Digestion 101
In This Chapter
![]()
- The steps of the digestion process
- How your body absorbs nutrients from food
- When food can physically hurt?
- How to strengthen your gut with pro- and prebiotics
- Why does your body need water?
The digestive process receives impulses from your five senses: sight, smell, taste, auditory, and touch. When you walk into a bakery, the sight and smell of freshly baked pastries is enough to get your digestive juices flowing. The digestion and absorption of food is a step-by-step process that involves a host of actions from various organs and metabolic processes.
In this chapter, we’ll look at how the nutrients in foods are utilized by your body for growth, repair, and protection. We’ll explore what occurs throughout each step in the digestive tract, along with the intricate processes of converting food into usable components. Additionally, we’ll examine what happens when a problem in the digestive process occurs and learn the best ways to deal with the issue.
The journey through the digestive system physically begins in the mouth. Food travels through the oral cavity, esophagus, and stomach, which are referred to as your upper digestive tract. The lower digestive tract includes the small and large intestines, with assistance from organs like the pancreas, liver, and gallbladder, which aid in the release of enzymes and chemicals into the intestines to help break down the nutrients. Through this chemical and mechanical action, food is broken down into small molecules your body can readily absorb.
The Mouth
The first step of digestion occurs in the mouth. The function of the mouth is to mechanically break down foods through the action of chewing, which grinds the foods into smaller particles to maximize access to nutrients. Strong jaw muscles also provide power to assist in this step. As food is broken down, saliva produced by the salivary glands adds moisture. Saliva is made up of 99.5 percent water, along with enzymes and mucus. There are three types of salivary glands: parotid, sublingual, and submandibular, which are located in the oral cavity above and below your teeth.
Amylase is the first enzyme contained in your saliva that acts on the food in its moistened state, which begins breaking down the bonds that hold starch molecules together. The tongue and back of the mouth also contain glands that secrete lingual lipase, another enzyme that acts on fats like triglycerides upon their arrival in the stomach. The enzyme’s role is minimal, and these particular enzymatic actions are more prevalent in infants to aid in the digestion of milk fats. This enzyme’s release decreases with age.
The action of swallowing is a voluntary muscle action initiated by you. However, it’s the brain that regulates the remaining involuntary swallowing processes that take place. Food must first pass through the pharynx, which is basically a 5-inch section in the back of the throat beginning at the base of the skull with openings to the nasal passageways and trachea, also known as the windpipe.
As food passes down the back of the throat, the larynx, which is part of the respiratory system and houses your vocal cords, receives a signal. The larynx moves up, which allows the epiglottis (a flap of skin) to slide over and cover the trachea to prevent food from going down into your windpipe and choking you. The larynx is made up of cartilage and is visibly recognizable on the outside front of the neck. It’s commonly referred to as the Adam’s apple.
Close to 3,000 adults die every year due to choking, which occurs when the trachea or windpipe, which leads to the lungs, becomes blocked. In most cases, it’s blocked by food. The Heimlich maneuver can be performed to remove the food, by grasping the choking person around the waist from behind with hands clasped and giving a short thrust in an upward motion directly below the diaphragm. This motion expels air from the lungs and hopefully dislodges the food from the blocked airway.
The swallowed food is referred to as a “bolus.” Once the bolus passes through the pharynx, it moves into the esophagus. The esophagus is a hollow tube about 10 inches in length and 1 inch in diameter. It runs from the base of the pharynx to the stomach, and its only function is to transport food. The presence of the food stimulates the parasympathetic nerves, which are responsible for propelling the food down into the stomach. This involuntary muscle action is called peristalsis. Peristalsis is the alternating of involuntary muscle contractions and relaxations to cause a wavelike movement. At the end of the esophagus is the lower esophageal sphincter, which controls the flow of food into the stomach.
DEFINITION
A sphincter is a circular muscle portal between key passages in the GI tract that controls the release of food.
