13
TAKING ACTION FOR HEALTH PLAN MEMBERS’ HEALTH
Contents
Actionable Information: A Conceptual Framework
Knowledge Discovery through Multivariate Analytics
“Hot spotting” has practically become the battle cry for managed care organizations since an article of the same name was published in The New Yorker in January 2011.1 In this article a physician, Jeffrey Brenner, realized after attempting to save a shooting victim that it was possible to study healthcare utilization patterns in much the same way assault and crime patterns are tracked. For example, Brenner discovered that across a six-year period, more than 900 people in Camden, New Jersey, accounted for more than $200 million dollars in healthcare expenses. One of these patients had 324 admissions in five years while the care for another patient cost $3.5 million dollars. In addition, he found that 1 percent of the patients who used Camden’s healthcare facilities accounted for 30 percent of the total costs.
Called the “Top 1%” by the managed care industry, Brenner’s observation was important not because it was new information,2 but because it clearly articulated this situation to the general public. Patients like these, “hot spots,” were the ones in need of better quality of care. From his experience as a physician, he knew that those patients with the highest costs are usually the ones who have experienced the worst care. Though hardly a new idea, the concept of identifying and intervening with the most severe or clinically complex patients to lower future healthcare costs has seen resurgence in the managed care arena.
State Medicaid agencies have embraced the “hot spotting” concept, challenging their Medicaid Managed Care Plans (MCPs) to decrease overall healthcare expenditures by increasing the quality of care for their member populations, especially those who are currently a significant cost burden to the program. As early as 2005, the Ohio Commission to Reform Medicaid (OCRM) published a report on Ohio Medicaid making recommendations and outlining action steps focused on (1) long-term care, (2) care management, (3) pharmacy management, (4) member eligibility, (5) financial administration, and (6) overall program structure and management.3 Recognizing the difficulty of healthcare reform, this report, and subsequent study, underscored the complexity of the relationships between quality, delivery, management, administration, cost, and payment of healthcare.
Clearly, quality of care, and cost of care are on a collision course. Is it possible to develop a system that establishes and supports our nation’s need for quality, affordable healthcare, or have decades of fee-for-service payment systems that are independent of quality of care and/or patient outcomes made it impossible to reform health care delivery? Unfortunately, as long as healthcare facilities, providers, and suppliers fail to work together and independently treat patients as profit centers, there appears to be little hope for healthcare reform.
This is one reason that the new healthcare reform law is so controversial. It is widely known that health plan members who receive the right type of care at the appropriate time have better health outcomes, thereby decreasing their cost burden on an already overstressed healthcare economic system. Proponents and critics of healthcare reform do agree on one thing: there are ways to decrease overall healthcare costs through population-based care management programs. Brenner asserted in The New Yorker article, “For all the stupid, expensive, predictive-modeling software that the big venders sell, you just ask the doctors, ‘Who are your most difficult patients?,’ and they can identify them.” tough this statement has simplistic appeal, it cannot exist as a management strategy applicable to broad populations. The process of designing and running a population-based program is not as trivial as this statement implies.
To be effective, a data-driven, procedural approach must be taken, which allows for the coordination and collaboration of all constituents in the healthcare delivery process. Moreover, robust data management, data mining, and analytic processes are essential for successful population-based programs because improvements in quality and cost of care can occur only when the right members receive the right services at the right time.4–6 For these data-driven methods to influence clinical and financial outcomes of our healthcare delivery system, the information derived from them must be actionable.
Clearly, care management programs already exist to address these issues. However, one must consider the following questions: If there are already programs, protocols, processes in place, why are we not seeing significant improvements in quality and cost of care? Why are health plans, facilities, and provider practices still challenged with improving quality of care while reducing overall costs? Therefore, we are not presenting new concepts in care management, but rather a conceptual framework comprising factors influencing one’s overall healthcare experience. This combination of factors allows for the optimization of care management interventions that maximize the ability to target and identify those members whose cost burden will continue to increase in the absence of care management support activities.
