Chapter 8
Food Additives, Drug Residues, and Food Contaminants
The food that to him now is as luscious as locusts, shall be to him shortly as bitter as coloquintida.
W. Shakespeare
Food Additives
Food and Drug Regulations
All developed countries have regulations governing the ingredients and additives that can legally be present in foodstuffs. The nature of the regulations may vary from country to country, but those of Canada are fairly typical.
In Canada, regulations governing foodstuffs and food additives are part of the Food and Drug Act and are enforced by the Health Protection Branch of Health Canada (http://www.hc-sc.gc.ca). The following are some important definitions:
Food: Any substance, whether cooked, processed, or raw, that is intended for human consumption including drinks, chewing gum, and any substance used in the preparation of a food, but not including cosmetics, tobacco, or any substance used as a drug. This definition includes food additives.
Food additives: Any substance, including any source of radiation, the use of which results in, or may reasonably be expected to result in, it or its by-products becoming a part of, or affecting, the characteristics of a food. This definition does NOT include
- Any nutritive material that is commonly recognized or sold as a food
- Vitamins, minerals, and amino acids
- Spices, seasonings, natural flavorings, essential oils, oleoresins, and natural extracts
- Accidental contaminants such as pesticides, or drugs administered to farm livestock
- Food packaging materials or components thereof
The regulations lay out which food additives are permitted, in what foods they may be used, and what are the maximum allowable amounts. A food additive must do at least one of the following:
- Maintain nutritive value
- Extend shelf life
- Prevent spoilage during shipment
- Enhance appearance or palatability
- Assist in the preparation of the food or in the maintenance of its physical form
The Health Canada website lists nearly 400 substances that can be used as food additives. It has been estimated that about 1 billion lb of food additives are consumed annually in North America, or about 3.5 lb (1.6 kg) per person. The vast majority of these are harmless, but demonstrated toxicity in some experimental animals for some and public concern about harmful effects of man-made chemicals have created pressure on governments to tighten up regulations controlling their use and establish stricter limits on allowable levels in foodstuffs. As is the case for any xenobiotic, the use of such agents should only be undertaken on the basis of a cost/benefit analysis. If the advantage is trivial, such as enhancement of texture, then any associated risk would be unacceptable. On the other hand, prevention of spoilage or of the growth of pathogenic microorganisms might justify the acceptance of a slight risk. It is this area that generates the greatest conflict between environmental groups and growers’ and manufacturers’ lobbies, who may differ markedly on the definition of acceptable risk.
Some Types of Food Additives
Food additives are used for a variety of purposes. The following are some of the major ones:
Acidifiers or acidulants provide tartness and act as preservatives by lowering pH. They may also improve viscosity.
Adjuvants for flavor facilitate the action of the principal flavoring agent.
Aerating agents (propellants, whipping agents) are used to produce a foam as in whipped toppings, etc.
Alkalies control pH, neutralize high acidity foods (tomato products, some wines), and may improve flavor.
Antibiotics are used to prevent bacterial spoilage during storage and transportation.
Anti-browning agents prevent oxidation on the surface of some foods such as lettuce may cause brown spots.
Anticaking agents are added to powdered or crystalline products (drink mixes, powdered spices, salt, cake mixes, etc.) to prevent caking (formation of lumps).
Anti-mold agents are added to foods (bread, baked goods, dried fruit, cheeses, chocolate syrup) to prevent mould growth. They are also called antimycotic or antirope agents (liquid or viscous products that become moldy are described as being “ropy”).
Antioxidants prevent the oxidation of fatty acids that causes rancidity, and of vitamins that lose potency.
Anti-staling agents prevent bread, etc., from going stale.
Binders are substances used to maintain “body” and hold a product together (e.g., processed meat, snack foods).
Bleaching agents are used to whiten flour, some cheeses.
Buffers are used in many processed foods.
Chelators or sequestrants are used to bind metallic ions that can hasten oxidation of fats and shorten shelf life.
Coating agents (glazing or polishing agents) are used to coat the skins of fruits and vegetables to prevent bruising, drying or spoilage, and to coat candies and tablets.
Defoaming agents (antifoaming agents, surfactants) are used to prevent excessive foaming in beverages when bottle filling.
Emulsifiers disperse fat droplets in an aqueous medium, for example, salad dressings, milk shakes, whipped cream, and toppings in pressure cans.
Extenders (fillers) are natural substances (casein, starch, soybean meal) used to add bulk to a food product.
Fixatives maintain the color of meat and processed meat.
Flavor enhancers intensify the natural flavor in soft drinks, fruit drinks, jams, and gelatin desserts.
Flavors (artificial): Any flavoring that does not occur in nature, even if the ingredients are all natural, is defined as an artificial flavor. When something is described as “chocolatey” rather than as chocolate, it indicates that the flavor is artificial, not natural, chocolate. This advertising ploy gets around the regulations prohibiting false advertising and it is widely used in North America.
Food colors are added to many products, including some fruit (oranges) to restore color lost in processing or transportation. Most (90%) are synthetic. Food colors that are bound to aluminum hydroxide are known as lakes. All synthetic food colors are highly water soluble. Only vegetable dyes are lipid soluble. This, of course, affects their absorption from the gastrointestinal tract. See in the following regarding artificial food colors.
Fumigants are toxic gases used to kill pests in harvested, dried grains, and nuts.
Fungicides prevent fungal growth on the surface of some fruits.
Humectants (hydroscopic agents) retain moisture and prevent drying in some candies and in ice cream.
Maturing agents (dough conditioners): Flour is better for baking if it is aged. Bleaches and other agents speed up the process.
Plasticizers (softeners) are used in chewing gum, candies, and edible cheese coatings to maintain pliability.
Stabilizers (suspending agents) prevent cocoa, orange pulp, and solids in ice cream from settling out.
Sweeteners (nonnutritional, artificial): There are many applications in low-calorie and diabetic diets.
The aforementioned is a partial list of the uses of food additives. It is probably unrealistic to expect that the use of such agents, many of which are synthetic chemicals, can be completely eliminated. Some of them at least are essential to allow the shipment of fresh fruit and vegetables over long distances as is necessary if these foods are to be available in countries with a short growing season. As is so often the case, public perceptions of risk cloud the issue of artificial food additives. Consumer advocacy groups continue to campaign for tighter controls on such agents. But when saccharin was banned because animal tests had shown the development of bladder tumors in rodents fed high doses, public outcry, originating from a perceived need for this product (vanity is a powerful motivator), resulted in a partial removal of the ban (see the following). It is now generally accepted that saccharin is not a carcinogen for humans. The remainder of this chapter will concentrate on the more common, or more controversial, food additives.
Artificial Food Colors
The common public perception is that synthetic food dyes are inherently more toxic than natural ones. In fact, they are highly purified chemicals, most of which have received extensive toxicity testing. Moreover, they are highly water soluble, so that absorption from the gastrointestinal tract is minimal. In contrast, natural dyes are complex mixtures of compounds that are generally more lipid soluble and therefore better absorbed. Since most natural food additives have been in use for decades, they are listed on the U.S. “Generally Regarded as Safe” (GRAS) list and have not been extensively tested. Most are lipid-soluble carotenoids (reds, oranges, and yellows) and are present in carrots, squash, yams, etc., and can be regarded as harmless. The possibility of an allergy to any food component cannot be discounted, however. Natural colors tend to be more subdued and to fade more quickly than synthetic ones. Thus synthetic colors are often preferred. (In Highland lore, “Ancient” tartans are those dyed with the original, more muted, vegetable dyes.)
Some synthetic dyes have been banned. Orange No. 1 and Red No. 3 caused diarrhea in children who consumed large amounts of candy, carbonated beverages, and other confections where these colors were used extensively. More recently, Red No. 2 (Amaranth) was banned because embryotoxicity was demonstrated in rats.
Considerable controversy surrounds the question of whether synthetic food dyes contribute to hyperactivity in children. Dr. Benjamin Feingold postulated that artificial colors and flavors, together with “salicylate-like” natural substances (present in apples, oranges, peaches, raisins and many berries, and in cucumbers and tomatoes) contribute to behavioral problems such as shortened attention span, easy distractibility, compulsiveness, and hyperactivity. Several studies have been conducted to examine this problem. In one type, groups of children were fed the “Feingold” diet or a normal diet and crossed over to the alternate diet after several weeks. This is called a double-blind crossover study. Neither the observers nor the subjects are aware of the treatment group to which they were assigned. Behavior was rated subjectively by parents and teachers. In studies at the Universities of Pittsburg and Wisconsin, 25%–33% of hyperactive children showed improvement when shifted to the Feingold diet according to the parents’ ratings. Teachers’ ratings showed much fewer differences. Moreover, shifts from the Feingold diet to the normal one were not accompanied by behavioral changes. In other studies, children received the Feingold diet throughout the experiment, but doses of a blend of eight certified colors were added periodically. Doses were 26–150 mg. The latter corresponds to the intake of the 90th percentile of American children. Both subjective estimates of behavior and objective tests of behavior and learning performance were used. At levels above 100 mg in a Canadian study, there was a slight deterioration in learning in 17 of 22 hyperactive children but no change in behavior. Two of 22 were affected at 35 mg. An Australian study employing a parent questionnaire reported substantial improvement on the special diet whereas a similar U.S. study did not.
The debate over the role of artificial food colors in causing hyperactivity in children is ongoing. Most researchers are in agreement that attention deficit hyperactivity disorder (ADHD) has a complex etiology dependent on the interaction of several factors. Autism Spectrum Disorder (ASD) is a rapidly growing problem in the population. Both may benefit in some cases from dietary modifications. Research conducted in the 20 years following Feingold’s initial study yielded mixed results with some positive and some negative findings. There has been a resurgence of public interest in recent years, part of a general rejection of food additives. Public pressure prompted the British government in 2009 to request that food manufacturers remove most artificial food colors from their products. This action was likely motivated by a large 2007 study by McCann et al. involving 153 three-year-old children and 144 eight to nine-year-old children who were randomized to three groups. Two groups received a drink containing an artificial food coloring plus sodium benzoate and the third received a placebo drink. The results were based on observations by parents and teachers and the group concluded that the younger children had adverse behavioral effects after drinking mixture A, while the older children had adverse behavioral effects after drinking either mixture A or mixture B.
Nigg et al. conducted a meta-analysis of 24 publications studying effects of artificial food colors on ADHD and found evidence of notable effects but when corrected for publication bias the finding did not survive. The McCann study and renewed interest in the food color debate led the U.S. Food and Drug Administration to review existing evidence and hold a public hearing. Their conclusion was that there was nothing that warranted agency action.