The Stomach
The lower esophageal sphincter controls entry of the bolus into the stomach. As you swallow food, the sphincter relaxes due to an overall drop in pressure. Neural and hormonal regulators manage pressure levels within the sphincter. Once relaxed, the sphincter allows the food to pass into the stomach. The volume of an adult stomach when empty is equivalent to about ¼ cup. It can expand to hold 4 to 6 cups or even more—think of all those food-eating contests. Food remains in your stomach for 2 to 6 hours where it’s chemically and mechanically broken down into small molecules your body can readily absorb.
The stomach is located on the left side of your body under your diaphragm at the base of your lungs. It has three types of muscles: longitudinal, circular, and diagonal. Their function is to help expand and contract to aid in combining food with the acidic contents of the stomach.
The stomach consists of four main parts: the cardia, fundus, body, and antrum. The antrum, the lower third of the stomach, is where most of the action takes place. The cardia is the top portion of the stomach near where food enters. The section to the right of the cardia is the fundus. The central part of the stomach is where food is held. The stomach is lined in folds called rugae. These folds can flatten out and allow the stomach to expand and accommodate a large amount of food.
The antrum is responsible for using the muscles to churn and mix up all that food with the gastric juices and enzymes contained in the stomach.
The stomach is protected from its acidic contents by a thick mucous membrane. Just below the mucous lining are epithelial cells that contain gastric glands and release a variety of digestive juices. What’s released is dependent on their particular location within the stomach. The glands secrete hydrochloric acid (HCL), mucus, water, electrolytes, intrinsic factor, and enzymes. Gastric juices are very acidic, with a pH around 2 in comparison to battery acid at 0.
The primary function of HCL is to activate pepsin, the enzyme needed to help break apart bonds within proteins, kill incoming foreign bacteria from foods you eat, and aid in the release of nutrients. After the food has been worked over by the stomach actions, it resembles a thin watery pastelike substance called chyme. Chyme will exit the stomach about a teaspoon at a time through the pyloric sphincter and into the small intestine.
DEFINITION
Intrinsic factor is a protein produced by cells in the stomach wall. It is required for the absorption of vitamin B12. Chyme is partially digested semifluid mass of food found in the stomach that passes from the stomach into the small intestine.
The Small Intestine
The small intestine is the primary site of nutrient digestion and absorption. It’s approximately 21 feet in length and about 1 inch in diameter. The longitudinal and circular muscles that make up the length of the tube are designed to help propel the food through the intestines via wavelike motions.
The small intestine is composed of three sections: the duodenum, jejunum, and ileum. The intestine, like the stomach, is covered in a thick layer of mucus to protect it from the highly acidic environment. Once the chyme from the stomach enters the first section of the intestine, called the duodenum, specialized cells residing in the lining begin to release alkaline secretions to help neutralize the acidic chyme. It then receives a dose of secretions from the pancreas, which contains bicarbonate to ensure the acid has been neutralized. If by chance there is an error in the levels of pH and the acid is not neutralized, then erosion will occur in the lining over time and cause the development of an ulcer.
The pancreatic enzymes digest approximately half of all carbohydrates and proteins and almost all of the fat. Bile is excreted from the gallbladder where it travels through a duct into the duodenum. Bile is made by the liver and stored in the gallbladder. It consists of acids, salts, cholesterol, phospholipids, and bile pigments. Bile’s role in the digestive process is to emulsify fats. Specifically, it connects water and fat molecules together in order to allow the enzymes to access and digest them.
The lining of the intestines contains circular mucosal folds, which look like steep, rolling hills with very deep valleys. The purpose of these folds is to increase the surface area to maximize nutrient absorption. Each of the folds is also covered in a layer of fingerlike projections called villi. These villi are wrapped in epithelial cells. Just beneath those cells are blood capillaries and lymph vessels ready to absorb and transport the nutrients throughout the body.
Additionally, the villi are covered in microvilli, which are referred to as the “brush border.” Microvilli are hairlike projections that contain digestive enzymes from the mucosa cells in the lining. These enzymes break up partially digested carbohydrates and proteins, allowing the nutrients to be readily absorbed into the brush-border cells where they can then move into the blood or lymph fluids.