To develop actionable care management information, it is necessary to create a framework that takes into account data derived from numerous sources. Expert systems created to support Clinical Decision Support Systems (CDSS) are relatively common in facilities and provider offices. Many of these systems are designed to improve (1) patient safety, (2) quality of care, and (3) efficiency of delivery.7,8 these expert systems are extremely helpful in clinical settings because they provide actionable information. That is, the information derived from these systems is directly applicable to improving the treatment of specific patients. If expert systems are successfully implemented at a provider/facility level, then it is reasonable to expect that expert systems can also be implemented at a health plan/managed care level.
Actionable Information: A Conceptual Framework
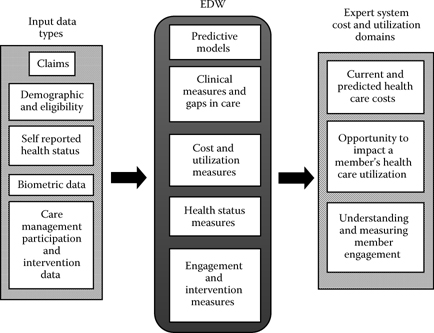
We propose developing a care management expert system that combines information from three healthcare cost and utilization domains.
• Current and Predicted Healthcare Costs
• Utilization Impact
• Member Engagement
Using current and predicted healthcare costs, it is possible to identify those health plan members who are currently highest cost and will remain high cost in the absence of healthcare interventions. Because it is known that current high cost does not necessarily predict future high cost,9 predictive modeling is necessary to determine those individuals with the highest probability of either remaining or becoming high-cost health plan members. Without these analytic methods, it would not be possible to direct care management interventions to the right risk groups to significantly influence the overall cost burden of these health plan members. To simplify the challenge, it is helpful to visualize the relationship between current and future healthcare costs using a resource allocation matrix.10
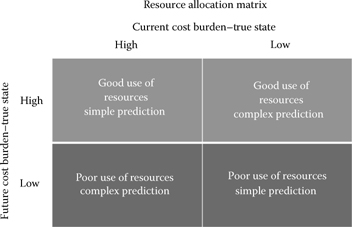
As shown in the diagram above, the relationship between current and future cost burden is an important factor in determining where to allocate resources. Simple predictions (i.e., those that do not require involved predictive modeling techniques) allow for the classification of members into either “good use” or “poor use.” Likewise, complex predictions (i.e., those that require involved predictive modeling techniques) do the same. It is, obviously, more difficult to determine those low-cost members who will become high cost as well as those high-cost members who will become low cost. By identifying those future high-cost members, the correct resources can be allocated to the appropriate interventions needed to help control healthcare costs. As the challenge of this care management strategy is to control future healthcare costs, the first step in creating actionable information is to classify the member population into these three groups.
Knowledge Discovery through Multivariate Analytics
Simple database queries can be utilized to search vast data sources to identify current high-cost patients in a patient population (e.g., those incurring extensive health treatments, as mentioned in The New Yorker). This information can be beneficial because resources can be applied to those particular cases to address those factors contributing to continued poor health maintenance. One limitation of this approach, however, is that it requires individuals to become high service utilizers or high cost before resources can be applied to alleviate or mitigate the problem. In other words, the limitation of this more hind-sight or reactive analytic method is that the focus is placed on what has already happened, where little knowledge is generated as to why individuals become high cost.
More effective cost reduction and health enhancement policies can be achieved through proactive analytics that identify likely future “poor health” or high-cost candidates.11 Advanced analytical methods applied to robust data resources enable decision makers to identify individuals at risk of requiring extensive health treatments or high-cost candidates. Methodologies such as logistic regression help identify noteworthy patterns existing in corresponding data. These patterns can include variables involving patient demographic and behavioral information, symptomatic and diagnostic data, and treatment-related data, to name a few. The resulting models not only identify the segments of a patient population that are likely high-cost candidates but also provide the possible factors that lead patients to be high cost—or the “why” behind the high-cost results.
