Chapter 10. Operational Case Studies
Sections
Timeliness of Self-Pay Collections on Commercial Accounts at Commonwealth Health Corporation
Reducing Ambulance Diversions at Providence Alaska Medical Center
Better Patient Charge Capture at Yale-New Haven Hospital
Ensuring Accuracy in Managed Care Operating Room Carve-Outs at Virtua Health
Addressing Bed Management at The Nebraska Medical Center
The Corporate Advance Directive at Valley Baptist Health System
Optimizing Respiratory Care Services at Valley Baptist Health System
It is sometimes difficult to categorize improvement efforts as either truly clinical or operational because the goals and processes often overlap to some degree. Clinical efforts, such as medication error reduction, may be linked more directly to patient care at the bedside. However, many of the projects within healthcare target opportunities in areas such as
• Reducing report turnaround time
• Improving accuracy in billing and collections
• Increasing radiology throughput
• Streamlining patient registration processes
• Optimizing information technology implementation
• Reducing patient wait time in ED
• Improving OR scheduling and room utilization
• Expanding volume and bed capacity
Addressing such issues successfully contributes to the overall capacity of the organization to function efficiently and with optimal resource utilization. Efforts to reduce paperwork and streamline nursing workflow, for example, can translate to additional time spent caring for patients. Money that is saved by eliminating redundant or unnecessary steps in one area can be used to expand services, hire additional staff, or introduce new life-saving technologies in another area.
Process improvement projects that reduce errors and inefficiency help to create a better environment in which to give and receive care. The case studies in this chapter illustrate this point and highlight the benefits of operational Six Sigma projects when appropriately selected and driven by the voice of the customer.
Timeliness of Self-Pay Collections on Commercial Accounts at Commonwealth Health Corporation
One Six Sigma initiative that provided Kentucky’s Commonwealth Health Corporation (CHC) with some early financial results targeted the timeliness of self-pay collections on commercial accounts. As employers increasingly pass healthcare costs to employees through higher deductibles and co-pays, this issue is one that many hospitals will eventually need to address.
Six Sigma Master Black Belt Pam Jones and her team began an effort to study the process for patients presenting with commercial insurance in an attempt to collect co-pays, deductibles, and co-insurance at point of service. In scoping the project, the focus was on reducing the length of time required to collect on commercial accounts and increasing the collection percentage on patient balances.
The team presented a strong business case for this initiative. The initial Z-score was 1.8, and the preliminary cost of a defect was $1,504,099. In addition to the financial aspect, this issue also represented a customer satisfaction issue and a significant amount of re-work.
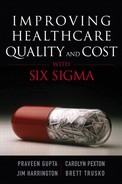
They decided to implement the pilot in the emergency department (ED) because data analysis had demonstrated that this area held the greatest opportunity for improvement, as shown in the Pareto chart for location in Figure 10.1. ED patient flow processes were modified to ensure all patients were routed through a formal “checkout” after being treated and discharged by clinicians. Financial counselor positions were established and comprehensive training was provided prior to implementation.
Figure 10.1. Pareto chart for location
The following information was provided by Commonwealth Health Corporation as background on the implementation plan for this project:
Improving and Controlling the Process
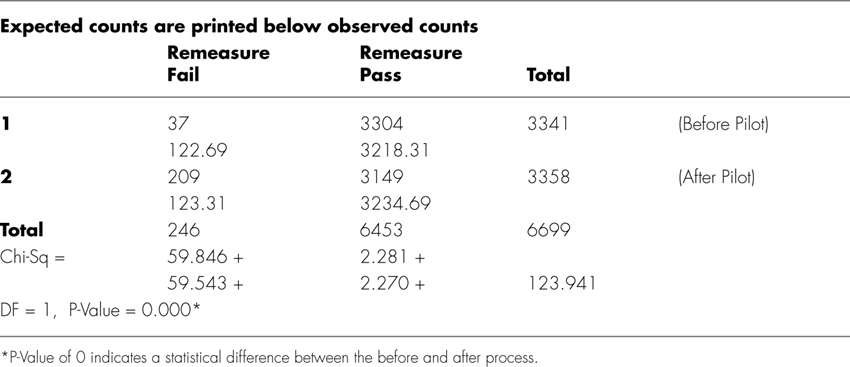
Using Chi Square, the team re-evaluated the process and found a statistical difference between the before and after measurements (see Table 10.1).
Table 10.1. Chi-Square Test: Remeasure Pass, Remeasure Fail
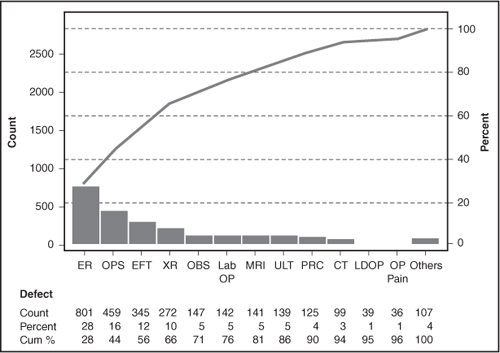
By the Control phase of this project, the Six Sigma team at CHC had achieved a 92 percent process improvement with final cost savings of $1,388,401 (see Figure 10.2).
Figure 10.2. Final cost savings and cost of a defect
Extending the benefits of this initiative, the project findings and solutions have since been replicated in other areas of the health system. The final results underscored the success of the initiative. Using the Six Sigma DMAIC process, the team was able to reduce the probability of a defect occurring from 37 percent to 2.9 percent, and improve the overall process by 92 percent, as shown in Figure 10.2.
Reducing Ambulance Diversions at Providence Alaska Medical Center
Many hospitals across the U.S. have had to confront the issue of emergency department overcrowding. In some cases, hospitals are forced to divert ambulances to other facilities due to lack of space or inpatient capacity. Several years ago, Providence Alaska Medical Center (PAMC) began to notice an increase in its ambulance diversion rate, which had risen from 3 percent to 5 percent in 2000 and then to 16 percent in 2001. The divert rate peaked at 21 percent in 2002—the hospital put policy and process changes in place and developed a web-based inpatient capacity tool.
Although the diversion rate fell to 12 percent in 2003 and to 8 percent in the first three months of 2004, the numbers again began to rise. In the second quarter of 2004, the diversion rate tripled to 24 percent and peaked in the month of July with the ED being on diversion 51 percent of the time.
In June 2004, a new ED project was launched using Six Sigma and change management methods. The project targeted reducing diversions as a result of critical care at capacity to zero, and reducing diversions as a result of ED at capacity to 3.4 percent.
The team began by trying to correlate multiple sources of information, using tools such as Work-Out to reach consensus on a common data set that would be made accessible to all stakeholders. Prior to this project, different departments had maintained multiple data sets on the same diversion episodes. Definitions and time stamps were not standardized, and access to the various databases was restricted.