The most reasonable conclusion after this decades-long debate is that there is a subpopulation of children with ADHD that is adversely affected by consumption of artificial food colors. Thus, this becomes a factor that parents of such children might want to consider in dealing with the condition.
Banned or Restricted Artificial Food Colors
Citrus Red No. 2 is restricted to surface use on oranges not to be processed. It has been shown to be carcinogenic in animals. Orange B is restricted to use in the casings of sausages and hot dogs. It is related to amaranth (Red dye #2). The manufacturer has discontinued production because of evidence of a carcinogenic contaminant. Red No. 40 was imputed to cause cancer but the evidence was ruled inconclusive. Yellow No. 5 (tartrazine) has been associated with allergic reactions, sometimes severe, and it is listed on the U.S. ingredients list (candies, desserts, cereals, dairy products). Cross-allergenicity with aspirin is common. Canada does not have a compulsory ingredients list. This is a matter of great concern to individuals, and their parents in the case of children, who have life-threatening allergies to foodstuffs and additives.
Blue Nos. 1 and 2, Green No. 3, and Yellow No. 6 are considered safe but WHO has raised questions about the adequacy of testing.
Emulsifiers
Carrageenin (Irish moss) is extracted from several species of red marine algae. It contains a variety of calcium, sodium, potassium and ammonium salts, plus a sulfated polysaccharide. It is widely used as an emulsifier and thickener in ice cream, milk shakes, and chocolate drinks. It keeps milk proteins in suspension. Estimated daily intake is 15 mg/person. Only the undegraded form is permitted. Rats fed 2000 mg/kg showed fetal deaths and young with underdeveloped bones. Increased vascular permeability and interference with complement have been shown experimentally. Although potentially serious, especially in ill people (complement is essential to the immune system) carrageenin is not well absorbed and the FAO/WHO Committee on Food Additives has established an acceptable level of 500 mg/day. Long-term testing is probably indicated. Furcelleran is a similar substance derived from a red seaweed and it is similarly used. Recent public concerns over the safety of food additives have raised again the issue of carrageenin’s safety, but reviews of the literature have confirmed its safety at the concentrations encountered. There is some justification in limiting its consumption by infants due to the fact that carrageenin acts as a bulk expander like all high-fiber substances. The safety issue is clouded by confusion over degraded carrageenin, now known as poligeenan, which has toxic properties but which is not approved as a food additive. Studies have shown that there is no significant degradation of Carrageenan in the gastrointestinal tract.
Brominated vegetable oil is also used as an emulsifier to keep flavoring oils in suspension in soft drinks. A study in 1976 indicated that the daily U.S. intake averaged less than 0.2 mg/person. These products have been in use for over 50 years but toxicology studies in the early 1970s showed that doses of 2500 mg/kg of cottonseed BVO caused, in rats, heart enlargement and fatty deposits in heart, liver, and kidney after a few days. Doses as low as 250 mg/kg caused fat deposition in the heart. Maximum daily intake for a child probably does not exceed 0.05 mg/kg but it may occur over a prolonged period. Corn oil BVO fed to rats and pigs at 20 mg/kg for weeks caused deposits of brominated fat in liver and other tissues. The UN joint FAO/WHO Committee on food additives recommended in 1971 that BVO not be used as an additive. The U.S. FDA removed it from the GRAS list pending further safety studies by the manufacturer. These were judged to be faulty by the FDA. It is still used as an emulsifier, however, in soft drinks in Canada and the United States. In 1997 Horowitz reported on an unusual case of bromism in California resulting from excessive consumption (2–4 L daily) of cola soft drinks. The patient presented with headache, fatigue, ataxia, and memory loss. Ptosis (drooping) of the right eyelid and loss of ability to walk followed. Hemodialysis was required to restore function. Bromism was common in the early twentieth century when bromides were used as sedatives.
Preservatives and Antioxidants
Butylated hydroxyanisole (BHA) and butylated hydroxytoluene (BHT) are synthetics used to prevent premature rancidity in oil- and fat-containing foods. Total daily intake for a child could approach 0.5 mg/kg, which is the maximum recommended by FAO/WHO. Animal studies have consistently shown that high doses (over 500× the average human consumption) caused liver enlargement and induction of microsomal enzymes. Less than this had no effect. Recent studies have revealed evidence of carcinogenicity in offspring of mice fed BHA. These agents may act as promoters through the enzyme induction mechanism. As free radical scavengers, these agents actually may have anticarcinogenic properties. Both the U.S. FDA and Health Canada have ruled that BHA and BHT are safe when used as directed both as a food additive and in cosmetics where they are also commonly used as antioxidants. Nonetheless, consumer resistance to food additives continues to generate objections to these agents. Limiting consumption in young children certainly will do no harm and may be a reasonable precaution. As is so often the case, it is a question of how much relevance should be attached to findings that suggest toxicity at high doses.
Sodium nitrate, sodium nitrite, and potassium nitrate are used as curing agents in meats such as bacon and smoked meats. They are always used in combination with salt. Nitrite also inhibits the growth of Clostridium botulinum, the organism responsible for botulism. Nitrate is converted to nitrite by bacterial and enzymatic action in the intestine. The average U.S. daily intake from food additives is about 11 mg. The major concern is that nitrites can combine with amines to form nitrosamines that are carcinogenic. This process is accelerated by cooking. However, it is important to note that nitrites from food additives account for less than 20% of daily intake, the rest coming from nitrates in drinking water and in vegetables such as celery, spinach, and other leafy vegetables. This is partly due to the use of nitrogen fertilizers and partly from natural sources. Saliva contains nitrate, perhaps providing over 100 mg/day to be converted to nitrites in the lower gastrointestinal tract through bacterial action. Thus the total nitrate load is about 90 mg from natural dietary sources, 100 from saliva and only 11 from food additives. The use of nitrates and nitrites is restricted to the minimum levels required to inhibit the growth of C. botulinum.
A particular concern has been the poisoning of infants by nitrates in well water. There are now thousands of such cases, and many deaths, reported because the formation of methemoglobin from nitrites from nitrates impairs the oxygen-carrying capacity of the blood. A high percentage of rural dwellers in North America and Europe draw their water supply from shallow wells supplied by groundwater. These are vulnerable to contamination by surface runoff and hence by nitrates from fertilizer. Typically, newborn infants in these rural areas would develop, after days or weeks, a syndrome that included cyanosis (blue baby), hypotension (nitrates and nitrites are potent vasodilators) and, eventually, coma and death. Most recovered when they were removed from the home and hospitalized. Invariably, these infants were being fed formula made with well water that contained 20–1000 ppm of nitrates. The latency period varied according to the degree of contamination. The conversion of nitrates to nitrites occurred as a result of bacterial action either in the well, or in the gastrointestinal tract of the infant, which is virtually neutral (pH 7±) and hence favorable to bacterial growth. With the decline in popularity of formula feeding and its replacement by breast-feeding, nitrite poisoning in infants has almost disappeared in North America.
In a rather perverse swing of the pendulum, there is now mounting evidence that dietary intake of inorganic nitrates and nitrites can have a protective effect on the cardiovascular system, reducing the risk of heart attack and stroke. It is proposed that the conversion of nitrite to nitric oxide, a potent vasodilator, helps to maintain vascular flow in the heart and brain. A Belgian study calculated the average daily intake of nitrate of 1.28 mg/kg bodyweight/day. The FAO/WHO recommends an acceptable daily intake (ADI) of 3.65 mg/kg bodyweight/day.
Artificial Sweeteners
Sodium saccharin is several hundred times sweeter than sucrose but leaves a bitter aftertaste. For many years it was the only sweetener in common use. The average daily intake is about 6 mg/kg but some individuals habituated to soft drinks may consume much more. Theodore Roosevelt first required a review of its safety in 1912. In the early 1970s, two studies, one by the FDA, reported that high doses (2500 mg/kg) caused an increase in the incidence of bladder cancer in rats. It was not known whether this was due to an impurity. In 1977 the Canadian Health Protection Branch confirmed that the saccharin was the causative agent, but only when rats were exposed in utero to high doses. It was concluded that saccharin is a weak carcinogen and probably a co-carcinogen, but public outcry blocked its recall in the United States. In Canada, it is available in tablet form in pharmacies but it cannot be used as a sweetener in prepared beverages or as a sweetener in restaurants. It was originally usually in combination with cyclamate (see the following), which originally was suspected as a carcinogen. It is also available in Great Britain. The International Agency for Research on Cancer, an agency of the United Nations, has not deemed it necessary to place saccharin on its list of proven carcinogens. It is doubtful if either agent poses a real risk.
Xylitol is a natural ingredient of many fruits and berries. It has the same caloric value as glucose but it does not affect blood glucose levels and so it can be used by diabetics. It does not cause caries because it is resistant to fermentation by plaque microorganisms. It has been used in “sugar-free” gum. Some evidence of carcinogenicity has been obtained in rats fed very high doses. Xylitol has been given i.v. to humans as a source of energy. Kidney, liver, and brain disturbances have occurred and some fatalities. Use in the United States has been voluntarily stopped pending a review. It has been replaced by aspartame. Sorbitol is another sugar substitute that is equal in calories to sucrose but which will not raise blood glucose levels. Its uses are the same as for xylitol. It is also used as a humectant in jellies, baked goods, and in canned bread to prevent browning. Nausea, cramps, and diarrhea have occurred in some individuals. Acesulfame potassium (an oxathiazinondioxide) was introduced in 1988 as a noncaloric sweetener. It is chemically similar to saccharin. No adverse reactions have yet been reported, but long-term safety is unknown.
Cyclamate was introduced as a sweetener after saccharin. It has the advantage of not leaving a bitter aftertaste. Both were included in the 1959 “Generally Regarded as Safe” (GRAS) list of the U.S. Food and Drug Directorate. Because cyclamate was fed along with saccharin in one study showing increased bladder tumors, it was removed from the GRAS list and it is not available in the United States or Great Britain, but it is in Canada because a Canadian study had shown saccharin to be the culprit. In May of 2000, the U.S. National Institutes of Health released its Ninth National Toxicology report on Carcinogens in which it dropped saccharin from its list as suspected carcinogens in light of recent studies that failed to show a clear association between the sweetener and cancer.