Advanced analytic methods that incorporate a multivariate approach and the utilization of mathematical and algorithmic processing of data in conjunction with statistical testing techniques are often referred to as “knowledge discovery techniques.” The “knowledge” refers to the identification of patterns or relationships between variables in a particular data set that explain “why” things happen, not simply “what” has happened. Perhaps the most important information to extract from data with regard to the complexity of individuals’ health status include patterns in dietary behavior, physical attributes, treatment and medication practices, and so forth that can provide insights as to what combination of behavioral and descriptive variables lead to a less healthy, higher cost individual. This information is truly actionable as it empowers healthcare providers to more accurately apply available resources to mitigate costs and maintain a healthier population by implementing preemptive or proactive treatment for high-risk candidates, thus mitigating costs before they incur. The result is not only reduced cost for providers but also a healthier population.
The next step in the conceptual model involves determining the opportunity to impact a member’s healthcare utilization level. This step is multifaceted and requires the integration of both a member’s health status as well as his or her use of healthcare services. Health status refers to the current standing of an individual’s clinical, physical, and mental health.12 Health status is commonly determined through general health assessments (GHAs), health risk assessments (HRAs), clinical severity estimators (e.g., Adjusted Clinical Groups [ACGs]), as well as other sources of member-specific healthcare information (e.g., provider records, treatment notes, etc.). This type of information allows care managers to better understand if they can impact these members’ utilization behaviors, given their current health statuses. If a member suffers from a disease or condition that cannot be impacted by care management interventions, then decisions must be made as to the level and type of services and support he or she receives.
Similarly, a member’s utilization history must be analyzed to determine the opportunity to modify his or her behavior. For example, it has been well documented that care management interventions can influence health plan members’ emergency department and hospital admission rates.13 With the current market focus on emergency department diversion (EDD), readmission rates, and prescription drug rates, it is becoming increasingly important to integrate these sources of information. The development of enterprise data warehouses (EDW) at health plans is a direct result of the need to collect and use these data sources to track their members’ utilization behaviors. As described earlier from the “hot spots” article, when a health plan member has 324 admissions in a five-year period, one has to ask if this level of utilization was necessary. Consequently, the second step of this process involves an assessment of health status and utilization history, which further filters the membership population by taking those members who are predicted to be future high cost and identifying those who can be impacted by care management interventions.
Understanding and measuring member engagement is the final step in this conceptual model. Engagement can mean many different things, but in this context it refers to a member’s willingness to transmit, receive, and act on customized communications. Engagement is emotional in nature; it often describes one’s connection with healthcare providers and predicts how actively a member participates in the management of his or her own healthcare.14 In other words, engagement involves a member’s management of his or her own healthcare services to meet his or her healthcare needs. When members are engaged, they are actively involved and focused on their healthcare behaviors, resulting in better choices, better provider communications, and, ultimately, better outcomes.15
Patient adherence to treatment regimens is a good example of why engagement is important in this conceptual model. For example, glycemic control is essential for individuals suffering from either type 1 or type 2 diabetes. This condition requires a high level of self-management; in other words, highly engaged individuals with diabetes have much better outcomes that those who are not engaged. Engaged individuals will most likely adhere to the treatments prescribed by their providers.16,17 therefore, when members are defined by their future high cost, impact of care management interventions, and engagement in healthcare, the resulting actionable information increases the opportunity provide the right members, the right services, at the right time (see following figure for a description of the process).
Conclusions
There is no mistaking that population-based care management programs are difficult to develop, implement, and manage. The following are a few of the more pervasive issues.
• Healthcare data sources are seldom standardized, often full of errors, and difficult to aggregate.
• Privacy and security regulations add additional complexity to data management efforts.
• Administrative claims data are collected on multiple systems and have varying file formats and record layouts.