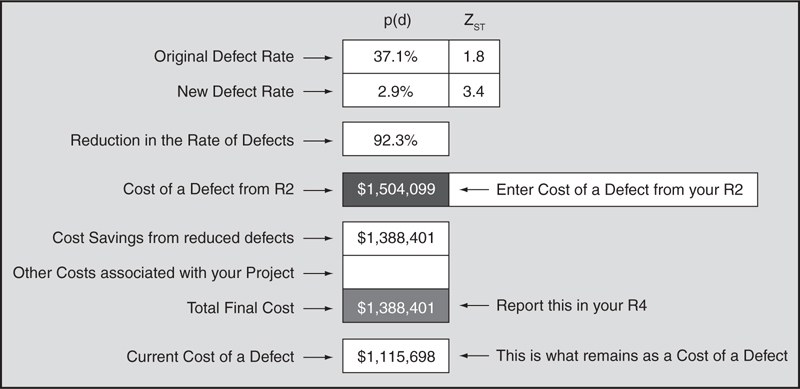
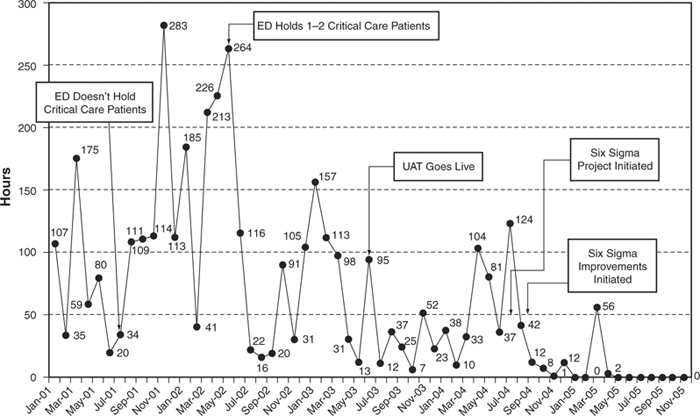
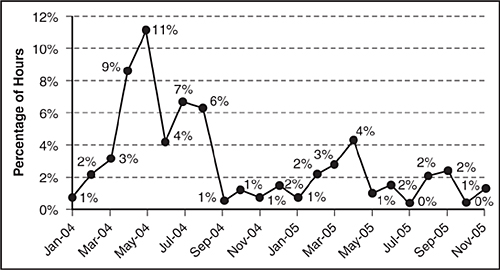
The team quantified the financial impact by estimating that the average cost for one hour of diversion was $3,400. A review of the data during the Analyze phase of the project indicated that the solution must focus on the adult critical care (ACC) unit (see Figure 10.3).
Figure 10.3. Linkage between diversion and access
The project team established clear definitions for each type of diversion and simplified the data-entry process, saving all raw entries in an electronic record designed to reduce errors. They created new standard operating procedures and defined roles and responsibilities to minimize variation in the way data would be gathered and interpreted.
With greater rigor in the data collection process, the team began to develop solutions for the primary causes of diversion. According to Dr. David Ingraham, Black Belt at PAMC, one of the most enlightening aspects of the project came from using the process to disprove an assumption that critical care diversions were due to not having an available bed. When “No Bed Available” was indicated, however, it was often because there was no staffed bed, indicating staffing issues rather than a lack of physical beds.
Through statistical analysis, the team was able to develop viable solutions:
• New SOPs were created for the collection of diversion data
• An electronic data collection tool was developed
• SOPs were developed for the translation of raw data to a summary sheet
• Diversion summary data was published on an accessible hospital intranet site
• Goals and targets for diversion were established
• Staff was educated on the importance of length of stay as a contributor to staffing needs in the adult critical care unit
• A high census policy was developed to correct resource issues before a diversion becomes necessary
• An interventional cardiac recovery unit was developed to reduce burden on the critical care unit
• Alternatives were established for placement of critical care patients with prolonged lengths of stay
• Critical care house conveniences were identified at times of high census
• The team recommended proper use of float pool staffing for unexpected vacancies rather than supporting core staffing
After changes were implemented, the diversion rates dropped and ED access improved, as illustrated in Figures 10.4 and 10.5.
Figure 10.4. Critical care diverts 2001–2005
Figure 10.5. Percentage of hours ED at capacity 2004–2005
The original timeline to achieve the target rates was 1.5 years, or by the end of 2005. The project was completed well ahead of schedule in January 2005. Key project benefits included:
• Net revenue increase of $1.04 million on annualized basis
• Better patient access through decreased diversions due to “critical care at capacity” by an average of 26 hours per month
• Provided substantial opportunities for organizational learning, collaboration, and growth
The project to reduce emergency department ambulance diversions was part of a larger improvement initiative at Providence Alaska Medical Center and across the Providence Health System. The organization has trained its own Master Black Belts, Black Belts, and Green Belts and is now incorporating Lean into its performance improvement toolset.
Note: This project was originally shared through an article by John Kalb and David Ingraham, MD, published in the iSixSigma healthcare newsletter (http://healthcare.isixsigma.com/library/content/c061011a.asp).
Better Patient Charge Capture at Yale-New Haven Hospital
Hospitals lose millions of dollars each year due to patient care items that are used but somehow never charged or reimbursed. A Six Sigma team at Yale-New Haven Hospital (YNHH) in Connecticut decided to look at the opportunities related to patient charge capture and began the scoping process for a project.
Previous attempts to address this issue had not met with great success due to the large number of items that might be included in a review. To ensure the project would be both manageable and measurable, the team decided to focus on the top 12 supplies based on quantity and expense, and also limit the scope of the project to 7 pilot units.
As they began the data collection and analysis process, they found that only 35.7 percent of medical/surgical supplies were being captured on inpatient nursing units. Based on this finding, they calculated an opportunity to increase gross charges by an estimated $4.5 million for just the top 12 supplies.
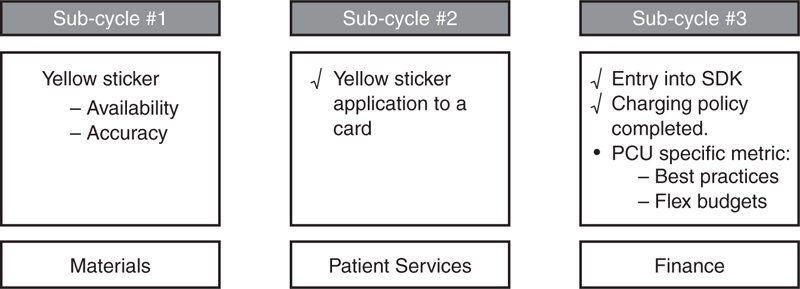
Another observation the team made was that there wasn’t a standard method of processing patient charge items within the inpatient units. Beyond the “Big Y” of patient charge capture, there were several sub-cycles to focus on. They created a process map that revealed numerous intertwined steps—making it difficult to see how any items could be properly charged. The process was divided into three sub-cycles with three sponsors (see Figure 10.6).
Figure 10.6. Three sub-processes and sponsors (sub-cycle 1: items without stickers)
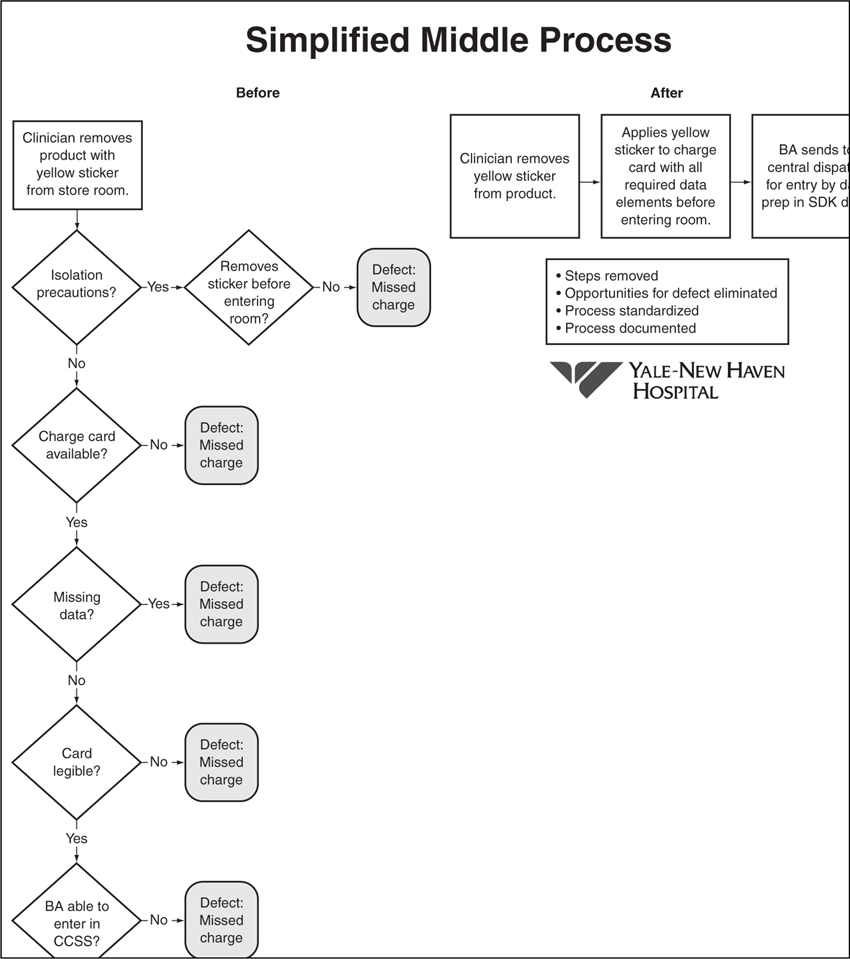
One of the sub-cycles the team decided to target was improving the documentation of the five required data elements on the charge cards. They believed this could help to reduce cycle time, beginning with use of product to charging of product, defects such as cards that can’t be billed, and re-work associated with manual data capture.