NOTABLE INSIGHT
Your small intestine has the largest surface area in your body. Picture the size of a tennis court (78 feet long × 36 feet wide). That’s about the same amount of square footage you have available for your body to absorb nutrients from the food you eat.
The majority of the absorption of digested nutrients occurs in the upper portion of the small intestine. Carbohydrates, proteins, fats, vitamins, and minerals are absorbed in each distinct section of the duodenum, jejunum, and ileum. The mechanism of absorption of the nutrients is generally through one of four ways:
1. Diffusion: Nutrients pass directly into the next membrane.
2. Facilitated diffusion: Nutrients need a carrier to assist in passing through the membrane wall.
3. Active transport: Molecules need a little extra boost of energy from adenosine triphosphate (ATP) to pass through the membrane wall.
4. Pinocytosis: Nutrients are surrounded by the membrane and then pinched off and absorbed into the membrane.
Leftovers that cannot be absorbed, such as fiber, dead cells, salt, bile, and water, are passed on to the large intestine.
Chyme is passed from the small intestine to the large intestine through the ileocecal valve into the large intestine. The length of the intestine is 5 feet long and about 3 inches in diameter. The beginning of your large intestine is called the cecum. The colon, which we commonly refer to as the large intestine, is made up of the ascending colon, transverse colon, descending colon, and sigmoid colon. The overall muscle structure differs from the small intestine, as it is designed to allow for indentions that, when filled with chyme, bulge outward. This increases the length of time the chyme has to be in contact within the intestinal wall, allowing for optimal absorption of nutrients. Chyme can remain in the colon for 1 to 3 days. During that time, sodium, potassium, chloride, vitamin K, biotin, and water are absorbed. What remains is mostly fiber.
The large intestine contains its own world of microflora or bacteria. The bacteria use the food leftovers, such as fiber, to help produce some vitamins. These microorganisms also help break down and ferment this fiber. This is a crucial role of the gut flora because humans lack the enzyme to break down fiber. Once everything has been absorbed that can be, the leftover residue is propelled to the end of the colon where the rectum is located. Waste remains there until it is time to be excreted.
When Digestion Goes Wrong
Most of the time our digestive process works flawlessly. Every now and then problems occur, like an upset stomach, which can be easily remedied by over-the-counter medications. Problems can also be more serious in nature, as in the case of ulcers, irritable bowel syndrome (IBS), food allergies, and leaky gut syndrome. Many of these causes are directly relatable to a specific error that occurs in the digestive tract and sometimes the diagnosis is not so clear-cut. Working closely with your doctor to get your digestive tract functioning again is important for good overall health.
DEFINITION
An ulcer or peptic ulcer occurs when stomach acids that digest food cause erosion in the stomach wall or duodenum. Ulcers can be caused by untreated gastroesophageal reflux disease (GERD), excessive use of aspirin and ibuprofen, or most commonly by bacterium known as Helicobacter pylori. While stress and spicy foods do not specifically cause ulcers, they can aggravate the symptoms.
Heartburn, Acid Reflux, and GERD
Heartburn, acid reflux, and gastroesophageal reflux disease (GERD) are often used interchangeably; however, heartburn is a symptom of acid reflux and GERD. Heartburn is literally a pain in the chest, which occurs about an hour after eating. It can be aggravated by lying down, which causes an alteration in pressure in the valve and allows seepage of the acidic chyme to backflow up into the esophagus. Many people end up in the emergency room thinking they’re having a heart attack when, fortunately, it’s only heartburn. The pain is caused by the acidic contents creating a burning sensation. Taking antacids can relieve it, but your doctor needs to determine the underlying cause.
Certain foods and lifestyle habits aggravate this condition by assisting in the alteration of gastric pressure or increasing the production of acid. These foods include high-fat foods, acidic foods, alcohol, nicotine, caffeine, calcium, and orange juice, along with some spices.
