosecker, C., Dipietro, L., Volpe, B., Krebs, H.I., Kinematic robot-based evaluation scales and clinical counterparts to measure upper limb motor performance in patients with chronic stroke. Neurorehabil. Neural Repair, 24, 1, 62–69, 2010, 19684304.
46. Capterra, 1999, January 2018, https://www.capterra.com/electronic-medical-records-software/.
47. The medical futurist, 2018, January 2018, http://medicalfuturist.com/top-artificial-intelligence-companies-in-healthcare/.
48. Iosa, M., Morone, G., Cherubini, A., Paolucci, S., The three laws of neurorobotics: a review on what neurorehabilitation robots should do for patients and clinicians. J. Med. Biol. Eng., 36, 1, 1–11, 2016.
49. Muradore, R., Fiorini, P., Akgun, G. et al., Development of a cognitive robotic system for simple surgical tasks. Int. J. Adv. Rob. Syst., 12, 4, 37, 2015.
50. Hidler, J. and Lum, P.S., The road ahead for rehabilitation robotics. J. Rehabil. Res. Dev., 48, 4, vii–vix, 2011.
51. Acosta, A.M., Dewald, H.A., Dewald, J.P., Pilot study to test effectiveness of video game on reaching performance in stroke. J. Rehabil. Res. Dev., 48, 4, 431–444, 2011.
52. Burgar, C.G., Garber, S.L., Van der Loos, H.M., PhD, O., Deborah Kenney, M.S., Shor, P., Robot-assisted upper limb therapy in acute rehabilitation setting following stroke: department of veterans affairs multisite clinical trial. J. Rehabil. Res. Dev., 48, 4, 445–458, 2011.
53. Saborowski, M. and Kollak, I., How do you care for technology?” – care professionals’ experiences with assistive technology in care of the elderly. Technol. Forecasting Soc. Change, 93, 133–140, 2015, Science, Technology and the “Grand Challenge” of Ageing.
54. Coster, W.J., Making the best match: selecting outcome measures for clinical trials and outcome studies. Am. J. Occup. Ther., 67, 2, 162–170, 2013.
55. Otten, P., Kim, J., Son, S.H., A framework to automate assessment of upperlimb motor function impairment: a feasibility study. Sensors, 15, 12, 20097–20114, 2015.
56. Oña, E.D., Jardón, A., Balaguer, C., The automated box and blocks test an autonomous assessment method of gross manual dexterity in stroke rehabilitation, in: Towards Autonomous Robotic Systems, Lecture Notes in Computer Science, Y. Gao, S. Fallah, Y. Jin, C. Lekakou (Eds.), pp. 101–114, Springer, Cham, 2017.
57. Hobart, J., Lamping, D., Freeman, J. et al., Evidence-based measurement which disability scale for neurologic rehabilitation? Neurology, 57, 4, 639–644, 2001.
58. Semigran, H.L., Levine, D.M., Nundy, S., Mehrotra, A., Comparison of physician and computer diagnostic accuracy. JAMA Intern. Med., 176, 12, 1860–1861, 2016.
59. Krebs, H.I., Palazzolo, J.J., Dipietro, L. et al., Rehabilitation robotics: performance-based progressive robot-assisted therapy. Auton. Robots, 15, 1, 7–20, 2003.
60. Roijers, D.M. and Whiteson, S., Multi-objective decision making. Synth. Lect. Artif. Intell. Mach. Learn., 11, 1, 1–129, 2017.
61. Ellis, M.D., Sukal-Moulton, T.M., Dewald, J., Impairment-based 3-D robotic intervention improves upper extremity work area in chronic stroke: targeting abnormal joint torque coupling with progressive shoulder abduction loading. IEEE Trans. Rob., 25, 3, 549–555, 2009.
62. Kahn, L.E., Zygman, M.L., Rymer, W.Z., Reinkensmeyer, D.J., Robot assisted reaching exercise promotes arm movement recovery in chronic hemiparetic stroke: a randomized controlled pilot study. J. Neuro Eng. Rehabil., 3, 1, 12, 2006.
