![]()
CHAPTER ONE
E-HEALTH
The Next Health Care Frontier
Joseph Tan
III. Foundations and Benefits of E-Health
A. Basic Components of an E-Health System
B. E-Health Core Value Propositions
IV. E-Health Domains and Applications
B. Domains of E-Health Applications
V. E-Health Strategies and Impacts
A. Planning E-Health Strategies
B. E-Health Implementation and Evaluation Issues
Learning Objectives
- Articulate the emergence of revolutionary thinking in the e-health paradigm, business models, and practices
- Identify basic components of an e-health care system
- Recognize the underlying value propositions of an e-health care system
- Understand the history of computing in health care and recognize how this process relates to the evolution of the e-health paradigm
- Organize the range of current and emerging e-health care applications according to whether they require a high degree of internal integration or a high degree of external integration
- Understand the scope of e-health care strategies and impacts
Introduction
The application and use of machines and computer-based technologies in health care have undergone an evolutionary process. Advances in information, telecommunication, and network technologies have led to the emergence of a revolutionary new paradigm for health care that some refer to as e-health. New experience and knowledge that crosses traditional disciplinary boundaries—particularly cross-disciplinary and multidisciplinary research in the fields of information technology and health care, along with emerging knowledge to promote evidence-based medicine (evidence-based medicine is discussed in the Case section of Chapter Thirteen), e-medicine, and remote e-health services—are causing not just episodic but systemic transformation of traditional health care systems and environments. Applications of electronic commerce (e-commerce) and electronic business (e-business) concepts to health care have resulted in efforts to use the availability of low-cost, high-speed Internet-related or wireless technology to revolutionize the health care business.
Health care administrators, clinicians, researchers, vendors, purchasers, and other health practitioners are facing increasing pressure to adapt to growing expectations for accountability from both the public and the private sector (see Chapter Sixteen). Major sources of this pressure include decreased government and third-party funding; increased patient education, participation, and expectations; and new and emerging forms of health organization reporting structures as well as breakthroughs in telecommunication and networking technologies. The simultaneous need for and technological opportunity to create more efficient, effective, secure, and economical health data sharing; large-scale health information processing; better and more effective communications; and seamlessly coordinated health knowledge management, data mining, and evidence-based health decision making demands a concerted effort to harness the power of e-technologies in the service of health care.
Those who understand electronic health (e-health) perspectives, domains, and challenges, as well as the potential benefits of e-health applications will be better prepared to work collaboratively through the use of computer-based groupware, virtual networks, and Internet appliances. E-health understanding will increase health awareness, improve decision-making effectiveness, cultivate more positive consumer-provider relationships, and enhance the partnership of e-health care product and service delivery networks. In addition, rapid shifts in the e-health market and environment also dictate a growing need for improved ergonomics and more intelligent interfaces in e-public health data systems and e-decision support applications and implementations.
E-health can be viewed as an integrated, multidisciplinary field, bridging the following key areas:
- Strategic health systems planning and e-marketing concepts
- Specialized e-record keeping and e-business operational analysis
- All forms of e-medicine linking health professionals to individuals
- Corporate and enterprisewide health technology management
E-technologies encompass the following:
- Complex information technology network design and methodologies for consumer-oriented system development
- E-health informatics (information sciences and methodologies)
- Wireless communications and emerging technological applications
- Web services implementation
- Ongoing evaluation of automated security of Web-based health information exchange
- Clinical monitoring and management systems
Three general topics characterize the eclectic field of e-health: (1) e-health foundations and benefits; (2) e-health domains and applications; and (3) e-health strategies and impacts.
Before discussing the e-health foundations and benefits, I will first attempt to answer a very basic question: “Can e-health help solve North America's health care crisis, particularly in terms of key challenges such as escalating health care costs, access for the underserved, and improving (or even maintaining) the quality of current health care service delivery?” Answers to parts of this question have remained unclear; e-health has sometimes been described as hype that may not make any appreciable difference in resolving current challenges. Thus, continuing investments and efforts that encourage investors, vendors, and purchasers to pursue e-health initiatives may well be limited by the lack of coordinated effort to unlock the potential benefits and powerful promise of the e-health paradigm shift (e-health paradigm shift is more fully explored in the beginning of Chapter Two). Essentially, the underlying argument is such that if we cannot diffuse medical and health care data, information, knowledge, and expertise from the e-providers and experts to the e-consumers so that we empower them to new heights of health and well-being rather than perpetuate their relentless dependence on care providers to cure their everyday problems, e-health investment will be fruitless. Until a few years ago, the thought of e-consumer empowerment from health information therapies was still a remote, far-fetched possibility. How could consumers have more current and detailed medical information on hand about their own illness or predicaments than their family physicians? Perhaps our question should be “Has the time come for us to move e-health knowledge and practice from being largely hype to being a new and respectable field?”
