![]()
CHAPTER THREE
E-HEALTH PERSPECTIVES
General Systems Concepts, Chaos and String Theories, and Social Science Thinking
Joseph Tan
A. Systems Thinking and Analysis
B. Metaphors and Mental Models as Systems Analysis Tools
IV. Chaos Theory and String Theories
A. Chaos Theory and Quantum Mechanics
A. E-Communities as Sociocultural Entities
B. Single Versus Multiple Contexts
IX. Multicommunity E-Health Promotion Programming Case
Learning Objectives
- Relate general systems concepts to the e-health care system and environment
- Apply systems thinking and analysis tools to understand the functioning of e-health systems
- Conceptualize self-learning systems in the context of chaos theory and quantum mechanics
- Articulate the concept of supersymmetry and its implications for changing the mind-set and redefining the role of e-health leaders
- Apply virtual global team thinking in social science to address e-health system perspectives
- Recognize how e-health systems can be conceived as evolving sociocultural entities
Introduction
This chapter allows the reader to take a closer look at the gradual breakdown of conventional thinking about organized health care delivery systems. Whereas in Part One this was done from the perspective of a historian, in this chapter it is done from the viewpoints of a systems philosopher, a physicist, and a social scientist. The reader may ask, “Why is it necessary to adopt such multiple views?” Perhaps the simplest answer is because e-health is a complex interdisciplinary field whose concepts, applications, methodologies, technologies, strategies, and impacts defy comprehension from a single perspective (see Part One). This chapter will provide a survey of theoretical perspectives applicable to e-health.
First, we review general systems concepts and discuss how these concepts relate to the e-health care system and environment. Next, we examine chaos theory and concepts of quantum mechanics, including a brief survey of different versions of string theories and an attempt to see how these theories may help transform our understanding of e-health. Following this, we examine emerging thinking in social sciences with respect to virtual global teams and relate this thinking to the development of e-health.
General Systems Concepts
General systems theory (GST) begins with the observation that what we see, hear, and interact with may be rationalized as a hierarchical network of systems and subsystems. In light of this, systems can be whole and be part of other systems (subsystems) at the same time. Examples of systems range from the galaxy to cells, organelles, and various submicroscopic and particulate systems to bed allocation systems, hospital information systems, the e-health care system, and the general health care system.
A system must have a purpose. In fact, a system may be defined simply as a set of interrelated parts that function together as a whole toward achieving a common purpose. Systems can also be characterized as being open or closed. For example, the U.S. health care system, which interacts actively with its environment on a minute-by-minute basis, is an open system, whereas a hospital room directory system, which is absolutely self-contained, is a closed system. The Canadian public health care system, for example, has the overarching goal of achieving excellence in public health and improving the quality of life and well-being for all Canadians. This purpose is expected to guide all subgoals of its embedded subsystems, including the bed allocation system, various health information systems, and various networks designed to support the main system. Systems can also range from simple (for example, a computerized payroll system) to very complex (for example, the computer network system for the New York Stock Exchange).
Open complex systems are characterized by input-process-output triads and feedback loops. GST easily describes the flow of appropriate and relevant information about sick patients (input), who are placed into the different subsystems of the acute health care system to be treated and cared for (process) until they are ready, perhaps, to be transferred to another subsystem such as a group home (intermediate output) before being discharged as healthy individuals who can continue to contribute to their work organizational systems (final output). Continual monitoring of the health status of these patients becomes the feedback loop in the system. These loops ensure the reliability and quality of health services provided, including those before and after the patients are discharged. A common example of an information system that controls this acute patient care process in a hospital setting is the admission-discharge-transfer (ADT) system.
In earlier works (Tan, 2001), the principles of GST concerning the behaviors of organizational systems and subsystems were used to think about the design of different classes of clinical and administrative health management information systems required to run hospitals and health provider organizations. To apply GST to the e-health care system and environment, the first step is to identify the various associated subsystems in terms of their inputs, processes, outputs and feedback loops. One subsystem that comes to mind is e-health records (EHRs), which will be discussed in detail in Chapter Four. In this system, the input consists of patient records stored in a data warehouse or a database. The processes are comprised in the management of those records, including automatic data gathering, cleaning and verifying, adding or deleting information, and retrieving or combining data to answer queries. The output of the system is the information or knowledge from the records that is displayed when queries from e-physicians or other e-caregivers are answered. Feedback loops in the system may include responses from e-patients on the information given to their e-physicians such as information on allergies and responses to queries for information from the EHRs that e-caregivers may make to ensure complete, correct information in the system.
While this description may appear unsophisticated and similar to the function of traditional health record systems, in part because EHRs are also used in traditional health care, in the e-health context, information sharing by the various e-stakeholders is far more complex. For example, information from police arrest documents may electronically follow the arrestee to the corrections facility. Understanding the types of data to be captured from e-stakeholders (multiple inputs) and the nature of the shared data flows (compound processes) needed to support the active exchange of information from EHRs (multiple intermediate and final outputs) in everyday activities can be challenging. Yet such understanding is needed to design relevant network infrastructures to support the many e-care delivery functions and continual data manipulation activities involved in the effective use of EHRs in e-health.
Systems Thinking and Analysis
Over the past fifty years, systems thinking and analysis have developed a body of knowledge and tools to make the complete patterns embedded in systems clearer and to help us see how to change them effectively. One such approach involves the execution of five learning disciplines: personal mastery, shared vision, mental models, team learning, and the overarching discipline of systems thinking (Senge, 1990). Systems thinking means seeing the connections among the processes of change, not just snapshots of changes; in other words, the focus should be on interrelationships rather than linear cause-effect chains. Owing to the prevailing focus on detail complexity at the expense of dynamic complexity, Senge notes that even elegant strategic planning fails, especially when the plan attempts to deal with too many variables and neglects dynamic cause and effect. Because dynamic complexity is subtle and does not necessarily happen at contiguous times, systems analysis efforts tend to focus on detail complexity. Unfortunately, the real leverage in most management situations lies in uncovering the underlying dynamic complexity.
In designing e-health care systems and networks, it is thus imperative to pay attention to the dynamic nature of e-health. In other words, not only should key factors and variables be tracked carefully, but moderating and intervening variables should also be monitored, to ensure more complete and intelligent management and decisions. For example, in developing an e-public health statistical system to examine and investigate the health of a population, key indicators such as average life expectancy (measured in number of years) and infant mortality (measured in infant deaths per 1,000 live births) must be tracked, and gender, age, race, and other moderating variables such as location and diet should also not be neglected. Ignoring intervening variables could result in an incomplete picture with too many unanswered questions. The power of e-technologies makes tracking all of these variables a less difficult task than it may seem.
Similarly, Capra (1996) identifies a number of key characteristics of systems thinking and analysis, including the shift from emphasizing the part to emphasizing the whole; from viewing objects as of primary importance to viewing relationships as being of primary importance (also called network thinking); from paying attention to a single system level to moving between system levels; from using an analytic approach to promoting contextual thinking; and from employing objective analysis to applying epistemic science, in which the method of questioning is key to how scientific theories are understood.
In analyzing the data contained in an e-government refugee immigrant statistical system, for example, considerable attention should be paid to available support for lifestyle and cultural changes, community services, language education, on-the-job training, and location with a view to increasing the number of job opportunities for the refugees. Unfortunately, the analysis is often done in isolation and without adequate assessment of the impact of possible inadequate supporting infrastructures such as language education and on-the-job training, as well as possible failures of community services (for example, Australia sometimes only permits new immigrant refugees to settle in remote, underserved areas). If ongoing support for community services and language education as well as on-the-job training is inadequate, increasing the number of refugees every year may backfire: incoming refugee immigrants may just decide to go back to their own or on to other countries. Even worse, they may turn to crime or other destructive activities and become a burden to society.
Lindstrom, Matheson, and Tan (1998) note that in systems thinking and analysis, the need to distinguish fragmentation from wholeness in our tendency to lean toward analytic reductionism is an important step. They argue that there is often a propensity to think that having better and faster information at our disposal will lead naturally to better and faster decisions. Bohm (1980) indicates that this may not necessarily be true, because a fragmentary view may eventually lead to conflicting and confusing biases. In other words, if explanations of a system are a result of analyzing piecemeal and fragmented data, applying system methodology to understand the events that gave rise to the information in the first place will only result in a stovepiped mentality. If we extend this thinking to the e-government refugee immigrant statistical system, we might see a healthy and balanced rate of new job opportunities and be impressed by the comparative increase in number of employed refugee immigrants. In the real-world case from which this example is drawn, the data on the refugee population had an undiscovered trend of increasing job dissatisfaction and deteriorating working conditions. No account had been taken of the fact that many of these refugees were skilled professionals who were now limited to poorly paid unskilled labor. Hence, in analyzing systems, we must be sure to examine all the relevant pieces in order to get the whole picture.
