[1] Watkins A.E, Scheaffer R.L, Cobb G.W. Statistics in Action: Understanding a World of Data. Wiley publishers; 2004.
[2] United Nations, World Population Ageing, Economic and Social Affairs; 2013.
[3] Hicks J. Hector: Robotic Assistance for the Elderly, Forbes Magazine. 2012. http://www.forbes.com/sites/jenniferhicks/2012/08/13/hector-robotic-assistance-for-the-elderly/ (accessed 27 January 2015).
[4] Wang F, Turner K.J. Towards Personalised Home Care Systems. In: Maglogiannis I, ed. Proceedings of the 1st International Conference on Pervasive Technologies related to Assistive Environments, L2.1-L2.7, ACM, New York, USA. July 2008.
[5] Overby C.L, Tarczy-Hotnoch P. Personalized medicine: challenges and opportunities for translational bioinformatics. Per Med. 2013;10(5):453–462.
[6] Tawfik H, Zhou S, eds. Special Issue on User-centred Health Informatics. Int J Healthcare Technol Manag; 2012.
[7] Brynjolfsson E, McAfee A. The Big Data boom is the innovation story of our time, Atlantic. 21 November, 2011. http://www.theatlantic.com/business/archive/2011/11/the-big-data-boom-is-the-innovation-story-of-our-time/248215/ (accessed 25 January 2015).
[8] Lohr S. The age of Big Data. New York Times. 11 February, 2012. http://www.nytimes.com/2012/02/12/sunday-review/big-datas-impact-in-the-world.html (accessed 03 February 2015).
[9] Pentland A. Social Physics: How Good Ideas Spread-The Lessons from a New Science. New York: Penguin; 2014.
[10] Maiden N, et al. Computing Technologies for Reflective, Creative Care of People with Dementia. Communications ACM. 2013;58(11):60–67.
[11] McCormack B, McCance T. Person-Centred Nursing: Theory, Models and Methods. London: Blackwell Publishing; 2010.
[12] McCormack B. A Conceptual Framework for Person-Centered Practice with Older People. Int J Nurs Pract. 2003;9(3):202–209.
[13] Malanowski N, Ozcivelek R, Cabrera M. Active Ageing and Independent Living Services: The role of Information and Communication Technology, JRC Scientific and Technical Reports. European Commission. 2008.
[14] McCormack B, McCance T.V. Developing a Conceptual Framework for Person-Centred Nursing. J Adv Nurs. 2006;56(5):472–479.
[15] McCance T, McCormack B, Dewing J. An Exploration of Person-Centredness in Practice. Online J Issues Nurs. 2011;16(2).
[16] Edvardsson D, Fetherstonhaugh D, Nay R. Promoting a Continuation of Self and Normality: Person-Centred Care as Described by People with Dementia, Their Family Members and Aged Care Staff. J Clin Nurs. 2010;19(17–18):2611–2618.
[17] McCance T, Gribben B, McCormack B, Laird E.A. Promoting person-centred practice within acute care: the impact of culture and context on a facilitated practice development programme. Int Pract Dev J. 2013;3(1).
[18] Kitwood T. Dementia Reconsidered: The Person Comes First. Buckingham: Open University Press; 1997.
[19] Nolan M.R, Davies S, Brown J, Keady J, Nolan J. Beyond person-centred care: a new vision for gerontological nursing. J Clin Nurs. 2004;13(3a):45–53.
[20] Brooker D. What is person centred care? Rev Clin Gerontol. 2004;13(3):215–222.
[21] Augusto J.C, Nugent C.D, Martin S, Olphert C. Towards personalization of services and an integrated service model for smart homes applied to elderly care. In: Giroux S, Pigot H, eds. Proceedings of International Conference on Smart Homes and health Telematic. IOS Press; July 4-6, 2005:151–158.
[22] Morgan S, Yoder L.H. A Concept Analysis of Person-Centered Care. J Holist Nurs. 2012;30(1):6–15.
[23] Ebling M.R. Pervasive Change Challenges Elders. IEEE Pervasive Computing. 2014:2–4.