Understanding the values and benefits of investing in the e-health field is therefore critical to the future success of e-health initiatives. In the next section, we discuss e-health perspectives, infrastructures, components, and services and relate these concepts to core e-health value propositions by focusing on how core e-health values can benefit e-health's investors as well as its users, enhancing or supporting complex e-health technologies and applications.
Later, we survey and highlight major aspects of e-health domains and applications. Specifically, we review e-health history to show how emerging domains of e-health applications are derived from our understanding of health management information systems (HMIS), health decision support systems (HDSS), health informatics, and e-medicine (also called telemedicine). Following this, we organize e-health application clusters, dividing domains and applications that provide seamless internal system process integration from domains and applications that provide external linkages with e-stakeholders and the public. Finally, we shift the discussion to the significance of e-health strategies and impacts and conclude the chapter by examining how these various topics can be combined to achieve an effective understanding of the e-health field and provide the basis for considering how e-health practices in the coming era may be affected by changing e-consumer needs, trends, and expectations.
FOUNDATIONS AND BENEFITS OF E-HEALTH
To grasp the fundamentals of e-health technology, it is necessary to recognize its diverse perspectives, as well as its basic infrastructures and components. Part Two of this book is devoted to the details of the foundations of e-health and covers various theoretical perspectives of the e-health paradigm as well as concentrates on the different network infrastructures that make e-health care delivery systems possible. In this chapter, we emphasize basic e-health components, including the core value propositions and the basic characteristics of the e-commerce services as applied to e-health care (for example, business-to-consumer [B2C] and business-to-business [B2B] e-health models), the e-stakeholders, and future e-health impacts. Without these basic components, the e-health paradigm shift would never have been possible and patients would always have to travel to their doctors instead of having the best health care information sources transported to their fingertips.
In fact, the e-health paradigm shift did not begin with the linking of e-consumers to the e-care providers; instead, its current success has been largely the result of linking one health care business to another, increasing efficiencies and eliminating the need for manual administrative information exchange and off-line business transactions. We therefore begin by discussing electronic data interchange (EDI) methods used in typical B2B e-commerce applications in health care and then move to examine the design of Web sites using HTML versus XML standards to provide e-consumers with specific or specialized health information and dynamic electronic data interchange capabilities.
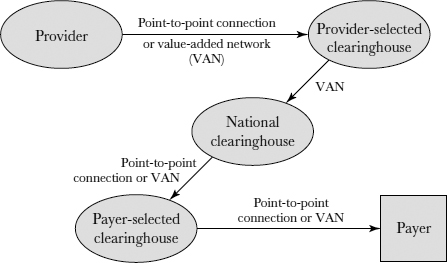
Since the advent of e-commerce, EDI has offered companies a largely automated way to conduct business transactions. Business processes that once required significant human intervention are now being done efficiently and effortlessly with little or no human interaction required. EDI, the standard method for conducting B2B e-commerce applications, is therefore considered the traditional basic infrastructure for electronic data sharing and transaction activities among e-stakeholders—for example, between a health provider and a payer. The best way to understand EDI processing is to divide the flow of data into several phases in the context of a provider-payer transaction, as depicted in Figure 1.1.
As shown, the provider sends data about services and care rendered to a selected clearinghouse by either using a value-added network (VAN) as an intermediary or using point-to-point (P2P) connectivity.
FIGURE 1.1. ELECTRONIC DATA INTERCHANGE TECHNOLOGY
A VAN essentially functions as a post office for EDI transactions. Users are assigned “mailboxes” that store their data. Each mailbox is given a unique identity (ID) or communication code, accompanied by a qualifier. Together, the ID and qualifier serve as an address to which data can be mapped. Once the data arrive at the clearinghouse, they are translated and reformatted to the payer's specifications. Many clearinghouses make it possible to check the validity and completeness of the document. From the provider's clearinghouse, data are then sent to the national clearinghouse via VAN. In essence, a clearinghouse provides connectivity between health care providers (physicians, hospitals, pharmacies, and clinics) and payers (health maintenance organizations, insurers, and government entities such as Medicare). Clearinghouses take claims, eligibility requests, claim status checks, and other information from providers in various formats, translate and reformat them according to the pre-specified or standardized formats demanded by payers, and transmit the reformatted versions to their destination. As an additional service, the clearinghouses may perform editing functions that check the claims.
At the national clearinghouse, data are further cleansed, and precautions are taken to ensure that the security, privacy, and confidentiality of the data set are kept intact. The data are then received at the payer-selected clearinghouse via a VAN or P2P connection. Then, data are again translated and reformatted before being sent to the payer via a P2P connection or VAN. With P2P connection, all of the data interchange and formatting activities discussed with the use of a VAN are preplanned and data transmission is performed through a secured channel.
If the data exchange process simply provides static health information from health information systems and legacy databases, then the information dissemination process is straightforward. In this case, the Internet and the typical HTML (Hypertext Markup Language) offer a convenient platform via which the information can be predesigned, validated, and captured or presented as a user-friendly multimedia document as with a P2P connection. To improve the data's timeliness, validity, and integrity, the preferred data collection method is automated and direct data input at the source—for example, using predesigned documents stored in organizational intranets or extranets, then warehousing the completed documents either centrally or via on-line distributed network technology. Data direct entry requires that the acquired data be converted into easily readable and appealing user-oriented information.
While most current documents on the Web are stored and transmitted in HTML because it is easy to use and generate, the need for dynamic and interactive Web interfaces as opposed to static ones resulted in the World Wide Web Consortium's introduction of a new standard known as XML (eXtensible Markup Language). With XML, data or even documents can be simultaneously transformed into useful, meaningful, and interactive information in a format that is readily retrievable, comparable and transactional, where data can be used for exchanging dialogues and executing monetary payments. The data transfer and data distribution functions (that is, data retrieval and transmission activities) become integrated with those of presentation, exchange, and use. A key problem with HTML data display is its inability to provide information by transaction and querying capability for users as well as its inability to convert e-commerce data into e-business information that can be further used in transactions. In contrast, XML technology allows the creation of multimedia and intelligent graphical Web interfaces and thus has the ability to compact large amounts of information conveniently. The information can be further packaged to support individual users by filtering out information that may not be needed for a particular application or for a particular data exchange transaction. For example, on an HTML Web site where an e-consumer may be looking for a quick answer to a question about the extent of her individual health insurance coverage, the presented information may only be tabulated. However, with an XML Web site, the e-consumer can ask the question via e-mail in an open format (that is, no special format is needed for the query to be understood and processed) and receive a direct answer within twenty-four hours through the secured Web site. On the same site, a direct transaction may be executed within a short processing time. Quality displays and functionality of Web-based e-health services are important because e-consumers are more likely to visit and use a Web site if it is dynamic rather than static.
Three common forms of data management technology can support Web-based information processing and management for data-centered and, to a lesser degree, for document-centered Web sites.
- Database management technology
- Model-base management technology
- Knowledge-base management technology
Database management enhances data collection and data storage activities, improves data integrity, reduces data update anomalies to ensure data consistency (see Tan, 2001), and promotes preservation and structuring of data for efficient data processing and effective data retrieval activities. Model-base management constructs, stores, manages, and interrelates models that may be needed by the user to make sense of the data being linked, analyzed, or computed. In fact, not all data collected are directly useful in the e-health care delivery or e-health information dissemination process. Some e-health information (including data elements and models) is collected merely to assist in the organization and generation of comparative data and statistics or simply for research purposes such as adding to the collection of data models and extending their applications.
More intelligent e-health data systems can assist e-health care providers and e-consumers in making complex decisions that may require provider-consumer interactions or teleconsultation (or e-consultation) in specialty areas. In this case, apart from the use of database and model-base management technologies, knowledge-base management systems come into play. Knowledge-base management assembles, stores, accesses, updates, and disseminates knowledge elements that may enhance specialized decisional processes. Regardless of the way e-health-related data are gathered, encoded, and entered as data or documents into a Web-based system, the information captured should be cleaned and meticulously verified for accuracy and validity. Put simply, bad data yield bad results, regardless of the sophistication of the systems that process them.