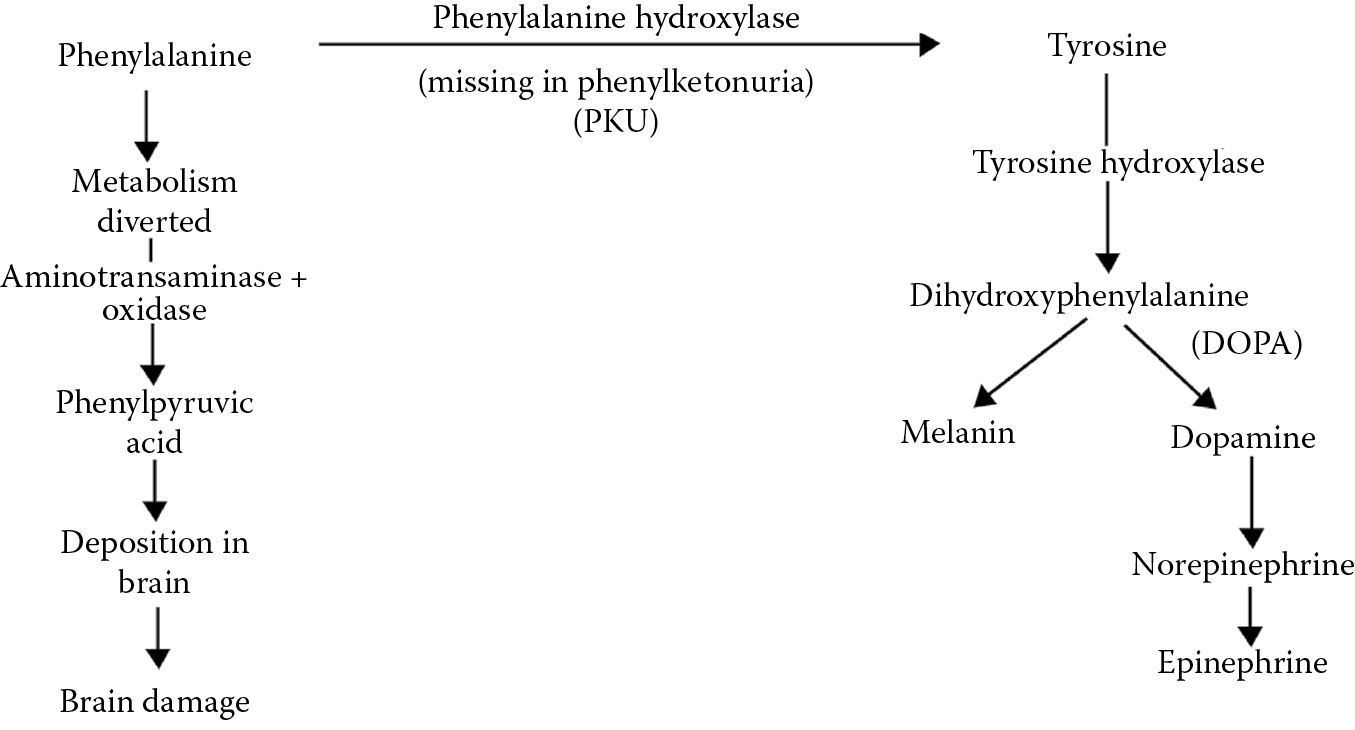
Aspartame is a dipeptide consisting of the amino acids aspartic acid and phenylalanine. Extensive testing has not revealed any carcinogenic potential and it has no aftertaste. It has largely replaced other sweeteners in soft drinks, gum, and other dietetic foods. It should not be used by people with phenylketonuria (PKU), a hereditary defect of the enzyme phenylalanine hydroxylase, which converts phenylalanine to tyrosine (Figure 8.1). These people use an alternate pathway that causes the accumulation of phenylpyruvic acid, which accumulates and deposits in the brain and causes mental retardation in infants. All newborns are tested for this and, if positive, are placed on a diet free of phenylalanine.
Since tyrosine is a precursor in the synthesis of catecholamine neurotransmitters, there was some speculation that high doses could cause behavioral changes but no evidence of this has been forthcoming in either children or adults.
An addition to this group is sucralose (trade name Splenda). It is a chemical modification of sucrose in which a number of H and OH groups are replaced by Cl. Sucralose cannot be broken down by digestive enzymes and it is not absorbed. Thus, it cannot enter metabolic pathways for glucose, it will not elevate blood glucose, and it provides no calories. It is rated as 600 times as sweet as sucrose. It has been pronounced safe by WHO and the Joint Expert Committee on Food Additives. In use for over a decade now, no adverse effects have been reported to date. A wide variety of products is presently in the laboratory testing stage of development, many of “natural” origin, and some of these will undoubtedly be making their appearance in the future.
One natural sweetening substance is stevia, from Stevia rebaudiana, known as sweetleaf or sugarleaf. It has been used as a sweetener in baking and elsewhere in South America for centuries. It is 200–300 times sweeter than sucrose and has been approved as an artificial sweetener in many countries including the United States and Canada. The United States has included it on the GRAS list. It has a negligible effect on blood glucose.
Flavor Enhancers
Monosodium glutamate (MSG) has been identified as the offending agent in the “Chinese Restaurant Syndrome.” Subjective symptoms of numbness and tingling of the mouth and tongue have been reported, but double-blind studies with doses up to 3 g failed to confirm an effect. It appears that certain individuals are highly sensitive. Because glutamate is an excitatory amino acid, MSG has been given in doses up to 45 g daily to mentally retarded patients with no behavioral changes or ill effects. Animal studies have shown hypothalamic lesions and infants under 6 months of age may be especially susceptible to MSG toxicity.
By far the most commonly used flavor enhancers and the ones responsible for massive amounts of ill health are sugar and salt. The total, adverse health effects of all synthetic food additives combined is trivial in comparison. Childhood obesity is epidemic in North America and type 2 diabetes is becoming so in adults. Cardiovascular disease is the leading cause of death if smoking-related cancer is removed from the comparison with cancer deaths. Children of the twenty-first century are believed to be the first generation whose life expectancy will be shorter than that of their parents. The finger of guilt for all this is pointed at the typical North American diet, which is overly rich in sodium and calories. Preprepared foods and fast foods are particular culprits. The American Heart Association recommends a maximum daily sodium intake of 1500 mg. There is convincing evidence that normal subjects who limit their sodium intake can delay or prevent the need for antihypertensive therapy.
The Northern Manhattan Study examined the role of sodium intake on the incidence of ischemic stroke. Patients were analyzed in groups according to their daily sodium intake in mg. These were: ≤1500, 1501–2300, 2301–3999, and ≥4000. Findings were adjusted for sociodemographics, diet, behavioral/lifestyle, and vascular risk factors. Follow-up period was 10 years. There were 235 strokes among the 2657 subjects. The relative risk of stroke was 2.59 times greater in the ≥4000 mg/day group as compared to the ≤1500 mg/day group and the finding was statistically significant. For every 500 mg/day increase in consumption there was a 17% increase in risk of stroke. The North Manhattan Study also examined the effect of dietary fat intake on stroke risk and found that an intake greater than 65 g/day increased the risk of stroke by 1.6-fold and the finding was statistically significant. Canada is no different. Health Canada calculates that the average Canadian consumes 3400 mg/day, more than double the recommended daily intake of 1500 mg. Table 8.1 lists the content of some common food items that could be found in most homes. It is worth noting that the values from product labels are given as a percentage of the maximum recommended daily intake from the Canada Food Guide. If one were to consume one serving of all of the products listed, a not-impossible feat, they would take in 2220 mg of sodium, almost the total maximum recommended limit. It is further worth noting that some of these food items would be considered to be part of a healthy diet. Another little deception practiced by the food industry is to round fractions down instead of up. Thus, a sodium content of 20.9% becomes 20% on the label, rather than 21%. No better illustration of the hidden nature of our sodium consumption could there be.
Sodium (Na) Content of Some Foodstuffs as Total mg and as a Percentage of the 2300 mg Maximum Daily Allowance*
|
Food Item |
Mg Na |
% Na* |
|
Two slices of ancient grains bread |
300 |
13.0 |
|
30 g of old cheddar cheese |
200 |
8.7 |
|
1 tablespoon of tomato ketchup |
140 |
6 |
|
16 pieces (85 g) of frozen French fries |
170 |
7.4 |
|
3/4 cup (188 mL) mixed frozen vegetables |
5 |
0.2 |
|
1 tablespoon (15 mL) calorie-wise dressing sauce (salad) |
140 |
6.0 |
|
1/2 cup (125 mL) frozen yogurt |
50 |
2.2 |
|
1 cup (250 mL) canned black beans |
270 |
12.2 |
|
2/3 cup (150 mL) beef broth |
550 |
20.9 |
|
1 cup (250 mL) “heart-healthy” soup |
480 |
20.9 |
* % of maximum daily allowance.
It should be noted that sodium is sodium, regardless of the source. MSG is a source and sea salt offers no advantages over table salt.
The consumption of sugar-sweetened beverages (SSBs) is believed to be a significant factor in the development of childhood obesity, which in turn, sets the child up for the future development of type 2 diabetes. Several studies have shown a positive association between the consumption of SSBs and weight gain in both children and adults. Since about 1985, the consumption of SSBs (mostly soft drinks) increased by about 300% in the United States with 56%–85% of schoolchildren consuming at least one drink daily. One can of soft drink contains about 65–70 g of sugar. It has been calculated that for every daily SSB consumed, the odd ratio for becoming obese is increased by 1.6. A school-based program in the United Kingdom designed to reduce consumption of SSBs was successful in preventing a further increase in obesity. In adult women, the consumption of SSBs has been associated with an increased risk of diabetes.
Of all the dietary factors that might concern a parent, including synthetic food additives and genetically modified foods, excessive sugar and salt intake by children are by far the ones that should give the greatest concern. Fortunately, there is some evidence that the consumption of SSBs in the United States has decreased in the last decade.
Drug Residues
The high-risk nature and narrow profit margin that are typical of the livestock industry have led to the extensive use of antibiotics, sulfa drugs, hormones, and other pharmaceuticals to improve productivity by increasing the rate or extent of weight gain per unit of food consumed. These pharmaceuticals are also used to prevent or treat disease. Many of the medications are also used in human medicine, others are unique to the agricultural field but they may have pharmacological or toxicological consequences for people as well. There are three main concerns about the possibility that traces of these substances might enter our food supply:
- They may serve as a source of allergic sensitization.
- Anti-infectives may contribute to the development of resistant strains of pathogenic bacteria.
