1
AN INTRODUCTION TO THE U.S. HEALTHCARE INDUSTRY, INFORMATION TECHNOLOGY, AND INFORMATICS
Content
Information Technology, Informatics, and Healthcare Productivity: A Historical Perspective
Productivity, Efficiency, and the Uniqueness of Healthcare
Management of Healthcare Processes
Effective Informatics through Management Theory
Project and Knowledge Management
Business Intelligence and Decision Support Systems
Four Areas of Focus for Healthcare Efficiencies
Quality Improvement in Clinical and Operational Activities
Customer Relationship Management in Healthcare
Closing Comments on the Ever Important Issue of Data Privacy
Healthcare is probably one of the most complex business models in American industry given the uniqueness of the marketplace in which it operates. It is perhaps the only industry in which the consumer does not necessarily pay for the service he or she receives, but rather third parties (in this case, insurance companies) negotiate arrangements with service providers to determine payment rates and types of service that are to be paid on the consumer’s behalf. The nature of the services required corresponds to a variety of ailments that are attributed to vast numbers of patients—factors that add to the mix of issues to manage. Complexities for healthcare organizations are heightened when considering the numerous data exchanges that are involved with services provided to patients. Data exchanges can be plagued by a myriad of formats, captured and stored in a variety of repositories. These exchanges introduce further complexities in the form of “vocabularies,” or, in other words, the coding languages that are required to identify types of services that vary considerably from payor to payor, state to state, and service type to service type. Also, data in general come from a multitude of different “niche” systems and are presented in many different ways (e.g., text reports, spreadsheets, HL7 messages, ANSI X12 formats) and need to be integrated and presented to a caregiver or analyst in a consistent and coherent manner. It is the combination of all of these factors that begins to describe the underpinnings of the spectrum of healthcare informatics.
Data provide the building blocks to information and constitute a vital resource to administrators, practitioners, and decision makers in healthcare organizations. The process of transforming data into information is a daunting task, and given the complexities described in the preceding paragraph, the task is particularly challenging in this unique industry. This challenge must be managed, as healthcare is one segment of American industry in which incorrect decisions or errors can cost lives or put innocent people in significant danger. The need to understand which patterns of treatment for a variety of different conditions will produce the best outcomes is profound. Adding to the challenge are the financial burdens healthcare providers are experiencing, as reimbursements are being cut and more and more conditions are being mandated in order to pay for services rendered. Healthcare organizations invariably lose money on certain classes of patients, and it is critical to understand where those areas are and how to address them.
The Affordable Care Act (ACA) has transformed the face of healthcare delivery in profound ways on many levels. It is rapidly changing the very manner through which providers are reimbursed by emphasizing “value-based reimbursement,” which in government-speak means that providers will be directly rewarded financially for demonstrating excellent care and may be penalized financially for care that does not meet the quality standards laid out by the Centers for Medicare and Medicaid Services (CMS). A number of different areas are monitored by CMS for adherence to these standards, but the concept of reducing “patient readmissions” has received particular attention. This concept is a fundamental change from the fee-for-service model that healthcare providers have been accustomed to for decades and requires a capability to measure easily outcomes that, up until very recently, was difficult if not impossible to do. Accountable Care Organizations (ACOs) and Patient-Centered Medical Homes (PCMHs) are also new models of care emphasizing collaboration across multiple providers, quality management, and incentives for cost efficiencies. These models fall under the rubric of a new concept that is being adopted by providers to accommodate new payor reimbursement models that are coming to the forefront: the concept of “Population Health Management,” or finding ways to keep people well, as opposed to just interacting with them when they are sick. Capturing the myriad of data points required to report properly on relevant metrics has become one of the primary challenges facing the healthcare industry today.
Information Technology, Informatics, and Healthcare Productivity: A Historical Perspective
One way to better manage the complex nature of the healthcare industry is through the incorporation of information technologies. Web platforms, data storage, analytic software, telecom and wireless communications systems, and so forth can help provide critical information and speed of information dissemination to those who require it, when they require it.
During the mid-1990s, organizations across industry sectors retooled their information technology infrastructures in response to dramatic innovations in storage, processing, analytics, and bandwidth (see Table 1.1). The enhanced capabilities facilitated by these technologies offered organizations opportunities to increase productivity in a variety of ways. Factors such as the dissemination of critical information to decision makers regarding process performance; the ability to communicate within organizations, across industry sectors, and on the global spectrum; and simplifying procedures, to name a few, enabled organizations to manage available resources better in providing a good or service to the ultimate consumer.
Table 1.1 Growth in Investment in Information Technologies
| YEAR | INVESTMENT IN INFORMATION TECHNOLOGY AS A PROPORTION OF INDUSTRIAL EQUIPMENT AND SOFTWARE (%) |
| 1980 | 30.7 |
| 1990 | 41.1 |
| 1999 | 47.2 |
Source: Economic Report of the President 2001, Table B-18, p. 296.