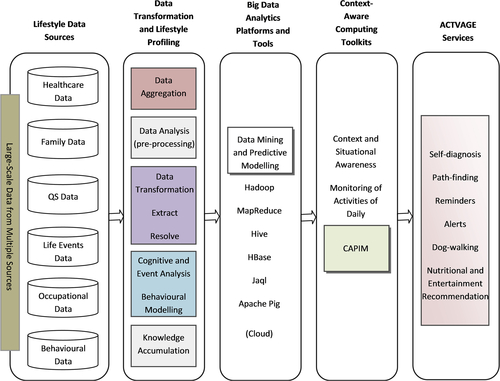
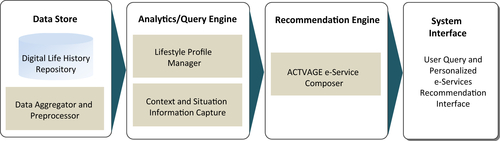
[24] Tawfik H, Anya O. Towards Lifestyle-Oriented and Personalised e-Services for Elderly Care. In: Proceedings of the 6th conference on Developments in eSystems Engineering (DeSE). UAE: IEEE; 2013:357–360. doi: 10.1109/DeSE.2013.69.
[25] Williams B, Grant G. Defining people-centredness: Making the implicit explicit. Health and Social Care in the Community. 1998;6(2):84–94.
[26] Mead N, Bower P. Patient-centredness: A conceptual framework and review of the empirical literature. Soc Sci Med. 2000;51(7):1087–1110.
[27] Armstrong D. A new history of identity: A sociology of medical knowledge. Basingstoke: Palgrave; 2002.
[28] Charness N, Boot W.R. Aging and information technology use: Potential and barriers. Curr Direct Psychol Sci. 2009;18:253–258.
[29] Chan M, Estève D, Escriba C, Campo E. A review of smart homes- present state and future challenges. Comput Methods Programs Biomed. 2008;91(1):55–81.
[30] Estève D. Questionnement sur l'organisation de la recherche et de l'action de terrain dans le développement des soins a domicile. Rapport LAAS Mars. 1997.
[31] Rogers W.A, Fisk A.D. Toward a psychological science of advanced technology design for older adults. J Gerontol Psychol Sci. 2010;65B(6):645–653.
[32] Rudder C. Dataclysm: Who We Are When We Think No One's Looking. New York: Crown Publishers; 2014.
[33] Chen L, Nugent C.D. Situation Aware Cognitive Assistance in Smart Homes. J Mobile Multimedia. 2010;6(3):263–280.
[34] Alam M.R, Reaz M.B.I, Ali M.A.M. A Review of Smart Homes—Past, Present, and Future. IEEE Trans Syst Man Cybern. 2012;42(6):1190–1203.
[35] Robles R.J, Kim T. Review: Context Aware Tools for Smart Home Development. Int J Smart Home. 2010;4(1):1–11.
[36] Demiris G. Electronic home healthcare: concepts and challenges. Int J Electr Healthcare. 2004;1(1):4–16.
[37] Brooks R.A. The Intelligent Room Project. In: Proceedings of the 2nd International Conference on Cognitive Technology (CT '97), Aizu, Japan. 1997:271–278.
[38] Cooper M, Keating D. Implications for the emerging home systems technologies for rehabilitation. Med Eng. Phys. 1996;18(3):176–180.
[39] Nisbet P. Integrating assistive technologies: current practices and future possibilities. Med Eng Phys. 1996;18(3):193–202.
[40] Cherry A.D, Cudd P.A, Hawley M.S. Providing rehabilitation integrated systems using existing rehabilitation technology. Med Eng Phys. 1996;18(3):187–192.
[41] Mozer M.C. The Neural Network House: An Environment that Adapts to its Inhabitants, Proc of the AAAI Spring Symposium on Intelligent Environments. Technical Report SS-98-02. AAAI Press: Menlo Park, CA; 1998 p. 110–4.
[42] Herbert J, O’Donoghue J, Chen X. A Context-Sensitive Rule-based Architecture for a Smart Building Environment. Int J Smart Home. 2009;3(1).
[43] Wactlar H, Bertoty J, Walters R, Hauptmann A. The Aware Community. Int J Smart Home. 2009;3(1):2009.
[44] Intille S.S. Designing a Home of the Future. IEEE Pervasive Computing. 2002:80–86.
[45] Páez D.G, Aparicio F, Ascanio J.R, Beaterio A. Innovative Health Services Using Cloud Computing and Internet of Things, Ubiquitous Computing and Ambient Intelligence. Lecture Notes Comput Sci. 2012;7656:415–421.
[46] Ou Y, Shih P, Chin Y, Kuan T, Wang J, Shih S. Framework of Ubiquitous Healthcare System Based on Cloud Computing for Elderly Living, Proc. In: of Signal and Information Processing Association Annual Summit and Conference (APSIPA). 2013:1–4 Asia-Pacific.