- They may exert direct toxic manifestations such as teratogenesis and carcinogenesis.
While there is ample evidence that 1 and 2 occur, the occurrence of 3 is mostly speculative at least as far as drug residues in meat are concerned.
Antibiotics and Drug Resistance
In the late 1950s, Thomas Jukes of Berkeley University reported that the antibiotic tetracycline at 50 ppm in animal feed significantly improved the rate of weight gain and the gain-to-food consumption ratio in livestock. Subsequent studies showed that this effect was not related to the prevention of disease and occurred even under optimal conditions of husbandry and hygiene. The effect was confirmed later for other antibiotics and the mechanism remains elusive although it is believed that alteration of the bacterial flora in the gastrointestinal tract is involved. There is by now a long list of antibiotics and other anti-infective agents that has been employed as growth promotants. Antibiotics approved by Health Canada as growth promotants for livestock are shown in Table 8.2. Others may be used in other countries.
These Antibiotics Are Approved by Health Canada as Growth Promotants in Livestocka
|
Bacitracin |
Monensin |
|
Bambermycins |
Penicillin |
|
Chlortetracycline |
Salinomycin |
|
Lasalocid |
Tylosin |
|
Lincomycin |
Tylosin |
a Other countries may employ other antibiotics.
Antibiotics are also used to prevent the outbreak of disease. Prophylactic use involves higher levels than those used for growth promotion and a typical mixture for preventing dysentery in swine in the 1960s contained chlortetracycline 100 g/T of feed, sulfamethazine 100 g/T, and penicillin G 50 g/T. Concern over the potential dangers of drug residues in food mounted over the next two decades. It began with a report in 1959 from Japan of an outbreak of Shigella dysentery in a hospital nursery. The outbreak was unique in that the infecting strain of the bacteria was resistant to several antibiotics and sulfa drugs, some of which had never been used in that hospital. The term multiple drug resistance (MDR) was coined for this phenomenon and in the next few years many reports emerged of MDR in livestock, and in 1965 an outbreak of Salmonellosis in Great Britain resulted in six deaths. It was traced to the consumption of veal from calves that had been treated with several antibiotics and the organism demonstrated MDR. In 1971, the Swann Commission in the United Kingdom recommended greater controls over the use of antibiotics in livestock. Government legislation was passed and many other countries, including Canada, followed suit.
Infectious Drug Resistance
During this period it was discovered that the pattern of resistance typical of one type of bacteria could be passed to other, unrelated, bacteria and species, and the term infectious drug resistance (IDR) came into use. It is also called transferrable drug resistance.
For many years it was thought that IDR involved Gram-negative enteric organisms exclusively. Gram-negative refers to the histochemical staining characteristics of the bacteria (one of the major means of classifying them, it is related to the composition of their outer cell wall) and “enteric” refers to the fact that they are common inhabitants of the intestinal or enteric tract of both animals and humans. This group includes strains of Escherichia coli, Salmonella spp., Shigella spp., and Klebsiella spp. It is now known, however, that most, and possibly all, bacteria are capable of developing MDR through transference of genetic information from one cell to another. This includes the transfer of resistance genes from nonpathogenic organisms to pathogenic ones.
The mechanism of IDR hinges on the fact that bacteria possess extra-chromosomal units of genetic information called plasmids. These are rings of DNA that are capable of replication independent of the chromosomes and that can be passed intact from one bacterial cell to another. Genes can be inserted into these plasmids from other sources, including bacterial chromosomes, and this is dependent upon the existence of discrete sequences of 800–1800 base pairs of amino acids called insertion sequences. When a gene for drug resistance is included between two insertion sequences, the unit is called a transposon or, more often, an R (for resistance) factor. The existence of plasmids has provided the means for genetic engineering and the bacterial synthesis of human insulin and other substances. There are several methods by which plasmids can be transferred from one bacterial cell to another. These are as follows:
- Transformation. The lysis of a cell may release plasmids into the environment that may subsequently be absorbed by other cells. This is a highly species-specific phenomenon.
- Transduction. This involves the participation of phage viruses that incorporate bacterial genetic information and transfer it to other cells. This also is very species-specific.
- Conjugation. The plasmids of many bacteria possess a gene, called a fertility or “F” factor, which regulates a form of sexual reproduction. A fine tubule or “pilus” is formed between cells and intact plasmids may then be passed, along with their complement of genetic information, from one to the other. This process is not species-specific and it is the basis for IDR since R factors will be passed along as well. In this way, resistance genes may be shared amongst all enteric organisms that contact each other, and a multiple resistance pattern acquired. This process is illustrated in Figure 8.2.
The process of conjugation is clinically important because
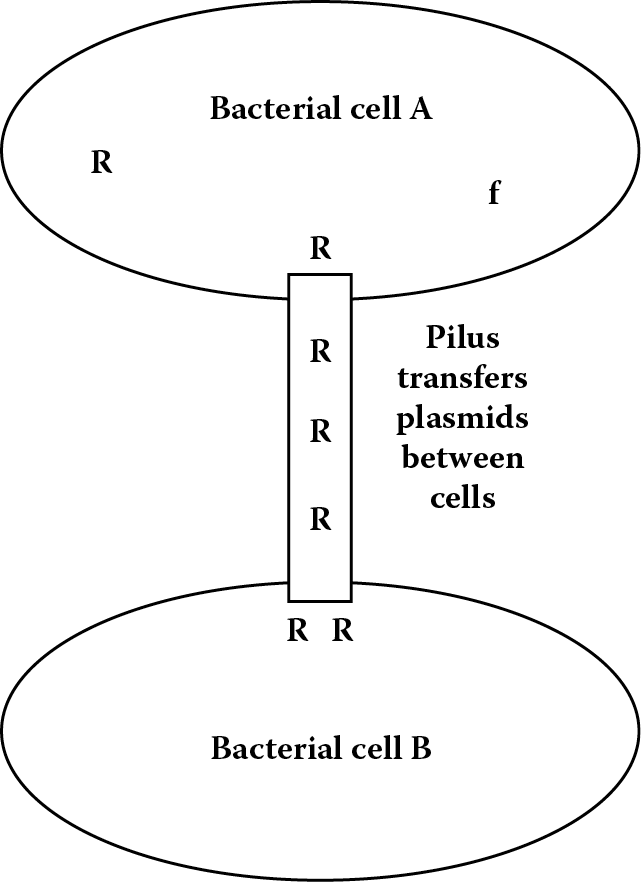
Bacterial conjugation and multiple (infectious) drug resistance. R = Resistance factor; f = Fertility factor.
- Nonpathogenic organisms may serve as a reservoir of drug resistance to be passed on to more virulent ones. There are few species barriers to transfer.
- The process of natural selection may, when an antibiotic is used therapeutically, result in the emergence of a strain of bacteria with MDR as susceptible strains are killed or inhibited.
- Resistance patterns, or resistant organisms, may be passed from animals to humans. Many organisms are infectious for both.
- The process is favored by exposure to low (nontoxic) levels of antibiotics.
The problem is attempting to strike a balance between the need to maximize production in the livestock industry, and thus keeping food costs down, while protecting the consumer from undue health risks. A study conducted in 1983 claimed that for an investment of $271 million in animal feed additives the American consumer saved $3.5 billion in food costs. Concern over the problems associated with antibiotics as food additives has resulted in a shift to hormonal ones (see the following). In 1984 the U.S. Centers for Disease Control issued a report on 52 outbreaks of Salmonellosis between 1972 and 1983. The source of the infection was identifiable in 38 of these and in 17 (44%) it could be traced to food animals (poultry, veal, and hamburger). These accounted for 69% of all outbreaks involving strains with MDR. The mortality from these strains was 4.2% versus 0.2% from nonresistant strains. In March and April of 1985 the most massive outbreak of Salmonellosis in U.S. history occurred in Chicago, with 14,000 people eventually infected. There were only two deaths, yielding a mortality of 0.014%. This was markedly lower than the previous rates reported for either resistant or susceptible strains (the 4.2% mortality rate would have caused 588 deaths) and a follow-up revealed that over 16,000 people were eventually infected for a final mortality of 0.012%. Both fatalities, however, involved a tetracycline-resistant strain.
By 2012 there was less controversy as the link between animal-sourced drug-resistant infections by enteric organisms in people became more and more evident. Foodborne infections with pathogenic enteric organisms of animal origin have become a major public health concern. One such is the strain of E. coli O157:H7. This is the organism that caused the outbreak of enteritis in Walkerton because of contaminated well water (see Chapter 3). This strain frequently produces Shiga-toxin, transferred by plasmids from Shigella strains and a potent enterotoxin.
Early attempts to limit the development of resistant strains of bacteria centered on restricting their use as agricultural food additives to so-called nontherapeutic antibiotics or NTAs. This was done in Europe but it was soon discovered that NTAs could serve to select for antibiotic-resistant genes in pathogenic bacteria. As final confirmation of this, studies have shown that when the use of NTAs was abandoned the frequency of antibiotic-resistant bacteria dropped off dramatically. In one study, 73% of isolates from broiler chickens of Enterococcus faecium were resistant to avoparcin in 1995 when its use was discontinued. In 1996, the use of avoparcin was banned because of a link with vancomycin-resistant enterococci (VRE), an organism that has caused disastrous hospital infections. By 2000, the number of resistant strains had fallen to 5.8%. Other studies have found similar decreases after antibiotic use in livestock was discontinued.
Avoidance of meat is no guarantee that multiple resistance patterns can also be avoided. In one study, vegetarians had a higher frequency of MDR bacteria than did meat eaters. The use of manure as fertilizer for vegetables can serve as an efficient means of transfer when the vegetables are eaten raw. A 2012 study of soil that had been fertilized with chicken waste revealed that tetracycline resistance was detectable in soil organisms 2 years after the poultry farm had ceased operations. Meat packers and farm workers tend to acquire MDR patterns.
It must be remembered that the use of antibiotics in agriculture is not the only source of MDR strains. In one study, resistance patterns of coliform organisms in the sewage effluent from a general hospital, a psychiatric hospital, and a residential area were compared. The results are shown in Table 8.3. It is evident that the incidence of MDR closely parallels the use of antibiotics in a particular setting. Thus, it is higher in the general hospital than in either the psychiatric hospital or the residential area. Moreover, resistance to chloramphenicol, which is reserved for life-threatening situations where less toxic antibiotics will not work, was very low in all situations, but the correlation still held. In 1985 chloramphenicol was withdrawn as an approved drug for use in food animals.
