Content development: a continuing cGMP training program
Abstract:
As a second example of the content of training materials, this chapter discusses continuing current good manufacturing practice (cGMP) training in four sections. The first section reviews statements taken from regulations and guidances about continuing GMP training, made by the US Food and Drug Administration (FDA) and other regulatory bodies. The interpretive nature of these statements, and the role that risk assessment plays in organizational response to gaps (deviations) between the statements and ongoing behavior, are stressed. The second section addresses the topic of individuals who are qualified to deliver the continuing GMP training, presenting two approaches to qualifying trainers – a formal approach such as a GMP train-the-trainer (TTT) program and an experiential approach. While the experiential approach is cheaper than the formal approach, the formal approach has the merit of reducing variation in employee performance, as well as facilitating root cause analysis (RCA) in case of deviations. The third section reviews major sources of topics that are available for continuing cGMP training, including regulations in 21 CFR 211, written procedures required by these regulations, and topics mentioned in FDA guidances, FDA warning letters, and the organization’s own records of deviations, investigations, corrective actions and preventive actions, and quality complaints. The final section reviews a major logistical issue in the delivery of continuing cGMP training: the frequency with which this training should be scheduled. FDA recommends training more frequently than just on an annual basis.
7.1 Introduction
Every organization in regulated industry must train its employees. This training is scheduled in several ways. There is a basic scheduling distinction between training that is delivered in response to a perceived deficiency in performance or qualification, and training delivered according to the calendar. Training according to deficiency in performance or qualification includes new employee orientation (NEO), training for business process redesign and standard operating procedure (SOP) revision, and most technical training. In each case, trainees lack skill, information, or motivation that can be remedied by the training intervention.
Training according to the calendar includes much of regulatory training – the periodic refresher training that is mandated in business ethics, non-harassment policies, non-discrimination policies, a number of Occupational Safety and Health Administration (OSHA) regulations,1 and current good manufacturing practice (cGMP) regulations. As will become clear in the case of the US Food and Drug Administration (FDA) regulations, refresher training may be scheduled more frequently than on an annual basis, which is why the regulations and guidance refer to “continuing” cGMP training rather than referring to “annual cGMP refresher training.”
The decisions that are made about either kind of training are informed by an implicit or explicit business risk assessment. The level of top-down support and the scheduling of continuing cGMP training reflect a business risk assessment made by various decision makers in the organization. Moreover, decisions about the content of the training, in contrast to mandate and schedule, may also be informed by a quality risk assessment, an assessment in terms of risk to the safety, identity, strength, purity, and quality (SISPQ) of the product.2
Consider an example of business risk assessment, as it applies at the program level to continuing cGMP training. Suppose there is a deviation between the number of employees who have documented attendance at the annual cGMP refresher training session and the total number of employees who are required by procedure to attend by the end of the calendar year. In this case, the alert level is any number of employees greater than zero, excluding those on medical leave, etc. The supervisor of an employee who has failed to attend by the beginning of the December recess will be alerted by an e-mail message automatically generated by the organization’s learning management system (LMS).3
Suppose the total number of non-compliant employees is one. Will this deviation occasion a Notice of Event (NoE) investigation, and corrective action and preventive action (CAPA)? No. What about 10 employees? Probably not. What about a hundred? Perhaps. Even if it does, will the CAPA be fulfilled? There have been cases where the corrective action – simply put, getting the remaining employees trained within a month – had to be extended until the middle of February. And there was no preventive action.
Does this mean that an organization can ignore deviations in processes that have been assessed as low risk? Hardly. The business case for an organizational activity is complemented by the compliance case for that same activity. Continuing cGMP training not only periodically reminds employees of the effect of deviations, rework, etc. on the bottom line, but is a regulatory requirement as well, and reminds employees about the organization’s commitment to the regulatory requirements. This commitment carries over to all aspects of regulation.
There are several independent assessments of risk for any process or system in regulated industry, no matter how low or high the level of risk. One is the assessment made by various decision makers of the organization including employees as well as managers, another is the assessment made by regulatory investigators. Both sides are weighing the criticality and complexity of the given process in making their independent risk assessments.4 The decision makers in the organization must constantly be aware of this intricate interaction between their own business risk assessments and the quality risk assessments of the regulatory investigators, and factor the latter into their own calculation of risk.
The quality risk assessment tends to be reflected in the topics to be presented in continuing cGMP training. The topics reflect in part a quality risk assessment made by various decision makers in the organization, perhaps other decision makers than those making the business risk assessments. Those making the quality risk assessment will be addressing the risk to the SISPQ of the product, and how that topic can be presented as a training topic. The level of risk associated with a process or system that is subject to a given regulation is based on the criticality and complexity of that process.5 The risk assessment represents the level of risk as well as the acceptable melioration of that risk.
Take two possible topics for continuing cGMP training, one topic of a higher level of quality risk and another topic of a lower level of quality risk. Suppose the choice was to be made between an episode in a higher risk activity such as aseptic processing and an episode in a lower risk activity such as secondary packaging:
(a) The decision maker(s) should consider the two processes and track and trend relevant deviations, out-of-spec findings, and investigations.
(b) Also, the decision maker should consider the transferability and relevance of each process for the specific training audience. In light of these three factors: risk, transferability, and relevance, the decision maker should estimate the potential training payoff.
(c) Finally, the decision maker should prioritize the episodes in terms of the highest payoff to the organization, and the highest priority example would be highlighted in the training.
The International Conference on Harmonisation (ICH) expressed it well: “…the level of effort […] of the quality risk management process should be commensurate with the level of risk.”6 And this level of effort includes training about the topics of the quality risk management process. Both kinds of risk assessment, business and quality, must be taken into account for continuing cGMP training.
7.2 Regulations call for continuing cGMP training
FDA regulations call for continuing cGMP training. The regulations for finished pharmaceuticals are quite explicit:
Training in current good manufacturing practice shall be conducted by qualified individuals on a continuing basis and with sufficient frequency to assure that employees remain familiar with cGMP requirements applicable to them.”7
Three points in this passage should be highlighted: the training shall be “conducted by qualified individuals,” shall be conducted “on a continuing basis,” and shall address “cGMP requirements applicable to them.”
Some FDA regulations tend to be more implicit. For instance, in the section “Blood and Blood Components,” it is stated that:
All personnel shall have capabilities commensurate with their assigned functions, a thorough understanding of the procedures or control operations they perform, the necessary training or experience, and adequate information concerning the application of pertinent provisions of this part to their respective functions.8
The European Union makes a similar point about the need for continuing training in GMPs:
Besides the basic training on the theory and practice of good manufacturing practice, newly recruited personnel should receive training appropriate to the duties assigned to them. Continuing training should also be given …
Health Canada also mandates continuing cGMP training, so that “all personnel are aware of the principles of GMP that affect them, and all personnel receive initial and continuing training relevant to their job responsibilities.”9
A rationale for continuing cGMP training is provided in several guidances. For example, the Quality Systems Approach to Pharmaceutical cGMP Regulations indicates that “continued training is critical to ensure that the employees remain proficient in their operational functions and in their understanding of cGMP regulations.”10 Likewise, the ICH states, “Training should be regularly conducted by qualified individuals and should cover, at a minimum, the particular operations that the employee performs and GMP as it relates to the employee’s functions.”11
The usefulness of continuing training has been observed outside the area of GMPs. Continuing training in good clinical practices (GCPs), for example, has been recommended for clinical trials staff, as well as for Institutional Review Board (IRB) members.12
Hence the FDA regulations provide a mandate for continuing cGMP training. Of course there are interpretive issues regarding these, as any, regulations. As Michael Breggar has correctly put it, “most drug regulations are subject to interpretation.”13 Organizations in the life sciences do not simply react to a regulation; instead there is an intricate interaction between organizational actors at all levels and the various regulations and regulatory regimes, all within a given organizational setting.14 Between an observation of a gap and an organization’s response is a complex decision process. This will occur whether the gap represents a higher level of risk, such as the level of viable particulates in a monitored area, or a lower level of risk, such as one, ten, or a hundred employees failing to attend the annual cGMP refresher training. As already noted, an observation is typically escalated, triaged, and may or may not become a record of interest in the organization’s quality management system. Whether the observation will or will not become a record of interest depends upon the risk assessment. It is that record that may or may not become the basis of an investigation and RCA. Whether the record is investigated further depends upon (possibly a further) risk assessment.
Neither employees nor the organization react to the standard, the regulation – they respond to the observed gap, in terms of risk assessments. The record of the observed gap can also become part of a set of similar records that can be tracked and trended within the quality management system. If necessary, the set itself can be investigated further. Again it is not a matter of reacting to standards, SOPs, or regulations. The organization is responding to the set of excursions, the set of gaps, as reported in the set of records. The conclusion of an investigation can be followed by the development and execution of corrective actions and preventive actions. At each decision node, the decision is based on interpretations and also on risk assessments.
The interpretive aspects and risk assessments of this investigative and remediation process may be more or less explicit in various areas of the life science industry, but the underlying need for interpretation and risk assessment remains. Moreover, since interpretive aspects and risk assessments underlie any organization’s response to compliance issues, no organization is simply reactive to regulations.
7.3 Who are the qualified individuals?
FDA regulations mandate that “Training in current good manufacturing practice shall be conducted by qualified individuals.”15 Likewise, Health Canada requires that “Training is provided by qualified personnel.”16
As Joanne Cochran and Joseph Nally point out, “Since 211.25(a) requires GMP training to be given by qualified personnel, the company should have a procedure and process for qualifying trainers.”17 Such a procedure would list the necessary steps (tasks) that, taken together, are sufficient to produce the desired outcome of the process, namely the qualified trainer.18
7.3.1 Qualification of SMEs versus trainers
The qualification of trainers is a specific instance of the more general process of qualifying subject matter experts (SMEs). As such, the SOP and process for qualifying trainers will be homologous to the SOP and process for the qualification of SMEs. (The qualification of SMEs will be discussed in the next chapter.) This is not to say that SMEs can be conflated with trainers. There are substantial differences between the two, even though a master trainer can be considered an expert in the subject matter of training.
Crucial differences exist between the kind of process requiring the qualification of a SME and the kind of process (i.e., a GMP training process) requiring the qualification of a trainer. A SME must be qualified, if the following relevant procedure or process:
![]() involves high skill level, complex activity or application of advanced knowledge or logic;
involves high skill level, complex activity or application of advanced knowledge or logic;
![]() is performed in the direct manufacturing of a pharmaceutical product;
is performed in the direct manufacturing of a pharmaceutical product;
![]() involves the quality attributes (SISPQ) of the product;
involves the quality attributes (SISPQ) of the product;
![]() has serious consequences for the batch, negative impact on the patient, or injury to the operator in the case of error or deviation.
has serious consequences for the batch, negative impact on the patient, or injury to the operator in the case of error or deviation.
These criteria clearly reflect aspects of criticality and complexity that go into risk assessment. By contrast, a trainer must be qualified to present any cGMP training, regardless of complexity and criticality.
7.3.2 Approaches to trainer qualification
There are two basic approaches to qualifying cGMP trainers. One is a formal approach, such as a TTT program; the other is an experiential approach, based on management’s judgment that an employee is qualified to provide training.19
A GMP TTT program provides a formalized approach to the selection of candidates for the training, the delivery of the classroom session, the aspiring trainer’s preparation and delivery of a presentation to demonstrate proficiency, and the assessment of the aspiring trainer’s performance.
In the case of the experiential approach to the qualification of trainers, management selects the “qualified trainer” based on more or (usually) less explicit criteria and documentation. This approach to trainer qualification is less demanding than the formal approach, including less demand on resources.
The formal approach to the qualification of trainers has several advantages over the experiential approach. Importantly, it tends to homogenize the delivery of training events. This tends to reduce the variation in subsequent performance across trainees (employees).
Human error – Reason’s “active failure” – is frequently cited as the root cause of deviations in investigations.20 The deviation is frequently attributed to a training inadequacy on the part of the employee whose performance has failed, causing the deviation. This training inadequacy, in turn, is attributed to an inadequacy of the trainee, the training event, or the trainer, in some combination. However, if three conditions are met:
1. the trainer has been rigorously qualified in terms of the formal approach;
2. the qualification has been periodically monitored; and
3. tracking and trending of other deviations does not show recurrences, then the trainer and the training event can reasonably be removed from consideration in an investigation.
By contrast, it would be implausible to remove the trainer and the training event from root cause consideration if the trainer had been decreed “qualified” by management through the experiential approach.
7.3.3 Staffing considerations
It is most desirable that a qualified trainer, who is also a SME in the topic to be trained, is available to deliver the training. What if such an individual is not available, either in-house or externally? In that case, there seem to be three staffing options that will meet regulatory requirements for cGMP training to be delivered by “qualified individuals.”
One option is to have a SME become qualified as a trainer. As Saundra Williams stresses, “Subject matter experts require training in adult learning theory and training techniques before they can adequately train others.” As a second point, she notes, “Subject matter experts tend to know much more information than they need to convey. This causes them to overload the learner with information that is unrelated to job needs.” Third, she continues, “Ineffective training delivery [by SMEs] wastes dollars invested in instructors, training materials, and employee time.” Finally, she points out that, “SMEs who have not been given enough support in the delivery of technical training may cause employees to feel demoralized because they cannot apply the skills on the job.”21
A second option is to have a qualified trainer become proficient as a SME on the topic to be trained. Linda Elengold cautions, however, that, “it can take the generic trainer weeks, if not months, to get up to speed on a specific process or skill.” She concludes: “Many employers believe that it is harder to turn a professional trainer into a technically savvy trainer than it is to turn a SME into a trainer.”22
But there is a third option. Vesper points out that, “sometimes it is difficult to find good trainers who also have solid experience or knowledge in a particular technical area.”23 He goes on to say, “that is an excellent opportunity for co-teaching: an experienced instructor helping to lead the formal sections of the course and the expert serving as a resource to relate experiences and answer questions.” He concludes that “if a co-teaching approach is used, both people should be qualified as a team, and that should be provided for in your training SOP.”24 Developing a training team consisting of a qualified trainer and a SME is a most effective way to address the staffing challenge in the short term.
7.4 Applicable cGMP requirements
The FDA regulations stipulate that the training will “assure that employees remain familiar with cGMP requirements applicable to them.” What are those “applicable requirements”? Conceptualize the regulatory framework as a pyramid, with the cGMPs at the top, corporate policies making up the next tier, divisional standards as a further tier, and local SOPs as the lower tier.25 Then the applicable requirements are those that filter down from the cGMPs and are refracted in the local procedures (Figure 7.1).
Topics for continuing cGMP training include not only the regulations in 21 CFR 211, as refracted to the local level, but also any “written procedures required by these regulations, as they relate to the employee’s functions.”26 Those written procedures include the following see (Table 7.1).
Table 7.1
Written procedures required in 21 CFR 211
| Regulation | Topic |
| §211.22(d) | Responsibilities of quality control unit |
| §211.56 | Sanitation |
| §211.67(b) | Equipment cleaning and maintenance |
| §211.80(a) | Control of components, containers, and closures |
| §211.100 | Production and process controls |
| §211.101 | Charge-in of components |
| §211.110(a) | In-process sampling and testing |
| §211.113 | Control of microbiological contamination |
| §211.115(a) | Reprocessing |
| §211.122(a) | Materials examination and usage criteria |
| §211.125(f) | Labeling issuance |
| §211.130 | Packaging and labeling operations |
| §211.142 | Warehousing procedures |
| §211.160(a) | Laboratory controls |
| §211.165(c) | Testing and release for distribution |
| §211.166(a) | Stability testing |
| §211.167 | Special testing requirements |
| §211.176 | Penicillin contamination |
| §211.180(f) | Records and reports |
| §211.198(a) | Complaint files |
| §211.204 | Returned drug products |
Suggested topics for continuing cGMP training are also given in several guidances. For example, the Quality Systems Approach to Pharmaceutical cGMP Regulations indicates that “training should address the policies, processes, procedures, and written instructions related to operational activities, the product/service, the quality system, and the desired work culture (e.g., team building, communication, change, behavior).”27
Likewise, Sterile Drug Products Produced by Aseptic Processing suggests that:
… fundamental training topics should include aseptic technique, cleanroom behavior, microbiology, hygiene, gowning, patient safety hazards posed by a non-sterile drug product, and the specific written procedures covering aseptic manufacturing area operations.”28
Also, the Guideline for Quality Assurance in Blood Establishments suggests that training topics may be derived from a review of
… management observations, proficiency test results, competency evaluations, technical changes, error/accident reports, complaints, QA audits, and problems discovered at critical control points identified in each system within the establishment’s total operation.29
Another source of topics for continuing cGMP training is the set of FDA warning letters, accessible from www.fda.gov. This is an extensive compilation of GXP deviations of all sorts that can be mined for topics. There are two problems that emerge when using these resources.
First, the warning letters refer to companies other than that of the training audience, which tends to blunt the significance of non-compliance, no matter how serious. For striking examples, FDA inspected the Peanut Corporation of America (PCA) in early January 2009 and found “one environmental swab collected on 1 October 2009 from the finished product cooler floor was found positive for Salmonella. The swab location was within three feet of pallets of finished product.” Moreover:
… mold was observed growing on the ceiling and walls in the firm’s cooler used for finished product storage. In addition, water stains were observed running down from the cooling unit fans in the cooler. On 1 October 2009, pallets of finished product were stored directly beneath this unit.30
The training audience can easily say, “Yes, these are terrible conditions, but they took place in Georgia.”
The second problem is that many times the warning letters do not provide the level of detail needed to develop compelling cGMP training. This is the case even when the warning letter is augmented by newspaper accounts. Again this tends to blunt the significance of non-compliance. It is very clear that something was seriously amiss in the PCA environmental monitoring program, but it is very hard to pin that down to make training points.
Still another source of topics is the organization’s own documentation of deviations, investigations, CAPAs, and product quality complaints, as captured in the quality management system. This documentation can be reviewed on a periodic basis, say quarterly or even monthly. The selected record can be worked up and presented in a training module. These records do not suffer from either of the shortcomings noted for the FDA warning letters. The organization’s documentation refers to the training audience’s own systems, and some members of the audience may have been involved in the observation, investigation, and remediation process. Second, the very demands for compliance and documentation in the organization’s investigation and remediation SOPs should ensure an adequate level of detail to make training points.
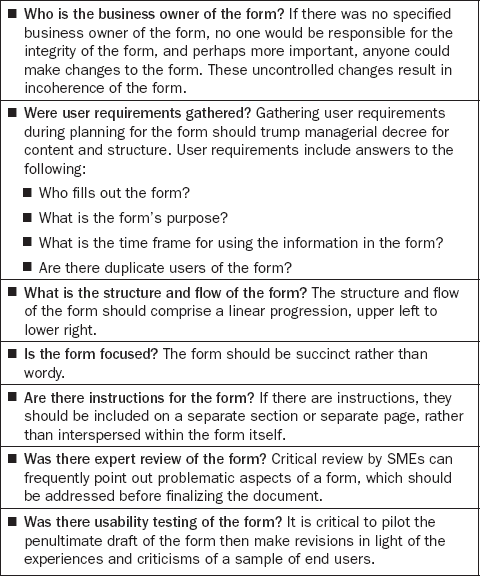
Take an illustrative example, one that might be a suitable topic for a quarterly cGMP training session. Recently, warehouse staff had trouble correctly filling out a particular form. Supervision caught the problem several times, while countersigning the document. Then supervision missed one, and it was recorded in the quality management system. Management was alerted, and requested an investigation of the problem – was it a matter of employee training, procedure, form design, or what?
During the investigation, training records were reviewed, and it was evident that each of the warehouse employees had been trained on the current version of the SOP by a qualified trainer. The SOP was reviewed. It looked straightforward on its face, and because it also covered two other forms for which no problems had been observed, it was given a clean bill of health. The form itself was reviewed, in terms of a checklist.31 (Table 7.2).
During the review of the form, it became clear that there were several serious content and formatting issues. When the form was redesigned, the warehouse staff’s trouble filling out the form ended. The problem seems to have been resolved. It is worth noting that re-training of the warehouse employees was not required, since training was not identified as the root cause of the problem, but the employees had to be trained on the rectified form.
This illustrative account could be proposed to the training council or other appropriate group and, if approved, could be worked up into a continuing cGMP training module. It would be of interest to the organization’s staff, because it refers to their warehouse, they may know the form in question, they may know some of the employees who were involved in the problem, and they will be pleased to see the satisfactory outcome of the investigation.
Perhaps the best approach to sources of topics for continuing cGMP training is a combination of local problems gleaned from records in the organization’s quality management system, with direction provided by the most serious compliance problems, as indicated by FDA warning letters32 (Table 7.3). For instance, one recurring topic from fiscal years 2005 through 2008 has been 21 CFR 211.22, “Responsibilities of Quality Control Unit.” Should the organization’s records provide any instances of such problems, the FDA warning letters might give additional weight to the training points.
Table 7.3
Most serious GMP problems in FDA warning letters, FY 2008
| Regulation | Topic |
| §211.192 | Production record review |
| §211.160 | Laboratory controls |
| §211.100 | Written procedures; deviations |
| §211.22 | Responsibilities of quality control unit |
| §211.42 | Design and construction features |
| §211.84 | Testing and approval or rejection of components, containers, and closures |
| §211.110 | Sampling and testing of in-process materials and drug products |
| §211.113 | Control of microbiological contamination |
| §211.165 | Testing and release for distribution |
| §211.188 | Batch production and control records |
A final point about applicable cGMP requirements is the relevance and effectiveness of particular cGMP training for various groups within an organization’s workforce. In Q9, Quality Risk Management, the ICH has suggested that a potential use of quality risk management principles and tools may be “to determine the appropriateness of […] ongoing training sessions based on education, experience, and working habits of staff.”33 Trainees can be grouped according to their task assignments. For example, employees who check batch records need not be given the same continuing cGMP training module as operators, even though both groups may be governed by the same broad set of procedures. Their workplace focus is much different. Likewise, ICH recommends that the appropriateness of continuing training be determined by “a periodic assessment of previous training (e.g., its effectiveness).”34
7.5 Logistics of continuing cGMP training
Having discussed the regulatory requirements for continuing cGMP training, the necessity of using qualified trainers to deliver the training, and the topics that could make up the training content, it is time to turn to the logistics of this training. The main logistical question is: How frequently should this continuing training be scheduled?
FDA regulations do not stipulate the frequency of continuing training, but recommendations are available in guidances. For example, the Current Good Manufacturing Practice for Medical Gases indicates that, “FDA recommends that cGMP training not be conducted in one massive training session. Rather, it should be presented in smaller more manageable sessions held throughout the year, or at a minimum be held once a year.”35 Speaking at an FDA workshop, compliance officer Duane Sylvia suggested that, “cGMP training should be revisited at frequent intervals and needs to be conducted by qualified individuals.” He continued, “Conducting cGMP training once a year is not recommended, but instead should be presented in smaller more manageable portions, presented throughout the year with documentation of the type, time, and attendance of each session.”36
Some regulated organizations have developed very elaborate schemes to schedule continuing cGMP training. One example will suffice. An organization required each employee to attend day-long refresher training at a specified location on the first Monday of the employee’s birth month. There was one makeup day a year for employees who missed their scheduled date. The training agenda was fixed for the entire year, regardless of intervening events. It incorporated OSHA, cGMP, business ethics, and other refresher training, as well as a “Meet the CEO” session. Given the packed agenda, less than an hour was devoted to cGMP topics. Birthday cake was provided to each attendee. Nonetheless, this scheme was simply a variant of the “one hour, once a year” cGMP training schedule.
Regarding industry practices, James Vesper has stated that “most companies conduct formal GMP training or reinforcement training at least annually; some do it twice a year; a few do it quarterly. “37 There are business considerations as well as regulatory issues here. More generally, John McConnell has indicated “How often the training course is to be conducted depends on several factors, including:
![]() total number of current employees to be trained;
total number of current employees to be trained;
![]() maximum size of training classes and method;
maximum size of training classes and method;
![]() required time to conduct training;
required time to conduct training;
![]() projected future training population.”38
projected future training population.”38
All of these factors should be taken into account in planning for continuing cGMP training.
7.6 Conclusion
This chapter addressed continuing cGMP training in four sections. The first section reviewed the statements that FDA and other regulatory bodies have made in regulations and guidances regarding continuing cGMP training. The role that interpretation and risk assessment plays in an organization’s response to gaps (deviations) between the statements and ongoing behavior was stressed. The second section considered the “qualified individuals” that deliver this continuing training, including similarities and differences between qualification of trainers and qualification of SMEs. A formal approach to qualifying trainers such as a cGMP train-the-trainer program was compared to an experiential approach such as management’s judgment that an employee is qualified to provide training. The experiential approach is cheaper than the formal approach, but the formal approach has the merit of reducing variation in employee performance, as well as facilitating RCA in case of deviations, as the next chapter will discuss in some detail.
Also, various staffing options were examined. The third section reviewed topics that are suitable for continuing cGMP training. Sources included cGMP regulations in 21 CFR 211, written procedures required by these regulations, topics mentioned in several FDA guidances, FDA warning letters, and the organization’s own records of deviations, investigations, CAPAs, and product quality complaints. The final section addressed the logistics of such training, including the frequency with which cGMP training should be delivered, concluding that FDA recommends training more frequently than just on an annual basis.
7.8 References
Adriani, W., van der Tuuk, P.A., Smit, S. The pyramid model as a structured way of quality management. Asian J. Transfus. Sci.. 2008; 2(1):6–8.
Becker, G. Warning letters report 2006. GMP News. 10(January), 2007.
Becker, G. Warning letters report 2008 – frequent deficiencies in deviation reviews. GMP News. 18(February), 2009.
Breggar, M. How to shift from reactive compliance to strategic quality management. Bioph. Intern. 22(7), 2009. [July].
Carnevale, A.P., et alTraining Partnerships: Linking Employers and Providers. Alexandria, VA: ASTD, 1990. [Report no. CE054867].
Clark, R.C. Developing Technical Training. Phoenix: Buzzards Bay Press; 1994.
Cochran, J.W., Nally, J.D., Organization and personnelNally, J.D., Willig, S.H., eds. Good Manufacturing Practices for Pharmaceuticals, 6th edn. InformaHealthcare, New York, 2006. [p. 31].
Cooper, J., Turner, P. Training institutional review board members. In Bankert E.A., Amdur R.J., eds.: Institutional Review Board: Management and Function, 2nd ed., Sudbury, MA: Jones and Bartlett Publishers, 2006.
Edelman, M., SOPs and the Technical Writer. Intercom. 2003. [April, 9].
Elengold, L. Teach SMEs to design training. Alexandria, VA: ASTD; 2001.
Enyinda, C., Briggs, C., Bachkar, K. Managing risk in pharmaceutical global supply chain outsourcing. Proc. Amer. Soc. Busi. Behav. Sci. 16(1), 2009. [February].
European Union. The rules governing medicinal products in the European Union, 2009. [vol. 4: Good manufacturing practice (GMP) guidelines].
Evans, K. A CDER official offers tips on inspections. CDER Inspection Tips. Master Control: Salt Lake City; 2006. [p. 4].
FDA. Guideline for Quality Assurance in Blood Establishments. Rockville, MD: CDER; 1995. [11 July].
FDA. Guidance for Industry: Current Good Manufacturing Practice for Medical Gases. Rockville, MD: CDER, May, p.. 4, 2003.
FDA. Guidance for Industry: Part 11, Electronic Records; Electronic Signatures – Scope and Application. Rockville, MD: CDER, August; 2003.
FDA. Guidance for Industry: Sterile Drug Products Produced by Aseptic Processing – Current Good Manufacturing Practice. Rockville, MD: CDER, September; 2004.
FDA. Guidance for Industry: Sterile Drug Products Produced by Aseptic Processing – Current Good Manufacturing Practice. Rockville, MD: CDER, September; 2004.
FDA. Pharmaceutical cGMPs for the 21st Century – A Risk Based Approach. Final Report – Fall 2004. (September):2004.
FDA. Guidance for Industry: Q9 Quality Risk Management. Rockville, MD: CDER, June, p.. 13, 2006.
FDA. Guidance for Industry: Quality Systems Approach to Pharmaceutical cGMP Regulations. Rockville, MD: CDER, September, p.. 13, 2006.
Garstka, A., Hagman, D.E. The benefits of training right. SP Forum, 9. (March):2000.
Canada, Health. Good Manufacturing Practices (GMP) Guidelines – 2009 Edition (GUI-0001). Ottawa: Health Canada; 2009.
Hubby, S.A. Integration of Q9 quality risk management when conducting GCP regulatory inspections and audits, presented at the 45th Annual Meeting, Drug Information Association (DIA). CA: San Diego; 2009.
International Conference on Harmonisation (ICH). Good Manufacturing Practice Guide for Active Pharmaceutical Ingredients – Q7A. Geneva: ICH Secretariat; 2001.
International Conference on Harmonisation (ICH). Quality Risk Management Q9. Geneva: ICH Secretariat, 2005; 2–4. [9 November, pp].
McConnell, J.H. How to Identify Your Organization’s Training Needs. New York: AMA; 2003. [p. 108].
Nielsen, J. Usability Inspection Methods. CHI’94 Companion, Association for Computing Machinery, Boston, MA, 24–28 April, 1994:413–414.
Nielsen, J., Molich, R. Heuristic evaluation of user interfaces. CHI’90 Conference, Proceedings of the Association for Computing Machinery, Seattle, WA, 1–5 April, 1990:249–256.
Nielsen, J., Pernice Coyne, K., Tahir, M. Make it usable. PC Mag. 20(3), 6. (February):2001.
Piton, A. Risk-based assessment applied to QA GLP audits. Annali dell’ Istituto Superiore di Sanità.. 2008; 44(4):382.
Saxena, A. SOP writing for clinical trials: staff training aspects. January: International Biopharmaceutical Association Publication; 2005.
Strack, B. Training for the real world. Appl. Clin. Trials. 14(3). (March):2005.
Sylvia, D. Fresh air 2002. CDER Medical Gas cGMP Workshop, Rockville, MD: CDER, 15. (March):2000.
Trautman, S., Klein, K. Ask an expert. Train. Devel.. 1993; 48:45–48.
US Department of Veterans Affairs. Credentials and training of employees involved in human subjects research, 2003. [VHA Directive 2003–036, 7 July].
Vesper, J. Defining your GMP training program with a training procedure. BioPharm (Eugene, OR). 2000; 13(11):28–32.
Williams, S.W. The effectiveness of subject matter experts as technical trainers. HR Devel. Quart.. 2001; 12(1):92.
1See OSHA, 29 CFR 1910.134(k) Respiratory Protection, “The employer [is required] to provide effective training to employees who are required to use respirators. The training must be comprehensive, understandable, and recur annually, and more often if necessary.” See also ∫ 1910.134(k)(5), “Retraining shall be administered annually.”
2For the distinction between quality risk assessment and business risk assessment, see Chris Enyinda, Charles Briggs and Khalid Bachkar (2009); for the distinction in the GLP context, see Alain Piton, (2008); for the distinction in the GCP context, see Sherri A. Hubby (2009).
3On the one hand, such an e-mail message would be exempt from Part 11 considerations. Among the few training related predicate rules that are covered by 21 CFR 11, Electronic Records; Electronic Signatures, is 21 CFR 111.14(b)(2), which stipulates “Documentation of training, including the date of the training, the type of training, and the person(s) trained,” relating to GMPs for Dietary Supplements. [Published in the Federal Register, Vol. 72, No. 121, 25 June 2007, p. 34810]. However, the message itself can include the proviso that “This message is not a GMP document; for GMP purposes, refer to the source document in the LMS,” etc.
4See FDA, Pharmaceutical cGMPs for the 21st Century – A Risk-Based Approach, Final Report-Fall 2004, September 2004. See also John Gardner’s comments, as reported in Joseph Pickett, “GMP audit imminent after 6-year inspection gap, states 2007 risk-based model: Gardner,” Validation Times, September 2007.
5See International Conference on Harmonisation (ICH) (2005).
6ICH, Q9, Quality Risk Management, op. cit., p. 2.
721 CFR 211.25(a), Personnel qualifications.
821 CFR 606.20, Personnel. The relevant phrase is “adequate information concerning the application of pertinent provisions of this part to their respective functions.”
9See European Union (2009) ∫ 2.9. Health Canada (2009), Regulation C.02.006. ∫ 6.
10See FDA (2006). Thus a business rationale as well as a compliance rationale can be made for continuing training. For the business rationale, see Anne Garstka and Donald E. Hagman (2000), “training must be continuous. By providing continuous training, pharmaceutical companies instill good habits that lead to safe, effective products and higher profits.”
11International Conference on Harmonisation (2001), ∫ 3.12. [Published in the Federal Register, Vol. 66, No 186, 25 September 2001, pp. 49028–49029.]
12Regarding clinical trials staff, see Barry Strack (2005), “the incorporation of continued training is an important element that many popular programs neglect to focus on.” See also Akanksha Saxena (2005), “management should see to it that there is continuous training of SOPs among the staff.” Also US Department of Veterans Affairs (2003), VHA Directive 2003–036, requires “appropriate training in the ethical principles and good clinical practices for human subjects research on an annual basis.” Regarding institutional review boards, see, for instance, Jeffrey Cooper and Pamela Turner (2006), who state “An institutional review board (IRB) ‘shall be sufficiently qualified through the experience and expertise of its members … to promote respect for its advice and counsel in safeguarding the rights and welfare of human subjects.’ Meeting this regulatory requirement requires initial and continuous training” (p. 313). They are citing 21 CFR 56.107, IRB Membership.
14Interpretive issues about observations arise on the regulatory side as well. Consider the FDA 483 observation to Medlmmune dated 29 March 2007 “on 28 March 2007 […] an operator was observed cleaning his/her personal prescription glasses in the ISO Class […] area.” Compare that to FDA warning letter to MedImmune dated 24 May 2007: “On 28 March 2007, an operator was observed removing his/her safety glasses, then removing and cleaning his/her prescription type glasses, thus allowing for skin to be exposed.” Available from: www.fda.gov/downloads/AboutFDA/CentersOffices/ORA/ORAElectronicReadingRoom/UCM056161.pdf and www.fda.gov/ICECI/EnforcementActions/WarningLetters/2007/ucm076398.htm
1521 CFR 211.25(a), Personnel qualifications.
16Health Canada (2009), Regulation C.02.006, J6.1.
17See Joanne W. Cochran and Joseph D. Nally (2006).
18“Standard operating procedures (SOPs) are sequences of steps for workers to follow to complete tasks.” See Mark Edelman (2003).
19See Cochran and Nally, op cit., “Minimum requirements for trainers may include some formal education (e.g., Train-the-Trainer course) or experience in presenting training …”
20See Table 7.3. As Breggar, op. cit., p. 26 has aptly put it, “Generally speaking, most FDA citations appear technical. But their root cause is nearly always managerial issues that impede the performance of people.”
21Saundra Wall Williams (2001) cites Anthony P. Carnevale et al. (1990); Ruth Colvin Clark (1994); and Steve Trautman and Kate Klein (1993). See also Cochran and Nally, op. cit., “Often the person who has the best technical knowledge is not necessarily the best trainer.”
23See J. Vesper (2000).
24Vesper, op. cit. This is a short-term option; in the longer term, management will likely prefer a SME becoming a qualified trainer, or a qualified trainer becoming a subject matter expert.
25See also Willem PA van der Tuuk Adriani and Smit Sibinga (2008).
2621 CFR Sec. 211.25(a), Personnel qualifications.
27See FDA (2006) Guidance for Industry: Quality Systems Approach to Pharmaceutical cGMP Regulations.
28See FDA (2004), Guidance for Industry: Sterile Drug Products Produced by Aseptic Processing – Current Good Manufacturing Practice.
29See FDA (1995).
30Available at www.fda.gov/downloads/AboutFDA/CentersOffices/ORA/ORAElectronicReadingRoom/UCM109834.pdf These are but two of an extensive series of observations.
31See Jakob Nielsen and Rolf Molich (1990); Jakob Nielsen, Kara Pernice Coyne and Marie Tahir (2001); and Jakob Nielsen (1994). While Nielsen and his colleagues address software and web usability issues, the principles of end-user and heuristic usability testing apply to paper-based forms as well.
32See Gerhard Becker (2007), for fiscal years 2005–2006, and Gerhard Becker (2009), for fiscal years 2006–2008.
33See ICH (2005), op. cit., p. 15.
34See ICH (2005), ibid.
35See FDA (2003).
36See Duane Sylvia (2000). See the interview with Kristen Evans, A CDER official offers tips on inspections, CDER Inspection Tips, Salt Lake City: Master Control (2000), p. 4: “Training should not be a one-shot deal. It has to be ongoing and dynamic.”
37See James L. Vesper (2000), op. cit., p. 29.