Typically treatment will involve eating smaller meals, which will decrease gastric pressure, and thoroughly chewing your food. It is also advised to avoid spicy or acidic foods, to drink water between meals, and to wait three hours before lying down after a meal. If you’re overweight, losing just 2 percent of your body weight may help alleviate symptoms.
Acid reflux is when the stomach contents (chyme) move backwards into your esophagus. The same treatment approach for heartburn can manage the symptoms of acid reflux. However, when acid reflux is ongoing and occurs more than twice a week, it’s labeled GERD and serious damage to the esophagus can occur. The acidic chyme will damage the esophageal mucosa lining and can cause inflammation and swelling. If left untreated, this inflammation and swelling can damage the esophagus by scarring and cause bleeding and ulcers. Severe damage can even progress to cancer of the esophagus.
Celiac Disease
The first known case of celiac disease dates back as far as the second century. This autoimmune disorder currently is considered to be a major public health issue on the rise. Celiac disease is four times more common today than it was 60 years ago. It affects about 1 in 100 people in the United States according to Mayo Clinic Research Education.
Celiac disease is an autoimmune disorder of the intestines and occurs when gluten, a protein found in wheat, rye, and barley, is ingested. When a person with Celiac disease consumes gluten, the protein is not broken down through the normal digestion process. It’s viewed as an enemy and is attacked by the immune system. Over time, the consumption of gluten damages the small intestine, specifically villi, the small fingerlike projections that assist in nutrient absorption. Damaged villi within the intestines will lead to less nutrient absorption and potential malnutrition.
Celiac disease can occur at any age and is also considered to be hereditary. While it’s not fully understood why the immune system attacks gluten and causes damage to the small intestine, it is crucial to recognize key symptoms. For children, these symptoms may include abdominal bloating and pain; chronic diarrhea; constipation; vomiting; pale, foul-smelling, or fatty stool; weight loss, fatigue; irritability and behavioral issues; and failure to thrive.
For adults, symptoms are less likely to be related to digestion. Symptoms for adults include anemia, fatigue, bone or joint pain, arthritis, depression or anxiety, tingling numbness in the hands or feet, seizures or migraines, missed menstrual periods, cankers sores in the mouth, itchy skin rash, and diarrhea.
It’s important to recognize symptoms early on as this disease can lead to other serious health problems, including the development of other autoimmune disorders such as type 2 diabetes and multiple sclerosis.
The current treatment for celiac disease is a gluten-free diet, which means avoiding foods with wheat, rye, and barley. Even the smallest amount of gluten can trigger damage to the small intestine; therefore, it’s important to follow a strict diet.
Inflammatory Bowel Disease (IBD)
Inflammatory bowel disease (IBD) is a general term for illnesses that result from a frequent immune response and chronic inflammation of the gastrointestinal (GI) tract. The two most common inflammatory bowel diseases are ulcerative colitis and Crohn’s disease.
DEFINITION
The immune response is how your body recognizes and defends itself against bacteria, viruses, and substances that appear foreign and harmful.
IBD is the result of the immune system mistaking food, bacteria, and other materials that can be found in the intestines as foreign objects. The immune system triggers a response to attack the cells of the intestines. During this response, white blood cells are sent to the intestines, specifically the lining, where they cause chronic inflammation.
In Crohn’s disease, inflammation affects the entire digestive tract. Only the large intestine is affected in ulcerative colitis. Both illnesses are characterized by an abnormal response to the body’s immune system.
Ulcerative colitis causes sores and inflammation within the lining of the colon (large intestine) and rectum. While most cases are diagnosed before the age of 30, ulcerative colitis can affect people of any age. The cause of ulcerative colitis is unclear, although some studies show IBD results from genetic and environmental factors. When the body is exposed to antigens or foreign objects in the environment, it defends itself by producing inflammation. This reaction may be enough to “turn on” the immune system. When the immune system doesn’t properly “turn off,” inflammation continues to damage the body, and in this case, the large intestine. The primary goal for people with an inflammatory bowel disease is to keep their immune system healthy.