Percent of Coliform Organisms Resistant to Chloramphenicol, Streptomycin, and Tetracycline
|
Effluent Source |
Chloramphenicol |
Streptomycin |
Tetracycline |
|
General hospital |
48.8 |
0.4 |
24.3 |
|
Psychiatric hospital |
9.5 |
0.03 |
0.04 |
|
Residential area |
0.6 |
0.0007 |
0.1 |
Resistance to antibiotics is not the only type of genetic information that can be passed in this manner by plasmid transfer. Resistance to metals and bacterial virulence also is regulated by plasmid genes. Both vertical (within a species) and horizontal (amongst species) transfer is now thought to be commonplace in the microbial kingdom. Even transfer between Gram-negative and Gram-positive organisms has been demonstrated.
One of the concerns regarding MDR is that nonpathogenic organisms can pass their transposable resistance to pathogenic ones. Sweden banned the use of all antibiotics as growth promotants for livestock in 1986, and the European Union banned tylosin, zinc spiramycin, and virginiamycin in 1998. In 1996, the U.S. government created the National Antimicrobial Resistance Monitoring System (NARMS) to monitor changes in susceptibility of pathogens from human and animal specimens, healthy animals, and carcasses of food animals. The 2010 NARMS report (http://www.cdc.gov/narms) focused on the emergence of resistance to nalidixic acid of nontyphoidal Salmonella. Nalidixic acid is an elementary quinolone and a forerunner to the fluoroisoquinolones such as ciprofloxacin, a drug of first choice for treating Salmonella infections. Nalidixic acid resistance correlated well with increased resistance to ciprofloxacin. MDR was also noted in many Salmonella organisms.
The question of antibiotic use for growth promotion has already created international trade disputes over the import/export of agricultural products.
Infectious Diseases
No discussion of environmental hazards would be complete without passing reference to the hazard of infectious diseases. Not only has the emergence of antibiotic resistance led to clinical problems in treating old diseases such as tuberculosis, which has developed MDR and is on the rise, but many organisms seem to be developing more virulent strains and new ones are emerging. The AIDS virus, the Hantavirus, the bacteria of Lyme disease, and Legionella, and the development of more virulent strains of enteric pathogens such as O157:H7 are but a few examples. Perhaps this should not surprise us, given the rapidity of cell division of bacteria and the adaptability that has allowed them to survive for eons. Next to malnutrition, infectious diseases are the leading cause of death worldwide. There is an obvious relationship between the two.
Allergy
Legislation in most Western countries prescribes withholding periods during which livestock may not be shipped for food following the administration of an antibiotic or other drug by any route. This is designed to prevent the entry of drug residues into the human food chain. One reason for this is the possibility that such residues could result either in allergic sensitization or in an allergic reaction in individuals who are already sensitive. Significant levels of drugs could remain at the injection site, which is usually a large muscle mass that also constitutes a preferred cut of meat. Certainly, prior to the introduction of withholding times such reactions did occur. Of the drugs used in agriculture, those with the highest allergic potential are the penicillins. Penicillin G is still available without prescription in many countries for use in livestock and it is commonly employed for the treatment of mastitis (udder infection) in dairy cattle. It may thus be present in milk, although testing procedures are usually mandated by law. The test is not specific for a particular drug but employs a strain of bacteria that is extremely sensitive to inhibition by almost all antibiotics. More recently enzyme-linked immunosorbant assay (ELISA) has been used.
It may be significant that in 30% of patients suffering severe allergic reactions when treated with penicillin have no history of previous exposure, suggesting that sensitization occurred through environmental exposure. Although allergic reactions from contaminated food are rare and difficult to trace, they may still occur when drug residues escape detection. Sulfa drugs may also be offenders in this regard.
Hormones as Growth Promotants in Livestock
Diethylstilbestrol
Diethylstilbestrol or DES is one of a number of synthetic estrogens first synthesized by Charles Dodds in 1938. Since the work was conducted under the auspices of the British Medical Research Council, the chemicals were not subjected to patent restrictions and they rapidly became widely available. As a group, they revolutionized endocrinology, made possible the development of oral contraceptives and had a major impact on the practice of gynecology. The possibility of sex without pregnancy and the consequent sociosexual revolution of the sixties can be attributed directly to the development of these compounds and their chemical manipulation by the pharmaceutical industry.
DES mimics natural estrogens but it is much more potent and more toxic, and it is effective orally, which natural ones are not. It is very cheap to produce and by 1939 it was already popular in the United Kingdom, France, Germany, Sweden, and North America. It was used to treat menopausal complaints, amenorrhea, genital underdevelopment, and to suppress lactation in mothers who did not wish to nurse their infants. By 1942, agricultural use had begun on a limited scale. Early studies showed that rats fed DES gained weight more rapidly with no increase in food consumption and subsequent tests in cattle yielded similar results. Moreover, the “marbling” (diffuse fat distribution) was greater and this was considered to be a desirable flavor enhancer at the time. Athletes were not the first to take steroids to increase weight gain.
By 1945 DES became the first hormonal substance to be used as a growth promotant in livestock. It was being widely used in beef and poultry production. There were two methods of administration. One was a feed additive and the other a slow release pellet that could be injected under the skin of a steer’s ear or the neck of a broiler chicken. The former method had the disadvantage of loss through spillage and the accidental ingestion by breeding stock caused some serious fertility problems. The necks and ears containing the remains of the pellet were supposed to be discarded at slaughter, but chickens are frequently sold with the necks attached, and in 1959, a report emerged of a 40-year-old male chef in New York who developed signs of feminization including loss of facial hair, mammary development, fat deposition of the female pattern, and a high voice. The problem was traced to the consumption of chicken necks taken from the restaurant and eaten as an economy measure. The use of pellet implants in poultry was banned that same year. The carcinogenic nature of estrogens has been known for some time. Experimentally, natural estrogens were shown to produce carcinomas of the vagina, cervix, and uterus in mice and carcinogenic potency was directly related to estrogenic potency. There were sporadic reports of DES inducing cancer in mice but in 1971 Herbst et al. reported a case of clear-cell adenocarcinoma in the vagina of a young woman who had been exposed to DES in utero. A DES registry was established in the United States and by 1984, 500 cases of clear-cell adenocarcinoma had been reported. It is now estimated that females exposed to DES in utero have somewhat less than a 1/1000 chance of developing it.
The use of DES in pregnancy was based on data indicating that it improved the vascularity of the uterus and promoted the synthesis of progesterone, both of which would help to maintain pregnancy in the face of a threatened abortion. Other conditions that have been causally associated with exposure to DES in utero include adenosis (a self-limiting condition involving the presence of cervical cells in the wall of the uterus), infertility, carcinoma of the cervix and vagina, and breast cancer. Cervical malformations occur in 18%–25% of DES daughters but most appear to correct themselves with age. Infertility is by far the most common problem experienced by DES daughters. Pregnancy may be difficult to achieve and maintain. DES daughters have now entered middle age, the possibility that increased frequencies of other forms of cancer might emerge cannot be discounted; however, the association with breast cancer is becoming more tenuous.
The fetal risks of exposure to DES appear to relate to the fact that the mechanisms that detoxify natural estrogens cannot handle DES. In rats, a glycoprotein called alpha fetoprotein binds natural estrogens but not DES. Its presence has not been confirmed in humans but human fetuses have a very active process for sulfonating natural estrogens that may be less effective for DES. Active metabolites of DES may have a high affinity for estrogen receptors in the reproductive system and oxidative metabolites may damage DNA. Reactive metabolites may form after attachment to the receptor by the action of peroxidase enzymes present in estrogen-dependent tissues.
Attempts by the FDA to ban the use of DES in beef cattle were blocked by court actions launched by the beef producers until 1979 when liver and kidneys from beef cattle showed significant levels of DES. Illicit use continued thereafter, and in 1980 the USDA conducted 115 prosecutions against violators. It must be emphasized that all of the health problems associated with DES in North America (barring the chef noted earlier) are of iatrogenic origin, that is, they arose from medical treatment. None has been attributed to the consumption of meat from treated animals. This has not been the case elsewhere.
In the late 1970s and early 1980s, two epidemics occurred in which infants and children under 8 years of age displayed signs of abnormal sexual development such as breast development and precocious puberty. In Puerto Rico over 600 children were involved. DES was available without prescription and meat inspection controls were poor. In Italy, high levels of DES were detected in baby foods, especially those containing veal. Several hundred infants were affected. Occurrences declined after 1979 due to tougher controls and greater public awareness. In 1985, the DES Task Force of the U.S. Department of Health and Human Resources released its findings. These were as follows:
- The risk of uterine carcinoma in situ was about twice as high in DES daughters as in nonexposed women (15.7/1000/year vs. 7.9/1000/year) although there were problems with the study.
- The risk of genital herpes also was about twice as high (11.8% vs. 6.3%).
- The risk of breast cancer was difficult to assess because of other predisposing factors.
The question of increased risk of breast cancer was addressed by an American multicenter epidemiological study. It compared over 3000 women who had DES prescribed during pregnancy with 3000 similar unexposed women. The risk of breast cancer/100,000 was 172.3 for exposed women and 134.1 for unexposed women. The rate increased markedly in both groups between 20 and 40 years post entry to the study. The results were statistically significant and it now seems conclusive that there is a real increase in the risk of breast cancer in DES-exposed women but probably not in their daughters.
A 2012 review of the DES problem by Harris and Waring reported significantly higher incidences in DES daughters of a host of gynecological and reproductive problems including infertility, spontaneous abortion, preterm delivery, loss of second trimester pregnancy, ectopic pregnancy, pre-eclampsia, stillbirth, early menopause, as well as increased incidences of intraepithelial neoplasia and breast cancer.
The psychological costs to DES daughters are difficult to assess but probably quite high. Increased incidences of psychiatric problems and suicide have been reported due to feelings of helplessness and frustration. Recently, one small report suggested a higher incidence of homosexual preference in DES daughters. It is well documented that experimental exposure to sex hormones before birth influences brain development and sexual behavior. In rats and guinea pigs, alpha-fetoprotein normally protects the brain from estrogens but it does not bind to DES and prenatal exposure resulted in abnormal patterns of sexual behavior.
There is statistical evidence that sons and daughters of DES daughters have an increased incidence of birth defects. Boys had a higher incidence of hypospadia, a condition in which the urethral opening is located on the underside of the penis. The story of DES is not over nor likely will be for some time as the consequences of its impact, both physical and psychological, on the third generation continue. It is again worth reminding readers that none of these were the result of its agricultural use. The removal of such use is a clear example of the implementation of the precautionary principle.