The significant investment in information technologies was initially questioned by many as to the payoff or gains from these dollar outlays for hardware, software, telecom platforms, and so on. This debate sparked a myriad of research from the academic and private sector arenas to investigate the potential gains to IT. Resulting studies illustrated positive returns on investment in information technologies by firms operating across industry sectors.1–3 On a macroeconomic perspective, U.S. productivity grew dramatically from levels achieved over the previous decade (see Figure 1.1).
This jump in productivity enabled the U.S. economy to grow at a robust pace without experiencing a noteworthy acceleration in price inflation as gains in efficiency helped reduce costs throughout the economic system (see Figure 1.2). These productivity gains have been maintained into current times as companies continue to invest in and apply information technologies in a variety of process-enhancing ways.
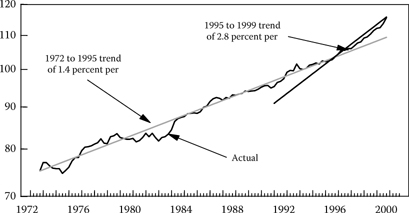
Figure 1.1 The trend rate of nonfarm productivity growth accelerated (Index 1992 = 100, log). (From the U.S. Department of Labor, Bureau of Labor.)

Figure 1.2 U.S. Gross Domestic Product vs. Consumer Price Index. (U.S. GDP data: U.S. Commerce Department Bureau of Economic Analysis. U.S. CPI: U.S. Department of Labor, Bureau of Labor Statistics.)
Historically, healthcare has been somewhat of a laggard in terms of investing in technology. The fragmented nature of the industry and the abundance of different coding systems and taxonomies are often cited as reasons for the lag in technological implementations, along with the persistence of traditional paper-based procedural modes of operations. The structure of the industry involving numerous individual hospitals and health-related entities created a dichotomous environment that involved diverse naming procedures and formatting standards of critical data resources and breakdowns in the ability to share them. Paper-based methods of operations (e.g., charting by physicians and nurses) limited the creation of vital data resources that describe critical treatment activities of patients.
These factors reduced gains in efficiency that otherwise could be achieved based on network effects of information sharing. In other words, the lack of data resources and the existence of disparate data resources involving diverse naming conventions existing in a variety of storage devices corresponding to separate providers of health services (e.g., hospitals, clinics, private practices) deter the ability of healthcare organizations to create robust information resources from available data. With only pieces of the puzzle (e.g., data existing in isolated systems, information in paper-based form) healthcare providers were limited in the amount of information available to them when attempting to enhance their knowledge regarding service effectiveness and efficiency.
To clarify this point further we need to turn to the evolution of the Internet. Forms of the Internet were actually in existence well before the information boom of the 1990s (e.g., the government ARPANET was in existence in the 1970s). However, the true gains in efficiency resulting from utilization of the Internet for consumers and businesses alike were not achieved until network effects took hold. In other words, the network of users who had access to the Internet needed to reach critical mass.4 As more and more consumers and businesses had access to the Internet, the more it became a viable mechanism to communicate and conduct commerce. In comparison, as data resources in the healthcare industry become more standardized and integrated within health organizations and across systems of corresponding service providers, the ability to extract information from and generate knowledge regarding better allocating resources to enhance process efficiencies in financial, clinical, and administrative activities should increase dramatically. The result should be fewer wasted resources, enhanced process performance, and a lower cost operating environment.5
The past few years have spurred another boom in healthcare information technology investment. The development and incorporation of wireless devices, sensors, apps, and continued advancement of computer processing and storage capabilities have underpinned this second wave of the information pulse. This time the healthcare sector was on board and kept pace with investments and applications in other industries. The Health Information Technology for Economic and Clinical Health (HITECH) Act, which was part of the ARRA (aka “the Stimulus Package”) provided billions of federal dollars in economic incentives to providers who could demonstrate “meaningful use” of healthcare information technology. That was the “carrot”; the “stick” was that those incentives would cease and financial penalties would begin in 2015 for those providers who could not attest to “meaningful use.” The HITECH program was extremely successful in getting hospitals and physicians to invest in Electronic Health Record (EHR) technology, but there are different schools of thought as to whether physicians, in particular, have found EHRs to have made their lives easier. Nonetheless, the need to demonstrate “meaningful use” and the need to capture a multitude of quality metrics has indisputably moved the industry forward. Now, with EHRs in place, there is a valid data source (albeit with many challenges) that can provide the measurements required.
The Internet has made it possible for providers to share patient clinical data across multiple sites of care in near real time, which brings us that much closer to allowing a provider to see a patient’s entire medical history when he or she is in the exam room. No, we are not there yet, for many of the reasons that you will learn about, but the potential is there and in some regions, very successful Health Information Exchanges (HIEs) are getting close to achieving this laudable goal.