Almost half of all people with ulcerative colitis have mild symptoms. However, others may suffer from severe abdominal cramping, bloody diarrhea, nausea, and fever. The symptoms of ulcerative colitis can come and go, with fairly long periods in between flare-ups.
Complications can include bleeding from deep ulcerations, rupture of the bowel, or failure to respond to the usual medical treatments. Another complication is severe abdominal bloating. People with ulcerative colitis also have an increased risk of colon cancer. In over one fourth of patients with ulcerative colitis, medical therapy is not completely successful, and surgery may need to be considered to remove all or part of the colon (known as a colectomy). Ulcerative colitis is “cured” once the damaged colon is removed.
Unlike ulcerative colitis that affects a specific area of the GI tract, Crohn’s disease is an inflammation in any location throughout the digestive tract. The majority of patients with Crohn’s disease will require surgery at some point during their lives. Surgery becomes necessary in Crohn’s disease when medications can no longer control the symptoms.
According to the Crohn’s and Colitis Foundation of America (CCFA), as many as 700,000 Americans are affected by Crohn’s disease, with both men and women being equally affected. Crohn’s can appear at any age, but it’s more predominant among adolescents and young adults between the ages of 15 and 35.
As with ulcerative colitis, the causes of Crohn’s disease are not clearly understood. Current research shows that it can be hereditary, along with the environment contributing to the advancement of Crohn’s disease.
Symptoms for Crohn’s disease mimic other inflammatory bowel diseases, including abdominal cramping, bloody or fatty diarrhea, fever, and weight loss. Due to the inflamed area of the intestine, the system is unable to absorb nutrients properly. Additionally, much fluid is lost through diarrhea along with blood. As the individual has recurring flare-ups with the disease, nutrient deficiencies can develop, such as anemia.
Sometimes the GI tract can become so inflamed that it is necessary to allow it to rest. The person then must eat an liquid diet intravenously in order for the gut to have proper time to heal.
The first step in treating both ulcerative colitis and Crohn's disease is to replace lost nutrients and fluids. Diet recommendations may vary in each case, but it’s important to identify food triggers in order to minimize flare-ups. Overall, a high-calorie and high-protein diet, along with a multivitamin supplement, is typically recommended. In periods of remission, high fiber is recommended to increase bowel motility.
Irritable Bowel Syndrome (IBS)
It’s important to know that irritable bowel syndrome (IBS) is common and can be less severe than IBD. Doctors consider IBS a functional GI disorder. This basically means your digestive tract performs in an irregular way but without evidence of the digestive tract damage that occurs with inflammatory bowel disease.
IBS affects the large intestine and occurs when there is too much or too little movement of food within the colon. IBS is characterized by abdominal pain and discomfort along with changes in bowel movement patterns. In order to provide the right treatment to patients with IBS, doctors classify IBS into four categories based on stool consistency.
The four types of IBS are as follows:
- IBS with constipation: Hard or lumpy stools at least 25 percent of the time and loose or watery stools less than 25 percent of the time
- IBS with diarrhea: Loose or watery stools at least 25 percent of the time and hard or lumpy stools less than 25 percent of the time
- Mixed IBS: Hard or lumpy stools at least 25 percent of the time and loose or watery stools at least 25 percent of the time
- Unsubtyped IBS: Hard or lumpy stools less than 25 percent of the time and loose or watery stools less than 25 percent of the time
Physical problems such as the brain-gut signal, GI motility, bacterial infections, genetics, and food sensitivities may all contribute to the development of IBS. When the brain signals the nerves in the gut to digest food, there may be a miscommunication or abnormal response that causes IBS symptoms. These symptoms may include bloating, cramping, gas, alternating diarrhea and constipation, and mucus in the stool. IBS is also found to affect more women than men and usually occurs in people under 45 who have a family history or a mental health problem.