Bovine Growth Hormone
Currently, a controversy is centered on the use of growth hormones in food animals. Bovine somatotropin, or bovine growth hormone (BGH), is used both to promote growth in beef cattle and to increase milk production in dairy cattle. It is produced by recombinant gene technology (rBGH). Studies indicate that it can increase lean content by at least 5% and feed efficiency by 8%. In dairy cattle, it can prolong the lactation period by several weeks, leading to greater profit. The consumer, however, remains understandably leery of such use. As long as profit margins in agriculture remain narrow, the pressure to use growth promotants will remain strong. The use of growth hormone in the United States has resulted in attempts to ban American beef in the European Economic Community. Canada has not approved its use and issued a notice of noncompliance in January of 1999. This decision was based largely on evidence of adverse effects in cattle including increased incidences of mastitis, lameness, and reproductive problems.
Concerns relate mainly to the fact that dairy cows injected with rBGH produce more of the natural hormone peptide insulin-like growth factor-1 (IGF-1) and IGF-1 is secreted in milk. Increased blood levels of IGF-1 have been associated with an increased risk of breast cancer in women. The debate is focused on whether IGF-1 in milk can be absorbed from the gastrointestinal tract. As a polypeptide the expectation is that it would be broken down by proteolytic enzymes. Some authorities claim that this prevented by the presence of casein to which IGF-1 is bound. While high molecular weight polypeptides and proteins are not generally absorbed from the gastrointestinal tract, there is some evidence that this can occur in some people. Experiments in rats showed that they can absorb IGF-1 from their intestinal tract, which is of course quite different from the human one (see Chapter 1).
A British study, published in 1998, of 397 women with breast cancer and 620 controls found that in premenopausal women under 50 with the highest levels of IGF-1, cancer risk was increased sevenfold over controls. The relative risk for other premenopausal women was 2.88. There was no significant increase in risk for any other subgroup. There is also evidence that elevated serum IGF-1 levels are associated with an increased risk of prostate cancer. A case control study within the (U.S.) Physician’s Health Study involved 152 patients and 152 controls. There was a strong positive association between serum IGF-1 levels and risk for prostate cancer. Men in the highest quartile had a relative risk of 4.3. This association was independent of baseline prostate specific antigen (PSA) levels.
While it seems clear that increased IGF-1 levels constitute a risk factor for both breast cancer and prostate cancer, the extent to which the hormone can be absorbed from rBGH milk remains open at least for humans. Meanwhile, it would seem prudent to invoke the precautionary principle, especially as milk production in developed countries has a capacity already in excess of the demand.
Other Hormonal Growth Promotants
The removal of DES from agriculture was by no means the end of the use of anabolic female hormones as growth promotants. Currently approved for use in Canada, but only for beef cattle, are three natural ones, progesterone, testosterone, and estradiol-17β, and three synthetic ones, zeranol, melengestrol acetate, and trenbolone acetate (TBA). These may also be used in the United States.
Of particular interest is zeranol, a semisynthetic estrogen, which is related to the naturally occurring mycotoxin zearalenone and which may even occur as a breakdown product of it. Zearalenone itself is an endocrine disrupter (see Chapter 10 for more on mycotoxins) and a potential health hazard. This has complicated the identification of natural versus anthropogenic sources.
An Italian study published in 2008 looked at serum levels of zearalenone and its congener α-zearalenol (ZEAs) in 32 girls with central precocious puberty and found that 6 of them had high levels that correlated with height. Since the European Union (E.U.) banned zeranol as a growth promotant in livestock in 1981, the origin of the ZEAs presumably was natural.
A New Jersey study reported in 2011, examined urinary mycoestrogens in 163 girls 9 and 10 years of age (Jersey Girl Study) and looked for a possible relationship to body size and breast development. Mycoestrogens were detected in 78.5% of the girls and levels were associated with beef and popcorn intake. This is presumably (but not proven to be) because the Fusarium mold that produces zearalenone is a common contaminant of corn and zeranol is widely used in the United States as a growth promotant in beef cattle. Girls with urinary mycoestrogens tended to be shorter and less likely to have reached the onset of breast development. The authors concluded that ZEAs may exert antiestrogenic effects on prepubertal girls and that the subject merits a larger, longitudinal study.
Since ZEAs are anabolic substances they have the potential to be abused in the field of sports. A 2011 German study examined the problem of distinguishing natural versus self-administered substances in athletes. The authors noted that the illicit application of zeranol to livestock was a continuing problem in the E.U. Antidoping tests routinely monitor for zeranol and its major human metabolites zearalanone, 7β-zearalanol, as well as the mycotoxin zearalenone and its unique metabolic products α-zearalenol and β-zearalenol. They concluded that mycotic sources of ZEAs were a potential confounding factor in interpreting antidoping test findings.
Natural Toxicants and Carcinogens in Human Foods
Through the acquisition of folk knowledge, human beings have learned to avoid eating rhubarb leaves, daffodil bulbs, and other plants that contain toxic chemicals. Under some conditions, however, foods that are normally safe may become toxic, at least for some individuals, and carcinogens may be more prevalent in human foods than previously realized.
Some Natural Toxicants
Favism
The broad bean (Vicia fava) may induce acute hemolytic anemia in individuals with the hereditary defect glucose-6-phosphate dehydrogenase (G6PD) deficiency. This is especially true for those individuals with the Mediterranean phenotype. It is a problem primarily for males under 5 years of age. The exact nature of the mechanism remains obscure, but there is evidence that these individuals may be deficient in hepatic glucuronide conjugate and hence unable to detoxify the offending ingredient. Susceptibility in the same individual varies from time to time, and all those with the same defect are not necessarily affected.
Toxic Oil Syndrome
In 1981 in Spain, there was a remarkable epidemic that eventually affected over 20,000 people. In the first 12 months of the epidemic there were 12,000 hospitalizations and over 300 deaths. According to a review of the event 20 years later, the final count was over 20,000 people affected and over 1200 deaths in the affected cohort. It began in a small town on May 1, when a boy was admitted to hospital with acute respiratory failure that rapidly led to death. The epidemic peaked in June, at which time 2000 new cases were being reported every week. The patients usually presented initially with respiratory distress, cough, low-grade fever, oxygen deficiency, pulmonary infiltrates and pleural effusions, and a variety of skin rashes. Nausea and vomiting were sometimes present, as were enlarged liver, spleen, and lymph nodes. Virtually all patients had elevated eosinophil counts (>500 to >2000/mm3, normal value, 0–500/mm3). The condition often progressed to severe muscle pain, muscle and nerve degeneration, and even paraplegia.
An astute medical clinician traced the problem to the consumption of a cheap, unlabeled cooking oil sold as pure olive oil in the open markets in small towns and villages. The oil consisted of low-grade olive oil mixed with various seed oils including a rapeseed oil that was imported in a denatured form by mixing it with aniline to render it unfit for human consumption. Two significant clues were the facts that the condition affected low-income families almost exclusively, and nursing infants were never affected. Geographically, the epidemic was limited largely to central and northwestern Spain.
Chemical analyses of suspect oil samples, and comparison with nonsuspect samples, failed to reveal the presence of known toxicants such as heavy metals, but the suspect oil contained significant levels of aniline and fatty acid anilides, reaction products of the oil with the aniline. A dose–response relationship between the degree of contamination and the severity of signs and symptoms was also noted.
The toxicity of aniline is well known because of its heavy industrial use and although there are some similarities with the toxic oil syndrome, skin lesions for example, aniline toxicity involves CNS symptoms (vertigo, headache, mental confusion) and blood disorders including methemoglobinemia and anemia. It was felt, therefore, that the offending agent was likely a reaction product. To date, however, the syndrome has not been reproduced in an animal model. Twenty years after the event the exact etiology remains unknown. If fatty acid analides were indeed the source of toxicity they must have been extremely toxic as they were present in very small amounts.
Eosinophilia-Myalgia Syndrome
The toxic oil syndrome might be regarded as a historical curiosity if it were not for the fact that in 1989, a similar problem emerged in the United States. Called the eosinophilia-myalgia syndrome (EMS), it affected over 1500 people and it appeared to be caused by consuming contaminated L-tryptophan as a food supplement. Again, the eosinophil count was usually elevated above 2000/mm3. Like the toxic oil syndrome, there was also inflammation of muscles and their nerve supply. There was a notable absence of acute respiratory symptoms, unlike the toxic oil syndrome.
The Centers for Disease Control determined that the product came from one supplier and that it had a contaminant, the di-tryptophan aminal of acetaldehyde. This was either the toxic agent or a marker thereof as there was a strong association between the level of this substance and the incidence of the disease. The FDA banned the sale of L-tryptophan as a precaution in 1991. The incidence of EMS fell rapidly. The FDA ban was lifted in 2002 and some new cases have emerged.
Efforts at identifying the toxic agent and developing an animal model for the condition are continuing. Elevated levels of serum quinolinic acid have been recorded clinically in patients with EMS. Self-injection of quinolinic acid over a 1 month period resulted in an almost threefold rise in the eosinophil count, a common observation in EMS. A 2007 paper showed that 3-(N-phenylamino) alanine or PAA is activated by human liver microsomes. PAA was identified as one of the contaminants in the batch of L-tryptophan associated with the EMS outbreak. The paper identified a common toxic metabolite, 4-aminophenol that could have been generated by a common pathway in both EMS and toxic oil syndrome.