Metaphors and Mental Models as Systems Analysis Tools
An important final point in the systems thinking and analysis approach to decision making is the development of models that are used to obtain valuable insights into the behavior of a system. For example, we often attempt to understand a system, such as the evolving e-health care system, by gathering and analyzing selected data and inputting them into a model without due consideration for known intangible factors that affect the behavior of the system. Potential intangibles in e-health care include impacts from redesign of work practices, resistance from labor unions, and other sociopolitical factors. Because many of these factors are too difficult or complex to simulate or model concretely, we try to piece together just the quantifiable parts to develop an aggregate. These quantifiable factors thus form the basis of our management or clinical decisions. Within the context of the e-health care system and its environment, variables often are not easy to quantify; for example, consider the variables involved in ethical, legal, and privacy issues. Ultimately, improving e-health care and achieving better health status of e-patient populations depend largely on the extent to which we can accurately model the system and its inherent behaviors. Since e-health is complex and requires dynamic as opposed to static simulations, models can represent only the first cut at predicting complex system behaviors.
Notwithstanding, Lindstrom, Matheson, and Tan (1998) note that the use of metaphors and mental models in the application of systems theory to organizational studies and to studies of complex information and network systems in organizations is a particularly eye-opening and refreshing approach. Based on this perspective, a virtual health network may be conceptualized by using the analogy of a neural network. Basically a neural network (NN) may be conceived as a simplified emulation of the connections of the human brain. It is used here for depicting learning and self-organization within an artificial environment. Neural networks, with their remarkable ability to derive meaning from complicated or imprecise data, can be used to extract patterns and detect trends that are too complex to be noticed by either humans or simple mathematical and programming techniques. Just like an NN, an e-health organization is capable of adaptive learning, self-organization, and real-time operation. This analogy will be relevant to our discussion of e-health network management.
Metaphorically, the memories, learning capacities, and mind-set of an organizational NN correspond to its enterprise-wide information, communications, and networked decision-making systems. Imagine John, the CEO of a major e-health care corporation, who is planning to retire. Before he steps down, he wants to ensure that critical pieces of information, communications, and decisions are captured in one form or another in a corporate enterprise resource planning (ERP) system. Perhaps this ERP system is a recently installed e-network, which is analogous to the NN. John's goal, then, is to make it possible for whoever succeeds him (he has his eye on his son, currently vice president of operations) to have access to the “neural network” capabilities and memories of the corporate culture now being captured virtually in the corporate ERP system. To the extent that this may be operative, John can have some assurance that the future administration of the corporation will have the benefits of his founding vision and his practices. Metaphorically, this implies that whoever takes over the corporation will understandJohn's history, strengths, culture, and orientation, and thus the corporation will continue to function and learn as if John were available to provide advice to his successors as needed. The ERP system or e-network thus projects a virtual mind-set and culture throughout the corporation.
How can the metaphor of the corporate neural network help us to understand the role of the e-health network infrastructure (enterprise system)? If system neural networks function in such a way as to pull together all of the necessary information and decision making processes of the organization, then we can argue that not only will these neural networks capture, store, process, and disseminate massive amounts of previously learned information, but they will also be able to coordinate and structure learning of new methods and better approaches among users so as to improve the management of the enterprise system (organization) over time. Morgan (1997) uses the term network intelligence to refer to this phenomenon. He believes that individuals, by accessing the “neural networks” from evolving knowledge networks and communication networks throughout an enterprise can become fully aware and participate in evolving networks of organizational memories and intelligence. System NNs create capacity for the evolution of a shared intelligence and memories. Going back to the example, John's intelligence and expertise, as well as his memories and learning during his leadership tenure, can now be easily and conveniently passed down to his son or whoever becomes the next CEO. Put simply, the NN metaphor implies that the communications among e-stakeholders within an e-health enterprise can be enhanced and enriched to a point where captured knowledge, key final decisions, and policies made by management can become easily accessible to those who need them.
To extend our NN metaphor and its implications for e-health networks and e-communities, evolving organizational knowledge and other enterprisewide networks could have major implications in altering or redirecting the bureaucratic principles of centralized control to a self-learning paradigm. The key here is to create a sharing network of interactions that can self-learn—that is, help generate further learning, shaped or driven by the intelligence of everyone involved in primary decision making throughout the virtual enterprise.
The “architecture of integration” articulated by Beckham (1993) is another interesting concept relevant to this metaphorical thinking. Integration in this sense is a process through which different parties (government, third-party insurers and payers, e-providers and e-vendors) can act as one mind within the system to serve e-consumers; that is, separate parties with individual minds can be meaningfully organized to act as if their minds were integrated. In many respects, the extent of integration can be used as an indicator of how well the networks support the infrastructure and functions of the virtual health care delivery system.
To determine the extent of virtual integration, especially in terms of network design and infrastructure, the following questions may be advanced:
- Are data collected electronically and directly from e-consumers? If so, how willing are e-consumers to provide the data? If not, why not?
- Do all e-providers have free virtual access to the same e-consumer records? If so, how is access authorization verified? Does the network provide the data unambiguously?
- Do the e-stakeholders operate as a well-coordinated virtual team in service delivery? If not, why not?
- Are e-consumer satisfaction and other measurable outcomes being tracked? If yes, how, and what other measurable outcomes are tracked? If not, why not?
- Does a single network serve the needs of e-stakeholders and decision makers at all levels? If not, why, and how can the challenges be overcome?
Mental models are also useful in systems thinking because they provide simplifications of complex e-health system structures. Networks can be designed using different mental models, depending on the perspectives of system users.
For B2C models, a service model perspective is most important because the availability of a convenient tool for e-transactions or e-purchases; on-line connection for inquiries to e-stakeholders, including e-providers, e-vendors, and e-insurers; and realtime access to relevant information resources are all key to meeting e-consumer needs.
For B2B models, the mental models reflect the views of the participating business entities. For instance, an e-vendor supplying prescription drugs wholesale to one or more retailers on-line will want to know the inventory status of the retailers, their account standing, and average monthly sales volume. An accounting model is therefore most relevant and appropriate.
Finally, for C2C models, active information exchange and potential for trading transactions lead to a model that balances the perspectives of the consumer-oriented service model and the transactional, accounting-oriented model; in other words, a hybrid model may be the best framework to pursue. In any case, mental models provide a starting point; system designers and leaders must interpret and determine what consumers and stakeholders expect and want from the system, since those consumers and stakeholders will eventually dictate the success of the new system.
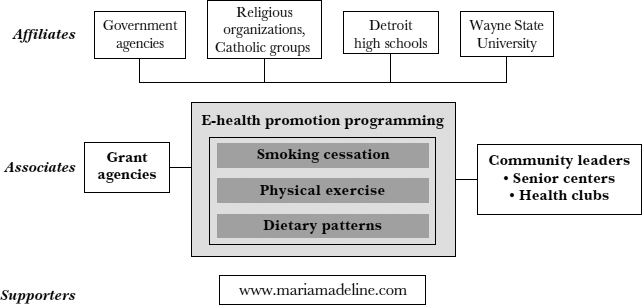
The rich picture approach (Tan, 2001) is an especially powerful context-setting visual tool. It provides a powerful tool for mentally modeling any form of complex system as it allows various entities and relationships to be depicted in any ways that are meaningful to the users. Figure 3.1 depicts a rich picture of a multicommunity network designed to promote e-health activities among seniors interacting with high school students in a recently funded e-multicommunity health project, the Maria Madeline project (see the case discussion in this chapter), investigated by me and my colleagues at Wayne State University School of Business. This is a “structural” depiction as opposed to a “pictorial” one. Typically, a rich picture allows the users to use any form of familiar symbols to depict ongoing activities and events or even conflicting views.
FIGURE 3.1. A RICH PICTURE OF AN E-MULTICOMMUNITY HEALTH PROMOTION PROJECT
A convenient tool for documenting themes or issues for an ill-defined problem situation, the rich picture is especially suited to our mental modeling of soft and fuzzy issues such as conflicting views and attitudes among different stakeholders. In the case of this project, which focused on designing and offering Internet-based Web access primarily to underserved seniors living in innercity Detroit, one such issue is the scope of computing training that may be needed by the seniors. Our project emphasized intergenerational programming by having high school students partner with seniors interested in learning to use the Internet. This instructional approach prepared the seniors to teach themselves to access available e-health services. The seniors first learn to extract data from the Internet via the Maria Madeline Web site (www.mariamadeline.com) and then via the World Wide Web, using various search engines. The rich picture we generated is only a simple first-cut mental modeling of the system based on one possible scenario of who would be these stakeholders in the system and what interactions will be expected among them.
Enriching this mental modeling process is the creation of differing realities, independent of the data observed. These differing realities can be initially investigated by using rich pictures to explore different scenarios to see how different designs of the community network would affect various e-stakeholders. These realities are imagined possibilities (idealized results), which are a combination of changing events, states of events and sequences of events. Further, when designing the network, exploring the relevance of different pieces of information (input or process variables) in the context of several metaphorical perspectives (which can be translated into different rich pictures) demonstrates that no given piece of information is of primary importance; instead, the entire metaphor or mental model is central to understanding the way the health care business should be changed, the way new e-health strategies should be implemented, and the way each of us read, understand, and shape our thinking and thereby our community, culture, and sociopolitical work life.
As we address the limitations of general systems theory and see how other frameworks can help us think about the role that decision makers and information will play in shaping the emerging e-health care era, we will soon discover new and emerging perspectives and conceptual frameworks provided by chaos theory, quantum mechanics, and string theories.
Chaos Theory and String Theories
The tools of systems thinking and systems analysis help us study and describe health care systems, including traditional hospital bed allocation systems; various administrative, financial, and clinical information systems; and even the traditional health care service delivery system (see Tan, 2001). Yet the application of these tools to self-learning systems, which are more dynamic in nature, is limited. Fortunately, recent developments in particle physics, chaos theory, quantum mechanics, and string theories together have unveiled further insights into the nature and characteristics of very complex systems.
Chaos Theory and Quantum Mechanics
Chaos theory, a mathematical science that has been examined subsequent to the era of computing and office automation, observes that extremely small changes, or perturbations, in the starting conditions of a set of equations or a mathematical model can lead to extremely different solutions. Nonetheless, solutions for any starting conditions derived by the mathematical model are always contained within a restricted set of solutions, commonly referred to as the strange attractor. Other aspects of chaos theory, such as the study of changing shapes and patterns known as fractals, are built on the idea of evolving complex structures that mimic natural biological systems. In fact, these complex structures behave like neural networks built on the successive “mutations” of simple equations. In other words, they reflect iterative applications of the initial equations, with each step depending on the results of previous steps. The methodology of neural networks is further described and illustrated in Hammad (1998).
Based on chaos theory, we can confidently infer that for any given set of constraints in an e-health system environment, small perturbations in a network can lead to major consequences. Moreover, this environment is not fixed in a set configuration but is dynamically changing. Just like any other organizational system, an e-health care system can be characterized as a living system thriving in an environment that has the potential for it to grow sensibly, creatively, and intelligently. It will be able to adapt to its changing environment and will seek order in order to maintain its meaning. An e-health system will naturally tend to organize itself, be it through a formal reporting structure or through informal structures such as virtual task groups and teams. Because the system is dynamic, its identity will continue to mutate, largely because of a changing infrastructure and evolving environment. In fact, there may be very little difference between the e-health system I am discussing here and the many social and political communities that we interact with in real life, except for the virtual aspect of the e-health care system.
Societal life is becoming more complex because of the increasing number of relationships being formed, the growing amount of information and knowledge that is available in each passing year, and turmoil in the daily sociopolitical environment. The interconnectedness and interdependence of these systems are reflected in the inter-connectedness and interdependence of components within the e-health system. Such systems dictate new forms of behavior that may be difficult to predict intelligently. Attempts to decompose the systems into series of fragmentary parts without a clear understanding of the interfaces among the various parts will result in a limited world-view that also lacks understanding of the system dynamics. Thus, we have to go beyond the GST approach when studying nontrivial systems.
In quantum mechanics and physics, how we observe electrons determines whether a field of energy or a particle exists. Because electrons are known to have the capacity to be either energy waves or particles, fields can affect particles and particles can affect fields. Coupled with the observations of chaos theory, new discoveries in quantum physics tell us that the basis for the reordering and restructuring of elements and interactions (particles and fields) within systems is perturbation; in short, some uncertainties are inevitable because perturbation can be conceived as part of what creates the system, and such perturbations are needed if we want the system to yield responses that will in turn evolve toward order. As nature is inherently orderly or will be “attracted” to order, perturbation in the system will lead to balancing change occurring in a system until a steady state is achieved. Therefore, however small and subtle the perturbations may be, when they are introduced at the very beginning of a process, they will eventually lead to changes that may not always be small; indeed, even significant transformations can result from subtle movements. As we have learned, the evolution of e-health systems is an outcome of successive perturbations experienced and witnessed in traditional health care, caused by factors such as user dissatisfaction, governmental interventions, and changes in directions of health leadership. Moreover, we would expect the current e-health environment to change further via some form of evolutionary strategy rather than through an act of force.
Just like any living system, e-health networks cannot and therefore should not be forced to change to achieve particular results within a set time period. Accordingly, strategic planning is best achieved by means of the natural forces influencing change instead of imposed change. The emphasis should be on balancing between “forced” change that is drastic in nature and no change at all because it is not characteristic of living systems to behave in both these manners. In view of our current understanding of dynamic systems and particle physics, we foresee that the evolving networks in e-health enterprises will be best altered in subtle ways as self-learning occurs. Nevertheless, a sense of achievement may be realized at particular times, representing milestones in the history of the health enterprise computing.
Even so, solutions derived from a virtual collaboration among team members resulting in “change” will be very different from those imposed by an individual or even those arrived at during a face-to-face meeting, because the change process will be different. For example, some team members who shy away from participating in face-to-face meetings may be aggressive and vocal in on-line communications. Conversely, those who are usually active in physical meetings may not be as active on-line. Others, feeling the need to show that they are listening and paying attention, may contribute new insights to group thinking. With virtual networking, results achieved may be more likely to be seen as the decision of the entire group and not of any one particular individual, making any proposed changes much easier to implement and sustain over the longer term.
Lindstrom, Matheson, and Tan (1998) note that in quantum physics, a “field” governs the particles within itself and that “fields” themselves may be perceived as particles and hence be governed by a larger field. In an interconnected e-health system, fields are analogous to the visions, missions, values, and goals of subsystems embedded in larger fields with overarching visions, missions, values, and goals. The clarity of the overarching e-health vision and goals (see Chapter Two) will reflect the clarity of a still larger field and will dictate how its subsidiary particles (or embedded fields) will respond. To a large extent, this process will define the strange attractor that forms the set of solutions to any perturbations that may affect the entire system (Lindstrom, Matheson, and Tan, 1998). Put simply, the interconnectedness among elements in e-health networks constrains the emergent solution set. The fact that even a very small perturbation instituted at the beginning of the process can lead to a major change in the system leads to reflection on how we should encourage exchange of ideas, even disagreements, among affected stakeholders in order to arrive at a reasonably acceptable consensus. In this system, fields (representing vision, mission, values, and goals) guide outcomes, leading to suitable and acceptable solutions, but do not predict those outcomes. Conversely, lack of clarity in the fields or vision will lead to the risk of inappropriate and inadequate “solutions.” In this view, the fact that the same values can be shared holistically among all e-stakeholders in an e-health network will naturally lead to self-learning and order, stabilizing the entire system.
Self-learning systems can therefore be defined as systems with “the ability of all living systems to organize themselves into patterns and structures without any externally imposed plan or directions” (Wheatley and Kellner-Rogers, 1995). In a self-learning system, change is not only inevitable but is a powerful, creative force resulting from earlier stages of system instability. Instability is sometimes desirable, even necessary. Purposeful (but subtle) perturbations can, if appropriately encouraged and balanced, lead to a desirable order for the system. If a system has always been stable, no change is ever warranted and no new learning can be achieved. For example, if the traditional health care systems were sufficient and there had been no technological advances, economic pressures, or breakthroughs in system thinking, health care would never have evolved into the e-health era.
Left alone, self-learning systems would improve over time on their own because they are preprogrammed to learn and adapt to changing environments. In our e-health network example, clarifying any ambiguity in the vision and values over time, welcoming contributions from team members and letting go of those who may hinder organizational productivity, as well as providing a means for everyone in the network to stay interconnected, will eventually result in a network that achieves the continuous improvements in availability, accessibility, affordability, and accountability that were discussed in Part One of this text.
Supersymmetrical Thinking
According to Lindstrom, Matheson, and Tan (1998), the principles of chaos theory and quantum mechanics offer insights into how to characterize the evolution of knowledge about complex structures and systems. It is suggested here that because complex structures and systems are mostly organic and dynamic with characteristics of self-learning, predicting the behavior of these systems therefore requires application of conceptual frameworks that may themselves be complex, that is evolving over time given the many interacting components that are to be modeled. The science of particle physics has been undergoing a revolution, and its theoretical development has provided new insights into how the properties of particles can be transformed. This is where string theories come in. Although there are many string theories, here we will examine only the underlying concept of supersymmetry.
Physicists can now safely infer that all known particles can be classified either as bosons or as fermions. Bosons are particles that transmit forces and can occupy more than one state at the same time—for example, energy and light—whereas fermions are particles that make up matter and can occupy only a single state at a given time—for example, the components of tables and chairs. In other words, fermions are physically visible and space-occupying objects, while bosons are, in a practical sense, energy forms of particles that can be digitally (or electrically) transmitted from one point to another and be in both places at the same time.
Both human beings and walls are made up of fermions. Since fermions can be in only a single state at any one time; that is, we cannot walk through walls without hurting ourselves. In particle physics, this idea is referred to as the exclusion principle.
The properties of bosons—for example, in light—are just the opposite. If we flash the beams of two flashlights at each other, we see that the two beams appear to pass right through each other without any interference. This is because bosons can occupy more than one state at the same time, allowing them to occupy the same space at the same time. Thus, the beams can overlap each other and still be part of both each other and themselves. In contrast, if we overlap two streams of voice—say, one coming from a radio and another from a television—what do we expect? Although these voices may appear to overlap, they will also appear scattered or disintegrated. This scattering is mostly electrical because the voices could have been electrically streamlined into one voice, given some transformational processes and time such as synchronizing the different analog sound waves into a single digital voice stream with equal speed and similar signal sequence intensity. This is just an analogy from which we can see that different signals appear to have produced the “scattering” that is felt. Hence, you can still hear two separate voices, when in fact, both voices are of the same form of energy.
Jim Gates, one of the foremost scientists in string theory, uses the example of connecting two streams of water from separate hoses into one. Because water may be transformed into a form of electrical energy, according to Gates, even if you could turn off the electrical charges from the separate hoses where the two streams hit each other and merge into one, the exclusion principle would still apply; hence, the water streams behave as if composed of fermions, although as a form of energy in transmission, they are essentially bosons. This phenomenon is known as supersymmetry and this same phenomenon applies to information, as will be demonstrated later. Here, our purpose is to provide counter examples of fermions and bosons behaving supersymetrically.
As indicated, the world we see, hear, touch, smell, and taste comprises an apparent separation of fermions and bosons. The moment we question why we should limit our thinking to this apparent dichotomy, we begin to move towards a skepticism known as supersymmetry thinking, which is the core dilemma in string theories. Indeed, would not the world be or become more symmetrical (supersymmetrical) if some forms of matter could pass right through one another, just as energy and light do, and if some forms of energy could scatter one another just as “physical matter” such as water does? To take another example, is information all bosons? It can be digitized and passed through electrical cables to our television screens or fax machines; however, if this information is displayed as physical words or images occupying some space, and we need to erase and change the written words or graphic images for one reason or another, is it then fermions on the output medium (for example, television screen or fax paper) but bosons in the brain or cable?
The basic idea of supersymmetry, then, is that perhaps both matter and energy can be transformed into either fermions or bosons, bringing about some convergence of the properties inherent in the two classes of particles. Such a finding would be a scientific breakthrough (a significant paradigm shift) that would defy and transform our conventional thinking about nature. If that becomes a possibility, we will soon arrive at supersymmetrical thinking. In the world of particle physics, the idea of supersymmetry is to break away from the stereotypical thinking of fermions versus bosons to define the world we live in. Right now, this is purely hypothetical. Many scientists are hopeful that this idea will one day be verified, bringing together the different string theories and collapsing all of them into a single M theory (the “mother” of all string theories).
Applying supersymmetrical thinking to e-health networks and systems, we see that the key idea in moving toward an e-health paradigm is to provide ubiquitous access to e-health information. Instead of limiting knowledge and specialized medical information to just a few, those who need to be guided can now have access to specialized knowledge and information so as to capitalize on the transformational power of advanced networking infrastructure and technologies. In other words, doctors and specialists (fermions) will behave like complex information dispensing systems (bosons) and the media or digital devices can in term be used to dispense such e-health information (bosons) to those who may need it (fermions). Ultimately, this will result in producing a supersymmetrical world in which intelligent agents (including humans, information systems, and hybrid systems) will be able to combat many forms of diseases because of the ubiquity of e-health knowledge and information. Globalization, integration, and empowerment are all aspects of supersymmetrical thinking based on the foregoing reasoning of transforming human experts into intelligent agents and e-health information dispensing systems. Similarly, these e-health information dispensing systems can be engineered to produce intelligent human or hybrid agents interacting with each other via ubiquitous networks. Accordingly, the rapid exchange of specialized information via e-health networks will further promote globalization, integration, and consumer empowerment. In e-health networks, typically dependent consumers can become more central while the health providers who used to be independent controllers are now partners, essentially blurring the lines between specialists and generalists and between health providers and e-consumers that choose to self-care.
Globalization
For the purposes of this text, globalization refers to viewing the world as a single community for propagating the promotion of health and well-being through evolving virtual network and the sharing of e-health information and services. Owing to the many interacting components and agents within such a complex community as suggested by our understanding of “chaos theory,” supersymmetrical thinking makes the transition to “globalization” possible because all of these agents can be “transformed” to behave like a common giant e-health knowledge and information dispensing and exchange system. The aim is to bridge social and cultural gaps by making health services affordable and conveniently available to anyone anytime, anyplace. Here, we are therefore using the word globalization differently from those in the antiglobalization movement, who are concerned about the exploitation of cheap labor forces and the export of jobs as well as the growth of multinational corporations.
Globalization of e-health care will require effective use of individual, group, community, organizational, and societal resources. With the implementation of global call centers and Internet-enabled transactional services, e-health purchasers and providers can significantly streamline many administrative and financial processes, promoting global exchange of data for scheduling, shipping, billing, ordering, and purchasing health care products and services.
Globalization of e-health services also has the potential to provide high-quality services to many underserved urban, rural, and remote areas. Another favorable outcome for e-consumers could be better morbidity and mortality rates, especially for e-consumers who choose e-home care and for those living in remote areas, including developing and underdeveloped countries. Another potential benefit not only for e-consumers but also for all participating e-stakeholders is learning from one another through shared responsibility, information exchange, and governance.
At the moment, only about 20 percent of the world's population receives 80 percent of the costly medical procedures and prescription drugs that advances in science and technology have made available. Globalization promises to close this gap and to extend these new discoveries to the underserved 80 percent. For e-consumers, global e-health networks can provide access to on-line consultations with qualified caregivers twenty-four hours a day, seven days a week; the potential for emergency assistance; and the portability of insurance coverage from one country to another. Other possibilities include e-prescription and e-claim services, instant messaging capabilities, realtime e-health information queries and retrievals, and on-line directory assistance.
Globalization also invokes the ideal of a universal e-health model rather than a competitive one. Currently, competition exists among major players, including venture capitalists, governmental bodies, nongovernmental organizations (NGOs) and multinational corporations. However, in order for the ideals of globalization to be realized, world leaders must be prepared to break down cultural gaps, conflicting views, and political differences among participating countries. Examples of health care initiatives that would be more effective should a global e-health infrastructure be put in place include the AIDS relief movements currently supported by the Gates Foundation, former U.S. president Bill Clinton, and former South African president Nelson Mandela.
Empowerment
Again, our supersymmetrical thinking of transforming the complex global community into one giant pool of an e-health knowledge and information dispensing system will lead to e-health consumer empowerment. Empowerment refers to providing on-line users of e-health systems, including e-consumers and other major e-stakeholders, with self-directed education, allowing them to participate actively in the decisions that affect them and their health. For example, an e-health service can permit prospective members to subscribe to information services; to check the scope of their insurance coverage; to change providers, choose options for coverage, and make premium payments; and to check out new products and services. Similarly, e-providers and e-caregivers can also be empowered via the use of e-health networks to exchange key patient data, to teleconsult, and to interact more frequently with clients, thus improving the quality of patient care.
Another aspect of empowerment is the ability of e-consumers to learn on their own or from one another, accessing current and relevant e-health information resources about treatments and medical procedures available for particular illnesses. Best practices can be easily shared. The increased ability of e-consumers to search, retrieve, store, learn about, and transmit specific health information regarding a certain disease group both for themselves and for others will make an appreciable difference in the management and control of these illnesses. Problems related to management of chronic ailments, such as diabetes and lower back pain, are especially amenable to this approach.
E-consumers can also benefit from being informed of breakthroughs in dealing with public health problems as well as potential symptoms arising from unknown exposures to hazardous bacteria, other dangerous biological agents, or threats due to bioterrorism (for example, anthrax). Medical problems that are on the minds of a growing number of both Americans and Canadians include AIDS/HIV, SARS, West Nile virus, mad cow disease, and avian flu. Many people turn to the Internet and other media for authoritative information about these life-threatening diseases. Knowing as much as possible about the vectors, symptoms, and treatment of these potentially threatening ailments is the best medicine; knowledge is power, and access to information may eventually offer some protection or, when no protection is available, at least the comfort of understanding the scope of the problem.
Integration
Finally, the supersymmetrical transformation will eventually lead to the creation of an integral e-health knowledge and dispensing system and an integration of intelligent agents among humans and machines. Integration is an ideal state, a longer-term goal to strive for as we make the e-health paradigm shift. Integration brings together various subcomponents of e-health care (stakeholders; hardware, software, and interface technology; and processes, tasks, and work designs) to create a practical solution that meets the needs of e-consumers. Integration needs to be achieved from several perspectives, including integration between or among e-stakeholders; integration of e-technologies; and integration of e-health processes and services.
Integration between and among e-stakeholders implies the clarification of their shared vision, mission, values, and goals. Without shared vision, mission, values, and goals, no e-health system or network will be profitable or even sustainable; strategies will be inadequately planned and poorly executed. Regardless of the amount of investment that has been sunk into e-health initiatives, the clarity of vision and goals must be the overriding concern. Achieving integration at the stakeholder level, though not an easy task, is nonetheless a necessary first step. Turf claims among competitors with conflicting visions and goals must be broken down. Turning those competitors into partners requires building trust among major e-stakeholders and nurturing their readiness to act as a unified entity. Integration among stakeholders represents a fusion of the vision, mission, values, and goals (reflecting the neural network metaphor and supersymmetrical thinking).
Integration of e-technologies is the ability to harness different e-technological developments, including network infrastructure, relevant hardware and software, and Web interface design, into a single, flexible, and integrated platform for the delivery of a seamless continuum of care. The Web development language chosen must be both flexible and functional in different computing systems, Web browsers, and search engines. As indicated in earlier chapters, the use of XML to support interactive functions and secured transactions on the Internet is one approach to a common and convenient interface. Other technologies that might be harnessed and integrated include an information grid to organize the piecemeal information captured throughout the Internet, with a language translator facility to extract information captured in different languages, and effective document management systems to ensure fast and effective delivery of information to e-consumers.
The integration of processes and services implies the ability to streamline, combine, and create new administrative, clinical, and financial processes from sometimes disjointed and poorly conceived procedures of legacy systems and to interconnect these functions within the e-health network. Integration also implies the use of advancing multimedia interface technologies so that health professionals can have access to integrated patient records and images, coordinate the scheduling and billing of on-line patient visits, monitor patient conditions intelligently on a remote basis, and provide e-consumers with integrated advising services.
Employing supersymmetrical thinking of ubiquitous exchange of e-health knowledge and information among e-stakeholders, then, our goal is that we should no longer be able to differentiate between e-consumer needs and e-stakeholder policies and procedures; between what customers expect and how providers offer what is expected; and between integrated information flow and user satisfaction with transactional processing. Customer and provider requirements should be simply translated into integrated information flow, a flow that essentially reflects e-health products and services as they are demanded in the e-marketplace. Thus, integration of e-stakeholders, integration of e-technologies, and integration of processes and services ultimately lead to integrated information flow that satisfies joint e-stakeholder requirements. Thus, integration is a crucial component of e-health care leadership and management and essential to the success of the e-health care system model, which represents a transformation of the fragmentary and piecemeal approach inherent in traditionally managed organizations. This brings me to the next topic, sociocultural entities—a move from a hard science to a social science perspective.
Sociocultural Entities
A final framework for our thinking about currently evolving e-health groups and communities (e-communities) is the perspective of virtual global teams and learning communities. Understanding the characteristics of sociocultural entities will enable us to generate meaningful e-health solutions, notably in the context of interrelationships among users of e-groups and e-communities.
E-Communities as Sociocultural Entities
With e-businesses and multinational corporations actively competing on a global scale in today's e-marketplace, global virtual teams are being formed at an unprecedented pace. These teams typically include experts from various countries who meet via e-technologies for the purpose of designing innovative approaches to corporate challenges. Members of these groups may have very few opportunities to meet one another face to face. Cultural differences among them are a key barrier that must be broken down if they are to work together successfully. Moreover, some form of socialization must take place among members of these groups if they are to become productive work partners. Time is needed for group members to get to know one another. Virtual group leaders (leadership may be rotated among the members) must learn how to create reliable working relationships among members of the group. For example, leaders must design tasks and set conditions that are conducive to collaborative learning both before and after the formation of the group.
E-learning cannot be overemphasized on virtual teams. For team members to work collaboratively and learn within a virtual context, their working conditions must be conducive to nurturing critiques, comments, and feedback on one another's work, with guided directives and summaries of discussions from the leaders. When individuals who are not familiar with one another's work habits are placed in a vacuum, they will assume that everyone else has the same sociocultural, economic, and political background, when the opposite is true. Conflicts will abound as perspectives are shared. When virtual teams include people from different sociocultural backgrounds, the context for working together is invariably complex. Over time, as team members exchange views and freely engage in discussions until they feel comfortable with one another's beliefs, cultural viewpoints, and social status, some differences will disappear. In other words, a virtual community will have members from many distinct cultures. Initially, when a person does not know another person's culture, it will not be easy for the two of them to communicate. Nonetheless, the virtual group is able to communicate because all the participants have agreed to use the same language—for example, English—and they are focusing their energy on a common task. When this works, the virtual group will evolve a sociocultural entity of its own that will have a group-defined identity.
Community health information networks (CHINs) that have evolved in recent years parallel the concept of global virtual teams (or e-communities). CHINs are virtual teams that are community-based and involve participants and e-stakeholders within a well-defined geographical region. A CHIN therefore represents a community-based electronic organization: essentially, a regional ring to transmit clinical, financial, and insurance data among not only e-providers and e-payers but also e-claimers (consumers), e-business coalitions, and other e-stakeholders, in order to conduct business transactions or simply to share information. The complexity of the CHIN shadows precisely the complexity of the global virtual teams.
According to Julia Gluesing and Cristina Gibson (2003), the complexity that the global virtual team (or virtual community) faces in meeting its objective can be characterized along several dimensions: task, context, people, time, and technology. We have already noted that time is important in allowing team members to get to know each other and technology is the means by which virtual teams choose to meet and work collaboratively. Hence, the focus of the following discussion will be on task complexity, people, and context.
Task complexity comprises four elements: workflow interdependence, task environment, external coupling, and internal coupling. Workflow interdependence relates to how much the team members are independent of or dependent on one another in completing a certain task. Task environment can vary from static to dynamic; a static environment is easily predictable and stable, whereas a dynamic environment is shifting and uncertain. External coupling refers to how tightly a team is linked to or affected by what goes on in its task environment—that is, tight versus loose coupling. Internal coupling describes how crucial the relationships among team members are to the task at hand and can be described as weak or strong. Team members who are weakly coupled do not have to be integrated with one another in order to accomplish their tasks.
Virtual teams are composed of people. The extent to which people are motivated to participate in the team varies depending on their workload, the degree of organizational support they receive, the level of endorsement from other team members, their own personal interest in the assigned task, and the acceptance of their work from those with whom they are linked within their organization. In global virtual teams, members are often required to perform numerous tasks and take different roles. These multiple demands can create conflicting roles, ambiguous decision making or policy-making, and unclear responsibility.
Single Versus Multiple Contexts
In addition to task characteristics, contextual differences also determine the complexity of global teams. Context is defined as “the way of life and work within a specific geographic setting characterized by its own set of business conditions, cultural assumptions, and unique history.” Essentially, work complexity is determined by the extent to which differences are represented on the team and the number of different contexts team members must negotiate in order to accomplish their tasks. Hence, when team members work in a common context, a single national culture frames their work and they share the same physical conditions, work environment, and sociopolitical framework.
In contrast, virtual global teamwork often must evolve across multiple sociocultural contexts. For this reason, virtual team members must be sensitive to how things appear in varying sociocultural contexts and thus must integrate differing sociocultural perspectives. If high-quality work is to be achieved within this multiplicity of sociocultural contexts, the team must address the following questions:
- Despite differences in opinions and sociocultural background, how can team members work together to make intelligent decisions?
- Which team members should be assigned to and be responsible for what part of the task, and why?
- How can information be integrated from all sources to help team members accomplish the task at hand?
- What would it take for individual team members to be able to see eye to eye with one another? If that is not possible, how can the concerns of team members be resolved?
- What and how can team members learn from one another, and what is the significance of this learning in the context of the task to be completed?
- How can learning from one another lead to a better understanding of the shared sociocultural contexts that will help in designing further tasks for virtual team members?
The world, and more specifically its e-health system, is often understood in terms of subsystem components that, when reconstituted and re-interpreted, give an illusory or mistaken view of the whole. Proliferation of virtual global teams that cut across sociocultural contexts has the potential to reduce or even eliminate this fragmentation. What is important then, is not the differences in opinions among the virtual team members (which represent a fragmented view) but the emergent, acceptable view, the solution that integrates the differing views and perspectives.
Increasingly, we ignore contexts by unwittingly focusing too heavily on gathering data (creating fragmented views) to support individual and isolated arguments. In fact, some virtual team members will be preoccupied with large amounts of data (but perhaps too little information). Such preoccupation with supporting our own biases locks us into stereotyped learning. When we focus on a fragmented view in relation to a single context, we become blind to information shared by other team members who move in other contexts. Consequently, we lose an essential understanding of the whole system or even its parts. Invariably, much team conflict is due to some team members wanting to select and observe information from within a single sociocultural context. To be useful, emergent solutions must be relevant to the understanding of the whole.
Conclusion
Concepts of systems theory, systems thinking, and integration, combined with advances in mathematics and physics such as chaos theory, quantum physics, and string theories, as well as social sciences thinking, all provide us with useful frameworks for deciphering the meanings of e-health. Application of these principles can provide direction and guidance to students, practitioners, and proponents of e-health. The process of system evolution and creation is continual and is built on the ideas of globalization, empowerment of e-stakeholders, and integration of e-stakeholders, e-technologies, and e-processes.
Lindstrom, Matheson, and Tan (1998) argue that few of the health administrative skills we have valued in the past—for example, planning and controlling—will remain important. According to them, controllers, planners, and leaders have overplanned the world into forms that were thought to be wanted and required but that have not succeeded very well. What is needed is more participation and less planning in order to allow an emergent new world to appear.
Thus, transformational health care leadership begins with a transformation of one's thinking. An example of this possibility is an attempt to resolve the problems of AIDS and malnutrition on the African continent via some form of e-technology (see Chapter Eight). Lindstrom, Matheson, and Tan (1998) note that health care leaders and managers, including chief executive officers, chief operating officers, and chief information officers, are facing new challenges during these turbulent times. Indeed, for brick-and-mortar health care organizations to move successfully into the e-health care realm calls for a profound shift in the way health executives and administrators think and do business. Similarly, health care educators need to rethink the way they have been teaching health care concepts, strategies, and planning. I have argued that health care is shifting between two paradigms: from a huge, difficult-to-manage, and traditionally fragmented system to a more unified, holistic, and integrative system based on collaborative partnerships, virtual interactions, and active contributions to a common vision, mission, values, and goals.
In addition to the usual external environmental opportunities and threats (including sociopolitical, economic, cultural, technological, and demographic factors), three major trends will determine the growth and future development of e-health networks: globalization, empowerment, and integration. While this argument has been inferred from time to time throughout the chapter, it is at this point that we consider these issues more thoroughly.
In light of this observation, e-health leaders today should behave more like coaches, facilitators, and team leaders in a virtual global team context. They should break away from stereotyped thinking and learn to transcend disciplinary boundaries in clarifying and focusing the vision and values of the e-health system. They must be prepared to adopt supersymmetrical thinking in order to face more complexity, uncertainty, and ambiguity.
Finally, the dynamic functioning of e-health networks must be understood beyond the use of metaphors and mental models. Key to successful design and implementation of e-health systems will be recognition of the limitations of fragmentary thinking in a single sociocultural context and a correspondingly greater emphasis on the multiplicity of contexts and cultures within which emergent solutions can be achieved. Shifting from thinking and problem solving within a single sociocultural context to a network-based sharing of thoughts within multiple sociocultural contexts will be an ongoing challenge.
Chapter Questions
- Explain why changes in mainstream health care have prompted new ways of thinking about planning and redefinition of business processes in the evolving e-health care system.
- How does supersymmetrical thinking combine various aspects of e-health? What is the significance of supersymmetrical thinking in redefining the roles and responsibilities of e-consumers as opposed to other e-stakeholders?
- Use the rich picture approach to portray an instance of a multiagency e-health system. What are the implications of globalization, empowerment, and integration for e-health systems?
- How does the neural network metaphor apply to evolving sociocultural entities in an e-health system? Can it be applied to an e-community? What is the significance of viewing e-communities as evolving sociocultural entities?
- Illustrate how an e-health system like the MMP project (see the case at the end of the chapter) can be conceived as an organic and self-learning system.
References
Beckham, J. (1993). The architecture of integration. Healthcare Forum Journal 36(5), 59.
Bohm, D. (1980). Wholeness and the implicate order. London: Routledge.
Capra, F. (1996). The web of life: A new scientific understanding of living systems. New York: Bantam Doubleday Dell.
Gluesing, J., & Gibson, C. (2003). Designing and forming global teams. In H. Lane, M. Maznevski, M. Mendenhall, & J. McNett (Eds.), Handbook of global management: A guide to managing complexity, forthcoming, Malden, MA: Blackwell.
Hammad, T. (1998). Computational intelligence: Neural networks methodology for health decision support. In J. Tan & S. Sheps, Health decision support systems (pp.). Sudbury, MA: Jones & Bartlett.
Lindstrom, R., Matheson D., & Tan, J. (1998). Organizational health decision support systems: The application of systems concepts, chaos theory, quantum mechanics, and self-organizing systems. In J. Tan & S. Sheps, Health decision support systems (pp.). Sudbury, MA: Jones & Bartlett.
Morgan, G. (1997). Images of organization. Thousand Oaks, CA: Sage.
Senge, P. (1990). The fifth discipline: The art and practice of the learning organization. New York: Doubleday.
Tan, J. (2001). Health management information systems: Methods and practical applications (2nd ed.). Sudbury, MA: Jones & Bartlett.
Wheatley, M., & Kellner-Rogers, M. (1995). “Self-organizing systems conference.” Sundance, Utah.
Multicommunity E-Health Promotion Programming Case
Joseph Tan
In Detroit, the Maria-Madeline Project, Inc. (MMP) provides e-technology training for seniors: young adults teach seniors how to use computers in nursing homes, assisted living facilities, retirement communities, senior apartment complexes, and community centers. The goal of the MMP is to provide developmentally appropriate informational e-health interventions for urban, at-risk populations. To that end, the program staff plans to develop, implement, and evaluate interactive, Web-based informational and expert consultation sites.
The MMP can be viewed as a complex system composed of many interacting agents (for example, seniors, school children, stakeholders who fund the project, e-health care providers and on-line professional consultants, evaluators such as university professors, and others) with diverging perspectives and decisions. The resulting behavior of this complex system is difficult to predict; yet the social and cultural exchanges amongst these various parties follow predetermined or predictable patterns depending on the relationships and partnerships that are built over time. Where string theory and supersymmetrical thinking apply is the partnership among the seniors and school children in the use of advancing telecommunication and network technologies to allow these seniors to absorb the free-flowing e-health information and knowledge provided through the on-line consultations with the experts to the point that they become confident of their own use of this dispensed knowledge.
Background
The United States in general and cities such as Detroit in particular face a formidable challenge in delivering and promoting health services efficiently and equitably in the face of competing resource demands from sources that include bioterrorism and homeland security, natural calamities, environmental concerns and global warming effects, K–12 education and higher learning, and, on the federal level, international relations and foreign affairs. During this era of shrinking resources paired with information and knowledge explosion, several major federal and national initiatives indicate that government agencies, health care providers, and consumers expect information technology, particularly e-technology and Web-based services, to contribute to meeting this challenge. People are looking to information technology to facilitate increased clinical expert consultations, rapid health information access, equity in health care delivery, and increased comprehensiveness and accountability of health care services through security and policy regulations. One theme permeating many recent conferences sponsored by major health care agencies has been the development of an e-health technology infrastructure.
With continued and increasing use of on-line health services, the question arises as to whether the on-line environment will provide effective health care services to urban at-risk populations. One mental model of e-health programming suggests that the Internet can be a convenient environment for senior patients who wish to obtain health information. The MMP asks important questions of both students and seniors to yield insights into the truth of this model.
The Maria-Madeline Project, Inc. (www.mariamadeline.com) began in 1999 to serve nine facilities of the Archdiocese of Detroit. There are now a total of thirteen centers in metropolitan Detroit, plus a growing number of facilities in Texas and New York. In addition, the MMP recently secured funding to work jointly with the Society of St. Vincent de Paul to further expand services. The MMP integrates technology into the lives of elementary and high school children and links them to senior citizens through a unique methodology called ExperienceSeniorPower®. Dell Computer Corporation is collaborating with the MMP, providing computers to all ExperienceSeniorPower locations at a significant discount. The MMP also works with Wayne State University School of Business researchers to better understand how seniors can be encouraged to change their health behaviors and lifestyles through the use of customized Web-based programming.
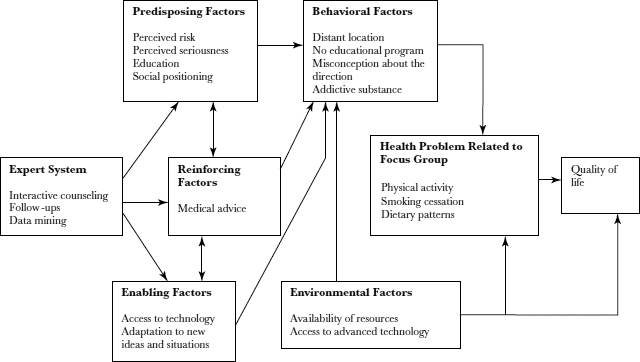
The Precede-Proceed Framework
We use the Green-Kreuter precede-proceed framework (Green and Kreuter, 1991) to guide our understanding in planning and evaluating this project. The overriding principle of this framework is that most enduring health behavior change is voluntary. This principle drives a systematic planning process that seeks to empower individuals with understanding, motivation, skills, and active engagement in community affairs. Thus, this model is applicable and practically helpful in the project planning, development, implementation, and evaluation stages of the MMP. These are nine phases of the precede-proceed model.
The first five phases of the precede-proceed model are diagnostic:
- Social diagnosis of the self-determined needs, wants, resources, and barriers to fulfilling the needs and wants in the target community
- Epidemiological diagnosis of the health problems
- Behavioral and environmental diagnosis to determine specific behaviors and environmental factors for the program to address
- Educational and organizational diagnosis of the predisposing, enabling, and reinforcing conditions that immediately affect behavior
- Administrative and policy diagnosis of the resources needed and available in the organization, as well as the barriers and supports available in the organization and community
The left-to-right arrows indicate the impact that educational and environmental interventions can have on problem areas at each level. The process consists of systematic identification of health problems and their behavioral and environmental antecedents and the development of educational interventions aimed at those antecedents as well as at the problems themselves. The step-by-step process of the model, from the identification of social problems and their etiology to the implementation of appropriate community-based interventions, flows logically from the assessment findings and serves as a basis for community health promotion.
The four remaining phases relate to implementation and evaluation, with emphasis on using the latter to improve the former. Evaluation begins as soon as implementation does, in order to detect problems early so that they can be corrected. As implementation proceeds, the planner starts evaluating in the order in which program effects are expected. First, its immediate effects (impacts) are evaluated, in order to determine the extent to which the program needs modification. Finally, when enough time has passed, as specified in the objectives, the ultimate intended and actual effects on morbidity, mortality, and quality of life are assessed. This phased evaluation allows the project planners to see what works and what does not.
According to the precede-proceed model, Web-based informational programs to provide developmentally appropriate e-health-promoting interventions for urban, at-risk populations can only be effective if they also influence the precursors to behaviors (or the environments in which they occur), including (1) predisposing factors (factors that provide the motivation or reason behind a behavior—for example, knowledge, attitudes, cultural beliefs, and readiness to change); (2) enabling factors (factors that make it possible for a motivation to be realized—for example, available resources, supportive policies, assistance, and services); and (3) reinforcing factors (factors that come into play after a behavior has begun and that provide continuing rewards or incentives and contribute to repetition or persistence of behaviors—for example, social support, praise, reassurance, and symptom relief). Exhibit 3.1 shows our adaptation of the precede-proceed framework for the development of a state-of-the-art Web-based educational system for promoting changes in the healthy lifestyles of urban at-risk populations.
EXHIBIT 3.1. PRECEDE-PROCEED MODEL APPLIED TO E-HEALTH INTERVENTION
The precede-proceed framework is a comprehensive planning and evaluation system based on the needs of the people or community to be served. It starts with extensive research and analysis to assess those needs, then plans the steps that will meet them or eliminate them. It deals with the individuals to be served (in our case, the underserved seniors) and with others who have resources or influence on them, including intermediaries and partners such as community leaders, media decision makers, parents, peers, teachers, and health professionals.
Computers and Internet Use Among Seniors
Here, a key question is: “Does MMP promote better health because of access to computers?” To answer this question, we look at the literature regarding computer use and its impact on changing health behaviors. Bernard L. Bloom (1996) found that computer technology is playing an increasingly important role in personality and behavioral assessment, diagnostic interviewing and history taking, health education, mental health consultation, and clinical training. In these areas, the reliability, validity, and utility of computers compare favorably with those of clinicians. Evaluations of the computer use with psychiatric patients conclude that even those who are quite disturbed interact very successfully with computers, including many patients who are unable to interact with mental health personnel. Computer-assisted psychotherapy programs have been most successfully implemented in cognitive and behavioral psychotherapy. In the case of psychodynamic psychotherapy, computer programs appear to be limited by our failure to make fully explicit the rules governing therapist behavior and by the continuing inability of computers to comprehend natural language.
Once the initial cost and effort have been invested in their development, computerized teaching programs can be cost-efficient. Computer-mediated communications and computer-assisted instructional programs have been shown to “cost-effectively enhance patient outcomes, quality, satisfaction, [and] be used as part of large-scale prevention and educational efforts” (Budman, 2000). These tools can be easily accessible, time-efficient, and instructionally consistent, providing effective modes of instructional delivery (Peterson, 1996). Computer educational programs also help to increase users' attention to the material, perhaps because they are interactive in nature and people can remember better doing the interactions than just passively listening to a lecture. These programs allow users to progress at their own learning pace, maximizing the technology's potential as a self-help health education medium. Finally, they help users assume responsibility for their own learning (Paperny, 1997; Barber, 1990; Bixler and Askov, 1994).
Prochaska, DiClemente, Velicer, and Rossi (1993) used a computer program to individualize self-help materials for community-based adult smokers, although participants did not actually interact with a computer. A questionnaire was administered to determine subjects' readiness to change their smoking behavior, and then they were randomly assigned to one of four study groups. Compared with subjects in the group that received standardized manuals, subjects in the three other groups who were given various forms of summarized versus detailed computerized information and with or without repeated follow-up, regardless of their readiness to change, had significantly higher quit rates after six months and after twelve months. This indicates that detailed information and repeated follow-up was the most helpful in changing smoking behaviors. Schneider, Schwartz, and Fast (1995) developed a computerized, telephone-based, interactive smoking cessation program, using a toll-free call to activate the system. The system automatically composed messages to fit the needs, expectations, and progress of callers on a twenty-four-hour basis. Results indicate that 35.1 percent of users quit smoking while using the program and 14 percent were still not smoking six months after their first call. Of those who called five or more times, 68 percent reported quitting and 22 percent were abstinent six months after their first call.