Given recent consolidation of individual providers into systems of providers (e.g., healthcare systems), advancements in hardware, software, telecom, wireless and Internet-based technologies, the ability of treatment- and diagnosis-based technologies to help enhance data capture, the creation of digital data resources from paper-based procedures, and enhanced data input and communication of information, healthcare providers are on the cusp of experiencing increased operational efficiencies that will enable them to manage their cost structure while providing the best care possible to patients. The incorporation of billing and financial related technologies, decision support systems, and data management and analytic capabilities enable healthcare providers to enhance their ability to identify misallocations of resources and increase the effectiveness and speed of processes from administrative and financial to clinical activities.
Enhanced efficiencies made possible by investment in information technologies could result in significant cost savings to healthcare providers. These gains are critical in addressing the ongoing growth in healthcare expenditures in the United States, which now account for roughly 17% of gross domestic product (GDP). Some recent studies have depicted significant returns on the investment in information technologies, with reduction in expenditures ranging from $100 to $450 billion over the coming years.6,7 Investment in technologies that seek to promote a more automated delivery system through workflow and medical records systems, evidence-based decision support systems, integration of information between healthcare providers, and streamlining the current claim-based transactions billing system to an all-electronic payment at point of service system can yield substantial savings to healthcare providers and the ultimate consumer/patient.8
Productivity, Efficiency, and the Uniqueness of Healthcare
Despite the fact that the healthcare industry possesses characteristics unique from those of other sectors (e.g., doctor–patient relationships and the ultimate objective of providing the best quality of care to patients that can override established business profit optimization goals) healthcare still entails procedures and processes that can be made more efficient.
Technologies can help providers discover more effective treatment tactics that may reduce ineffective, redundant, and unnecessary tests and procedures that inconvenience patients and providers and increase costs. The rapid scaling of business intelligence systems, through tools such as Hadoop and others, allow for previously unimaginable amounts of data to be analyzed quickly. New tools such as IBM’s Watson computer (the robot that won on Jeopardy!) can parse huge amounts of patient data against a massive database of best practices and offer diagnostic advice to physicians in real time. The application of Watson in healthcare is in its early stages but the possibilities for it are limited only by the imagination.
These technologies can reduce bottlenecks in administrative processes, alleviating waiting times for patients and directing them to the most appropriate areas to address their problems. They can minimize complexities in billing activities that can result in overbilling recipients. Technologies can help enhance preemptive treatment to mitigate illnesses from developing into fully developed chronic diseases.
Management of Healthcare Processes
Management and economic concepts can play a key role in enhancing efficiencies in the industry given the methodologies that address the allocation of the correct resources to the demand for those resources. Accomplishing this helps preserve the essence of healthcare organizations and those individuals involved in providing treatment for patients. With the aid of accurate and timely information and the ability to communicate and apply that information, physicians, nurses, technicians, and administrators can improve the process of caring for those in need in a more efficient, less costly manner. Techniques and methodologies that create, disseminate, and analyze data comprise the realm of informatics. Two basic definitions of informatics are provided to clarify what is meant by this concept.
Informatics are the sciences concerned with gathering, manipulating, storing, retrieving, and classifying recorded information. (Source: wordnetweb.princeton.edu/perl/webwn)
Health informatics or medical informatics is the intersection of information science, computer science, and healthcare. It deals with the resources, devices, and methods required to optimize the acquisition, storage, retrieval, and use of information in health and biomedicine. Health informatics tools include not only computers but also clinical guidelines, formal medical terminologies, and information and communication systems. (Source: Wikipedia)
Effective Informatics through Management Theory
Pure investment in information technologies is not the final solution to enabling providers to operate more productively, however. Applications in management theory are essential to ensure effective implementation and utilization of these technologies to best leverage their capabilities to increase labor and process productivity. Management theory that must be considered includes strategic management, management information systems, project management, knowledge management and organizational behavioral, quantitative techniques, and decision support theory, to name a few. These management concepts focus on the acquisition of technologies that provide the correct functionality to facilitate a particular process and proper implementation of the technology to ensure its proper utilization (this includes creating a receptive culture within the organization by users to adopt the platform as an essential tool to enhance their daily routines). Theoretical concepts also address analysis, communication, and best utilization of the results and outputs of systems that are employed.