Herbal Remedies
In recent years there has been a tremendous upsurge of interest in, and use of, herbal remedies. One in five Canadians and one in three Americans indicated in a recent survey that they used herbals, often in conjunction with prescription drugs and often without informing any health care professional. This has created a five billion dollar industry with poor controls for efficacy and potency. The phenomenon appears to be another manifestation of the simplistic “natural is good, synthetic is bad” philosophy that arose following public concern over the presence of toxic chemicals in the environment. This concern was fuelled by episodes such as the Love Canal situation and perhaps by the emergence of “New Age” spiritualism. The attraction to herbals is mostly based on the assumption that, because they are natural, they must be safer. This assumption ignores the fact that, if they possess enough of the active ingredient to have a pharmacological effect, they must also carry the potential to cause adverse reactions and to interact with other pharmacological agents, including other herbals. Of course, if they do not possess such potency, they are unlikely to be effective. Since these preparations are presently defined as food supplements they are not subjected to the rigorous regulations governing prescription and patent medicines. Leaving aside the question of potency, which often is an unknown quantity, there is mounting evidence of the potential for some herbals to do harm. A wide variety of herbals possess diuretic activity with associated potassium loss. They may thus interact with prescription diuretics used to treat hypertension and cause excessive potassium loss and low blood pressure. St. John’s Wort, cherry stems, and parsley are but a few examples. Others may interfere with antihypertensive therapy and cause a dangerous elevation in blood pressure. Ephedra, the active ingredient of which is ephedrine, a known hypertensive agent, is present in natural weight loss products including fen-phen and these have been associated with over a dozen deaths and hundreds of cases of illness reported to the U.S. Food and Drug Administration. Licorice can cause pseudoaldosteronism in which sodium is retained, with a resulting increase in blood pressure. Numerous other products may depress blood pressure to dangerous levels in patients receiving antihypertensive therapy. Cat’s claw, devil’s claw, and garlic fall into this category. Rauwolfia serpentina is present in many natural products. Its active ingredient is reserpine, a potent depressor of blood pressure.
The agents listed earlier are but a small sample of the host of herbal agents with the potential to cause untoward side effects and drug interactions. Public demand for these products will force regulatory agencies to divert billions of dollars to analyze and test them, with the predictable result that many will be banned and others reclassified as drugs. This will no doubt lead to an even greater public outcry. For a more complete list of herbal remedies and their potential side effects and interactions with prescription drugs refer to Philp (2004).
Natural Carcinogens in Foods
Considerable evidence exists that bracken fern produces bladder cancer in cattle that eat excessive amounts when better fodder is unavailable, and in rats fed large amounts of it. Because the young shoots, called fiddleheads because of their curled shape, are eaten as a delicacy in many parts of the world, including Canada and Japan, there has been concern over the potential for carcinogenic effects in humans. Epidemiological studies, however, have failed to demonstrate such an association, and it is now felt that the eating of fiddleheads does not constitute a risk factor for cancer.
Natural carcinogens and precursors have been detected in many other foods. In their 1987 review, Ames et al. list the carcinogenic TD50 for nitrosamines present in many foodstuffs as 0.2 mg/kg for rats and mice. In contrast, PCBs, with a similar daily dietary intake of 0.2 μg, had Td values of 1.7–9.6 mg/kg in these species. Other substances shown to be carcinogens in animal tests, but for which evidence of a risk to humans is weak, include allyl isothiocyanate (in kale, cabbage, broccoli, cauliflower, horseradish, and mustard oil), safrol (nutmeg, cinnamon, black pepper) and benzo[a]pyrene (produced during cooking, especially charcoal broiling). By extremely conservative methods, the risk for benzo[a]pyrene has been estimated at 1.5/100,000 at high levels of consumption.
It has been stated that exposure to carcinogens is an unavoidable fact of life, but that the levels in foods are so low that further reductions would not have a significant effect on cancer incidence. This “bad news” is offset by the “good news” that there are probably many more anticarcinogens in natural foods than there are carcinogens. In one study of human dietary habits, individuals who ate meat but not vegetables on a daily basis had a colon cancer risk (per 100,000 population) of 18.43, those who ate vegetables but not meat on a daily basis had a risk of 13.67, whereas those who ate both had a risk of only 3.87. Vitamins A, C, and E and carotenoids have been shown to be protective against cancer, probably because of their antioxidant properties. Dietary fiber is protective, and even meat has been shown to have anticancer properties. Indoles and isothiocyanates present in cruciferous vegetables such as cabbage, cauliflower, broccoli, and Brussels sprouts have been shown to be anticarcinogenic.
Carcinogenic mycotoxins abound in nature and these will be dealt with in Chapter 10, and irradiated foods in Chapter 12.
Case Study 17
Three men were admitted to the emergency department of a large hospital, all suffering from similar symptoms. Inquiry revealed that they had just finished dining in a nearby Chinese restaurant. All had a severe headache, cardiac palpitations, facial flushing, vertigo (dizziness), and perfuse sweating. The symptoms commenced shortly after finishing their meal. Their faces and chests were reddened, blood pressures slightly below normal, and their pulses were quickened.
Q. What is the likely portal of entry of this apparent toxicant?
Q. Is this likely due to
- Food poisoning of bacterial origin
- Contamination with a pesticide
- A food additive
Q. In a call to the restaurant in question, the attending physician inquired as to whether the trio had consumed mushrooms or fish. Why was this question asked?
The response to the aforementioned question was no. It was revealed that many other patrons had eaten similar food without trouble, the exception being pork chow yuk. These three were the only ones to consume this dish.
Q. How can this information be helpful?
Review Questions
- For Questions 1 to 13 use the following code:
Answer A if statements a, b, and c are correct.
Answer B if statements a and c are correct.
Answer C if statements b and d are correct.
Answer D if statement d only is correct.
Answer E if all statements (a, b, c, d) are correct.
- With regard to diethylstilbestrol (DES):
- It was used mainly to synchronize the estrus cycle of dairy cows.
- It was given to livestock as a growth promotant in feed or as subcutaneous pellets.
- In North America and Great Britain its use as a feed additive for livestock resulted in significant human health problems.
- It was given parenterally to pregnant women to prevent impending abortion.
- Human health problems associated with diethylstilbestrol (DES):
- Have been reported in some countries in infants who were fed formula containing high levels of DES
- Affect women who were exposed in utero to high levels from their mother’s blood
- Generally involve abnormalities of the genitourinary system
- Have caused widespread problems in people who eat meat containing pellet residues
- With regard to Salmonella infection:
- It is commonly transferred to humans by eating or handling undercooked meat.
- It is most often a problem for the general public.
- It sometimes involves multiple drug-resistant strains.
- It has a high mortality rate in normal individuals.
- Which of the following statements is/are true?
- Estrogens, including DES, have been shown to be carcinogenic.
- Women exposed to DES in utero have an increased incidence of cervico-uterine deformities.
- DES is not metabolized significantly by the human placenta or fetus.
- The human fetus cannot deactivate natural estrogens.
- Regarding the use of antibiotics in agriculture:
- They are used exclusively for treating infections in animals.
- They may be used prophylactically to prevent infections in animals.
- There are no regulations governing their use in agriculture.
- Very low levels added to feed might have a growth-promoting effect.
- Multiple drug resistance is
- Characteristic of Gram-negative enteric bacteria
- Possible even when the organism has not contacted all of the anti-infective agents to which it is resistant
- Determined by extrachromosomal DNA
- Seen only in farm livestock exposed to antibiotics
- The process of bacterial conjugation
- Refers to the release of DNA from lysed cells
- Requires the participation of plasmids
- Refers to the transfer of DNA by phage viruses
- Requires the participation of an “F” (fertility) factor
- Which of the following statements is/are true?
- Salmonella infection is rarely a problem in nursing homes.
- The rank order of frequency for resistant forms of intestinal infections is general hospital > psychiatric hospital > extrahospital environment.
- Multiple drug resistance occurs only in enteric organisms from animals.
- The frequency of MDR increases with antibiotic exposure.
- The legal definition of food additives in most countries includes
- Vitamins
- Food colors
- Spices
- Nitrates
- 10. Which of the following substances used in or on foods have been associated with a high degree of allergic reactions?
- Tartrazine
- Carrageenin
- Sodium metabisulfite
- Saccharin
- 11. Which of the following statements regarding nitrosamines, nitrates, and nitrites is/are true?
- The major source of nitrosamines for people is the nitrates and nitrites used as meat preservatives.
- Nitrosamines have been shown to be carcinogens in animals.
- There are no natural food sources of nitrates and nitrites.
- Nitrates and nitrites inhibit the growth of C. botulinum, the cause of ptomaine poisoning.
- 12. Regarding artificial sweeteners:
- Individuals with phenylketonuria should avoid aspartame.
- There is no convincing evidence that aspartame in normal amounts causes behavioral problems.
- Saccharine has been shown to cause bladder cancer in rats exposed in utero to very high levels.
- Cyclamate or a metabolite is a proven carcinogen for humans.
- 13. Toxic oil syndrome
- Involves respiratory distress, eosinophilia, and myalgia
- Produced a high mortality rate in an outbreak in Spain
- Resembles a disease traced to tryptophan consumption in the United States.
- May be due to a reaction product of aniline and a component of a cheap, low-grade mixture of cooking oils
Answers
- C
- A
- B
- A
- C
- A
- C
- C
- C
- 10. B
- 11. C
- 12. A
- 13. E
Further Reading
Aarestrup, F.M., Seyfarth, A.M., Emborg, H.-D., Pedersen, K., Hendriksen, R.S., and Bager, F., Effect of abolishment of the use of antimicrobial agents for growth promotion on the occurrence of antimicrobial resistance in fecal enterococci from food animals in Denmark, Antimicrob. Agents Chemother., 45, 2054–2059, 2001.
Allen, J.A., Peterson, A., Sufit, R., Hinchcliff, M.E., Mahoney, J.M., Wood, T.A., Miller, F.W., Whitfield, M.L., and Varga, J., Post-epidemic eosinophilia-myalgia syndrome associated with L-tryptophan, Arthritis Rheum., 63, 3633–3639, 2011.
Ames, B.N., Magaw, R., and Gold, L.S., Ranking possible carcinogenic hazards, Science, 236, 271–280, 1987.
Baily-Klepser, T., Doucette, W.R., Horton, M.R., Buys, L.M., Ernst, M.E., Ford, J.K., Hoehns, J.D., Kautzman, H.A., Logemann, C.D., Swegle, J.M., Ritho, M., and Klepser, M.E., Assessment of patients’ perceptions and beliefs regarding herbal therapies, Pharmacotherapy, 20, 83–87, 2000.
Bandera, E.V., Chandran, U., Buckley, B., Lin, Y., Isulapalli, S., Marshall, I., King, M., and Zarbi, H., Urinary mycoestrogens, body size and breast development in New Jersey girls, Sci. Total Environ., 409, 5221–5227, 2011.
Boden-Albala, B., Elkind, M.S., White, H., Szumski, A., Paik, M.C., and Sacco, R.L., Dietary total fat intake and ischemic stroke risk: The Northern Manhattan study, Neuroepidemiology, 32, 296–301, 2009.
Boullata, J.L. and Nace, A.M., Safety issues with herbal medicine, Pharmacotherapy, 20, 257–269, 2000.