McDaniel and others (2002) developed and conducted usability testing of an interactive computer program designed to promote smoking cessation in low-income women. Participants comprised one hundred women who received care at an innercity community health center in Indianapolis. After baseline data were collected, the subjects completed the computer program in the clinic. Next, they completed a brief satisfaction instrument. Data indicated that satisfaction with the program was high (mean satisfaction score was 60.2 on a scale in which 70 indicated highest possible satisfaction). Average time required to complete the computer program was 13.6 minutes. In a follow-up survey, 79 percent of participants reported at least one behavioral change related to smoking. Results indicated that interactive computer technology might be useful for promoting smoking cessation in low-income women. Clearly, research is needed on the use of this mode of intervention not only for smoking cessation but also for other health-promoting activities.
MMP Evaluation Plan
The evaluation plan is the most important aspect of the MMP. The design of the project includes collection of data from participating seniors over a period of interactions. Data are collected both on their learning to use the Internet and on any self-directed attempts to extract resources from the MMP Web site. Although eating habits are an important aspect of the MMP, other e-health promotion activities and intervention developments are also being considered. In fact, the Web site currently allows seniors to ask questions of a nurse, a dietitian, and a dentist. The idea is to promote as many health-promoting behaviors as possible, including physical movement (such as walking), smoking cessation, and dental care. A questionnaire also obtains data directly from participating seniors on their training, satisfaction, and other impacts of the technology. The development of a questionnaire designed to extract these self-reported data for the purpose of determining the appropriate programming mix involves understanding different areas affecting the training process, the frequency of use of the MMP system for e-health purposes as opposed to other purposes, and how to define levels of satisfaction with the technology involved—that is, the Internet and Web browsers.
The data gleaned from this project are expected to be complex due to the varying e-health promotion activities involved (physical exercise, smoking cessation, dietary patterns, dental health, and so on). Efficient analysis, modeling, and evaluation of such a multidimensional data set in order to obtain useful, yet often subtle knowledge is a challenging task. Making health trend predictions is appealing but also challenging. Those involved in the project expect that analysis and assessment of the information will yield results that are particularly useful for promoting the health of urban, at-risk populations. We hope to find important yet somewhat latent factors associated with health risks and to evaluate lifestyles in order to accurately identify future health risks for individuals or groups. Based on such findings, we can alert these individuals (or groups) about unhealthy factors in their daily routines so that they will be better able to avoid risks.
Conclusion
The at-risk populations in the Detroit metropolitan area are multiethnic, multiracial, and multicultural. Each section of the city has different percentages of African Americans and whites represented in their respective populations. Arab Americans, Hispanic Americans, Asian Americans, and Native Americans make up a small percentage of the population in the metropolitan Detroit area.
The MMP project serves seniors from a variety of ethnic groups, all of low to middle socioeconomic status. This project may be conceived as the creation of a complex network that nurtures e-health promotional learning; the generation of a new sociocultural entity involving the interactions of students, seniors, and other key stakeholders; and the formation of an experimental learning community. Different e-stakeholders, including community leaders, grant agencies, government agencies, supporting religious organizations, children from the schools, and researchers from the university participate in this network. Central to this network are the participating seniors and students.
Key questions to be answered about the implementation and evaluation of the MMP include the following:
- What are the effective content themes for implementing an appropriate e-health promotion program such as the MMP?
- How effective is the use of an e-health promotional network for urban at-risk populations, specifically those served by the MMP, in terms of changes in healthy lifestyle awareness, attitudes, knowledge, and beliefs?
- What challenges are faced in diffusing the MMP, especially to seniors that live outside Detroit?
- How does MMP contribute to the globalization, integration and empowerment concepts discussed in the chapter?
While we expect results of the MMP evaluation to provide evidence that supports the use of the Internet and intergenerational programming in e-health initiatives, we may find that the seniors have not been empowered and have not benefited, perhaps due to inadequate planning, design, development, or even testing of the network. Moreover, the participants may not find e-learning an acceptable method of instruction. Conversely, we may find that the MMP brings about a positive relationship and a transformational perception among seniors and student groups. Also, other seniors may be brought into the learning community, so that learning among seniors comes not only from intergenerational programming but also from electronic connections with other seniors outside of Detroit. Awareness, attitudes, knowledge, and beliefs about e-health promotion activities may change due to new opportunities for the participants or the evolution of a strong learning community. In addition, the information resources accessible through the Web may empower seniors and further transform their lifestyles and daily routines. At this point, all of these outcomes are purely speculative. Hence, the emerging impacts of ongoing interactions between students and seniors, as well as among the seniors themselves, are worth examining. Moreover, the learning that emerges within the virtual senior group may be characterized by the sociocultural sharing of views. In the larger context of the e-health care system, we may expect this learning to be guided by the vision and values of the e-health network—that is, the vision as provided by the MMP.
Finally, the vision for the MMP project continues to evolve, expanding to include senior groups interacting with student groups across the nation. Current discussion includes ideas for generating an artificial intelligence–based programming prototype that would support e-health programming over the life span of the seniors being served. The activities to be facilitated can include physical exercise, management of common diseases such as diabetes, and pain management. If and when this happens, it will be interesting to mine the data on the use of new and powerful e-technologies to understand how an underserved population can truly be empowered to alter the quality of members' lives.
Case Questions
- What aspects and features of the MMP qualify it as part of the e-health care system?
- Why would the MMP appeal to seniors? What types of e-health services are most likely to appeal to seniors?
- How would you go about determining the content for the e-health promotion programming in the MMP project?
- Do you agree that students should be used to teach seniors how to use the Internet? Why or why not?
- Think about the future growth and development of the MMP. What are the most significant next steps, challenges, and critical success factors in expanding the MMP within Detroit and Michigan? How does the MMP community mirror the social cultural entities as detailed in the chapter?
References
Barber, J. (1990). Computer-assisted drug prevention. Journal of Substance Abuse Treatment, 7, 125–131.
Bixler, B., & Askov, E. (1994). Characteristics of effective instructional technology. Mosaic: Research Notes on Literacy, 4(1), 7.
Bloom, B. L., & Berki, S. E. (eds.). (1996). Cost benefit, cost effectiveness, and other decision-making techniques in health care resource allocation (p. 87). New York: Biomedical Information.
Budman, S. (2000, November). Behavioral health care dot-com and beyond: Computer-mediated communications in mental health and substance abuse treatment. American Pyschologist, pp. 1290–1300.
Green, L. W., & Kreuter, M. W. (1991). Health promotion planning: An educational and environmental approach (2d ed.). Mountain View, CA: Mayfield Publishing.
McDaniel, A., Hutchison, S., Casper, G., Ford, R., Stratton, R., & Rembush, M. (2002). Usability testing and outcomes of an interactive computer program to promote smoking cessation in low income women. In Proceedings of the AMIA Symposium (pp. 509–513). American Medical Informatics Association, Washington, DC.
Paperny, D. (1997). Computerized health assessment and education for adolescent HIV and STD prevention in health care settings and schools. Health Education and Behavior, 24(1), 54–70.
Peterson, M. (1996). What are blood counts? A computer-assisted program for pediatric patients. Pediatric Nursing, 22, 21–27.
Prochaska, J., DiClemente, C., Velicer, W., & Rossi, J. (1993). Standardized, individualized, interactive, and personalized self-help programs for smoking cessation. Health Psychology, 12(5), 399–405.
Schneider, S., Schwartz, M., & Fast, J. (1995). Computerized, telephone-based health promotion: I. Smoking cessation program. Computers in Human Behavior, 11(1), 135–148.
I acknowledge the contributions of my colleagues from the School of Nursing at Wayne State University, especially Mary Nies, Rosalind Peters, and Linda Weglicki for their input and feedback on the Green-Kreuter diagram discussed in this case as well as Tim Butler and Alexandra DePetro for their contributions to generating a survey instrument for use in this project.