Technology was another area to consider. Although a variety of technology solutions are available for inventory management and billing, they are often costly and do not guarantee a return on investment. Furthermore, as many healthcare organizations have discovered the hard way, implementing a new technology on top of a broken process can lead to disappointing results. Simply automating a broken process isn’t the answer.
To address some of the issues and determine the factors and solutions within its immediate control, the team held a Work-Out with nurses, patient care associates, and business associates. Frequently, the staff would point to missing yellow stickers on products. This was considered out-of-scope for the first Work-Out. The patient care unit staff was informed that another team would explore reasons for missing yellow stickers.
The primary factor within the immediate control of the unit staff was incomplete information on the charge card to which the yellow stickers were affixed. Cards were not accessible to clinicians, or one of the five essential data elements was missing from the charge card. Many business associates complained that the product names on the yellow stickers did not match the computer name. After the Work-Out, a new process was implemented in which the five data elements would automatically be printed on labels, replacing the handwritten process. This prevented missing and illegible data elements on the charge card. It was also determined that the current process of business associates entering cards into the computer would be replaced with a centralized data-entry process that could be more easily monitored. Ensuring appropriate staff training on the new procedures and written reference materials was another key change the team put into place.
Figure 10.7 illustrates an effort to streamline and simplify sticker application to a patient charge card. One area of concern involved making sure all products had yellow stickers for capturing charges, because an audit revealed that 10 percent of the items were arriving from vendors without them. Auto-substitution and back-ordered items were the two factors most often behind the missing stickers. Also, the outer package sometimes had yellow charge stickers affixed, but the product inside did not. The team held a second Work-Out to simplify some of the process steps, making sure stickers were on the products when they were delivered to the units.
Figure 10.7. Simplified middle process
Developing and Piloting Solutions
As a result of the second Work-Out for the first sub-cycle, three solution areas surfaced: improving the pick process, developing an accurate list of patient charge items, and improving communication systems.
There were a number of suggestions to improve the pick process, and several changes were implemented:
• Training and awareness programs for pickers both at YNHH and the supplier
• Develop solid QA procedure to ensure patient charge items were labeled at supplier and YNHH
• Develop procedure to flag auto-substitutions
• Achieve visual control by flagging on shelf what is to be a patient-charged item at YNHH and the supplier
• Instruct all YNHH pickers on how to print out own labels
• Supplier to scan all YNHH orders for charge items
• Education and QA orders to ensure labels are attached in the proper spot
• Supplier and YNHH representative to meet regularly to provide feedback and discuss problems
To address the accurate list of items, the following solutions were proposed:
• Finance and Materials to agree on what is chargeable
• Supplier and YNHH materials department will complete an accurate list of patient charge items
• A new process for reconciling different lists between YNHH and supplier using automation
• New patient charge policy and standard operating procedure
• Users educated with “getting-to-know you” patient charge items
• Any patient charge item will be reviewed with “unit of measure,” which is each item versus carton/pack to validate that patients are charged for each as appropriate
With respect to the communication systems, solutions included the following:
• Communicate with supplier when product was not labeled; standardize this communication daily and then weekly
• All parties work off accurate list of patient charge items
• Materials should always check for yellow stickers to ensure consistent training
• Floor staff (RNs, PCAs, BAs) should be aware of which items are patient charge items, and ensure stickers on bins
• Identify a clear point of contact in Finance
• Develop regular update process to verify all systems have same patient charge items flagged, minimize manual verification, investigate common data field for each system, and send summary to supplier for verification
• Identify in product catalog which items are chargeable
• Communicate to floor staff new chargeable items added to formulary
New Systems and Fewer Defects
As a result of the project, the team was able to eliminate some of the unnecessary steps and opportunities for defects involved with the patient charge capture process. The charge card was redesigned so that the required data elements would automatically print out to a label. To minimize confusion, the team had the cards placed in the same highly visible places within every care unit. They also developed a unit report to reconcile differences between items purchased and what is being charged to patients. One unit may borrow supplies from another unit, which can throw off the tracking system. For instance, an ICU may purchase multiple kits that don’t necessarily make sense for the entire floor to stock, so people tend to borrow the items when needed. As the hospital was looking for technology to automate the charge capture process, it was important to ensure that vendors had a mechanism for charging borrowed supplies.
The project team succeeded in implementing key changes and achieving statistically significant results. Within the seven pilot units, they moved from 35.7 percent capture of patient charges to 87.5 percent captured. For the 12 products on the 7 pilot units, the hospital was able to capture $197,000 more in gross charges than it would have at the January charge capture rates. On an annualized basis, this is estimated to be $600,000 for 7 pilot units and 12 items, or for all 34 inpatient units, the annualized gross revenue is estimated at $3 million. Assuming net revenue at 10 percent of gross, net revenue on $3 million is $300,000.
By capturing the right information by patients in the database, the hospital is able to increase accuracy as to what is spent on each DRG (diagnosis-related group) and better reflect the actual cost of caring for patients.
Ensuring Accuracy in Managed Care Operating Room Carve-Outs at Virtua Health
One of the early Six Sigma initiatives at Virtua Health targeted revenue generation by improving the process to identify, charge, and bill carve-out items for managed care and Medicare. Leveraging opportunities uncovered through these initial efforts led to scoping a project in 2005 to focus on managed care operating room (OR) carve-outs at Virtua’s Marlton and Memorial campuses.
Within managed care contracts, “carve-out” arrangements have become common practice for particular conditions or types of services. Payers and health plans use carve-outs to separate specific items from the overall plan’s risk pool. Potential revenue can be gained from managed care carve-outs if the costs can be tracked and charged accurately.
“For a variety of reasons, we had been struggling for some time to accurately capture costs for implantable devices,” says Adrienne Elberfeld, Master Black Belt on the project. “When we originally looked at the data in 2001, we found we weren’t capturing charges to the tune of about $7 million. We had made improvements through our first project, but learned some lessons as well. We actually built a process that was dependent on one person generating reports, and without that person the process fell apart. Many things were happening at once that impacted our ability to control the project results—including changes in process owners and leadership, and the introduction of new OR systems. We decided a follow-up effort would be required.”
Despite all the work they had done initially, something had slipped. By carefully scoping a new project, they were able to take a fresh look at the issue and uncover opportunities to review internal processes to make sure paperwork got through and charges were appropriately captured.
The goal for this project would be to increase revenue by ensuring all managed care OR carve-outs are correctly billed and documented to meet compliance standards. The “Y” to be measured was identified as the number of managed care OR carve-outs that were accurately billed, and the sub-Y defect would be any managed care OR carve-out not posted within five days of the procedure or discharge. Both factors would be measured through the “Managed Care OR Carve-Out Report,” and data sources would include 100 manual chart reviews from each hospital. To analyze measurement system accuracy, a gage R&R was completed and found 96 percent agreement among the sources of information.
Education frequently is a key component in Six Sigma projects to make sure that employees understand and embrace any process changes or workflow adjustments that are introduced through the initiative. At Virtua, focused educational sessions were conducted in November 2005 to help OR staff understand the importance of proper implant documentation. Monitoring the frequency, descriptions, and volumes of “like” items would help to determine the need for an action plan to help control costs by reducing the amount of supplies being ordered unnecessarily.