63. Reinkensmeyer, D.J., Kahn, L.E., Averbuch, M., McKenna- Cole, A., Schmit, B.D., Rymer, W.Z., Understanding and treating arm movement impairment after chronic brain injury: progress with the arm guide. J. Rehabil. Res. Dev., 37, 653, 2000.
64. Casadio, M., Sanguineti, V., Morasso, P.G., Arrichiello, V., Braccio di ferro: a new aptic workstation for neuromotor rehabilitation. Technol. Healthcare, 14, 3, 123–142, 2006.
65. Vergaro, E., Casadio, M., Squeri, V., Giannoni, P., Morasso, P., Sanguineti, V., Self-adaptive robot training of strokesurvivors for continuous tracking movements. J. Neuroeng. Rehabil., 7, 1, 13, 2010.
66. Loureiro, R., Amirabdollahian, F., Topping, M., Driessen, B., Harwin, W., Upper limb robot mediated stroke therapy— gentle/s approach. Auton. Robots, 15, 1, 35–51, 2003.
67. Coote, S., Murphy, B., Harwin, W., Stokes, E., The effect of the gentle/s robot-mediated therapy system on arm function after stroke. Clin. Rehabil., 22, 5, 395–405, 2008.
68. Bionik Laboratories Corp, 2010, October 2017, https://www.bioniklabs.com/.
69. Jackson, A.E., Culmer, P.R., Levesley, M.C., Makower, S.G., Cozens, J.A., Bhakta, B.B., Effector force requirements to enable robotic systems to provide assisted exercise in people with upper limb impairment after stroke, in: 2011IEEE International Conference on Rehabilitation Robotics, Zurich, Switzerland, pp. 1–6, 2011.
70. Jackson, A., Culmer, P., Makower, S. et al., Initial patient testing of ipam a robotic system for stroke rehabilitation, in: 2007 IEEE 10th International Conference on Rehabilitation Robotics, Noordwijk, Netherlands, pp. 250–256, 2007.
71. Micera, S., Sergi, P.N., Zaccone, F. et al., A low-cost biomechatronic system for the restoration and assessment of upper limb motor function in hemiparetic subjects, in: 2006 The First IEEE/RAS-EMBS International Conference on Biomedical Robotics and Bio mechatronics, BioRob, Pisa, Italy, pp. 25–30, 2006.
72. Colombo, R., Pisano, F., Micera, S. et al., Robotic techniques for upper limb evaluation and rehabilitation of stroke patients. IEEE Trans. Neural Syst. Rehabil. Eng., 13, 3, 311–324, 2005.
73. Lum, P.S., Burgar, C.G., Van der Loos, M., Shor, P.C., Majmundar, M., Yap, R., Mime robotic device for upper-limb neurorehabilitation in subacute stroke subjects: a follow-up study. J. Rehabil. Res. Dev., 43, 5, 631–642, 2006.
74. Masiero, S., Armani, M., Rosati, G., Upper-limb robotassisted therapy in rehabilitation of acute stroke patients: focused review and results of new randomized controlled trial. J. Rehabil. Res. Dev., 48, 4, 355–366, 2011.
75. Masiero, S., Armani, M., Ferlini, G., Rosati, G., Rossi, A., Randomized trial of a robotic assistive device for the upper extremity during early inpatient stroke rehabilitation. Neurorehabil. Neural Repair, 28, 4, 377–386, 2014, 24316679.
76. Toth, A., Fazekas, G., Arz, G., Jurak, M., Horvath, M., Passive robotic movement therapy of the spastic hemiparetic arm with reharob: report of the first clinical test and the follow-up system improvement, in: 2005 9th International Conference on Rehabilitation Robotics, ICORR, Chicago, IL, USA, pp. 127–130, 2005.