WAKE-UP CALL
Chronic diarrhea can lead to dehydration. A person can tolerate 3 to 4 percent loss of water but any higher than that can cause serious adverse health effects. It’s important to try to replace lost fluids, especially during an illness.
Leaky Gut Syndrome
Leaky gut syndrome occurs when there’s increased permeability within the intestines. This simply means that undigested food particles and toxins that would normally be blocked are able to flow into the bloodstream. These foreign particles and toxins cause the immune system to react, and often cause allergies. For example, if you eat a banana and you have leaky gut syndrome, bits of undigested banana will escape the intestines and find their way directly into the bloodstream. When this occurs, the immune system considers these particles a dangerous threat and reacts by producing antibodies and attacking healthy cells.
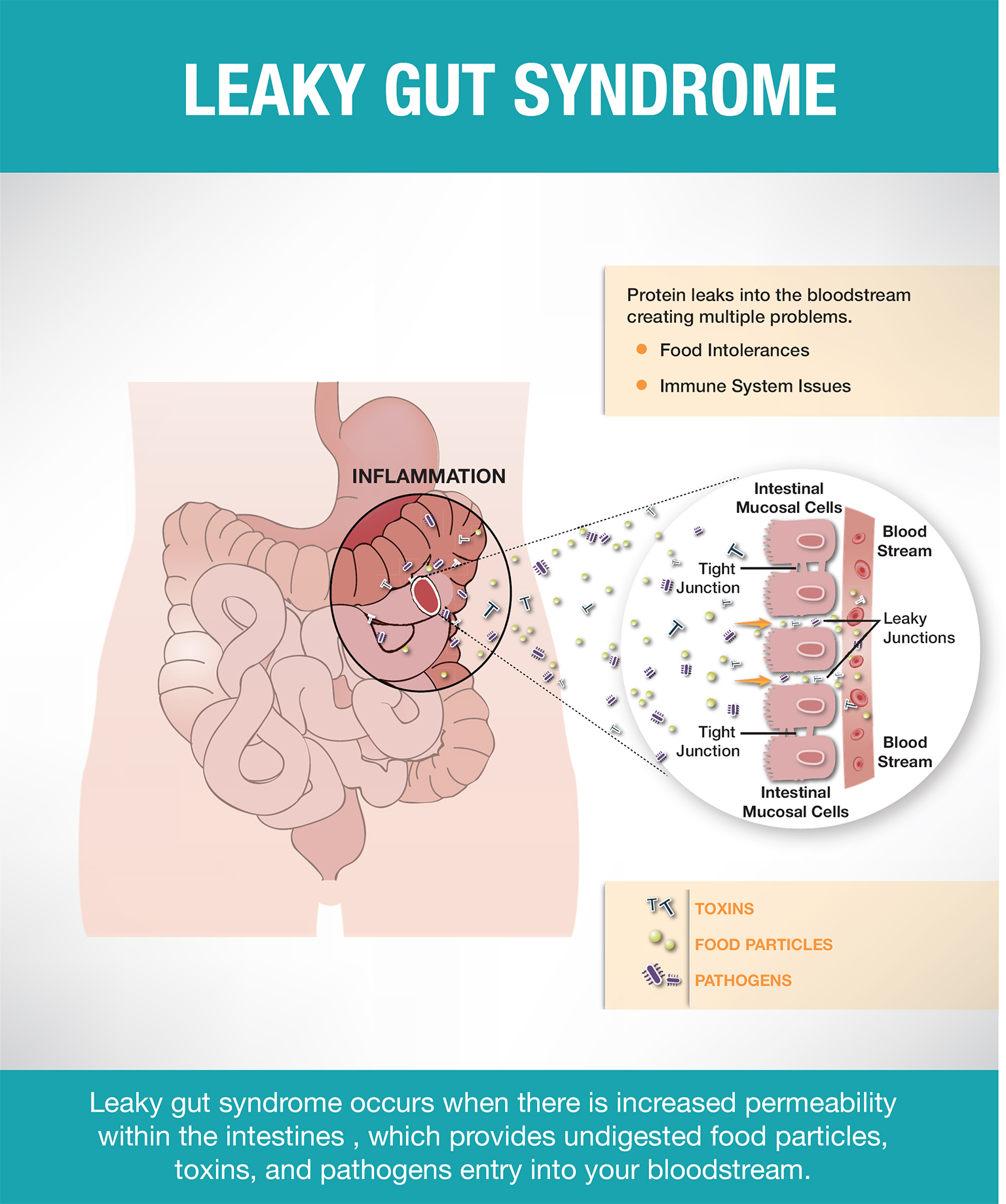
There are several factors that can lead to leaky gut. One reason may be chronic constipation due to toxins in your stools. Over time, these toxins can irritate your intestinal lining, which can lead to inflammation. The constant inflammation then causes pores within the intestines to expand, leading to increased permeability in the intestinal lining.