During the Improve Phase, a review of the Employer Sponsored Insurance (ESI) category/revenue codes from the100 chart reviews revealed opportunities for improvement. The probability of a defect was measured at both campuses: 30.9% at the Marlton campus and 19.3% at the Memorial campus. The root cause analysis shown in Table 10.2 illustrates the team’s effort to identify the underlying drivers for the defects and propose solutions. The revenue code defects are shown in Figure 10.8.
Table 10.2. Root Cause Analysis
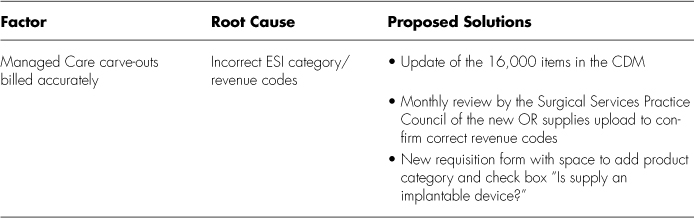
Figure 10.8. Revenue code defects
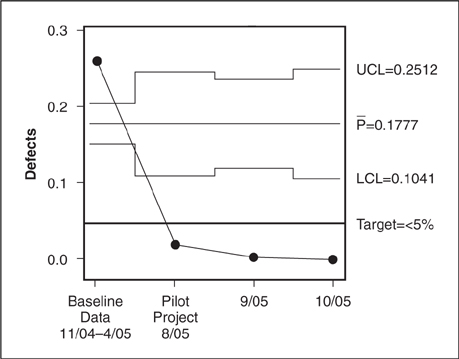
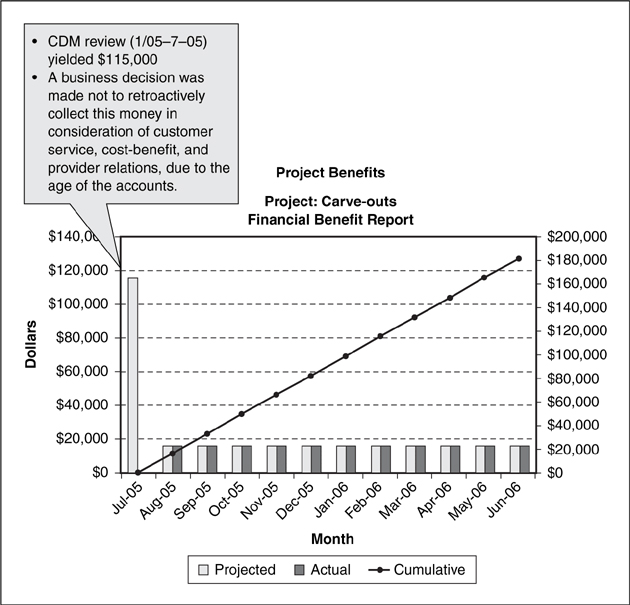
At the outset of the project, the Z score was measured at 2.14, with a 26 percent probability of a defect. After the project entered the Control phase, the Z score was measured at 3.60 with a 1.8 percent probability of a defect. Initial measurements indicated the accuracy of managed care OR carve-outs at Marlton was 69.1 percent and at Memorial it was 80.7 percent. In August, results from the pilot project demonstrated a 98.2 percent accuracy. The team noted one change in September and 0 changes in October. Statistical analysis indicated that September results were 99.7 percent accurate, while results for the month of October were 100 percent accurate. The Chi-Square analysis in Figure 10.9 shows the significance of the pilot project results.
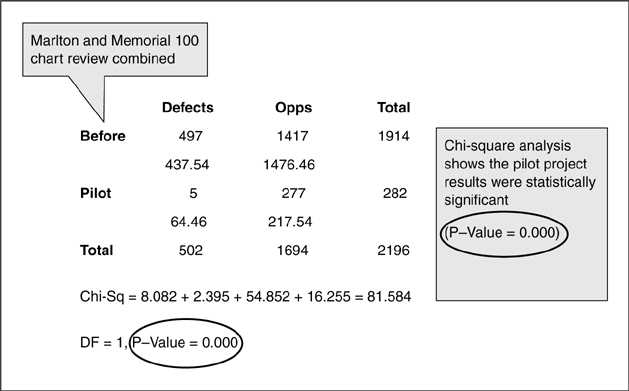
Figure 10.9. Chi-square analysis MHBC and Marlton—Combined versus pilot project
The projected financial benefit from this initiative was estimated at $196,000, with $115,000 from the CDM review (1/05-7/05) and $82,000 (8/05-6/06) if the changes were not made to the CDM and the activity remained unchanged. The surgical services council now reviews all information on a monthly basis. They also were able to benefit from a multidisciplinary approach. By educating clinicians and finance staff, and making everyone aware of the issue, they instituted a workable review process to make sure charges are consistently captured in the system. The financial benefits are demonstrated in Figure 10.10.
Figure 10.10. Project financial benefits
Data results confirmed that the improvements had achieved the goal defined in the DMAIC team charter. The team selected ongoing measures to monitor performance of the process and ensure continued effectiveness of the solution, and determined that key charts or graphs would be used within a “process dashboard.” With changes implemented, the team created a plan to sustain the process. This would include having the hospital’s Surgical Services Practice Council conduct a monthly review of the new OR supplies uploaded the previous month to confirm accuracy of the revenue codes. The plan also called for product coordinators to use the new requisition form that had been developed.
To facilitate better communication and staff education, part of the Control plan involved establishing clear roles, policies, and standard operating procedures. The team carefully documented the revised process, and then identified a process owner to assume responsibility for maintaining results and managing operations going forward. They also developed charts detailing requirements, measures, and responses to problems in the process, and updated the project binder documenting the work that had been done and the key findings.
Other issues or opportunities that couldn’t be addressed adequately during the course of the project were shared with senior management. The team took time to recognize and celebrate their achievements, which is a key aspect that helps build enthusiasm for improvement initiatives. The carve-outs project had measurably improved service quality, decreased expense, and created a more accurate process for revenue collection.
Carve-Out Project Team
Sponsors: J. Dower/B. Segin
Process Owners: D. McKenna/M. Paglione/P. Schultz/L. Walker
Ad-Hoc Team Members:
K. McRory
C. Sambucci
S. Fiorini
D. Flagg
C. Childress
A. Annuzzi
B. Cain
L. Ackley
M. Schultz
N. Rivera
K. Pape
C. Bosco
R. Altmark
J. Kurz
M. Paglione
Finance Approvers: R. Rueblinger/W. Christie
Green Belts: H. McNally/A. Kitz
Black Belt: K. Goodman
Master Black Belt: A. Elberfeld
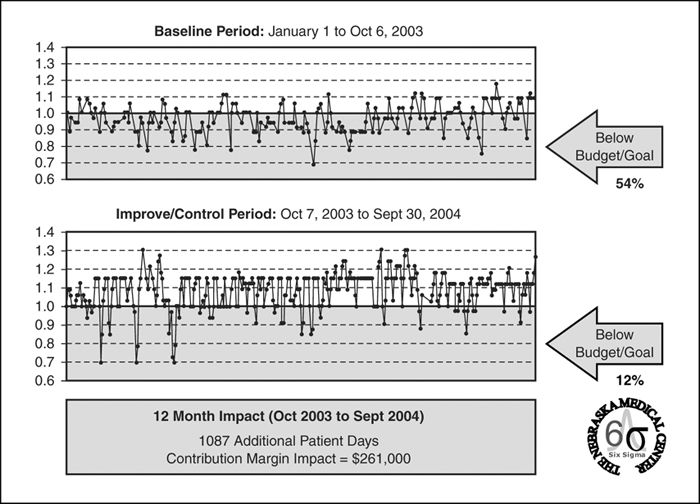
Addressing Bed Management at The Nebraska Medical Center
In many hospitals, a certain number of inpatient beds are unavailable each day due to staffing-related issues. This restricts access to care and can result in lower patient, staff, and physician satisfaction; reduced physician referrals; quality issues; and lost revenue or market share. At The Nebraska Medical Center, an effort to deal with bed restrictions became one of three individual projects derived from a larger scoping effort initially described as “bed availability.”