Centers for Disease Control, Analysis of l-tryptophan for the etiology of eosinophilia-myalgia syndrome, Morb. Mortal. Wkly Rep., 39, 581–591, 1990.
Chan, J.M., Stampfer, M.J., Ma, J., Gann, P., Gazianio, J.M., Pollak, M., and Giovannucci, E., Plasma insulin-like growth factor-I and prostate cancer risk, Science, 279, 563–566, 1998.
Cohen, S.M. and Ito, N., A critical review of the toxicological effects of carrageenan and processed eucheuma seaweed on the gastrointestinal tract, Crit. Rev. Toxicol., 32, 414–444, 2002.
Colton, T., Greenberg, E., Noller, K., Resseguie, L., Van bennekom, C., Heeren, T., and Zhang, Y., Breast cancer in mothers prescribed diethylstilbestrol in pregnancy: Further followup, JAMA, 269, 2096–2100, 1993.
Comas, A.P., Precocious development in Puerto Rico, Lancet, 319, 1299–1300, 1982.
Dupont, H.L., The growing threat of foodborne bacterial enteropathogens of animal origin, Clin. Infect. Dis., 45, 1353–1361, 2007.
Flamm, W.G., Pros and cons of quantitative risk analysis. In Food Toxicology: A Perspective on the Relative Risks, Taylor, S.L. and Scanlan, R.A. (eds.), Marcel Dekker, New York, 1989, pp. 429–446.
Frisoli, T.M., Schmeider, R.E., Grodziki, T., and Messerli, F.H., Salt and hypertension: Is salt dietary reduction worth the effort? Am. J. Med., 125, 433–439, 2012.
Fujisawa, S., Atsumi, T., Kadoma, Y., Ishihara M., Ito, S., and Yokoe, I., Kinetic radical scavenging activity and cytotoxicity of 2-methoxy- and 2-butyl-substituted phenols and their dimers, Anticancer Res., 24, 3019–3026, 2004.
Gans, D.A., Behavioral disorders associated with food components. In Food Toxicology: A Perspective on the Relative Risks, Taylor, S.L. and Scanlan, R.A. (eds.), Marcel Dekker, New York, 1989, pp. 225–254.
Gardner, H., Rundek, T., Wright, C.B., Elkind, M.S., and Sacco, R.L., Dietary sodium and risk of stroke in the Northern Manhattan Study, Stroke, 43, 100–1205, 2012.
Hall, R.L., Dull, B.J., Henry, S.H., Schleuplein, R.J., and Rulis, A.M., Comparison of the carcinogenic risks of naturally occurring and adventitious substances in food. In Food Toxicology: A Perspective on the Relative Risks, Taylor, S.L. and Scanlan, R.A. (eds.), Marcel Dekker, New York, 1989, pp. 205–224.
Harrington, S., The role of sugar-sweetened beverage consumption in adolescent obesity: A review of the literature, J. Sch. Nurs., 24, 2–12, 2008.
Harris, R.M. and Waring, R.H., Diethylstilboestrol—A long-term legacy, Maturitas, 72, 108–112, 2012.
Holly, J., Insulin growth factor-I and new opportunities for cancer prevention, Lancet, 351, 1373–1375, 1998.
Holmberg, S.D., Osterholm, M.T., Senger, K.A., and Cohen, M.L., Drug-resistant Salmonella from animals fed antimicrobials, N. Engl. J. Med., 311, 617–622, 1984.
Hord, N.G., Tang, Y., and Bryan, N.S., Food sources of nitrates and nitrites: The physiologic context for potential health benefits, Am. J. Clin. Nutr., 90, 1–10, 2009.
Horowitz, B.Z., Bromism from excessive cola consumption, J. Clin. Toxicol., 35, 315–320, 1997.
James, J. and Kerr, D., Prevention of childhood obesity by reducing soft drinks, Int. J. Obes. (Lond.), 29(Suppl. 2), S54–S57, 2005.
Johnson, R.J., Gold, M.S., Johnson, D.R., Ishimoto, T., Lanaspa, M.A., Zahniser, N.R., and Avena N.M., Attention-deficit disorder: Is it time to reappraise the role of sugar consumption? Postgrad. Med., 123, 39–49, 2011.
Kanarek, R.B., Artificial food dyes and attention deficit hyperactivity disorder, Nutr. Rev., 69, 385–391, 2011.
Kaneene, J.B., Warnick, L.D., Bolin, C.A., Erskine, R.J., May, K., and Miller, R., Changes in tetracycline susceptibility of enteric bacteria following switching to non-medicated milk replacer for dairy calves, J. Clin. Microbiol., 46, 1968–1977, 2008.
Loizzo, A., Gatti, G.L., Macri, A., Moretti, G., Ortolani, E., and Palazzesi, S., The case of diethylstilbestrol treated veal contained in homogenized baby food in Italy. Methodological and toxicological aspects, Ann. Ist. Super. Sanita., 20, 215–220, 1984.
Lundberg, J.O., Cardiovascular prevention by dietary nitrate and nitrite, Am. J. Physiol. Heart Res., 296, H1221–H1223, 2009.
Lundberg, J.O., Carlstrom, M., Larsen, F.J., and Weitzberg, E., Role of dietary inorganic nitrate in cardiovascular health and disease, Cardiovasc. Res., 89, 5525–532, 211.
Malik, V.S., Schulze, M.B., and Hu, F.B., Intake of sugar-sweetened beverages and weight gain: A systematic review, Am. J. Clin. Nutr., 84, 274–288.
Marshall, B.M. and Levy, S.B., Food animals and antimicrobials: Impacts on human health, Clin. Microbiol. Rev., 24, 718–733, 2011.
Marti, L.F., Effectiveness of nutritional interventions on the functioning of children with ADHD and/or ASD. An updated review of research evidence, Bol. Assoc. Med. P R, 102, 31–42, 2010.
Martinez-Cabot, A. and Messeguer, A., Generation of quinoneimine intermediates in the bioactivation of 3-(N-phenylamino)alanine (PAA) by human liver microsomes: A potential link between eosinophilia-myalgia syndrome and toxic oil syndrome, Chem. Res. Toxicol., 20, 1556–1562, 2007.
Mashour, N.H., Lin, G.L., and Frishman, W.H., Herbal medicine for the treatment of cardiovascular disease, Arch. Intern. Med., 158, 2225–2234, 1998.
Massart, F., Meucci, V., Sagesse, G., and Soldani, G., High growth rate of girls with precocious puberty exposed to estrogenic mycotoxins, J. Pediatr., 152, 690–695, 2008.
Mcann, D., Barrett, A., Cooper, A., Crumpler, D., Dalen, L., Grimshaw, K., Itchin, E., Lok, K., Porteous, L., Prince, E., Sonuga-Barke, E., Warner, J.O., and Stevenson, J., Food additives and hyperactive behavior in 3-year-old and 8/9-year-old children in the community: A randomized, double-blinded placebo-control trial, Lancet, 370, 1560–1567, 2007.
Munro, I.C., A case study: The safety evaluation of sweeteners. In Food Toxicology: A Perspective on the Relative Risks, Taylor, S.L. and Scanlan, R.A. (eds.), Marcel Dekker, New York, 1989, pp. 151–167.
Nigg, J.T., Lewis, K., Edinger, T., and Falk, M., Meta-analysis of attention deficit/hyperactivity disorder or attention deficit/hyperactivity disorder symptoms, restriction diet, and synthetic food color additives, J. Am. Acad. Child Adolesc. Psychiatry, 51, 86–97, 2012.
Noakes, R., Spelman, L., and Williamson, R., Is the l-tryptophan metabolite quinolinic acid responsible for eosinophilic fasciitis? Clin. Exp. Med., 6, 60–64, 2006.
Oberrieder, H.K. and Fryer, E.B., College students’ knowledge and consumption of sorbitol, J. Am. Diet. Assoc., 91, 715–717, 1991.
Pariza, M.W., A perspective on diet and cancer. In Food Toxicology: A Perspective on Their Relative Risks, Taylor, S.L. and Scanlan, R.A. (eds.), Marcel Dekker, New York, 1989, pp. 1–10.
Philp, R.B., Herbal-Drug Interactions and Adverse Effects: An Evidence-Based Quick Reference Guide, McGraw-Hill Medical Publishing, New York, 2004.
Poirier, L., Lefebvre, J., and Lacouriere, Y., Herbal remedies and their effects on blood pressure: Careful monitoring required, Hypertension Canada, 65, 1–8, 2000.
Poseda de la Paz, M., Philen, R.M., and Borda, A.I., Toxic oil syndrome: The perspective after 20 years, Epidemiol. Rev., 23, 231–247, 2001.
Report of the DES Task Force, J. Am. Med. Assoc., 255, 1849–1886, 1986.
Saito, M., Sakagami, H., and Fujisawa, S., Cytotoxicity and apoptosis induced by butylated hydroxyanisole (BHA) and butylated hydroxytoluene (BHT), Anticancer Res., 23, 4693–4701, 2003.
Sun, M., Use of antibiotics in feed challenged, Science, 226, 144–146, 1984.
Temme, E.H.M., Vandevijvere, S., Vinkx, C., Huybrechts, I., Goeyens, L., and Van Oyen, H., Average daily nitrate and nitrite intake in the Belgian population older than 15 years, Food Addit. Contam. A, 28, 1193–1204, 2011.
Thevis, M., Fussholler, G., and Schanzer, W., Zeranol: Doping offence or mycotoxin, Drug Test Anal., 3, 777–783, 2011.
Titus-Emstof, L., Troisi, R., Hatch, E.E., Palmer, J.R., Hyer, M., Kaufman, R., Adam, E., Noller, K., and Hoover, R.N., Birth defects in the sons and daughters of women who were exposed in utero to diethylstilbestrol (DES), Int. J. Androl., 33, 377–384, 2010.
Weiner, M.L., Toxicological properties of carrageenan, Agents Actions, 32, 46–51, 1991.
Weiss, B., Synthetic food colors and neurobehavioral hazards: The view from environmental research, Environ. Health Perspect., 120, 1–5, 2011.
Welsh, J.A., Sharma, A.J., Grellinger, L., and Vos, M.B., Consumption of added sugars is decreasing in the United States, Am. J. Clin. Nutr., 94, 726–734, 2011.
You, Y., Hilpert, M., and Ward, M.J., Detection of a common and persistent tet(L)-carrying plasmid in chicken-waste-impacted farm soil, Appl. Environ. Microbiol., 78, 3203–3213, 2012.