Another possible cause of leaky gut is the imbalance of healthy gut bacteria. When there is an imbalance between the “good” and “bad” bacteria, irritation and inflammation can occur.
Establishing a diagnosis for leaky gut syndrome can be tricky, as there is a wide range ofunrelated symptoms and no definitive tests to confirm. The symptoms may include gas, bloating, diarrhea, inflammation, chronic fatigue, diagnosed autoimmune disease, food allergies, or food intolerances. It has also been linked to medications such as aspirin and nonsteroidal anti-inflammatory drugs, which can irritate the bowel lining.
Lifestyle modification, including changing the diet and reducing stress, may be the best ways to treat leaky gut syndrome. Glutamine, an amino acid that can be taken in supplement form, may also protect the lining of the intestines, but clinical research is lacking and more results are needed in order to understand glutamine’s effect on digestion. Probiotics also can be added to your diet in order to balance healthy gut bacteria. Foods such as yogurt, kefir, or fermented foods can all help restore balance among healthy gut bacteria.
Malabsorption Syndrome
Malabsorption syndrome is the direct result of another disease or disorder that causes the intestines to not properly absorb certain nutrients. These diseases include gastrointestinal diseases, such as Crohn’s and celiac disease, but also AIDS/HIV, chronic liver disease, and treatment from radiation, certain types of cancer, parasitic infections, and some medications.
When any of these diseases or disorders occurs, the small intestine is damaged and inflamed. Since proteins, carbohydrates, fats, and fluids are absorbed in the small intestine, a person with any of these disorders will most likely suffer from malabsorption syndrome because the intestines simply can’t absorb those important nutrients and fluids. Many of these conditions also cause the body to be incapable of producing certain enzymes needed to digest food.
NOTABLE INSIGHT
Traveling abroad to Southeast Asia, the Caribbean, and India can lead to malabsorption as in the case of tropical sprue. It is caused by toxins in foods, infection, or parasites and can lead to anemia, diarrhea, sore tongue, and weight loss.
Recognizing the signs and symptoms of malabsorption is crucial for people with these disorders. Some symptoms include low blood pressure, weight loss, fatty stools, fluid retention, bloating, diarrhea, anemia, and weight loss. Other risk factors can include excessive alcohol consumption, family history of cystic fibrosis, intestinal surgery, and travel to Southeast Asia, the Caribbean, and India. A diagnosis of malabsorption syndrome can be easily confirmed by a biopsy of the small intestine or through blood work.
The first steps to manage and treat malabsorption syndrome start with nutrient and fluid replacement. In extreme cases, hospitalization is sometimes necessary if sufficient nutrient loss occurs. Diet is key to recovery, and small meals should be eaten throughout the day. The recovery diet should be rich in carbohydrates, fats, minerals, proteins, and vitamins. It’s also important to stay hydrated.
NOTABLE INSIGHT
One easy way to recognize if you’re drinking enough fluids is to look at the color of your urine. It should be the color of light yellow lemonade.