In December 2002, the hospital began its first round of training and initial wave of Six Sigma projects. Following discussions with senior leadership, three Black Belts were asked to focus on the general topic of bed availability. The hospital considered this to be an important issue given the impact on patients who might have to wait for a long time in the ED or who may be referred to other facilities for admission. By targeting issues related to staffing utilization and bed restrictions, the hospital hoped to identify ways that nursing staff could be better deployed to increase the capacity to care for more patients.
As the project began, team members included managers from a rehab unit, the patient placement unit, a medical surgical floor, an intensive care unit, a telemetry floor, a nursing director, and a nursing resource coordinator. This level of participation illustrates how broad the initiative was even after initial scoping. The team began by analyzing the daily reports that indicate whether or not a bed is available. By following the Six Sigma process, their goal was to find solutions that would help them to reduce the number of unavailable beds and thereby improve their ability to admit and care for patients. As they entered the measure phase of the project, 75 to 80 percent of beds in the hospital were still in scope.
“In addition to helping the hospital resolve a key issue impacting access to care, this project served as a great learning opportunity for the team,” says Jason Lebsack, Manager of Six Sigma at The Nebraska Medical Center, who in 2003 served as the Black Belt on this project. “It wasn’t simply a matter of identifying a problem with bed availability and deciding to launch a project to fix it, given the complexity and amount of scoping required. We all learned to be more focused in our efforts and to set clear, measurable parameters.”
As it turns out, bed availability was not a single project in itself, but rather a focal point from which separate projects could be scoped and executed. They were starting from scratch, given that data was either hard to come by or at least widely dispersed throughout the organization.
To set reasonable boundaries, the team made some decisions on the areas that would be in scope and out of scope for this particular project:
• In scope
• Medical/Surgical, Telemetry, intensive care units
• All unit staffing practices
• Use of nurse/patient ratio
• Use of current acuity rating approach
• Sick call, holiday, vacation approach
• Out of Scope
• Burn, LSCU (Liver Special Care Unit), OB, pediatrics, PICU, NICU, LTCC (Lied Transplant Cooperative Care) and TRU units (Transitional Rehabilitation Unit)
• Redefining medical necessity
• Nursing shortage
• Non-staffing bed restrictions
• Process for determining patient acuity
• Student nurses
Obtaining the “voice of the customer” (VOC) helped to ensure alignment with the organization’s strategic plan and validate connections with two key objectives, which are two of The Nebraska Medical Center’s five Priorities for Excellence:
• Most attractive employer. Internally, there were concerns that issues surrounding lack of bed availability could make it difficult to recruit and retain staff, and to adequately manage the patient load taking safety and acuity into account. Referring physicians had become dissatisfied with the capacity issues.
• Highest quality of customer service and care. Feedback from patient surveys indicated concern over waiting too long for a bed, or being turned away to other hospitals for care. Being able to address bed restrictions would positively affect the hospital’s ability to provide high-quality patient care in a timely manner.
At the outset of the project, there were some hard feelings between staff on the various floors making requests for beds and others who were taking the calls. “Decentralized patient assignment requires a lot of cooperation and teamwork,” says Lebsack. “Interactions over the phone were sometimes tense because they were based on a sense of urgency.”
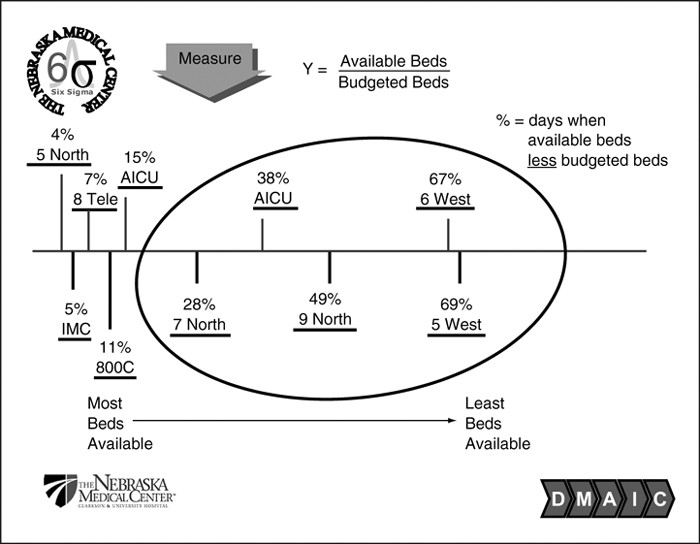
The goal or “Y” for the project would be that at 3PM each day, each unit should have at least as many available beds as budgeted beds. By measuring current performance they found they were starting with a 29 percent defect rate.
Simply arriving at the basic formula of available beds divided by budgeted beds required a tremendous amount of effort and discussion. There had previously been no set target for nurse managers as to the number of beds they needed to have open. Figure 10.11 shows the available beds in the areas that were within scope, and points to the variability between different floors.
Figure 10.11. Available beds divided by budgeted beds
Analyzing this information was another key aspect of the scoping process. Of the 10 units evaluated, data revealed that at least 5 did not present availability issues. They narrowed their focus to staffing issues within the five units that had the highest percentage of unavailable beds.
Further scoping led to a concentration on 6 West with a 67 percent rate of defects. They decided to exclude 5 West from the study at the time, even though the rate was slightly higher, because their issues with vacancy rates would be addressed by recent new hires.
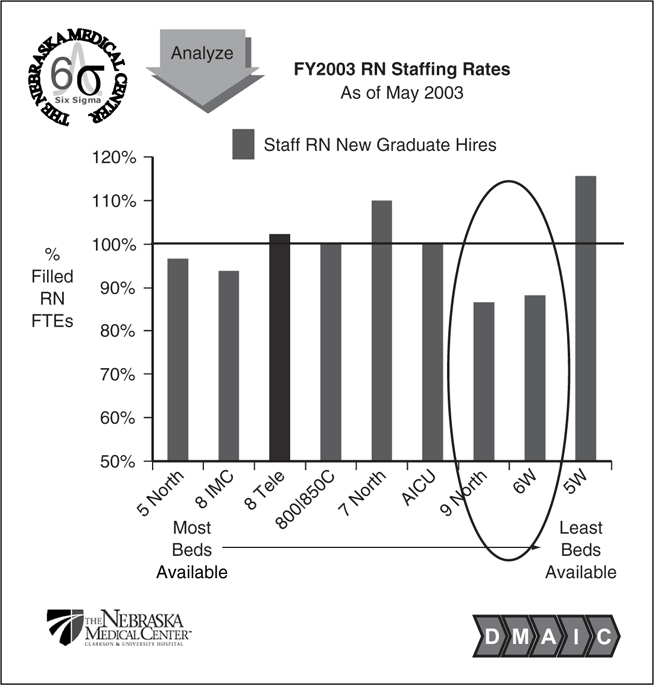
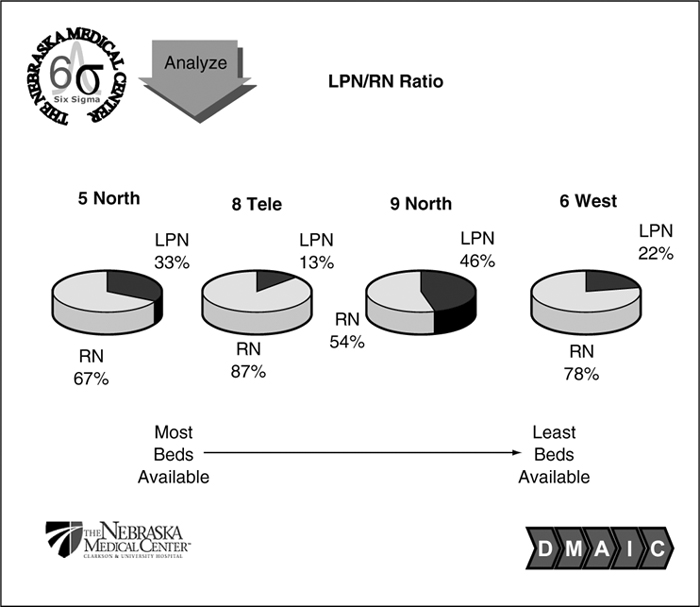
The team then began to prioritize the underlying factors, narrowing down to people-related (see Figure 10.12) and “other” (see Figure 10.13). This didn’t necessarily reveal a trend, other than the obvious with regard to staffing rates, as indicated in Figures 10.12 and 10.13.