Project and Knowledge Management
Project management addresses methods that support successful implementations of information technologies. It addresses the incorporation of correct tactics to acquire the most appropriate technology platform to facilitate an organizational need in the most seamless way possible. For example, when a healthcare provider wants to implement a new database system that facilitates the conversion of paper-based routines into digital assets for clinical and treatment activities, the organization must consider which technology best offers the most feasible functionality corresponding to the operational structure of the organization. This includes the cost of the technology, scalability, ability to integrate with existing systems both within the organization and with other systems at area provider sites, as well as user friendliness. Once the technology is chosen, factors to promote the most seamless integration into the work environment must be considered. This includes timing schedules, training for users, and eventual complete roll out to the workforce. Knowledge management theory overlaps project management to some extent when considering the implementation stages of new technologies. It addresses the additional critical factors of ensuring the systems adoption by users with the ultimate goal that it becomes a key component in the everyday activities of its users and stakeholders. Knowledge management also addresses those factors that support leveraging the output produced by users working with systems and the dissemination and collaboration of corresponding information among individuals connected to processes and procedures. In other works, knowledge management theory promotes the active utilization of information and creation of knowledge within an organization, concepts that drive best practices and innovation.9,10
Other management-related concepts also must be considered in attempting to best leverage information technologies and these involve such strategic initiatives as Lean/Six Sigma, Total Quality Management, Supply Chain Management, and Workflow Optimization and advanced analytics such as data mining to not only analyze past data patterns, but also to offer a platform for predictive analytics that can identify high-risk patients and offer appropriate treatment for them. The process of treating a patient incorporates a network of activities that are complementary and interdependent in nature, where breakdowns in aspects of one operational entity can cause disruptions to the overall process of patient care. The patient treatment process can include diagnosis, prescription of medications, radiology and lab tests, administration of treatment procedures, monitoring of results and outcomes, and so forth. These activities include input from numerous personnel in corresponding operational departments in the healthcare organization. Workflow analytic methodologies must be considered to understand better the efficiencies of the entire treatment process. The overall process can be compared to managing a supply chain or supply network of activities that are complementary and interdependent, with the ultimate objective of achieving the best allocation of available resources to provide the best care to corresponding patients. These management methodologies can be augmented with the incorporation of statistical and quantitative-based analytics such as the Six Sigma approach.
Six Sigma and Data Mining
Six Sigma is an analytic method that leverages available data resources and incorporates statistical applications and visual capabilities to monitor process variance and efficiencies. By analyzing data resources corresponding to various operational processes with the utilization of statistical techniques, analysts can better determine which types of practices result in unacceptable variances in performance metrics.11 Lean Six Sigma is a strategic initiative that complements the variance identification focus of Six Sigma and seeks to eliminate non-value-add processes or activities in an organization that can add to waste. Value stream mapping is often used to enhance throughput of processes.
For example, a Lean Six Sigma approach could be implemented in a radiology setting. Are there bottlenecks or unnecessary steps that can be improved on in the network of activities in the radiology department that produce high time delay variances in getting x-ray results back to an attending physician?
More robust and sophisticated techniques to analyze data involve the utilization of quantitative methods to process data and statistical testing to determine patterns and trends that may exist in particular service activities. Traditional regression methods and data mining methodologies enable analysts to better identify recurring trends in the various activities of healthcare services. Resulting models can determine whether particular treatment procedures result in enhanced health outcomes according to patient populations, whether particular procedural activities result in unacceptable outcomes measures, and so on. These types of analyses are becoming increasingly important as “patient experience” feedback directly from clients is now a parameter for the new concept of “value-based reimbursement.” A significant percentage of the potential payment adjustment for a provider is predicated on feedback patients share, so being able to directly address likely patient “dis-satisfiers” head-on is very important now.
Business Intelligence and Decision Support Systems
Other methods of data analysis that can help increase the knowledge of healthcare practitioners involve the more simple creation and presentations of reports and graphics through Online Analytic Processing and dashboards. The advantage is these methods focus on presenting data in a timely and understandable manner, enabling decision makers to view these analytic platforms quickly to identify factors impacting operational performances.
These various data driven software technologies and initiatives comprise the realm of decision support systems and business intelligence. The functionalities of the components including report generation, trend and pattern detection, and quantitative and statistical based analytics complemented with graphical interfaces provide users/ decision makers in various functional areas of healthcare organizations with timely, actionable information to enhance strategizing. Informatics to improve efficiencies include optimizing resource allocations corresponding to a variety of activities and procedures. The utilization of decision support systems and business intelligence that leverage essential data resources can ultimately help reduce lag times in patients waiting for treatment, adjust treatment procedures to enhance outcomes, reduce inefficiencies in billing, reduce lag times in lab and radiology exam completion and reporting times, and so forth. The ultimate result is better management of healthcare operations and costs and care effectiveness and quality outcomes for patients.
Four Areas of Focus for Healthcare Efficiencies
With all of the turbulence present in the healthcare landscape, it comes as little wonder that healthcare organizations are embracing the potential of leveraging information technologies and informatics and their ability to enhance efficiencies. Informatics applications and capabilities within the healthcare spectrum can be categorized into four different discrete areas:
• Financial (tracking activity-based costing, ensuring that services rendered are properly billed and compensated and that expenses stay within acceptable budgetary parameters). With CMS and other insurers monitoring cost-per-patient and adjusting reimbursement based on this, the financial component is especially important.