77. Fazekas, G., Horvath, M., Troznai, T., Toth, A., Robot mediated upper limb physiotherapy for patients with spastic hemiparesis: a preliminary study. J. Rehabil. Med., 39, 7, 580–582, 2007.
78. Tyro motion gmbh, 2007, October 2017, http://tyromotion.com/.
79. Sale, P., Lombardi, V., Franceschini, M., Hand robotics rehabilitation: feasibility and preliminary results of a robotic treatment in patients with hemiparesis. Stroke Res. Treat., 2012, 5 pages, 2012.
80. Hwang, C.H., Seong, J.W., Son, D.-S., Individual finger synchronized robot-assisted hand rehabilitation in subacute to chronic stroke: a prospective randomized clinical trial of efficacy. Clin. Rehabil., 26, 8, 696–704, 2012.
81. Hesse, S., Schulte-Tigges, G., Konrad, M., Bardeleben, A., Werner, C., Robot-assisted arm trainer for the passive and active practice of bilateral forearm and wrist movements in hemiparetic subjects. Arch. Phys. Med. Rehabil., 84, 6, 915–920, 2003.
82. Schmidt, H., Hesse, S., Werner, C., Bardeleben, A., Upper and lower extremity robotic devices to promote motor recovery after stroke -recent developments, in: 2004 26th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, San Francisco, CA, USA, vol. 2, pp. 4825–4828, 2004.
83. Takahashi, C.D., Der-Yeghiaian, L., Le, V.H., Cramer, S.C., A robotic device for hand motor therapy after stroke, in: 2005 9th International Conference on Rehabilitation Robotics, ICORR, Chicago, IL, USA, pp. 17–20, 2005.
84. Takahashi, C.D., Der-Yeghiaian, L., Le, V., Motiwala, R.R., Cramer, S.C., Robot-based hand motor therapy after stroke. Brain, 131, 2, 425–437, 2008.
85. Motorika medical ltd, 2004, October 2017, http://motorika.com/.
86. Treger, I., Faran, S., Ring, H., Robot-assisted therapy for neuromuscular training of sub-acute stroke patients. A feasibility study. Eur. J. Phys. Rehabil. Med., 44, 4, 431–435, 2008.
87. Meyer-Rachner, P., Passon, A., Klauer, C., Schauer, T., Compensating the effects of fes-induced muscle fatigue by rehabilitation robotics during arm weight support. Curr. Dir. Biomed. Eng., 3, 31–34, 2017.
88. Montagner, A., Frisoli, A., Borelli, L. et al., A pilot clinical study on robotic assisted rehabilitation in vr with an arm exoskeleton device, in: 2007 Virtual Rehabilitation, Venice, Italy, pp. 57–64.
89. Myomo, inc, 2017, October 2017, http://myomo.com/.
90. Page, S.J., Hill, V., White, S., Portable upper extremity robotics is as efficacious as upper extremity rehabilitative therapy: a randomized controlled pilot trial. Clin. Rehabil., 27, 6, 494–503, 2013.
91. Kim, G.J., Rivera, L., Stein, J., Combined clinic-home approach for upper limb robotic therapy after stroke: a pilot study. Arch. Phys. Med. Rehabil., 96, 12, 2243–2248, 2015.
92. Rahman, T., Sample, W., Jayakumar, S. et al., Passive exoskeletons for assisting limb movement. J. Rehabil. Res. Dev., 43, 5, 583–590, 2006.
93. Hocoma, 1996, October 2017, https://www.hocoma.com/.
94. Gijbels, D., Lamers, I., Kerkhofs, L., Alders, G., Knippenberg, E., Feys, P., The armeo spring as training tool to improve upper limb functionality in multiple sclerosis: a pilot study. J. Neuroeng. Rehabil., 8, 1, 5, 2011.
95. Sanchez, R.J., Liu, J., Rao, S. et al., Automating arm movement training following severe stroke: functional exercises with quantitative feedback in a gravity-reduced environment. IEEE Trans. Neural Syst. Rehabil. Eng., 14, 3, 378–389, 2006.