Figure 10.12. RN staffing rates
Figure 10.13. LPN/RN ratio
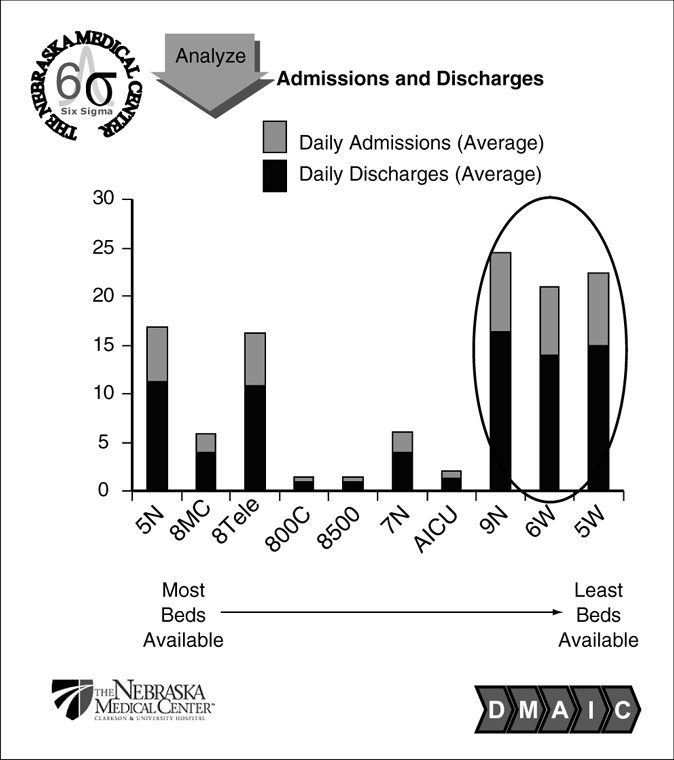
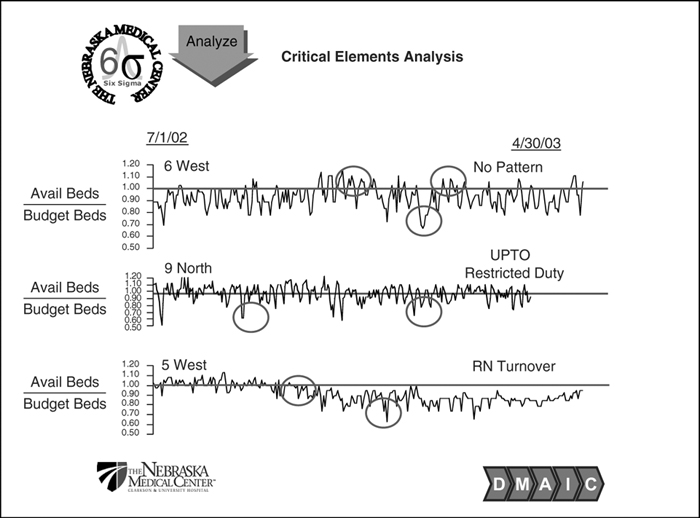
It was initially assumed that the more established units would be able to take more patients, but in fact the opposite relationship was identified. As shown in Figures 10.14 and 10.15, they analyzed data on daily admissions and discharges, staffing ratios, and critical elements such as specific time periods to see if they could statistically confirm the most important factors.
Figure 10.14. Admissions and discharges
Figure 10.15. Critical elements analysis
During the critical elements analysis phase of this project, the application of Lean Thinking provided critical insights into factors contributing to beds unavailable due to staffing-related issues on 6 West. A detailed analysis of the RN and LPN shift structure on 6 West revealed a number of opportunities for improvement.
At the time of the project, nursing schedules on 6 West included various combinations of 4-, 8-, and 12-hour shifts. Having so many different shifts built in numerous handoffs of patient care throughout the day (non-value-added time from the patient’s perspective) and created an almost daily nursing gap in the number of nurses working to provide care in the late afternoon.
In fact, 6 West chronically had vacancies in the 3 PM-to-11 AM shift and frequently had to scramble to find additional nurses to work during this time. This scramble placed a significant amount of stress on Lead RNs each day.
Developing Solutions
In all, the project team identified three major improvement strategies for 6 West as well as four main improvements to improve the overall utilization of nursing staff:
• 6 West Improvements
• Improved floor aesthetics and computer upgrades (installed in hallways close to patients)
• Creation of an Admission and Discharge RN role
• Simplified RN shift structure
• Overall Improvements
• Nursing staff floatation
• Bed Status report simplification
• Lead and Charge RN/Patient Placement Unit RN job shadowing program (“Trading Places”)
• Lead and Charge RN response timeliness to Patient Placement Unit pages
During the course of the project, the team identified other possible changes that could be addressed later, and placed them on the project “parking lot.” The issue of nurse staff flotation eventually became one of several Work-Out sessions. Through another separate Work-Out, the team developed revisions to the bed report to increase usability, streamline content, and provide clearer definitions.
Sometimes necessity really is the mother of invention. When one of the nurses had to be on restrictive duty for medical reasons, the team decided to pilot the idea of a specialist role for admissions and discharge. The nurse would handle some of the duties in this critical area to reduce the workload for other staff, and would also back up an LPN in this role. Although this idea originated because a nurse happened to be on restrictive duty, it turned out to be such a positive change that they figured out a way to make it work long-term. According to Lebsack, several different nurses now fill this role, and they are very pleased with the arrangement.
One innovative solution coming from this project was the creation of a shadowing program where the lead staff was asked to spend a few hours at the bed desk and learn about what they do, while others went to the floors. Because of its power to create a more collegial atmosphere, this framework for trading places has since been integrated into the hospital’s orientation process. It allows staff to meet face to face and gain some appreciation for the complexity of other jobs, and has helped strengthen relationships between the two groups.
In looking at the unit aesthetics and layout, the team brought in some useful Lean concepts, particularly around the 5S method to Sort, Set in Order, Shine, Standardize, and Sustain. They helped to clean and organize the nurses’ lounge, fix monitors, install two additional computers, and revamp traffic patterns to reduce some of the back and forth travel to the nurse’s station. The changes enabled caregivers to stay closer to the patients.
The team also re-instituted a 10/10 bed assignment process with the expectation that floors would return a page within 10 minutes, then be paged again, and then if there was no answer in 10 minutes the manager would be paged. This system was devised through a Work-Out to monitor response time from page to floor to bed desk, and it continues to be monitored on a quarterly basis. The team had found that about 50- to 60 percent of the time calls weren’t being returned in a timely basis, but this has is now consistently under 25 percent and has been tracked for more than two years since the project was completed. One of the keys to making the monitoring of this Work-Out possible was the Patient Placement Unit’s transition from a paper monitoring system to a computerized database.
Project Results and Sustainability
Two years after the changes were implemented on 6 West, the hospital has continued to see positive results, while also working through remaining challenges. The admission/discharge nurse is still in place, and this change has been well received by the staff. The 12-hour only shift structure has been maintained, and 6 West has been fully staffed for more than a year, although two LPNs did leave the unit at least partially due to the 12-hour shifts. All beds, other than those with isolation restrictions, are usually available for patients. All ten private beds on the floor were converted to pediatric beds in January 2005. The lack of private rooms presented challenges with patient bed assignment, especially given isolation patients treated on the floor. Improvements in bed availability are demonstrated in Figure 10.16.