[47] Brownsell S, Bradley D, Blackburn S, Cardinaux F, Hawley M.S. A systematic review of lifestyle monitoring technologies. J Telemed Telecare. 2011;17(4):185–189.
[48] Gokalp H, Clarke M. Monitoring activities of daily living of the elderly and the potential for its use in telecare and telehealth: a review. Telemed J E Health. 2013;19(12):910–923.
[49] Bricon-Soufa N, Newman C.R. Context awareness in health care: A review. Int'l Journal of Med. Inf. 2007;76:2–12.
[50] Al-Bashayreh M.G, Hashim N.L, Khorma O.T. Context-Aware Mobile Patient Monitoring Frameworks: A Systematic Review and Research Agenda. J Software. 2013;8(7):1604–1612.
[51] Hong J, Baker M. Wearable Computing. IEEE Pervasive Computing. 2014:7–9.
[52] Ni Scanaill C, Carew S, Barralon P, Noury N, Lyons G.M. A review of approaches to mobility telemonitoring of the elderly in their living environment. Ann Biomed Eng. 2006;35:547–563.
[53] Rantz M.J, Marek K.D, Aud M, Tyrer H.W, Skubic M, Demiris G, et al. A technology and nursing collaboration to help older adults age in place. Nurs Outlook. 2005;53(1):40–45.
[54] Knight W. Your Retirement May Include a Robot Helper, Computing News. 2014. http://www.technologyreview.com/news/531941/your-retirement-may-include-a-robot-helper/.
[55] Cowley S.J, Kanda T. Friendly machines: Interaction-oriented robots today and tomorrow. Alternation: Int J Study Arts Humanities Southern Africa. 2005;12:79–106.
[56] Pineda L.A, Meza I.V, Avilés H.H, Gershenson C, Rascón C, Alvarado M, et al. IOCA: An Interaction-Oriented Cognitive Architecture. Research in Computer Science. 2011;54:273–284.
[57] Anya O, Tawfik H, Nagar A, Westaby C. An Ethics-Informed Approach to the Development of Social Robotics. In: Weir D, Sultan N, eds. From Critique to Action: The Practical Ethics of the Organizational World. Newcastle: Cambridge Scholars Publishing; 2011:231–253.
[58] IHTT. Transforming Health Care through Big Data. 2013. http://c4fd63cb482ce6861463-bc6183f1c18e748a49b87a25911a0555.r93.cf2.rackcdn.com/iHT2_BigData_2013.pdf.
[59] Davenport T. Big Data at Work: Dispelling the Myths, Uncovering the Opportunities. Boston: Harvard Business Review Press; 2014.
[60] Boyd D, Crawford K. Critical Questions for Big Data: Provocations for a Cultural, Technological, and Scholarly Phenomenon. Inform Commun Soc. 2012;15(5):662–679.
[61] Neff G. Why Big Data Won't Cure Us. Big Data. 2013;1(3):117–123.
[62] Gitelman L. “Raw Data” Is an Oxymoron. Cambridge: MIT Press; 2013.
[63] Carr N. The Limits of Social Engineering. MIT Technology Review. April 16 2014.
[64] Wang T. Big Data Needs Thick Data. Ethnography Matters. 2013. http://ethnographymatters.net/blog/2013/05/13/big-data-needs-thick-data/.
[65] Raghupathi W. Data Mining in Health Care. In: Kudyba S, ed. Healthcare Informatics: Improving Efficiency and Productivity. Boca Raton, FL: CRC Press; 2010:211–223.
[66] Raghupathi W, Raghupathi V. Big Data analytics in healthcare: promise and potential. Health Information Science and Systems. 2014;2(3). http://www.hissjournal.com/content/2/1/3.
[67] IBM. Data Driven Healthcare Organizations: Use Big Data Analytics for Big Gains. 2013. http://www-03.ibm.com/industries/ca/en/healthcare/documents/Data_driven_healthcare_organizations_use_big_data_analytics_for_big_gains.pdf.
[68] Wolf G. The Data-Driven Life. The New York Times. 28 April, 2010.
[69] Singer E. The Measured Life. MIT Technology Review. 2011. http://www.technologyreview.com/featuredstory/424390/the-measured-life/ (accessed 25 Feb 2015).
[70] Wolf G. The Quantified Self and the Future of Healthcare. The Health Care Blog. 2011. http://thehealthcareblog.com/blog/2011/05/12/the-quantified-self-and-the-future-of-health-care/.