• Clinical compliance (ensuring that the appropriate procedures are applied to the right patient at the right time, making sure that staffing patterns and other reportable parameters are within acceptable mandated bounds, and alerting as quickly as possible when they are not). An interesting note is that, with the new reimbursement models that are coming to the fore, for the first time, clinical quality will play a direct role in a significant percentage of a provider’s reimbursement. So, in essence, the financial team is directly accountable for clinical excellence and the clinical team is directly accountable for financial excellence.
• Quality improvement (analyzing clinical data to see which treatment protocols provide the best outcomes in an economically sustainable way).
• Patient satisfaction/marketing (what aspects of a patient’s stay were problematic—how are those measured, identified, and remedied for the future).
The following section takes a quick look at each of these areas to give a broader sense of just how informatics can be so important in managing the critical factors that healthcare leadership needs to understand better to manage their respective organizations properly.
Financial Activities
Hospitals and many other healthcare providers have undergone a drastic transformation during the last 15 to 20 years. This transformation is characterized by the change in environment as is evidenced by organizations, who saw their role almost as benevolent charities whose mission it was to provide care to all without particular regard to reimbursement (the guiding assumption was “if you bill it, they will pay”), to rough-and-tumble competitive businesses who needed to track all aspects of financial performance to satisfy their boards, shareholders, and other organizational stakeholders. Over this period of time, large public companies or organizations have invested significant sums and acquired many healthcare organizations with the expectation of receiving an aggressive return on their investments. Also during this time, regulations on healthcare payors were loosened, which helped spark the managed care (HMO) and “capitated payment” (fixed monthly payment to providers not directly tied to specific visits) movements. As more players entered the healthcare space with specific bottom-line interests, reimbursement schemas became increasingly more complex; more entities needed to be measured (e.g., are we getting more in monthly capitated payments than we are paying out in actual patient encounters?). With all this going on, one can only imagine how critical it became to understand in great detail what one’s reimbursement and cost foundation was, where timeliness and accuracy of information describing these activities was critical to determine potential trends over time. Modeling capabilities needed to be generated to analyze corresponding data and alert mechanisms needed to be incorporated to highlight what key indicators breached certain predetermined levels. Again, the Affordable Care Act has introduced a whole new dynamic for the finance teams at healthcare institutions through its emphasis on quality and requirements that key indicators are measured on an ongoing basis.
In 2015, diagnosis coding migrated from the ICD-9 system, which has been in use for decades, to the ICD-10 system. The change here is profound: the ICD-9 coding set had about 14,000 different diagnosis codes; the ICD-10 coding set has about 69,000 codes with much more granular detail. Payment contracts that pay a certain amount for particular conditions need to be reevaluated using new codes and providers need to have sophisticated modeling tools in place to assess the financial impact of mapping from one ICD-9 code to a potential multitude of ICD-10 codes.
Computerized financial systems have existed in healthcare for decades. Their ability to generate data- and report-driven balance sheets, profit-and-loss statements, and other relevant accounting reports lend themselves to an acute need for informatics. For instance, many hospitals, especially not-for-profit systems, finance growth and other capital initiatives through the use of fixed income securities (e.g., bonds), many of which may be guaranteed by a governmental or quasi-governmental authority. Conditions are attached to many of these securities stipulating that if certain key financial indicators breach agreed-on values, sanctions may be invoked that may include deeming these bonds as in “technical default.” This can have far-reaching implications for organizations in terms of ongoing financial viability, future access to credit, and changes in administrative personnel or board membership in impacted organizations. It is critical for an organization to be able to, at the very least, access vital information that would indicate whether variances in financial metrics exceeded preestablished thresholds of acceptance, and also to know in advance that trends among various other key indicators may be leading the ỏganization to this precipice.
There are also financial metrics that are unique to healthcare that speak to how efficiently the organization is being run and, indirectly, what the quality of care is likely to be based on important factors such as staffing patterns. Some of those metrics that are typically tracked include “full-time equivalents (FTEs) per occupied bed” (e.g., is the organization staffing its units commensurate with the patient volume on those units?), “net revenue” versus “net cash collected” (is the organization getting properly reimbursed for what it thinks it is rightfully owed for the services it renders?), and productive hours and agency hours (e.g., is the organization having to rely on expensive and less predictable “agency” nursing to fulfill its regulated staffing requirements?), to name a few.
With the advent of managed care and capitated contracts with payors, a whole new realm of tracking becomes critical. These types of contracts have become increasingly more complicated over the years, and it can be a challenge for an organization to have an accurate sense of the correct monetary allocation for particular types of services. Issues such as which services may not be reimbursable, which services may qualify as “outliers,” and under what circumstances “extraordinary” services would entitle the organization to reimbursement over and above the agreed-on base rate from the payor may need to be considered. “Contract management systems” surfaced during the 1990s to address this new paradigm and have, over the years, become a much more important part of a healthcare organization’s informatics toolkit. Combining information from contract management systems such as gauging receipts for particular services by particular payors with financial decision support systems becomes “strategic” for healthcare providers. Tracking both revenue as a whole and costs per different types of services (e.g., activity-based costing) and disseminating profitability information of different aspects of managed care contracts to decision makers provide the strategic information to implementing more effective initiatives.
Compliance Issues
The next area in which informatics could yield significant efficiencies involves the realm of clinical compliance. There are important regulations that can impact an institution’s accreditation status if procedures are not strictly adhered to. Organizations such as the Joint Commission or the Department of Health have very stringent and detailed regulations as to the exact protocols that need to be followed under different care circumstances. Also, governmental entities are reporting on websites accessible to the public the different levels of compliance of organizations corresponding to adherence to protocol standards. This can translate into lost revenue, lost market share, or diminished stature for those who underperform their competitors by registering subpar results of relevant indicators. For instance, at a relatively basic level, any patient who enters a facility exhibiting signs of respiratory problems is supposed to be given smoking-cessation counseling. Another example is that any patient presenting at a hospital with signs of a cardiac “event” is to be given an aspirin right away. These are basic care guidelines that are universally recognized as being important in ensuring that a patient has a desired health outcome. The challenge, however, arises when considering how an entity can capture this type of data and disseminate reports that indicate whether rules are complied with or not. With this information, organizations can take strategic initiatives to mitigate any undesirable performance variances.
There are also important factors to consider regarding time and allocation of resources to minimize the risk of complications to certain classes of patients. There is a particular focus on limiting readmissions: hospitals with unsatisfactorily high rates of readmissions will face a significant reduction in their overall reimbursement. Deviations from quality outcomes for different types of conditions, most of them cardiac in nature, will also result in penalties from a value-based purchasing perspective.
Regulatory mandates govern areas such as medication reconciliation and pain assessments as well, where once again, informatics enables organizations to better identify breakdowns in processes and procedures that cause subpar performance results so appropriate steps can be taken to adjust resources allocations such as staffing to mitigate negative outcomes. When addressing the issue of optimizing staffing resources within the organization, a number of complicated factors need to be considered. These include the notion of “acuity tracking,” or matching the severity of the conditions in a particular hospital unit with staffing allocations. Also, because staffing schedules tend to be projected a number of weeks into the future, census trends need to be analyzed. Factors such as day of week or time of year (e.g., winter months involving snow and ice could result in increased injuries and demand for healthcare services) must be considered. Proper staffing in light of these various factors can contribute to improved and more comprehensive care, which in turn will contribute to better outcomes, fewer complications, fewer medical errors, and so forth. However, as noted, because staffing decisions are based on best estimates of what may happen in the future, it becomes all the more important to have the best data available to ideally model what these needs will be. Informatics can synthesize data from a myriad of different systems, such as electronic medical records, financial systems, or even external Web-based systems that can provide information on factors outside of the hospital walls such as temperature, or perhaps the severity of the flu season in the area, and can enhance the understanding of potential demand for staffing resources.
The migration from ICD-9 coding to ICD-10 coding comes with a host of compliance challenges for healthcare providers. Medicare, Medicaid, and other third-party payors are auditing claims more than ever to ensure that the level of care being reimbursed for is consistent with the coding and documentation found on the claim. The newness and specificity of ICD-10 codes will have a major impact on providers as they scramble to ensure that they are appropriately documenting the legitimate level of care being provided to patients.
Quality Improvement in Clinical and Operational Activities
Another area that is rapidly maturing in the healthcare provider arena involves the growing utilization of devices that can interface directly with an EHR system and, ultimately, an informatics system. Ventilators, “smart” pumps, IVs, vital sign tracking monitors, and other devices like these can “talk” to electronic medical records and populate data directly into an EHR. Some EHRs, facilitated by information technologies, offer a capability to page a clinician or otherwise provide a real-time alert if a certain clinical value is outside of accepted medical bounds. These technologies also add to existing data elements to enhance the overall data resources for more advanced analytics.
Statistically based analytics such as correlations can help providers identify the best possible order sets to use for a given condition (in conjunction with evidence-based medicine protocols). Informatics incorporating statistical correlations and causation can identify that individuals who receive a certain type of specialized therapy can have much shorter lengths of stay and lower rates of readmission than those who do not. Analytics can also allow for comparing different clinical regimens to factors such as patient satisfaction survey scores. They can identify whether certain high-priced medications or medical devices may provide a less desirable outcome than lower-priced medications and can identify which doctors have a predisposition to order those medications or devices. Looking at physician comparisons, informatics will enable hospitals and other organizations to compare physician ordering patterns with desired outcomes such as reduced length of stay, lower readmissions, fewer complications or comorbidities, and revenue generation metrics. This provides a key level of accountability for all involved in the interdisciplinary plan of care of a patient to ensure that the right people are doing the right things at the right time.
Many factors affiliated with clinical compliance apply to our third area of focus, quality improvement programs. At the end of the day, all healthcare providers certainly strive to provide the highest quality of care possible at all times. However, attempting to define what constitutes quality can be elusive. Recently, regulatory agencies and payors have offered their own parameters as to what constitutes quality care. So-called “pay for performance” programs and “never event” prohibitions have helped crystallize much of what providers need to measure to demonstrate to appropriate agencies or payors that they are adopting the correct procedures for their patients. Many of the new programs being rolled out to providers are truly “pay for performance” programs that specify that there will be either incentives or penalties based on a providers’ demonstrated compliance with a certain set of quality protocols. If the provider complies effectively, incentive payments are provided. If not, differing levels of reduction of payment come into play. “Never events” are significant medical errors that can cause grave patient harm, and Medicare, and other payors, have made it a policy that they will not reimburse providers for costs incurred from provider events that should “never” happen; hence the name. Not only does “pay-for-performance” and “never event” tracking impact the long-term financial viability of healthcare organizations, but these types of statistics now are also among those that typically are compiled by governmental agencies, benchmarked, and posted on websites, where consumers (potential customers) can view them and compare them with those of a provider’s competitors.
Other indicators that are being tracked and reported via the web include hospital-acquired infection rates, readmissions, and indicators such as average waits to see a doctor in an Emergency Department. It becomes imperative that healthcare organizations develop the wherewithal to track these types of metrics accurately and in ways that allow for interceding proactively to address procedural issues to manage negative outcomes in the pipeline. “Benchmarking,” or comparing an organization against its peers and against what is considered to be “acceptable” performance is becoming increasingly common and increasingly visible to larger sections of the public. For a provider, knowing where its performance should be early in the process allows for more aggressive programs to be designed and deployed to ensure that the organization is applying the most optimal procedures.
The concept of quality improvement can also be articulated in a somewhat different, but extremely important, way as well. Though, as noted previously, there are a multitude of clinical metrics that often can and should be shared both internally and externally, quality improvement can also be construed as using data to improve business processes in general and enforce accountability for appropriate and acceptable performance. Informatics can be used, for instance, to compare the length of time it takes physicians in an emergency room to see a patient. This can be a significant motivating factor to enhance performance by comparing individuals to their peers. In general, informatics enables healthcare providers to aggregate and analyze data in constructive and actionable ways, the results of which are continuous improvement in various procedures throughout the organization.
Customer Relationship Management in Healthcare
Our final aspect of healthcare operations that can benefit immensely from informatics is the realm of “patient satisfaction.” As noted earlier, healthcare institutions increasingly have to view themselves more and more as businesses, and part of maintaining a viable business is producing positive experiences for your “customers.” In the health-care industry customers can take on a number of forms, ranging from patients, patients’ families, to doctors. Providing an exceptional experience for customers remains a significant goal for healthcare organizations as it promotes repeat visits from individuals in need of services. Happy customers also provide good word-of-mouth recommendations of their experiences that help rein in new customers, which maintains positive demand and, hopefully, increased revenue. And while the concept of “happy customers” is certainly important from a marketing perspective, the fact that patient satisfaction scores are significant factors in value-based reimbursement now means that unhappy patients can adversely affect a provider’s bottom line. Though much of this is intuitive, certainly, what is not so intuitive is how a healthcare institution gauges satisfaction rates of its customers.
Measuring patient satisfaction in a healthcare setting can take on multiple forms, but the prevalent metric comes from surveys that are sent to patients that, when tallied, generate an Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) score. Not only are these scores important from a bottom-line perspective, but they are also publicly published so patients/consumers can directly compare one hospital’s score to another’s. These surveys offer patients the opportunity to add comments to their response, where proactive healthcare organizations can build systems to route these comments automatically to the appropriate decision makers in the organization and track the timeliness of issue resolution. Medicare regulations spell out a formal procedure for what are called “grievances,” which have mandates attached to them about how facilities need to address them. Clearly tracking these to ensure the responses to these grievances stay within the bounds of the regulations is most important for the organization to avoid falling out of CMS compliance parameters, which may lead to financial or other, perhaps more severe, sanctions.
Another type of patient satisfaction interaction can be performed via surveys that are administered directly to the patient while he or she remains in the facility. These surveys allow for an organization to receive more timely feedback of issues as they are occurring and take steps to address them and, if necessary, initiate a formal service recovery procedure for particular types of unfortunate customer service situations. The general process for how this type of survey works involves interviewing patients (assuming their condition allows the interview) at certain time intervals and asking them questions regarding issues such as their perception of the food they received, demeanor of nurses, and so forth. Responses can be entered into a database and tracked and trended over time through the utilization of informatics methods that can also drilldown to identify if particular areas are problematic. Furthermore, certain types of responses and comments can be routed automatically to key individuals and processes can be built to track the timeliness and completeness of responses to these issues. The main advantage of this type of survey is the rapid-response capability it offers. The organization can find out right away if something is wrong and react and correspond directly with the individual to ensure that the remedy to the problem was effective. This can transform a dissatisfied customer into a satisfied one.
More and more, informatics can and does provide value in a multitude of different care settings and in a number of different operational processes. Organizations invariably will derive significant benefits from having a mechanism to generate an accurate read of data on all fronts and the ability to turn that data into actionable information. This information enhances the knowledge of service providers who can implement appropriate strategic initiatives to enhance efficiencies throughout the organization.
Closing Comments on the Ever Important Issue of Data Privacy
A critical element that needs to be maintained, preserved, and perhaps strengthened refers to the privacy safeguards of healthcare-related data of individuals. The integration of data resources from various healthcare providers and databases no doubt enhances efficiencies from analytics capabilities and information generation. As the process of developing more robust data resources enhances efficiencies, it also introduces the requirement for well-defined and strictly enforced standards to protect the privacy rights of individuals regarding health-related data. New privacy policies (mentioned in the text that follows) need to be designed to address any changes that transpire within the realm of data access and exchanges in the evolving healthcare system. The U.S. Department of Health and Human Services issued a privacy rule to implement the requirement for the Health Insurance Portability and Accountably Act of 1996 (HIPAA) which addresses the use and disclosure of individuals’ health information. A major goal of the Privacy rule is to ensure that individuals’ health information is properly protected while allowing the flow of health information needed to provide and promote high-quality healthcare and to protect the public’s health and well-being. The rule strikes a balance that permits important uses of information, while protecting the privacy of people who seek care and healing.12 New initiatives are currently addressing privacy requirements in this evolving data intensive environment. The American Recovery and Reinvestment Act of 2009 (ARRA) incorporates improvements to existing law, covered entities, business associates, and other entities that will soon be subject to more rigorous standards when it comes to protected health information.13 As data resources become more comprehensive, so too should policies that safeguard individual privacy rights.
References
1. W, Lichtenberg F. 1998. Computer use and productivity growth in US federal government agencies, 1987–1992. J Indust Econ, pp. 257–79, June.
2.Brynjolfsson E, Hitt L. 2000. Beyond computation: Information technology, organizational transformation, and business performance. J Econ Perspect 14(4):23–48.
3.Kudyba S, Diwan R. 2002. Increasing returns to information technology. Inf Syst Res, pp. 104–11, March.
4.Shaprio C, Varian H. 1998. Information rules: A strategic guide to the network Cambridge, MA: Harvard Business Press.
5.Kudyba S, Diwan R. 2002. Information technology, corporate productivity and the new economy. Westport CT: Greenwood.
6.Kayyali B, Knott D, Van Kuiken S. 2013. The big-data revolution in US health care: Accelerating value and innovation. McKinsey & Co. Available at: http://www.mckinsey.com/insights/health_systems_and _services/the_big-data_revolution_in_us_health_care.
7.Digital health solutions expected to save U.S. healthcare system more than $100 billion over next four years, Accenture finds. June 4, 2015. Available at: https://newsroom.accenture.com/news/digital-health -solutions-expected-to-save-us-healthcare-system-more-than-100-billion-over-next-four-years-accenture-finds.htm.
8.Patterson N. 2009. The ABCs of systemic healthcare reform: A plan for driving $500 billion in annual savings out of the US healthcare system. Cerner Corporation: Healthcare Industry Brief. Available at: http://www.cerner.com/ABCs.
9.Davenport T, Prusak L. 2000. Working knowledge. Cambridge, MA: Harvard Business Press.
10.Davenport T, Harris J, DeLong D, Jacobson A. 2001. Data to knowledge to results: Building and analytic capability. Calif Manage Rev 43(2): 117–38.
11.Pande P, Neuman R, Cavanagh R. 2000. The Six Sigma way: How GE, Motorola, and other top companies are honing their performance. New York: McGraw-Hill.
12.U.S. Department of Health Human Services (Summary of the HIPPA Privacy Rule). Available at: http://www.hhs.gov/ocr/privacy/hipaa /understanding/summary/privacysummary.pdf.
13.The American Recovery and Reinvestment Act of 2009. Available at: http://frwebgate.access.gpo.gov/cgi-bin/getdoc.cgi?dbname=111_cong _bills&docid=f:h1enr.pdf.
