8
APPLICATION OF HEALTHCARE INFORMATICS TO IMPROVING PATIENT SAFETY AND OUTCOMES
Contents
Case Study 1: Physician-Led Informatics
Case Study 2: Integrated Information Shared Services (I2S2) Intranet
Case Study 3: Clinical Adverse Drug Event (ADE) Alert System
Overview
Most healthcare information technology (IT) efficacy publications emerge from academic institutions that often develop their own proprietary information systems (IS). However, most patients in the United States are discharged from community hospitals. Community hospitals often implement advanced technology with a focus on global safety or quality, yet are faced with cost issues pertaining to large implementations and generally lack resources to measure the impact of such systems. This explains, in part, the limited research conducted among community hospitals to measure the economic and performance outcomes of healthcare IT. Therefore, it is important that experiences of community hospitals are documented and shared with hospital decision makers.
This chapter overviews the experiences of Trinity Health, a large multihospital community-based health system that initiated a systemwide information technology strategy to improve patient safety and clinical outcomes. Termed Project Genesis, the implementation of Trinity Health’s strategy is represented through three case studies. Case Study 1 makes the argument that hospitals must involve physicians and effectively communicate with them to implement safety and cost containment initiatives. Case Study 2 presents Trinity Health’s approach to developing an information systems tool, how physicians’ access to information helped them identify changes to be made, and the resulting impact on patient safety and hospital outcomes. Finally, Case Study 3 presents an example of an IT-supported initiative that led to the reduction in adverse drug events (ADEs) among the hospitals of Trinity Health.
Introduction
Trinity Health is the fourth largest Catholic health system in the United States and employs 44,500 full-time equivalent employees with more than 8,000 active staff physicians. Its facilities include 44 hospitals, 379 outpatient clinics/facilities, numerous long-term care facilities, home health and hospice programs, and senior housing communities across seven U.S. states. For FY 2008, Trinity Health revenues were $6.3 billion, including $376 million that were returned to the communities in the form of healthcare for the poor and underserved.
Trinity Health gained nationwide exposure when it received the 2004 National Committee for Quality Health Care’s annual award. The effective creation and implementation of the intranet-based information system called Integrated Information Shared Services (I2S2) played an important role in gathering, processing, and delivery of information. I2S2 delivered safety and quality outcome indicators for decision makers across the organization. The implementation of IT in Project Genesis employed an incremental step-by-step development approach in which the organizational and managerial issues were aligned with the IT.
Case Study 1: Physician-Led Informatics
This case study focuses on a continued initiative involving the tenets of customer relationship management (CRM) with the physicians.1 Trinity Health learned from the CRM literature to build a service-oriented mechanism that consisted of delivering information and soliciting physician involvement. Trinity Health had previously deployed a web-based information system to deliver physician profiles of quality and costs. The Physician Profiling System (PPS) contained three fundamental hospital-based CRM characteristics: (1) administrative data-driven decision-making processes for healthcare problem identification, variation reduction, statistical process control, and other physician-driven performance pattern analyses; (2) identification of areas for improvement by benchmarking (either internal, external, or both) physician practices to desired patterns of quality and cost out-comes; and (3) involving the physicians as customers in improving operations using (1) and (2) by establishing critical success norms or other related evidence-based initiatives, particularly by using technology for rapid deployment, prompt feedback, and support for replication of best practices. The PPS deployment incurred an approximate cost of US$163,000 for the development and implementation in a single hospital. The return on investment (ROI) for that endeavor exhibited a mean decrease of 0.24 days of hospitalization, with an aggregate decrease of 845 total inpatient days along with multiple hospital department cost savings of US$1.42 million. For details of this initiative, please see Kohli et al.1
Approach
Although the one-off PPS was successful and provided the proof of concept, Trinity Health could not afford a multihospital implementation, one hospital at a time. So it extracted the learning from the PPS, enhanced the existing decision support system’s (DSS) reporting capabilities, and delivered it through a web-based system for the entire organization (see Case study 2). The defining requirements emerging from the physician-led informatics initiative were as follows:
1. User-friendly design with common data structures for each ministry organization and a metadata level to speed query processing times
2. Enforced reconciliation of data with operational systems to ensure that all information systems provide consistent data
3. Seeking of value-added information such as cost accounting, expected reimbursement, and severity adjustment and assignment—processes that inform physicians about the impact of their decisions
4. Continuous improvement through cross-learning among ministry organizations and application development for quick deployment of best practices
Trinity Health created baseline assessments for disease categories (Table 8.1) to achieve the objectives of the physician-led informatics and to enhance ongoing physician alignment. These objectives were to share an innovative model for depicting individual physician resource utilization, the ability to identify physician variation in the clinical management, and to demonstrate the use of comparative benchmarking.