96. Motus nova, 2016, October 2017, http://motusnova.com/.
97. Kutner, N.G., Zhang, R., Butler, A.J., Wolf, S.L., Alberts, J.L., Quality-of-life change associated with robotic assisted therapy to improve hand motor function in patients with subacute stroke: a randomized clinical trial. Phys. Ther., 90, 4, 493–504, 2010.
98. Koeneman, E.J., Schultz, R.S., Wolf, S.L., Herring, D.E., Koeneman, J.B., A pneumatic muscle hand therapy device, in: 2004 The 26th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, San Francisco, CA, USA, vol. 1, pp. 2711–2713, 2004.
99. Schabowsky, C.N., Godfrey, S.B., Holley, R.J., Lum, P.S., Development and pilot testing of hexorr: hand exoskeleton rehabilitation robot. J. Neuroeng. Rehabil., 7, 1, 36, 2010.
100. Bouzit, M., Burdea, G., Popescu, G., Boian, R., The Rutgers master ii-new design force-feedback glove. IEEE/ASME Trans. Mechatron., 7, 2, 256–263, 2002.
101. Merians, A., Jack, D., Boian, R. et al., Virtual reality augmented rehabilitation for patients following stroke. Phys. Ther., 82, 898–915, 2002.
102. Allington, J., Spencer, S.J., Klein, J., Buell, M., Reinkensmeyer, D.J., Bobrow, J., Supinator extender (sue): a pneumatically actuated robot for forearm/ wrist rehabilitation after stroke, in: 2011 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Boston, MA, USA, pp. 1579–1582, 2011.
103. Sanchez, R., Reinkensmeyer, D., Shah, P. et al., Monitoring functional arm movement for home-based therapy after stroke, in: 2004 The 26th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, San Francisco, CA, USA, vol. 2, pp. 4787–4790, 2004.
104. Rocon, E., Belda-Lois, J.M., Ruiz, A.F., Monto, M., Moreno, J.C., Pons, J.L., Design and validation of a rehabilitation robotic exoskeleton for tremor assessment and suppression. IEEE Trans. Neural Syst. Rehabil. Eng., 15, 3, 367–378, 2007.
105. Nef, T. and Riener, R., Shoulder actuation mechanisms for arm rehabilitation exoskeletons, in: 2008 2nd IEEE RAS EMBS International Conference on Biomedical Robotics and Bio mechatronics, Scottsdale, AZ, USA, pp. 862–868, 2008.
106. Guidali, M., Duschau-Wicke, A., Broggi, S., Klamroth-Marganska, V., Nef, T., Riener, R., A robotic system to train activities of daily living in a virtual environment. Med. Biol. Eng. Comput., 49, 10, 1213–1223, 2011.
107. Nef, T., Mihelj, M., Colombo, G., Riener, R., Armin – robot for rehabilitation of the upper extremities, in: Proceedings 2006 IEEE International Conference on Robotics and Automation, Orlando, FL, USA, pp. 3152–3157, 2006.
108. Nef, T., Mihelj, M., Riener, R., Armin: a robot for patient cooperative arm therapy. Med. Biol. Eng. Comput., 45, 9, 887–900, 2007.
109. Loureiro, R.C.V. and Harwin, W.S., Reach & grasp therapy: Design and control of a 9-dof robotic neuro-rehabilitation system, in: 2007 IEEE 10th International Conference on Rehabilitation Robotics, Noordwijk, Netherlands, pp. 757–763, 2007.
110. Huang, J., Tu, X., He, J., Design and evaluation of the Rupert wearable upper extremity exoskeleton robot for clinical and in-home therapies. IEEE Trans. Syst. Man Cybern.: Syst., 46, 7, 926–935, 2016.
111. Balasubramanian, S., Wei, R., Perez, M. et al., Rupert: an exoskeleton robot for assisting rehabilitation of arm functions, in: 2008 Virtual Rehabilitation, Vancouver, Canada, pp. 163–167, 2008.
- * Corresponding author:
