14. Lubricating Points of Friction
“Complexity kills. It sucks the life out of developers, it makes products difficult to plan, build and test, it introduces security challenges, and it causes end-user and administrator frustration.”
—Ray Ozzie
Because of the co-dependencies inherent in crafting solutions to other problems, we have already discussed proposed fixes for universal patient identification and government regulatory efforts. One result is that our discussion of “lubricating” points of friction within healthcare has been reduced to the sole topic of optimizing medical recordkeeping and transaction processing. They are important enough to merit their own chapter. In many respects, these two tasks make up the bulk of what clinicians and their supporting organizations actually do in the course of a 24-hour day.
The good thing about friction is that it often responds to simple, inexpensive, and rapidly deployable solutions. The bad thing about friction is that it’s ubiquitous, and poor decisions can easily make it worse.
Understanding the Role of Transactions and Information in the Healthcare Industry
No matter how much technology and “progress” might suggest otherwise, every industry—including healthcare—is based on a few simple underlying principles. Its basic stock in trade is to gather information about people, process it in some way, and then use the results to prescribe and execute a management plan of some type, whether that plan happens to be a prescription, an operation, physical therapy, or counseling.
The net result is that healthcare is an industry based upon the generation and dissemination of enormous amounts of data. In 2007, there were 3.8 billion prescriptions filled, 600 million outpatient visits, and 3.5 million hospitalizations in the United States. Each of these represents multiple transactions—from the writing and filling of a prescription, to scheduling patients for outpatient visits, to the hundreds of tests, examinations, prescriptions, and visits performed in the course of a typical hospitalization.
With so many transactions, anything that slows down the process of obtaining, processing, and relaying accurate information is the source of friction in the healthcare world. It does not matter where in the process the delay occurs—delays in extracting the correct referral and insurance information from a patient can be just as disruptive as the time taken to pull a chart or losing a prescription. This is a key point, and explains in large part why it is that the newest, fanciest, and most expensive technologies do not always improve the speed and accuracy of healthcare transactions. If a computer program speeds up one part of the process (for example, data retrieval) but slows down another essential transaction (for example, having to record information by forcing a provider to type and click with a keyboard and mouse or having to navigate a cluttered and poorly designed computer screen), no net benefit is derived.
Primary Sources of Friction in Healthcare Transaction Processing
There are many different types of healthcare transactions, and therefore many potential sources of friction. However, as in many other industries, the vast majority of healthcare transactions are repetitive. This means that a relatively few simple tasks consume an inordinate amount of the time and effort required of healthcare personnel. The most important are
• Gathering information. Medical information comes from many sources: patients, families, existing medical records (either in-office or in the clinics and offices of others), in-person observations such as physical examinations, imaging centers, laboratories, and insurance and billing companies.
• Recording information. Nearly every healthcare transaction involves recording information. The results of patient histories and physical exams are recorded as baselines for later reference, for legal purposes, and as a way of justifying charges. Clinicians write prescriptions and order tests by recording their requests. Laboratories and imaging centers record their results for reference, comparison, and transmission to the providers who ordered them. Patients are asked to record data at home to bring back to the office, and billers have to record procedure information in a specific desired format for it to be acceptable to insurers.
• Storing information. Data generated and recorded internally or externally generally has to be stored in case it’s needed again.
• Retrieving information. Some, but not all, of the information recorded in the course of healthcare transactions ends up being retrieved. Some of this information is retrieved quite often. Examples include insurance information, patient identifiers, prescription information, and test results. Some of the information might never be seen again after it is recorded. Examples of these include most provider progress notes, vital signs, records of medications and treatments provided, and correspondence. Not all healthcare information is equal in importance, quality, or value over time.
• Transmitting information. Decisions made and results obtained are of little or no value unless they are passed on to others for the appropriate action.
Although the amount of time required for each of these functions might only take from a few seconds (in the case of pulling a chart close at hand) to many minutes (in the case of trying to secure copies of records held far away), the sheer number of such transactions is staggering. Every minute of effort spent in data entry, retrieval, or transmission is a minute of effort that is not spent in patient care or making better decisions.
Because friction is common, expensive, and hazardous to our health, the primary criterion for any healthcare information technology needs to be that it reduces friction rather than increases it. How can we know when this is the case? It’s simple—the market will tell us. The right health information technologies are those that providers willingly buy and implement on their own, without the need for government subsidies or penalties. Subsidies can speed the deployment of appropriate technologies, but penalties will almost guarantee that inefficient and inappropriate technologies will be deployed. Let’s look at how healthcare information technologies (HIT) can serve a positive role in our healthcare system, quickly, cheaply, and efficiently.
Rationally Applying Healthcare Information Technologies
Computers and software systems are simply tools. Their blessing and their curse is that they can be so powerful. It’s no exaggeration to say that computers have already revolutionized medicine in a host of ways. They’ve created whole new fields of medical imaging, ranging from computerized tomography and magnetic resonance imaging to PET scans and telemedicine. The computerization of medical laboratories and pharmacies has produced extraordinary increases in productivity as these functions grew from small operations to an industrial scale. The computerization of healthcare literature and the creation of the World Wide Web have made it possible for researchers, clinicians, and patients to find and disseminate information with a speed and thoroughness that were unheard of just 20 years ago. Computerization of medical information systems over the next decade will undoubtedly make it easier to share and effectively utilize clinical information.
But as we’ve seen, medical information systems that are poorly designed, implemented, and deployed can be a powerful source of disruption, frustration, clinical error, and deadweight economic loss. We can do much better than we have at computerizing healthcare information, but we’re going to have to approach it in a far more rational and constructive manner than has been the case in the past. We can make this easy, or we can make this hard. We already know how to make it hard. Making it easy is going to require discipline: The discipline to be thoughtful, patient, and most importantly, to keep things simple.
What Are We Trying to Accomplish?
The first step in creating an appropriate solution is to ask two questions: (1) what are we trying to accomplish? and (2) how much are we willing to pay for it? Our most important goal should be to minimize friction in the delivery of healthcare services. This means creating systems that will make it easier, faster, and cheaper to gather, record, store, retrieve, and transmit clinical information securely and on demand. The price that we’re willing to pay should be less than the economic benefits we obtain in the process.* If we can accomplish that, any system that we create will sell itself and save money.
* One could argue that we should be willing to pay as much or more than the current “nontechnological” cost of accomplishing these tasks if we can show an improvement in the quality of care provided, but that will still result in a net increase in the total cost of care. We’re looking for ways to reduce total costs, not increase them.
Given these goals, some design parameters are self-evident. Although it might be fast and convenient as a means of entering data, paper is bulky and difficult to store, retrieve, and transmit. Medical records have to be computerized if we are to make storage, recall, and transmission easy. A second design parameter is that the system must be easy to learn, use, and maintain—preferably as easy, or easier, than current paper-based systems. Third, whatever we implement must facilitate the secure, rapid, and painless transmission of information. A nationwide HIT system with just these three modest “tier one” capabilities would be a great help.
A “tier two” requirement is that any system we develop ought to be able to store, transmit, and display images of all types—from photographs to video to x-rays.
Finally, there is one other capability that would be extremely useful. This is the ability to record, store, retrieve, and transmit certain types of data in discrete, quantifiable form. These are specific pieces of information that are routinely referenced, compared, and transmitted on a daily basis for millions of patients nationwide. They include patient demographics, lab values, vital signs, prescription information, diagnoses, and procedures. Each of these pieces of information is routinely generated and used in terms of numbers. Diagnoses and procedures are always assigned codes (ICD and CPT codes) that allow them to be used for billing and record-keeping. Lab values are almost always numerical values that are generated automatically by machine, and immediately stored in computer databases. Prescriptions are also conveniently numeric; each drug can be identified through a universal code number and is associated with a numerical pill or bottle size, dosage, frequency of use, number to dispense, and number of refills. Vital signs are numeric. They can include not only pulse, blood pressure, temperature, and respiration rate, but also machine-generated numbers such as blood sugars and the oxygen saturation of the blood.
Combining these two sets of capabilities (the tier one “have to haves,” the ability to handle images, and the ability to capture, store, and transmit naturally quantitative information in a quantitative way) would provide 95% or more of the benefits that our society can expect to receive from any widespread healthcare information technology system, no matter how expensive and complex it might be. Although additional bells and whistles might be nice for researchers, IT professionals, historians, and vendors, they are hardly essential.
None of this requires technology that is particularly expensive to deploy, operate, and maintain. More importantly, all these benefits can be obtained without asking providers to change their workflow significantly, undergo long periods of training, or even use a computer when they see patients if they do not wish to do so.
Paying Attention to What’s Important
The one thing that we don’t want to do is mandate one iota more of cost or functionality than we really need to get the job done. Every additional feature adds complexity, cost, and its own set of adverse side effects. Keeping our HIT efforts as simple as possible will reduce barriers to entry and utilization, therefore giving us the most bang for our bucks.
So what is the lowest common denominator for HIT? Let’s start with gathering information.
Basic National HIT Requirements: Gathering and Displaying Information
Information comes into the clinical record from many sources, including conversations, mailed, faxed and emailed correspondence, prescription lists, imaging systems, lab machines that spit out numerical values, and even (occasionally) electronic medical record systems. The lowest common denominator for collecting the data coming from any of these sources is paper. Paper is cheap and ubiquitous, and still accounts for the vast majority of medical record-keeping.
Given this reality, the first requirement of any electronic medical record (EMR) should be able to accommodate paper as a primary data input and output medium. If we simply scanned all our paper medical records and made the images available to authorized users online as PDF files, we would see a huge improvement in healthcare productivity. As low-tech and unsophisticated as this seems, it would allow us to start saving time and money tomorrow.
Still higher productivity could be achieved by making this scanned data searchable. After paper-based medical records (in the form of provider notes, correspondence, test results, and so on) are scanned, they can easily be classified by date, patient, and record type, and placed into a searchable computerized database. (Much of the classification process can be automated.) With this small enhancement, a specific piece of any patient’s medical record could be located immediately. From there, a couple of keystrokes could fax or electronically transmit the data to wherever it’s needed. Inexpensive systems with these capabilities already exist, and are commonplace in industries such as law, banking, mortgage, trucking, and public schools.
How would such a system fit into the next step in the healthcare process—recording information?
Basic National HIT Requirements: Recording Information
If we’re interested in efficiency, providers need to be able to enter data using whatever medium is most effective and convenient for them, including pen and paper, dictation, computer mouse devices, and keyboards, digital cameras, or anything else. A nationwide system that accommodates paper-based input and output allows for this, but is the continued use of pen and paper medically acceptable? After all, poor handwriting has been implicated in a large number of studies and news reports as contributing to medical errors, a loss of productivity, and even deaths.1,2,3 At least one patient safety organization has called for a complete ban on handwritten prescriptions.4
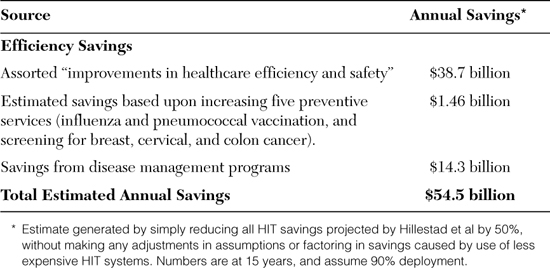
As is often the case in healthcare, the reality is never as simple as the rhetoric. Although there is no question that errors and ambiguity can and do occur with the use of handwriting, there is a good chance that typing, clicking, and computer order entry are not much better. In one of the largest studies of its kind, in 2003 U.S. Pharmacopeia reviewed more than 235,000 error reports submitted by 570 healthcare facilities.5 The results are shown in Figure 14.1.
From: U.S. Pharmacopeia. “MEDMARX 5th Anniversary Data Report—A Chartbook of 2003 Findings and Trends 1999-2003,” Figure 11.
Figure 14.1. Causes of Medication Errors, Study Year 2003 Compared with 5-Year Data
As we can see, handwriting accounted for about 2.9% of errors in 2003 and was the 15th leading cause of medication errors. Entering data into computer systems was the 4th leading cause and accounted for 13% of errors. Many of these computer data entry errors were due to mistakes made while transcribing orders from paper into computer software. Presumably what’s really needed to reduce errors is to switch completely over to computerized physician order entry (CPOE) systems. If we eliminate the paper and handwriting, surely we’ll eliminate the errors?
To test this supposition, the USP study compared the error rates of facilities utilizing CPOE prescribing systems with those that did not utilize CPOE. As shown in Table 14.1, the error rates were almost identical between the two different types of institutions on both an absolute basis and per 100,000 doses prescribed. Although it might appear that there were fewer harmful errors made with CPOE, the difference is not statistically significant.
Table 14.1. Comparison of Reported Medication Errors Between CPOE Facilities and Non-CPOE Facilities
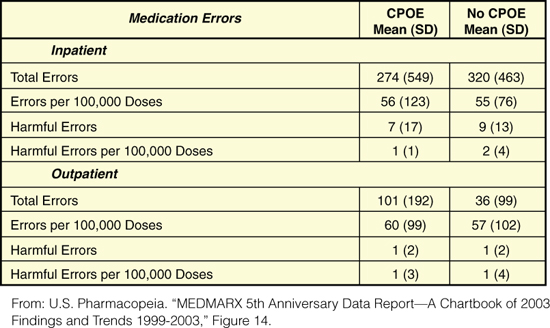
Another study done in 2009—a meta-analysis of 12 studies looking at prescription errors occurring with and without CPOE in pediatric patients or patients in intensive care units—supports these findings. It found that even though there were fewer reported medication errors when CPOE was used, the use of CPOE produced no significant reduction in adverse drug events or mortality rates.6
Ironically, although there are many strategies that could be used to reduce the number of errors associated with the use of pen and paper prescriptions, few ever seem to be implemented.† Instead, the emphasis has been on switching over entirely to more expensive and complex technology-heavy CPOE systems that carry high price tags and introduce their own unique sets of errors and inefficiencies.
† One could, for example, simply ask that the relatively few characters required when writing a prescription be printed rather than written in cursive. Another strategy is to implement relatively inexpensive handwriting/computer software hybrid systems that allow providers to enter data by hand as usual. Their writing is then immediately interpreted by computer (skipping potential human errors in the transcription process) and immediately displayed to the provider, who would verify that the computer got it right. These systems can provide all of the benefits of CPOE with correspondingly fewer errors due to clumsy and complex user interfaces.
A similar situation seems to apply when looking at handwritten chart notes. Although it’s obvious that many providers have poor penmanship, there has never been a single published study that looks at whether asking providers to type or point-and-click to create their medical records has any beneficial impact on patient care. Instead, there are many reasons to believe that these systems might be less accurate and informative than the paper records they’re replacing.7 If we can’t trust providers to write correctly, can we really trust them to type or use pick-lists properly?‡ Just because information is neatly typed instead of scrawled doesn’t mean that it’s more correct or more valuable.
‡ Two famous quotes by computer technology experts articulate the problem quite well. The first is from Paul Ehrlich: “To err is human, but to really foul things up you need a computer.” The second is from Mitch Radcliffe: “A computer lets you make more mistakes faster than any invention in human history—with the possible exceptions of handguns and tequila.”
The bottom line is that we’re right back to where we began with respect to recording data at the point of care. We should be implementing HIT systems that frankly don’t care where or how data is entered—whether by pen and paper, dictation, Palm Pilot, or computer mouse and keyboard. The decision of which medium to use should be left up to healthcare providers based upon their own practice, their own finances, and what works best for them. In the meantime, both government and private industry should develop strategies and technologies that make all forms of healthcare data entry faster, safer, and more reliable.
Basic National HIT Requirements: Storing, Retrieving, and Transmitting Information
Storing, retrieving, and transmitting information is where computers really demonstrate unequivocal value, and the reason that we desperately need a basic, nationwide healthcare information technology infrastructure. Computers can handle images, documents, text, sound, and video equally well; a big advantage in a diverse and complex medical environment. Given the unparalleled supremacy of computing for these functions, what type of functional infrastructure makes the most sense?
Here as elsewhere, there is no one-size-fits-all solution. Large and technologically sophisticated medical centers and health systems such as Kaiser, the Mayo Clinic, and the Veterans Administration will have their own business reasons for deploying expensive, complex integrated systems. Because they own their own labs, pharmacies, providers, and facilities, they have powerful business reasons to force everyone to use the same systems and the same centralized and wholly owned data centers. As large institutions, they are in a position to bear the high cost of training and maintenance.
Smaller providers are in a completely different position. Already strapped with expenses, staff shortages, and administrative overhead, they are in a poor position to take on the additional expense of buying and maintaining computer and software systems that require constant attention, upgrades, and maintenance. Moreover, the systems that they do buy are unlikely to be the same as systems owned by other providers and healthcare facilities in the community. The integration of proprietary medical software systems is one of the most difficult and expensive challenges in HIT today. For them, it makes far more sense to outsource their HIT needs to Internet and web-enabled applications service providers (ASPs). By leasing the software and storage as a service (in fact, much like a utility), these clinics can concentrate on providing care instead of supporting IT departments.
With all the different pieces of proprietary software in use nationwide, what’s needed most is for all HIT systems be able to seamlessly communicate on the most basic level—that of at least being able to transmit, receive, and handle PDF-based healthcare data without the need for any special software integration whatever. In this respect, each piece of medical record software should behave something like a fax machine. When one piece of software requests another distant system, something like a “handshake” should occur in which the systems describe each other’s capabilities. If they are integrated to the extent that they are custom-integrated and can share formatted quantitative data such as text-based notes, lab results, vital signs, prescriptions, and so on, information is transferred as discrete, formatted computer-readable data. If, on the other hand, the two systems are either not integrated or one system only reads and writes to image-based documents, the clinical information is written to a common format such as PDF, and sent as a set of labeled documents to the receiving healthcare facility.
What has largely prevented the implementation of such a simple solution to sharing records is the attitude of HIT advocates and the HIT industry that such a simple, inexpensive, and rudimentary solution is somehow insufficiently “technologically advanced,” “state-of-the-art,” and “clinically sophisticated.” It is as if solving the problem of medical data transparency and portability must somehow be solved perfectly and in favor of high-tech, or it should not be solved at all.
The irony is that if had we chosen to support and deploy this basic healthcare data storage and transfer technologies 10 or 15 years ago, every practice in America would already be connected. Technology adequate to the task existed then, as it does now. Even these basic capabilities would have saved thousands of lives and billions of dollars in the interim—from results that were available faster and more completely, tests that did not need to be repeated because their results were available, and emergency services that could have been delivered after referencing the history, physical, allergy, medication, and lab information that resides even in the most basic paper health record. With every provider connected and functioning at a higher level of clinical efficiency, we would now be talking about incremental increases in capability rather than wallowing in the mire of trying to get more than 10% of providers to use an expensive “certified” system.
To quote Voltaire: “the perfect is the enemy of the good.”8
Basic National HIT Requirements: Dealing with Quantitative Data
Simply being able to exchange images of medical data in the form of PDFs and image files meets our tier one basic criteria, but does not address our tier two desire to capture and maintain inherently quantitative information as discrete digital data. A great deal of this information is currently recorded in handwritten form—as vital signs, lab results, medication lists, allergies, patient demographics, and prescription information. Turning these values into discrete data (or keeping them as discrete values when imported from other medical information systems) would greatly expand the degree to which automation could be used to enhance healthcare services. Indeed, combining tier one and tier two data would give us the potential to have at least 95% of the functionality of the most expensive and sophisticated electronic health records (EHRs) in existence. How can we provide this capability quickly and cheaply?
There are at least three ways to make this happen. All of them use relatively inexpensive computer technologies that have already been proven in medical practice.
Tablet computers use a pen-type stylus to record information on-screen using a number of different tools, including handwriting recognition, radio buttons, check boxes, and even built-in cameras for capturing images. They are extremely useful for entering relatively small amounts of discrete data, and many manufacturers are now specifically building them with clinical use in mind. There are many obvious advantages of using a tablet configuration with pen-based input rather than typing, including greater portability, the ability to interact with patients rather than type, and the ability to take advantage of computing power to convert handwriting to text in real time as the data is being entered. Although heavier and far more expensive than paper in most situations, one can easily see how using a tablet for quantitative data such as prescriptions, vital signs, checklists, and emergency room and home health care examinations would be an excellent alternative to both paper and conventional EHRs.
Tablets are already in everyday use in a wide variety of clinical applications. These include home-based eye exams, pharmaceutical trials, CPOE, oncology, sports medicine, nursing home care, and many more.
Digital pens use a special pattern of dots printed on a page of paper to “read” and record pen strokes with respect to size, shape, and location. Once the position and shape of these strokes is interpreted by computer, they can be converted into machine-readable text, interpreted as check marks and saved as image data depending upon the type of data they represent and the desired application. Digital pen technology allows providers to use paper for virtually any data capture purpose; it has already been tested successfully in a number of different clinical applications. Implementations include the creation of medical records on cruise ships, traumatic brain injury screening for the Department of Defense, data collection in pharmaceutical studies and other clinical trials, long-term care, and the recording of vital signs in acute care facilities.
A recent public health drill tested this technology as a very quick way to enter clinic registration data in the event of flu pandemic. It was extremely successful, allowing for vaccination rates of up to 350 patients per hour. This rate would have been difficult or impossible to achieve in a timely fashion, and at a reasonable cost, with ordinary paper records or conventional EHRs.9 Even in situations where digital pen implementation has been troubled with programming errors, defective printers, and substantial system downtime, user satisfaction is high and the technology was found to be very workflow-friendly.10
Paper scanning with handwriting recognition is a third, inexpensive, and very reliable technology for capturing handwritten data in digital form. It has the added advantages of being able to scan any type of document into a digital record and not requiring the use of a special pen. High-quality scanners are now inexpensive and able to scan both sides of a page simultaneously. Multifunctional peripheral devices (MFPs) produced by companies such as Canon and Xerox give clinics the ability to scan, print, fax, and copy in a single high-speed digital machine. Properly designed, scanning-based clinical software can essentially duplicate the capabilities of digital pen-based applications, handle all types of medical paperwork, and yet minimize the need for specialized hardware.
The author has personal experience with one such system that was developed specifically for the purpose of improving the speed and efficiency of data capture and office workflow. Tested and found to be extremely effective in clinical practice, the system allowed providers and their staff to enter vital signs, lab results, prescriptions, and billing information on paper forms specifically customized for each individual patient, provider, visit, and clinic for which they are being used. These individually identifiable pages can be mixed up or even scanned upside down without affecting the results.
Quantitative data is automatically converted to digital form and verified, while other information such as progress notes and correspondence is saved in image form. All the information is uploaded to a simple searchable electronic medical record. Once the data is safely stored, a password-protected website specifically customized for each patient is automatically created and populated with listings of the patient’s providers, medical conditions, procedures, medications and links to medical consent forms and educational materials on each one. All this—along with processing the data needed for medical billing—happens within minutes of scanning.
Simple but effective systems like this provide the vast majority of benefit that anyone would want from an electronic health record. This includes instant 24-hour accessibility, the ability to search for specific quantitative data, and the ability to add considerable numbers of quality and safety features. Perhaps the most extraordinary thing about this system is its cost. At less than $200 per provider per month, it would take 20 years of use before equaling the per-provider purchase price of a “conventional” EHR.
Basic National HIT Requirements: Sharing Information
With widespread provider deployment of a basic computer-accessible medical record, the final step is to share this clinical information quickly, safely, and securely.
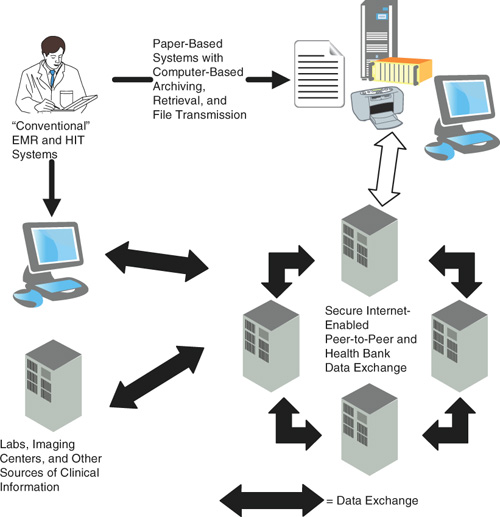
There is certainly no shortage of proposals with respect to how medical records might be distributed. The most commonly cited suggestions include community health information networks (CHINs), medical record “health banks,” and peer-to-peer file sharing that takes place directly from one provider’s computer to another. Recently some of the largest technology companies in the world got into the act when Google and Microsoft launched their respective medical record archives.
From the perspective of healing, it makes no difference how the information gets from Point A to Point B. However, exactly who has control over our medical records and how that data can be accessed or released makes a great deal of difference. According to public polls, Americans are extremely concerned about the privacy of their medical information and wary of the willingness or ability of the government to protect it. Sixty-two percent of adults are concerned that the existing federal health privacy rules protecting patient information will be reduced in the name of efficiency, and 68% feel that the trend toward EMRs threatens their privacy.11 An overwhelming 92% oppose allowing government agencies to see their medical records without their permission. This suggests that, at least in the eyes of voters, centralized government-sponsored medical data repositories might not be the best way of distributing medical information.§
§ In fact, medical information can be so sensitive that its large-scale aggregation by any entity could signal a broad erosion of personal privacy. An individual’s medical and demographic information contains such a large amount of personal information that it might as well be the starting point for their dossier. Medical files routinely include information about age, sex, race, occupation, address, phone, spouses and children, medications, smoking, drug, and alcohol histories, illnesses of family members, and a host of other details. Combined with financial information from the Internal Revenue Service, they can paint quite a detailed portrait of any private citizen or political opponent. Moreover, information does not always have to be leaked to exercise untoward influence. Simply the threat of release can have a chilling effect on careers and behavior. A single centralized medical record under the control of government officials would represent a profound change in the social status quo.
To the extent that we want to improve the efficiency of healthcare, we really need two distinct methods of storing and sharing medical data. The first is the point-to-point transfer of data from the records of one provider to another. Because this data is created by providers and must be maintained by them anyway, it requires no action on the part of patients to create or maintain. It is the only “mandatory” system because providers with this capability can get along just fine without “health data banks.” A second optional system would be largely under the control of patients, who could then choose to aggregate, update, and share whatever specific medical information they want in their own time and in their own way—or even choose not to have their data centralized at all. These records would be stored in health banks, via online services, on hard disks or smart cards, or in any other way that makes sense to patients and the businesses that offer these services. While nice to have, it has to be assumed that patient participation in health banks and similar efforts cannot be relied on 100% of the time. This means that we need to concentrate on an economical and efficient way to transmit medical data to and from point-to-point storehouses. In this model, health banks simply become an additional point on a diffused Internet-like medical network.
Putting It All Together
There is no doubt that the widespread computerization of medical information can increase the speed, economy, and efficiency of providing healthcare services. The important take-home message is that we can achieve these goals much faster, more efficiently and with less expense than we’ve been led to believe. The key lies in understanding that we don’t need to start with the fanciest, most expensive, and feature-laden capabilities for the vast majority of our healthcare information needs. The notion of forcing doctors to buy expensive, elaborate, centralized, and feature-laden “certified” systems as the only way to promote health is a false one, and the sooner we abandon it, the better. If the government is going to provide money to stimulate adoption of HIT, it should be awarded for purchases that meet the lowest common denominator for rapid storage recall and transmission. As shown in Figure 14.2, this consists of scanned paper documents residing in a database that can be sorted by patient, date, and provider. Higher levels of functionality are a bonus, but not nearly as important. As in so many other areas of healthcare, simplicity, ease of use, and universality are the real sources of lubrication, and the solution to what ails us.
Figure 14.2. Key Components of a Basic, Inexpensive, and Rapidly Deployable National HIT Infrastructure
Government can help in this process by helping establish and promulgate minimal, secure, healthcare file and data-sharing standards that can be rapidly adopted by vendors of even the most rudimentary HIT systems.
The Financial Impact of Realistic HIT Deployment
The best known study of the financial benefits of widespread HIT deployment in the United States was published by Hillestad et al in the September/October 2005 edition of Health Affairs.12 This analysis was part of a 2003–2005 RAND Health survey titled “Extrapolating Evidence of Health Information Technology Savings and Costs.”**,13 Based on the RAND survey data, Hillestad and colleagues concluded that:
** This study was funded by Cerner Corporation, General Electric, Hewlett-Packard, Johnson & Johnson, and Xerox. These companies all have substantial HIT business interests and happen to be potential beneficiaries of the results.
“...effective EMR implementation and networking could eventually save more than $81 billion annually—by improving health care efficiency and safety—and that HIT-enabled prevention and management of chronic disease could eventually double those savings while increasing health and other social benefits. However, this is unlikely to be realized without related changes to the healthcare system.”
To roughly $77 billion in efficiency gains, Hillestad adds additional financial benefits of $4 billion dollars from preventive services and improvements in the care of chronic diseases.††
†† Many of these economic gains may be questionable. As we’ve seen, studies have shown that at least the use of EMRs does not have a measureable impact on diabetes care.
The fact is that it’s extremely difficult to calculate the benefits of HIT with any degree of confidence. There are too many assumptions involved. For example, this study calculated that CPOE could eliminate 200,000 adverse drug events and save about $1 billion annually if installed in all hospitals. It predicts that even larger savings would accrue in outpatient practice—about 2 million adverse drug events and annual savings of $3.5 billion yearly. But as we’ve seen previously, it’s not clear that CPOE (at least as currently implemented), actually has any significant impact on medication errors or adverse drug events. Unless CPOE technology and operational effectiveness increases substantially, it is difficult to know what the true savings (if any) would actually be.
Other assumptions are equally tenuous. The analysis assumes that the information technology will cause preventive medicine interventions to reach 100% of people not currently complying with the U.S. Preventive Task Force’s recommendations regarding vaccinations and screening for preventable cancers. But as the study’s authors correctly point out, it’s impossible to imagine how those savings might be achieved without a wholesale overhaul of the healthcare machine. Other questionable assumptions include: (1) the period of time over which providers lose productivity after installing conventional EMRs (this was only three months in the analysis); (2) intentionally disregarding evidence of HIT having negative or no beneficial effect on efficiency; and (3) that HIT can potentially produce “lifestyle changes” that will prevent chronic disease.
It is possible that a basic, inexpensive, and rapidly achievable nationwide HIT infrastructure based upon simple record imaging and transmission could produce even more savings than Hillestad and his colleagues project. A simpler approach could be implemented far faster, at a lower cost, and with fewer cost and productivity losses than the vast majority of “conventional” HIT systems—even as it achieves virtually all the projected benefits. But it seems more realistic to question many of the health and productivity gains (such as those from CPOE) for which there is hope and anticipation, but little or no objective evidence.
Rather than attempting a wholesale revision of assumptions and assaulting on the evidence (or lack of it) for various aspects of HIT productivity, for our purposes it seems most rational to be grimly optimistic, but more conservative.
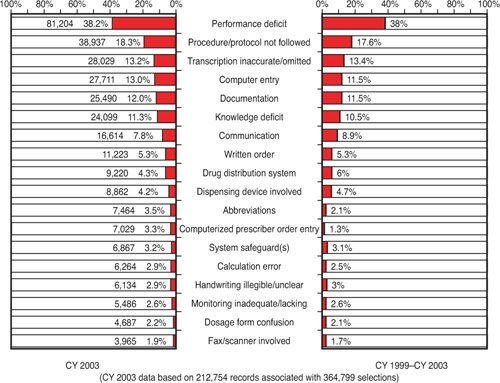
As a result of all this uncertainty, we can somewhat arbitrarily take Hillestad’s figures and uniformly reduce the projected economic benefits attributed to HIT by 50%. The results are shown in Table 14.2. While possibly high in some areas and low in others, this probably represents a more realistic overall estimate of the likely financial impact (as opposed to the potential impact) of HIT than the original report.
Table 14.2. Estimated Source of Annual Cost Savings As a Result of Widespread Implementation of a Basic System for Gathering and Sharing Healthcare Information