Results
The results from physicians’ involvement were manifested as lower average length of stay (ALOS) and reduced patient charges. By contrast, among the hospitals where data were yet to be shared with physicians, the ALOS and charges began to increase. Trinity Health continued to monitor outcomes through the utilization collaborative team (UCT). Hospital- and physician-specific scorecards were developed by the UCT and distributed. Figure 8.1 presents a sample physician utilization report.
Table 8.1 Benchmarking Data to Support Physician Informatics
| BENCHMARKING FOR CEREBROVASCULAR ACCIDENTS OR TIA | ||||
| N | MEAN | MEDIAN | SUM | |
| Quality | 449 | |||
| Mortality | 449 | 0.093 | 0 | 42 |
| Expected mortality | 449 | 0.114 | 0 | 51.186 |
| Complications | 449 | 0.167 | 0 | 74.983 |
| Readmissions | 449 | 0.081 | 0 | 36.369 |
| Expected readmissions | 449 | 0.109 | 0.106 | 48.941 |
| LOS | 449 | 4.55 | 4 | 2,042.95 |
| Expected LOS | 449 | 4.67 | 4.84 | 2,096.83 |
| Costs | 449 | |||
| ER | 449 | $247.40 | $233.50 | $111,082.60 |
| ICU | 449 | $659.70 | $0.00 | $296,205.30 |
| Lab | 449 | $217.50 | $110.80 | $97,657.50 |
| Misc. | 449 | $574.60 | $538.70 | $257,995.40 |
| Pharmacy | 449 | $370.40 | $143.30 | $166,309.60 |
| Radiology | 449 | $404.60 | $260.10 | $181,665.40 |
| Room | 449 | $1,290.70 | $1,052.20 | $579,524.30 |
| Supply | 449 | $54.45 | $8.41 | $24,448.05 |
| Surgery | 449 | $19.62 | $0.00 | $8,809.38 |
| Therapies | 449 | $256.20 | $179.10 | $115,033.80 |
| Total cost | 449 | $4,095.60 | $3,209.40 | $1,838,924.40 |
| Expected cost | 449 | $4,307.60 | $4,342.50 | $1,934,112.40 |
The utilization-based scorecards compared each physician’s actual versus expected outcomes for ALOS, mortality, and patient charges for services. Comparable metrics for physicians within the specialty as well as other specialties are also reported. Finally, the scorecard presents a breakdown of charges by major categories such as lab, surgical, and pharmacy. Supported by the informatics, the physician and clinical staff practice changes resulted in lower than expected mortality rates as well as patient charges. With 2,932 patients, a drop in 0.32 day per patient in LOS equated to 938 fewer patient days and a reduction of $661.27 per patient in charges resulted in savings of nearly US$1.939 million.
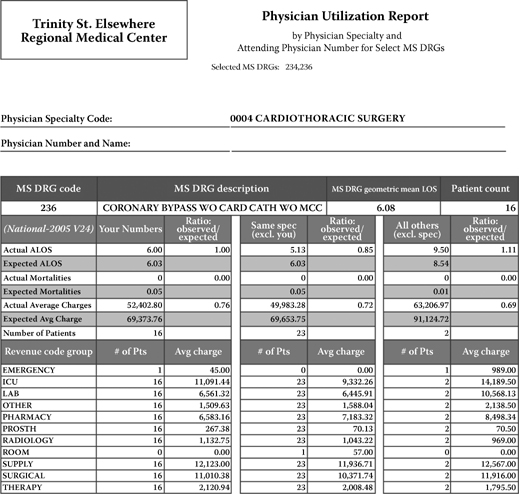
Figure 8.1 A sample physician scorecard.