• Health plan membership constantly changes, with members entering and exiting the program based on employment and eligibility status.
• Provider enrollment is extremely variable based on the provider’s participation status, physical location, and professional specialty.
• The prevalence of chronic conditions continues to rise at an alarming rate.
• Treatment and drug regimens continually evolve as well as practice guidelines, evidence-based medicine, and medical technology.
• Healthcare reform brings new concepts such as Health Homes, Accountable Care Organizations, and Health Insurance Exchanges.
The preceding list only scratches the surface. However, as one contemplates current healthcare delivery challenges, a common theme surfaces. All of these issues have a singular dependency—actionable information.
The following figure represents a very elementary formulation of the conceptual framework proposed in this chapter. The input to this model (Multiple Data Sources) continues to be an important topic by itself. Data management, data aggregation, and data warehousing of the multitude of disparate healthcare data sources must occur before any other activity can take place. The scope and magnitude of this effort cannot be overemphasized. To manage health plan members effectively at a population level, administrative claims data sources (e.g., medical claims, pharmacy claims, durable medical equipment and supply claims, laboratory claims, behavioral health claims, dental claims, home health claims, skilled nursing and nursing home claims, etc.), health and risk assessment data sources (e.g., general health assessments, health risk assessments, disease specific surveys, etc.), risk and grouping data sources (e.g., Episode Treatment Groups®, Diagnosis-Related Groups, adjusted clinical groups, etc.), as well as many other healthcare data sources must be combined in an understandable, functional way. Health plans and business intelligence vendors are working on this challenge, with varying degrees of success as they work toward building enterprise data warehouses (EDWs). This is the healthcare industry’s biggest challenge because without clean, robust data, it is not possible to implement data-driven care management programs, not to mention all of the new processes and programs created by the Affordable Care Act (ACA).
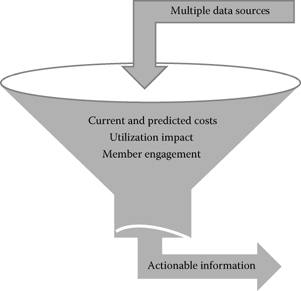
Once data are entered into the system, the process of identifying the best candidates for care management programs begins. Following the proposed framework, each of the three categories acts as a population filter. Once the target population is identified (e.g., members with asthma), current and predicted cost burden is calculated for each individual member. The result of this analysis is a ranking of all members with asthma (continuing with this example) from highest to lowest predicted cost. The next step involves assessing the estimated utilization impact of the care management program’s interventions on these members with asthma. Those members who are determined to be most “impacted” by the care management program are ranked higher than those who are not. These two sources of information (predicted cost burden and utilization impact) are then combined to produce a new risk ranking; this ranking takes into account those members with the highest predicted cost burden who also have the highest probability of utilization impact by the care management program.
Combining these two sources of information gives care managers the ability to identify not only those members with the highest predicted costs but also those members they will have the best opportunity to impact. Consequently, a member with high predicted cost with low utilization impact would be ranked lower than a member with a moderately high predicted cost with a high utilization impact. Using this methodology, the entire population of members with asthma can be ranked from highest to lowest risk based on predicted costs and utilization impact. As described previously, this actionable information allows care managers to make appropriate resource allocation decisions. Because it would be a poor use of resources to concentrate efforts on high-cost members with low to no probability of utilization impact, this information would be very valuable for program management.
Nevertheless, this proposed framework has one final filter: member engagement. Once the member population is identified and risk ranked by predicted cost and utilization impact, member engagement is assessed. It does not matter how high someone’s financial risk might be or how impacted he or she could be by care management interventions if the member is not engaged in the process. If a member is not emotionally invested in the program, there is little chance that he or she will benefit from the care management interventions. Without engagement, care management does not work. Consequently, at a population level, using engagement as the last filter will further refine the information derived from the model, thereby increasing the chances that care managers are expending efforts on those members who will be high future cost, have high utilization impact opportunities, and are engaged in the care management process. This framework, comprising three information filters, will identify those members who, if left unattended, will present the highest cost and utilization risk and are able to engage successfully in the program. This information is essential at a population management level because only limited care management resources are available and correct resource allocation is paramount to program success.