[71] Sherman J. How Theory Matters: Benjamin, Foucault, and Quantified Self—Oh My!, EPIC Perspectives. 2015. https://www.epicpeople.org/how-theory-matters/ (accessed March 27 2015).
[72] Manyika J, Chui M, Brown B, Bughin J, Dobbs R, Roxburgh C, et al. Big Data: The Next Frontier for Innovation, Competition, and Productivity. McKinsey Global Institute. 2012.
[73] Hey T, Trefethen A.E. The uk e-science core programme and the grid, Future Gener. Comput Syst. 2002;18(8):1017–1031.
[74] Chen C.L, Zhang C.Y. Data-intensive applications, challenges, techniques and technologies: A survey on Big Data. Inform Sci. 2014;275:314–347.
[75] Jagadish H.V, Gehrke J, Labrinidis A, Papakonstantinou Y, Patel J.M, Ramakrishnan R, et al. Big Data and Its Technical Challenges. Commun ACM. 2014;57(7):86–94.
[76] Burghar C. Big Data and Analytics Key to Accountable Care Success. IDC Health Insights. 2012.
[77] Hinssen P. The age of data-driven medicine, Across Technology. 2012. http://datascienceseries.com/blog/download-the-age-of-data-driven-medicine.
[78] Dobre C, Xhafa F. Intelligent services for Big Data science. Future Generation Computer Systems. Jul 2014;37:267–281.
[79] Su C.-J, Chiang C.-Y. IAServ: An Intelligent Home Care Web Services Platform in a Cloud for Aging-in-Place. Int J Environ Res Public Health. 2013;10(11):6106–6130.
[80] IBM. The Big Data and Analytics Hub. 2014. http://www.ibmbigdatahub.com/infographic/four-vs-big-data.
[81] Zicari R.V. Big Data: Challenges and Opportunities. In: Akerkar R, ed. Big Data Computing. Boca Raton, FL: Chapman and Hall/CRC; 2013:564.
[82] Marz N, Warren J. Big Data: principles and best practices of scalable realtime data systems. Manning. 2012.
[83] Dey A.K. Understanding and Using Context. Pers Ubiquitous Comput. 2001;5:4–7.
[84] Coutaz J, Crowley J.L, Dobson S, Garlan D. Context is key. Commun ACM. 2005;48:49–53.
[85] Dey A.K, Abowd G.D, Salber D. A conceptual framework and a toolkit for supporting the rapid prototyping of context-aware applications. Hum Comput Interaction. 2001;16:97–166.
[86] Henricksen K. A Framework for Context-aware Pervasive Computing Applications. University of Queensland; 2003.
[87] Dourish P. What We Talk About When We Talk About Context. Pers Ubiquitous Comput. 2004;8(1):19–30.
[88] Sokol L, Ames R. Analytics in a Big Data Environment, IBM. Redbooks. 2012.
[89] Dobre C. CAPIM: A Platform for Context-Aware Computing, Proc. of International Conf. on P2P, Parallel, Grid. Cloud and Internet Computing. Oct. 2011;266:26–28.
[90] García A.O, Bourov S, Hammad A, Hartmann V, Jejkal T, Otte J.C, et al. Data-intensive analysis for scientific experiments at the large scale data facility. IEEE Symposium on Large Data Analysis and Visualization (LDAV). 2011:125–126.
[91] Beyer H. User-Centered Agile Methods. Hum Centered Inform. 2010;3(1):1–71.
[92] Tambouris E, Vintar M, Tarabanis K. A life-event oriented framework and platform for one-stop government: The OneStopGov project. In: Proceedings of Eastern European eGov Days Conference. 2006.
[93] Wu L.L. Event History Models for Life Course Analysis. In: Mortimer Jeylan T, Shanahan Michael J, eds. Handbook of the Life Course. New York: Kluwer Academic/Plenum Publishers; 2003:447–502.
[94] Prince M, Bryce R, Albanese E, Wimo A, Ribeiro W, Ferri C.P. The global prevalence of dementia: a systematic review and metaanalysis. Alzheimers Dement. 2013;9(1):63–75.e2.
[95] De Chaudhury M, Counts S, Horvitz E.J, Hoff A. Characterizing and predicting postpartum depression from shared facebook data. In: Proceedings of the 17th ACM conference on Computer supported cooperative work & social computing. New York: ACM Press; 2014:626–638.