The deployment of physician-led informatics prompted various feedback comments. Some admitted that they didn’t realize the procedure costs that much, while others found the scorecards helpful and expressed eagerness for the next report. The outcomes in the report card prompted some physicians to review previous patients’ charts and examine why they were in the hospital for that long, resulting in a retrospective learning and ideas about patient safety, improvement in ALOS, and how to contain costs.
Case Study 2: Integrated Information Shared Services (I2S2) Intranet
In the clinical arena, there is an expectation that quality must be measured on an ongoing basis. Healthcare organizations are monitored for quality and patient safety by the accrediting agencies and the U.S. government. Various agencies, public and private, publish hospital and physician comparisons (see http://www.hospitalcompare.hhs.gov, http://www.qualitynet.org/, and http://www.healthgrades.com/). Prior to many of the public sources of comparisons, Trinity Health desired transparency, so it published the quality performance for each ministry organization (MO) on an intranet website called Integrated Information Shared Services (I2S2). The transparency of quality indicator performance enabled each hospital to identify another hospital with better performance. Conversations about higher performance led to performance improvement strategies and action plans.
Approach
I2S2 was originally planned as an intranet web-based site. The development and maintenance was to be outsourced. However, owing to the projected high costs of development, in-house resources completed the project. The I2S2 design uses content management software. Content management software is most often used for storing, controlling, and publishing industry-specific documentation such as articles, manuals, and guides. The content may include files, graphs, images, databases, and documents with links to other websites (for more information, see http://www.contentmanager.eu.com/history.htm). Content management software integrated the interdependent layers of data for managing Trinity Health’s content as well as for publishing the results to any individuals across the organization.
I2S2 recycles automatically every two hours. Costs include the server hardware, the content management software, and the incremental labor from IT and clinical operations staff needed to input content. The benefits clearly outweigh the costs. I2S2 is now a web content management (WCM) system. This simplifies the publication of the web content and allows the domain experts to focus on creating content. The advantage of the WCM-based architecture is the ease of use. Since the majority of contributions are from clinicians, content submission does not require technical knowledge of HTML or file uploads. As a result of the WCM, I2S2 is fully transparent to the more than 50,000 Trinity Health employees who simply have to sign on to the Trinity Health webPage for the vast information resources available to them.
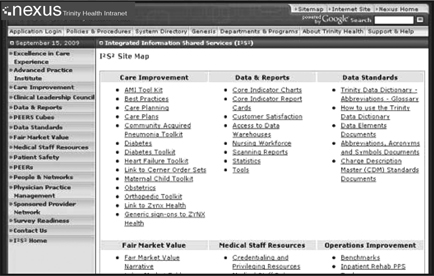
Figure 8.2 I2S2 user interface listing a site map with various categories of information and reports available.
The spectrum of I2S2 content, shown in Figure 8.2, can be logically organized in three primary areas: governance, data requirements, and guidelines and education. The following list provides descriptions of the salient topics for which I2S2 delivers support for decision makers. For each of the three areas, we discuss topics for which information is available.
1. Governance
Excellence in care experience. Patient satisfaction data, employee engagement, and physician satisfaction data are at the core and should be used to improve the overall experience of the patients and their families.
The Advance Practice Institute provides data to promote evidence-based best practices through advanced skills of nursing leaders, development of leadership skills to facilitate and complete projects, and the fostering of networks for creative thinking and issue resolution in the practice of evidence-based care.
Care improvement provides evidence-based tools, strategies, and resources to assist in providing excellence in care for specific clinical conditions such as acute myocardial infarction (AMI), pneumonia, diabetes, heart failure, newborn and neonatal, obstetrics, orthopedics, and vaccine information.