Clearly, population management programs rely on data-driven methods to target populations, identify high-risk members, allocate limited resources, and assess program outcomes. To increase quality of care while decreasing healthcare costs, care management programs must focus their efforts on intervening with the right members, with the right services, at the right time. Once data are transformed into actionable information, program successes are possible, resulting in positive care management utilization and financial outcomes. Possessing data is not enough—actionable information must be created and used by health plans to meet current and future challenges. The conceptual model proposed in this chapter is one example of how the thoughtful consolidation of information can assist in the correct allocation of resources in a population-based care management program.
To be effective, a data-driven, procedural approach must be taken, which allows for the coordination and collaboration of all constituents in the healthcare delivery process.
Acknowledgment
This chapter was first published by the International Institute of Analytics, Using Advanced Analytics To Take Action For Health Plan Members’ Health, January 2012.
References
1. Gawande A. 2011. The hot spotters: Can we lower medical costs by giving the neediest patients better care? The New Yorker January 24.
2. Stanton M, Rutherford M. 2005. The high concentration of U.S. health care expenditures. Research in action, Issue 19. AHRQ Pub. No. 06-0060. Rockville, MD: Agency for Healthcare Research and Quality.
3. Revisiting Medicaid reform: A project of The Center for Community Solutions and the Center for Health Outcomes, Policy, and Evaluation Studies (HOPES) of Ohio State University. 2009. A status report on recommendations from the Ohio Commission to Reform Medicaid four years later: January 2005–January 2009.
4. Cousins M, Shickle L, Bander J. 2002. An introduction to predictive modeling for disease management risk stratification. Dis Manage 5:157–67.
5. Perry T, Tucker T, Hudson L, Gandy W, Neftzger A, and Hamar G. 2004. The application of data mining techniques in health plan population management. IT solutions series: Managing data mining. Hershey, PA: Idea Group Publishing.
6. Perry T, Kudyba S, Lawrence K. 2007. Identification and prediction of chronic conditions for health plan members using data mining techniques. In Data mining methods and applications (pp. 175–82). New York: Taylor & Francis.
7. Coiera E. 2003. The guide to health informatics, 2nd ed. London: Arnold.
8. Raghupathi W. 2007. Designing clinical decision support systems in health care: A systematic approach. Ijhisi 2(1):44–53.
9. Ridinger M, Rice J. 2000. Predictive modeling points way to future risk status. Health Manage Technol 21:10–12.
10. Donaldson C, Currier G, Mitton C. 2002. Cost effectiveness analysis in health care: Contraindications. BMJ 325:891.
11. Kudyba S, Hamar B, Gandy W. 2005. Enhancing efficiency in the health care industry. Commun ACM, pp. 107–10, December.
12. Kudyba S, Perry T, Rice J. 2008. Informatics application challenges for managed care organizations: The three faces of population segmentation and a proposed classification system. IJHISI 3(2):21–31.
13. Brandon W. 2011. Reducing emergency department visits among highusing patients. J Fam Pract FindArticles.com. November 15, 2011.
14. Arnold S. 2007. Improving quality health care: The role of consumer engagement. Robert Wood Johnson Foundation Issue Brief October 2007.
15. Protheroe J, Roger A, Kennedy A, MacDonald W, Lee V. 2008. Promoting patient engagement with self-management support information: A qualitative meta-synthesis of processes influencing uptake. Implement Sci 3:44.
16. Delamater A. 2006. Improving patient adherence. Clin Diabet 24(2):71–77.
17. Milano C. 2011. Can self-management programs ease chronic conditions? Managed Care, pp. 28–31, January.