Figure 10.16. 6 West available beds (Monday-Sunday 3 PM)
Gaining VOC is important at each phase of the initiative. For this project, positive impact on the staff was evident through comments such as the following:
• “We don’t have downtime from direct patient care at 3 PM anymore.”
• “Most of staff is content with 12-hour shifts and would not go back to an 8-hour shift structure.”
• “Nurses love it that they only have to work every third weekend.”
• “Admission/Discharge RN role still working well. Exploring the need to expand hours and further specify duties.”
• “6 West is fully staffed. In fact, currently there are three RN students interested in working on 6 West but there are no open positions.”
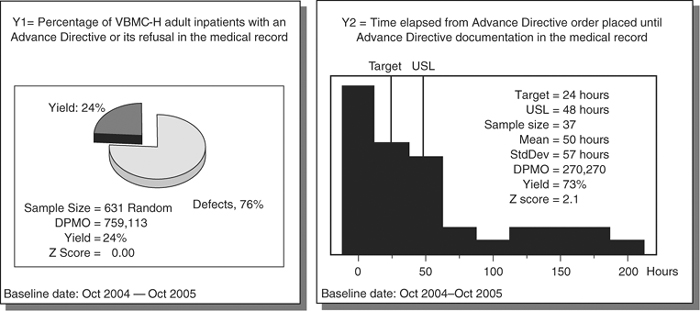
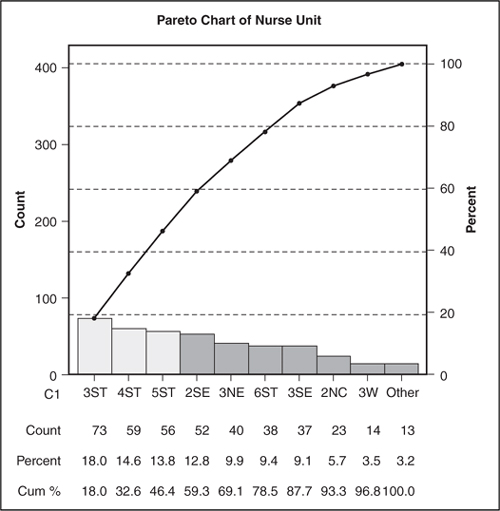
The Corporate Advance Directive at Valley Baptist Health System
One of the many successful Six Sigma projects at Valley Baptist Health System in Harlingen, Texas, targeted the existence of an advance directive. The hospital sought to institute a single, consistent and effective process to ensure that 100 percent of the adult patients at Valley Baptist Medical Center-Headquarters (VBMC-H) have an advance directive in their medical record.
For the purpose of this initiative, the groups considered in scope would be all VBMC-H adult inpatients, 18 years of age or older, and ED and direct admit patients. Surgery and outpatients would not be included in the scope of the project.
The team believed that one of the primary benefits of the project would be compliance with the JCAHO standard to address the wishes of the patient regarding end-of-life decisions. In addition, the hospital sought to enhance patient education and improve patient and caregiver satisfaction. The project aligned with the overall strategic plan in terms of integration, simplicity, and relentless service and Six Sigma quality. The team looked for input from a variety of stakeholder groups including patients and families, physicians, nurses, case managers, social workers, pastoral services, admissions, medical records, risk management, and JCAHO.
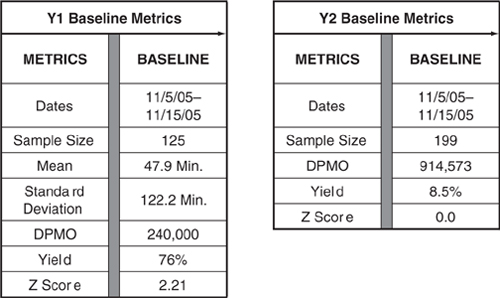
The first Y to be measured would be VBMC-H adult inpatients with an advance directive or its refusal in the medical record. The second Y would be time elapsed from the advance directive order placed until advance directive documentation is added to the medical record (see Figure 10.17).
Figure 10.17. Baseline metrics/process capability
Statistical analysis revealed that the critical Xs causing most of the variation were the nurse unit and the patient language (see Figure 10.18).
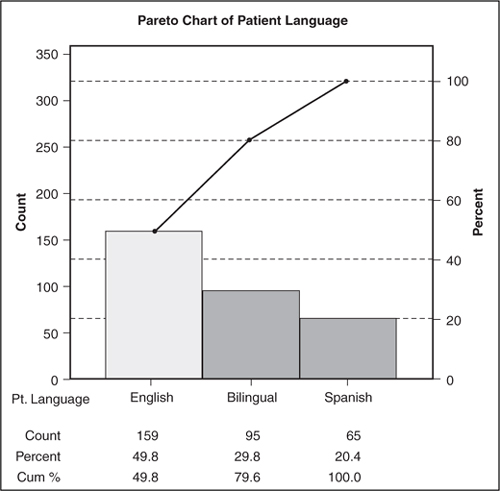
Figure 10.18. Pareto charts
The Valley Baptist Health System team implemented several improvements during the course of the project, including streamlining processes and removing rework, improving accessibility and clarity by introducing online forms, improving process control and accountability by introducing an order-based system, and simplifying interpretation by creating a combined English/Spanish form.
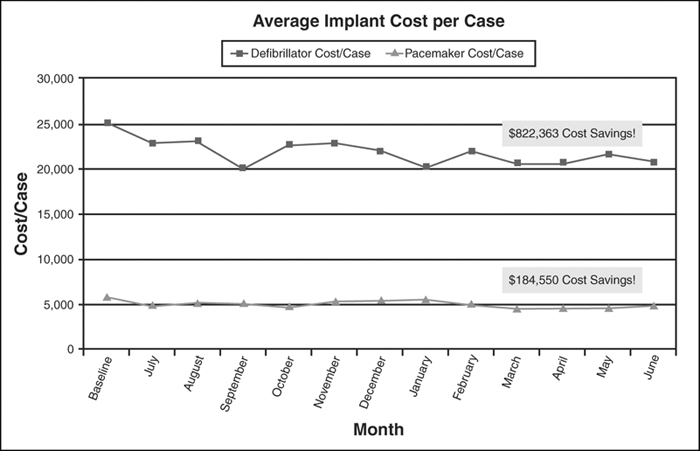
Cath Lab Utilization of Implantable Devices at Memorial Hermann Heart & Vascular Institute-Southwest Hospital
The Memorial Hermann Heart & Vascular Institute on the campus of Memorial Hermann Southwest Hospital in Houston is one of Houston’s largest heart programs, and the only freestanding heart facility in Houston. The Southwest Heart & Vascular Institute is one of three in the 16-hospital Memorial Hermann system. As part of a large training and improvement initiative, a Six Sigma team began a project to address the rising cost of implantable devices in the Cath Lab. The effort aligned with one of the organization’s key strategies to achieve and maintain operational excellence.
The team included a Black Belt, two Green Belts, a Project Sponsor, Executive Champion, and Physician Champion. They began to focus on defibrillator and pacemaker utilization as the two primary cost drivers in the Cath Lab, collecting data on the type of implant used, the implant description, physician, manufacturer, and implant cost.
Data was collected during a three-month period. Implant utilization and cost by physician, implant cost by manufacturer, and implant type (biventricular versus dual-chamber versus single-chamber) were used to benchmark against other facilities in the system. This provided useful background for the team and revealed that the average implant cost per case for both defibrillators and pacemakers exceeded the organization’s benchmark, which was set as the upper specification limit to determine process capability.
With clinician support, the team shared its findings with the cardiologists on the hospital’s Cath Lab Review Committee, which was responsible for overseeing program development. The data analysis and discussions with cardiologists led to the following conclusions:
• Significant variation in implant utilization existed among cardiologists
• Manufacturer presence during procedures heavily impacted implant selection
• Cardiologists were unaware of the cost of the device used in the case
• No specific control or attention was paid to implant pricing and utilization by the cardiologists
The cardiologists realized the need to manage the increasing implant costs and assumed responsibility for implementing a physician-owned accountability system and structure. Two sub-committees were designated: Defibrillator/Pacemaker and Stent Utilization. Both meet monthly and report back to the parent committee.