The Clinical Leadership Council provides documentation for value and strategies of Trinity Health clinical services in accordance with the Trinity Health strategic plan. The goal is to develop high-quality and world-class service and to optimize value for the entire health system while maintaining organizational integrity and regulatory compliance. Minutes of monthly meetings and links to evidence-based practices and core clinical indicators are also provided.
2. Data requirements
Data standards connect decision makers to tools and resources related to Trinity Health’s data standardization activities and include the data dictionary, approved abbreviations, dangerous abbreviations, supply chain links, glossary, data elements documents, and charge description master with standards. In addition, the charge description master file contains standardized detailed information on all services provided by the institution, including description, department codes, service code, and so forth.
The Data and Reports section provides views of clinical data, such as core indicator charts, report cards, customer and physician satisfaction data, medication/pharmacy scorecards, and scanning reports. For FY 2009, 28 core indicators are also available for each Trinity Health hospital, as well as other indicators for emergency room care, home care, and long-term care. Decision makers can also access data warehouses and download data for further analysis.
Patient Safety and Potential Error and Event Reporting (PEERs). This site links to best practices and related websites, patient safety tool kits, and numerous quality and safety reports for clinicians, as well as Trinity Health historical safety data. PEERs was designed by Trinity Health physicians, nurses, attorneys, and quality and risk management professionals to capture near-miss and errors/events data. Modeled after NASA’s voluntary reporting system, PEERs is rated very high in the ease of use and ensuring anonymity.
3. Guidelines and education
Medical Staff Resources delivers policies, procedures, links, articles, and more on current issues affecting medical staffs. Links and related topics include credentialing and privileging resources, medical staff by-laws, rules and regulations, medical staff development plans, hospital–physician partnerships, peer review, and physician recruitment and satisfaction development forums.
Fair Market Value. This site provides information to find competitive national survey data and the fair market value narrative that provides a methodology on how to complete a fair market value assessment. The links are in compliance with the Stark II regulations that established a new safe harbor for determining the fair market value of physician compensation.
People and Networks is a resource to find a person who has the information decision makers need to move forward with an idea or project. The clinical operations department provides additional assistance in connecting people. Other items include information pertaining to the Pharmacy Council, the Health Information Management Council, the Educator Network, and related links.
The Physician Practice Management site provides a variety of practice management tools to assist the physician networks in best practice management from a broad spectrum of business disciplines, including finance, operations improvement, compliance, legal, human resource management, planning and marketing, clinical quality, insurance and risk management, and payor contract negotiations.
Sponsored Provider Network provides networking opportunities for executives, controllers, and physician leaders to share best practices in revenue management and expense reduction to drive improved financial and operational performance of the employed primary care physician networks. The meetings are rooted in the application of correct business principles and sharing of management philosophy to develop and achieve performance targets.
The Survey Readiness link connects administrators and clinicians to resources and useful tools for The Joint Commission preparation and continual readiness. It also contains Trinity Health hospitals’ Joint Commission survey highlights, news flashes, and hot topics.
Results
I2S2 has emerged as the go-to online resource for decision makers at Trinity Health. The users span the spectrum of functions across the hospitals. Usage statistics for August 2009 tracked 2,972 average daily hits. More than 901 Pages were viewed by Trinity Health users, who viewed an average of 12.69 Pages per visit. These metrics indicate that I2S2 had indeed been helpful in delivering pertinent information to decision makers. It can be hypothesized that availability of data and the expanse of use contributed to an informed decision maker and resulted in improved performance outcomes.
Trinity Health received the 2004 National Committee for Quality Health Care’s Annual Award. At that time it was only the 12th healthcare system in the United States to be so designated. In 2009, Trinity Health was named as one of the top 10 health systems in the Thomson Reuters 100 Top Hospitals®: Health System Quality/Efficiency Study, which identifies the top U.S. health systems by objectively measuring the clinical quality and efficiency of member hospitals.* terefore, it is reasonable to assume that I2S2 contributed to Trinity Health hospitals’ above national average performance and top decile ranking on many critical measures. This information delivery tool is dynamic and must be updated regularly. To ensure that the information in I2S2 remains current, relevant, and appeals to a wider user base, Trinity Health has instituted a process for reviewing the topical areas and the content available to decision makers, as well as a forum where innovative uses of data are shared.
Each year Trinity Health reviews its quality indicators and targets areas for improvement. Changes in the scientific evidence, data definitions, and public awareness are a few of the several reasons for the periodic review of the I2S2 clinical indicators. Other reasons include improvements in performance and the board’s oversight. Trinity Health has established the following internal criteria for choosing indicators to monitor and disseminate through I2S2.
1. Applicable to multiple reporting organizations (e.g., The Joint Commission/Centers for Medicare & Medicaid Services)
2. Sufficient patientvolume to demonstrate change in performance
3. Emerging opportunities for improvement (includes variation in performance)
4. Evidence of improved process that influences the indicator
5. National norms for indicator are available
6. Alignment of metrics with the Trinity Health strategic plan
7. Burden of data capture does not exceed the value of the indicator
The process of selecting quality indicators involves representatives from each of the MOs, and is subsequently approved by senior management and the board.
In order to assist in this sharing of ideas, the I2S2 People and Networks section enables individuals to identify who to call for assistance. I2S2 has become a virtual library resource for standardized content. Any employee or physician can access the website and view a current or historical document that shows a six-month rolling average performance. A link for each indicator for a particular MO allows the user to drill down and view a 24-month trend graph.
Case Study 3: Clinical Adverse Drug Event (ADE) Alert System
Background
In the 1990s the pressure of managed care challenged U.S. hospitals to ask the following questions: How does a healthcare organization link patient care quality with investment in clinical IT? What part of healthcare is in need for urgent technological support? At about the same time, the issue of adverse drug events or medical errors had gained attention through various publications.2,3 Subsequent studies examined hospitals’ responses and established that ADEs could be prevented.4
Previous research indicates that implementation of computerized ADE systems involves at least three steps: (1) capturing patient data electronically; (2) applying algorithms, rules, and queries to find cases that might be consistent with ADEs; and (3) determining the accuracy of the systems.5 Many hospitals have information systems that contain integrated patient encounter data that include demographics, pharmacy orders, and laboratory results.6 Some hospitals create their own systems, while others integrate off-the-shelf commercial products. There are two forms of ADE systems. Basic systems perform functions such as drug-allergy checking, dosage guidance, formulary decision support, duplicate therapy checking, and drug-to-drug interaction evaluations. Advanced systems perform more complex functions, including dose adjustment, guidance for medication-related laboratory testing, and drug–disease contraindication flags.7
Approach
Trinity Health led the effort to build an advanced ADE alert system with support from a commercial provider, Discern Expert, Cerner Corp., as part of Project Genesis. A rules engine with 17 ADE alert rules was installed. These alerts were triggered using a computerized algorithm after examining demographics, clinical lab values, and medications.
A key assumption to construct an ADE model is that as much as possible, all data about the events and actions taken must be derived and analyzed to develop the model. For instance, the ADE information must include the drugs administered, mode of administering the drug, patient demographics, actions taken, and the result. For an ADE system to be successful, it is imperative that data standards must be developed and followed. The scope of data standardization for the first phase included general laboratory results, pharmacy descriptions/Charge Description Master (CDM), and a partial list of ADT (Patient admitting/discharge/transfer systems)/registration data elements required to support the ADE functionality and patient chart capabilities. However, achieving data standardization is also a political exercise in building consensus. Trinity Health entrusted its Functional and Clinical Councils and Standards Leadership Team with approval from the COO/CFO and Clinical Leadership Council (CLC) oversight groups. The Standards Leadership Council directed the implementation of policies and procedures for change management, audit and reporting mechanisms, and outcome measurement. Data standards have met the requirements and are adjusted to meet the changing business environment.
After literature reviews for medication safety and quality from the pharmacoepidemiological and pharmacoecomonical literature, rules were generated using computerized algorithms to examine demographics with clinical lab values and medications. An example of a rule is presented in the following paragraphs.
Trinity Health ADE Alerts An alert is triggered based on a number of grouped events. A rules engine with 17 of these alerts is generated by computerized algorithms examining patient demographics, clinical lab values, and medications. The ADE alerts are triggered in real time so that any change in medication or lab result will be evaluated as soon as reported. This allows pharmacy intervention immediately and eliminates the possible 12- to 24-hour delay seen before implementation of the system. The pharmacists rely on the system to screen new lab results as they are reported, and this allows the pharmacists to prioritize their workflow to address the most critical issues and patients in a timely manner. The following is an example of this alert process. A pharmacist inputs a physician order for a potassium-containing or potassium-sparing drug. Yet the patient has a lab result for serum potassium > 6.0 mEq/L. Consequently, the potassium medication dose or medication itself needs to be adjusted for these patients because the alert is evoked when a high potassium level is evidenced. Current orders are checked for any of the specified drugs that may cause hyperkalemia.
Trinity Health’s experience suggests that to implement an ADE system successfully, the following conditions must be met.
1. This project must have executive support for the adoption of defined data standards.
2. The data standards must be approved by the senior leadership and implemented organization-wide.
3. .All hospitals and entities must actively participate in the Functional and Clinical Councils.
4. Project participants must provide a timely response to data requests and data review to ensure timely implementation.
5. Following the implementation of data standards, the organization must provide ongoing support of the change management process and commitment to the standards developed.
6. The implementation should be stratified and should be deployed in areas where quick results can be achieved. Learning from such projects can be applied to more complex applications.
7. The recommended model must be accurate, consistent, user-friendly, and compliant with existing computer applications and all governing bodies.
8. Although data standards do not cause any operational changes, redesign efforts must be accommodated in the clinical and patient administration projects.
9. A change management process will be defined and followed to add to the standards. Conformance to standardization will be monitored and reported.
Results
Once buy-in from the stakeholders was achieved, work planning and milestone schedules for the laboratory and pharmacy were established. Trinity Health’s philosophy is to design once, implement many times. The ADE application followed this guiding principle to implement the ADE system across several hospitals. For ease of maintenance and updates, the computing hardware was standardized and the ADE application software was centrally developed. In using the ADE system, Trinity Health focused on evaluating the effects and derived benefits from usage and expected to achieve cost savings and reductions in patient mortality in line with the published literature that decreases in the harmful events save both human lives and money.
The ADE project implementation assigned a project manager, a data manager, a systems technical analyst, a systems business analyst, and an administrative support staff. There were 4.5 FTEs (full-time equivalent employees) at start-up and implementation, and now 2.5 FTEs are assigned for maintenance and reporting. The following are additional activities required by the hospitals to support the ADE project.
| Lab kickoff meeting | 2 hours/site | Laboratory Council |
| Lab phone interview | 1–2 hours/site | Med Tech |
| Lab Standards Review | 8 hours/site | Med Tech × 3 sites |
| Lab standards approval | 3 hours | Laboratory Council |
| Pharmacy kickoff meeting | 2 hours | Pharmacy Council |
| Pharmacy phone interview | 1–2 hours/site | Pharmacists |
| Pharmacy standards review | 24 hours | Pharmacy subgroup |
| Pharmacy approval | 3 hours | Pharmacy Council |
| Pharmacy mapping review | 8 hours/site | Pharmacist |
| Reg./HIM/pt. acct. kickoff meeting | 2 hours/site | Directors |
| UB92 review | 8 hours | Pt. admin./reg./HIM managers |
| UB92 mapping review | 8 hours | Pt. admin./reg./HIM managers |
In deploying the ADE system among the hospitals, the senior leadership declared that a financial impact analysis was not required. The urgency and the impact on patient mortality outweighed the need for economic justification. As seen in the preceding text, labor was the cost driver for implementing the ADE system. The question then is: How much cost has to be absorbed when the financial benefits are not assessed? For ADEs there are significant financial costs affixed to each event. Yet there are clinical “costs” as well in human pain and suffering, not to mention litigation. Previous literature has cited that each ADE costs about $6,685,8 and that computer systems play a decisive role in preventing ADEs.9 Thus, there is significant evidence in the literature to support that preventing ADEs can reduce hospital costs in addition to increasing patient care quality.