Gut Support with Probiotics
A healthy GI tract contains trillions of healthy or “good” bacteria, which help maintain a natural balance between healthy and unhealthy bacteria. Probiotics are healthy bacteria, and live cultures are found in fermented dairy products and foods. Yogurt and kefir typically contain lactobacillus, bifidobacteria, and other strains. These healthy bacteria may help strengthen your immune system, reduce the risk of certain cancers, decrease inflammation as with IBS, and help with other nonspecific forms of diarrhea.
Prebiotics are nondigestible carbohydrates, such as plant fiber, that assist in growth of existing bacteria in the colon. Oligosaccharides and inulin are common types. When the naturally occurring healthy bacteria are out of balance due to long-term use of antibiotics or poor diet, it’s a good idea to replenish the good bacteria. Fermented foods that contain probiotics, such as yogurt and kimchi, along with prebiotics like legumes, whole grains, and garlic, are good choices.
Water: An Essential Nutrient
Water is part of every chemical reaction that takes place in the body. You can only survive for about a week without water as opposed to several weeks without food. The function of water is to transport nutrients, oxygen, and waste throughout the body. It also helps to regulate body temperature, lubricate joints, protect organs, and relieve constipation.
The majority of water in the body can be divided into cellular and intracellular. Cellular water is found inside the cells, and intracellular water is found between the cells. Water helps facilitate the movement of molecules. The human body weight ranges from 45 to 75 percent water depending on age, sex, and level of body fat. Infants are about 75 percent water. An obese person with higher body fat will have less water than those with high muscle content.
On average, adults lose about 2½ to 3 liters of water per day. Water loss can occur through regular bodily functions such as maintaining body temperature, sweating, going to the bathroom, and breathing.
Fluid homeostasis in your body is regulated very closely. It involves the kidneys, lungs, liver, adrenal glands, and the thirst centers of your brain. Each works in conjunction with the other to release hormones and electrolytes in order to maintain the fluid stores.
Recommended intake for water is 1 milliliter per calorie. For example, if you consume 2,000 calories per day, you need approximately 2,000 milliliters or 2 liters of water per day. Of course, this amount varies based on your activity level and your environment.
Common symptoms of dehydration are dizziness, headache, weakness, fainting, dry mouth and cracked lips, increased thirst, decreased urine output, and dark-colored urine.
Water is an essential nutrient for your body and it’s important to consume an adequate amount each day. Most fluids you drink will count toward your fluid goals. Water from beverages like coffee, tea, and milk can count toward your goal, too. Highly caffeinated beverages can cause a slight increase in fluid output, but the body quickly adjusts.
The only beverages that don’t count toward fluid needs are alcoholic beverages such as wine, beer, and hard liquor. These have a diuretic effect and promote the production of urine. It’s a good idea to drink one glass of water per alcoholic beverage to maintain your hydration levels. Foods such as fruit and vegetables contain water, too. Some are even considered to have high water content, such as cucumbers, melons, strawberries, and grapefruit. Other foods like soup can also count toward your daily needs.
WAKE-UP CALL
When increasing high-fiber foods in your diet, it’s important to drink more water. Some fibrous foods absorb water and can cause an unpleasant experience in the bathroom: constipation.
Can You Drink Too Much Water?
Overconsumption of water is rare. A person would have to drink 10 to 20 liters of water over several hours, which would lower the sodium levels in the body and cause hyponatremia. This condition would lead to swelling of the brain, coma, convulsions, and possibly even death. Individuals at the greatest risk are endurance athletes, those with mental illnesses such as schizophrenia, and infants who receive only water instead of formula.
- Digestion is a complex process that allows you to absorb the vital nutrients from foods you eat.
- Food should never cause you pain. If pain is persistent, it can lead to serious digestive disorders and diseases. Be sure to seek medical help if this occurs.
- Include fermented foods such as yogurt, kimchi, and kefir in your diet to build up a healthy bacterial colony in your gut.
- Water is vital for good overall health. It’s important to be sure to meet your water goal each day.