Changes identified to help positively impact implant cost per case included educating cardiologists on implant cost through use of a physician pocket card listing all devices by manufacturer in order of price. Similar devices (biventricular, dual-chamber, and single-chamber) were also grouped together. Using this tool, conversations began to change between manufacturer and physician.
As the cardiologists became more involved in implant selection, the manufacturers were required to bring in more than just “high-end” devices. With strong physician influence and leadership, manufacturers began to explore avenues to help the hospital appropriately manage implant cost.
The project began in May 2005, and results were monitored for a 12-month period starting in July 2005. The hospital saw a $1,006,913 hard dollar cost savings for fiscal year 2006. The average defibrillator implant cost per case decreased by $4,420, leading to a 54 percent reduction in defects. This surpassed the project goal of 50 percent defect reduction compared to the organization’s benchmark. In addition, average pacemaker implant cost per case decreased by $1,146, leading to a 44 percent reduction in defects (see Figure 10.19).
Figure 10.19. Implant average cost per case
According to the team, the success of this project was due in large part to physician support and having a motivated group of cardiologists involved in the process. In addition, having participation and support from the Project Sponsor and Executive Champion was key in working with physicians to remove barriers. The team’s persistence was also a factor, along with the development of a solid control plan to sustain project results.
Optimizing Respiratory Care Services at Valley Baptist Health System
In Fall 2005, the area of respiratory care services at Valley Baptist Health System became a target for a Six Sigma improvement initiative when a retrospective chart review uncovered a number of treatment and documentation errors. Feedback from staff confirmed that this was an important issue affecting patient care, and would require a focused effort to validate root causes and put sustainable solutions in place.
A Six Sigma team was assembled with the specific goal to improve the timeliness of respiratory treatments and eliminate incomplete and inaccurate documentation. The objective clearly aligned with the organization’s strategic plan in terms of ensuring excellence in service, quality, integration, and simplicity.
In scoping the project, the team determined it would include all inpatient therapeutic respiratory treatments on 2T, 3T, Pediatrics, Telemetry, MICU and SICU, but the ED and NICU patients would be considered out of scope. To gather VOC and understand how respiratory services could be improved, the team surveyed physicians, nursing staff and case managers.
The project involved the following details:
• Y1: Timeliness of subsequent treatment (measured in minutes)
• Y1 defect: Treatment administered less than 30 minutes before or after scheduled treatment time
• LSL: 30 minutes before treatment due (target: scheduled treatment time)
• USL: 30 minutes after treatment due
• Y2: Accurate and complete documentation of initial and subsequent treatments (measured as “yes” or “no”)
• Y2 defect: Documentation that is not accurate and complete
• Y2 target: 100 percent
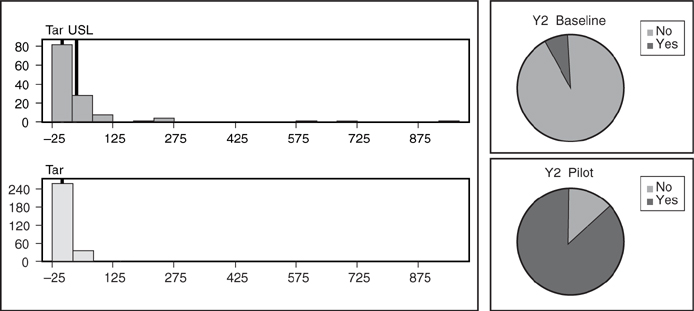
Looking at the baseline metrics and process capability for both focus areas revealed significant opportunity for improvement (see Figure 10.20). At the outset of the project, the “Y” dealing with timeliness of subsequent treatment had a Z score of 2.21, and the “Y” that focused on accurate documentation had a Z score of 0.
Figure 10.20. Baseline metrics
When the team analyzed the data to determine statistical significance, it found that for subsequent treatments, the RT (respiratory therapist) was a key factor. With respect to the second “Y”, the team did not find any significant statistical difference, accounting for variation, because the incomplete documentation was common to every unit, respiratory therapist, and shift.
During the Improve phase, several new standard operating procedures (SOPs) were developed and implemented for equipment techs, handling codes, load leveling and staff assignment criteria, unit-based RTs, charging for treatments, and order retrieval from IDX. The team also created RT notes to replace the orange stickers and charge sheets that had been previously used.
The documentation process was streamlined from five down to just two documents, including the multidisciplinary care plan, which is now completed once every 24 hours. All other documentation is done with every treatment on one single form. Other changes that were put in place as a result of the project included the development of supply par levels and the replacement of existing pagers with alpha numeric pagers to eliminate the RTs having to call back to the units.
Two pilots were conducted to test the viability and impact of the solutions that had been introduced. While documentation had significantly improved in the first pilot, treatment times had actually increased. The staff was informed of this situation, and increased surveillance of the process was implemented before the second pilot began. Stricter adherence to the new SOPs was required, and the second pilot was successful for both timely treatments and improved documentation.
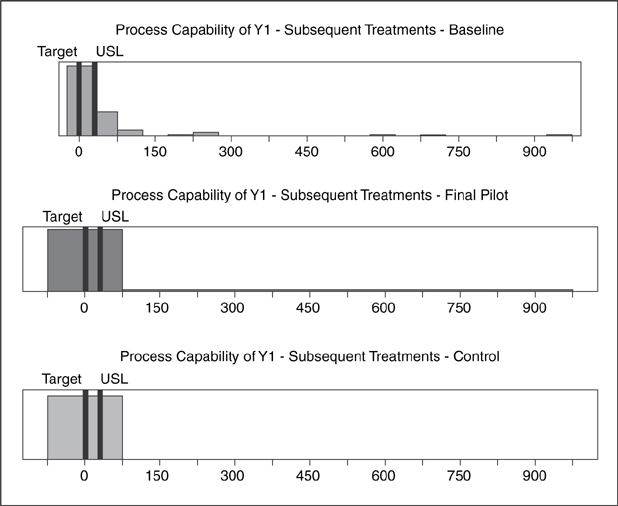
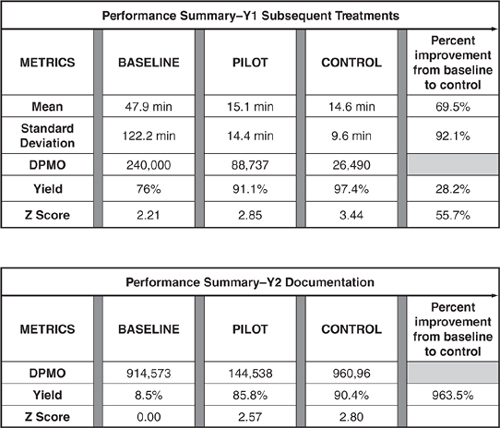
As a result of the pilot, several process changes were integrated into daily operations, including unit-based RTs, streamlined documentation by reducing the number of forms the RTs were using, and the development of supply par levels (see Figure 10.21).
Figure 10.21. Performance metrics: baseline versus pilot
The RT project proved to be both successful and sustainable, given the fact the initiative is already house-wide, and showed improvement from pilot to control, even though the Pyxis medication system was a new component of the process added after the pilot.
Maintaining results long-term will require adherence to the control plan and staff accountability. The control plan has specific alerts and processes to deal with defects when performance drops below certain levels. SOP accountability will be strictly monitored and enforced, and the control plan and control charts will be monitored by the process owner on an ongoing basis.
Reaching Six Sigma levels of excellence will be accomplished by ensuring that every step of the process adheres to the SOPs, with the clear understanding of the staff’s role and accountability. Staff will be accountable for adhering to the new SOPs, knowing there will be consequences for poor performance and rewards for excellent performance. To ensure results are maintained, the process must be constantly monitored and immediate actions taken when defects occur (see Figures 10.22 and 10.23).
Figure 10.22. Process capability before and after
Figure 10.23. Performance summary Y1 and Y2