At Trinity Health the impact of implementing the ADE system was evident principally in the reduction in pharmacy costs, a savings of 5%. These pharmacy cost savings in the targeted hospitals exceeded US$3.5 million. Internal and external control groups demonstrated no such cost savings. There was also evidence of decreases in severity-adjusted LOS and mortality rates.10
Conclusion
This chapter chronicled three case studies as milestones in the journey of Trinity Health to gather, process, and disseminate data to improve patient safety and outcomes. We established that for hospitals to be effective in using information for improved decision making, physicians’ leadership and involvement is necessary. Once metrics are agreed on, an effective data delivery mechanism must be put in place. Through rich descriptions and examples we presented Trinity Health’s intranet-based information system, I2S2. Descriptions of categories of information content provide an overview of range of data available to the decision makers. Finally, we presented an example of a value-added application that emerged from the leadership by physicians and the development effort of the information systems professionals to implement an ADE alert system. Lessons learned from building the ADE system will assist readers in avoiding pitfalls and preparing for their own value-added applications.
This chapter was originally published in Healthcare Informatics, Improving Efficiency and Productivity, Taylor & Francis, New York, 2010.
References
1. Kohli R, Piontek F, Ellington T, VanOsdol T, Shepard M, Brazel G. 2001. Managing customer relationships through an e-business decision support application: A case of hospital physician collaboration. Decis Support Syst 32:171–187.
2. Bates DW, Leape LL, Petrycki S. 1993. Incidence and preventability of adverse drug events in hospitalized adults. J Gen Intern Med 8:289–294.
3. Grasela TH, Walawander CA, Kennedy DL, Jolson HM. 1993. Capability of hospital computer-systems in performing drug-use evaluations and adverse drug event monitoring. Am J Hosp Pharm 50: 1889–1895.
4. Bates DW, Leape LL, Cullen DJ et al. 1998. Effect of computerized physician order entry and a team intervention on prevention of serious medication errors. Jama 280:1311–1316.
5. Evans RS, Pestotnik SL, Classen DC, Horn SD, Bass SB, Burke JP. 1994. Preventing adverse drug events in hospitalized patients. Ann Pharmacother 28:523–527.
6. Raschke RA, Gollihare B, Wunderlich TA et al. 1998. A computer alert system to prevent injury from adverse drug events—Development and evaluation in a community teaching hospital. Jama 280:1317–1320.
7. Wolfstadt JI, Gurwitz JH, Field TS et al. 2008. The effect of computerized physician order entry with clinical decision support on the rates of adverse drug events: A systematic review. J Gen Intern Med 23:451–458.
8. Senst BL, Achusim LE, Genest RP et al. 2001. Practical approach to determining costs and frequency of adverse drug events in a health care network. Am J Health Syst Pharmacy 58:1126–1132.
9. Yan Q, Hunt CA. 2000. Preventing adverse drug events (ADEs): The role of computer information systems. Drug Inf J 34:1247–1260.
10. Piontek F, Kohli R, Conlon P, Ellis J, Jablonski J, Kini N. 2010. Effects of an adverse-drug-event alert system on cost and quality outcomes in community hospitals. Am J Health Syst Pharmacy 67:613–620.
_______________
* http://www.reuters.com/article/pressRelease/idUS87944+10-Aug-2009+PRN20090810. The study evaluated 252 health systems—with a total of 1,720 hospitals—on measures of clinical quality and efficiency. The top ten represent the top 2.5% of the systems studied. Five measures of performance were used to evaluate systems: mortality, complications, patient safety, length of stay, and use of evidence-based practices. All of these are available in I2S2. I2S2 allows decision makers in all Trinity Health hospitals to leverage the collective clinical knowledge and best care practices and for rapid replication and improving the quality, safety, and satisfaction of patients throughout the course of their delivery of care.