Basic Components of an E-Health System
The basic function of an e-health system is to gather and exchange appropriate and accurate data from various sources to satisfy the administrative, clinical, and transactional needs of e-health providers, payers, and users. Proposing an e-health business is not exactly the same as proposing a brick-and-mortar health business, and it is vital to understand the factors and barriers that determine e-health business success or failure. The fundamental components of an e-health system include
- Its core value propositions
- The characteristics of the e-health service model
- The community of e-stakeholders involved
- The potential to process a critical mass of transactions, to ensure enough revenue for sustainability and e-commercialization, that is, the potential for e-business ideas and models to thrive in a free online market system.
- The potential to accommodate future features such as product or service expansion, profitability, growth, and global development
First, understanding an e-health system's current value propositions is critical. Value propositions are the added values or quantifiable cost savings, efficiencies, or intangible benefits that can be achieved through implementation of a system. To evaluate these propositions, the observer needs to know the characteristics of the e-health service model—for example, whether the e-health business is to be set up as a completely virtual B2C or B2B enterprise or a more complex hybrid of brick-and-mortar and point-and-click models (called a brick-and-point model) in which the consumer can choose whether to get the service on-line or physically go to a designated service facility.
The community of e-stakeholders comprises the e-providers, e-payers, e-consumers, e-vendors, and e-purchasers connected to the system. It is important to know what each of these players see as the values that the e-health service model provides for them; all stakeholder groups will play by different rules.
The potential for a critical mass of transactions to be processed is significant because the number of transactions determines the amount of capital investment needed to implement the model and sustainability of the e-business model. The central business proposition boils down to the anticipated amount of dollar transactions generated from e-consumers or between the trading partners in a day versus the daily costs of maintaining the service. If there is no critical mass of transactions, there is no profit leading to e-commercialization.
Finally, the business potential to accommodate future features indicates potential future investment returns such as the potential for spin-off businesses that can take advantage of the operation of the current system. For example, a model that mimics Amazon.com or eBay by selling medical devices on the Web could have expansionary possibilities such as collaboration with other health equipment suppliers to resell used medical devices or recycling of expensive hospital-based medical technologies such as CT (computed tomography) scan and MRI (magnetic resonance imaging) equipment.
Careful consideration of each of these components is particularly important when proposing a new e-health business model. For instance, an e-health Web site that provides very specialized information on a specific illness such as ADD (attention deficit disorder) would not be likely to last very long. In fact, such a proposal could be very costly because it would most likely have only a limited number of users; the Web site might be completely static, with no interactive querying capacity; and more than a few hundred, even thousands, of competing Web sites might provide the same or better information, along with other valuable and useful functions. Many contemporary e-health Web sites allow the user to link to authoritative e-health providers or are supported by a major brick-and-mortar pharmaceutical chain and/or are sometimes endorsed by well-known professional associations. Successful Web sites will offer a unique mix of services and attract hundreds or even thousands of visitors daily.
E-Health Core Value Propositions
Both the United States and Canada face rapidly increasing health care costs. Health care expenditures in the United States now exceed 14 percent of the country's gross national product (GNP), which implies that Americans spend roughly $2 billion a day on health care products and services. Yet despite these large expenditures on health care, millions of Americans are denied access to medical care because they lack medical insurance coverage. In Canada, where the majority of health care funding comes from the government, citizens and residents are experiencing long waits and bed closures due to shortages of nurses, family physicians, and various health specialists.
Fortunately, the e-health paradigm shift has been supported by core value propositions that can help alleviate some of these problems by reducing costs and increasing efficiencies of processes in several areas. For example, e-health database management and on-line submission and processing of medical claims can vastly reduce the need for clerical personnel. In addition, on-line processing will eliminate many unnecessary clerical errors due to faulty transcription; the need to satisfy repeated requests on status of claim processing; and submissions of identical patient information for different interventions, as well as the failure to simultaneously update redundantly maintained patient records in various physical files located in different places (update anomalies).
Virtual patient records (VPR) is an integrated health database processing engine that links the accurate and rapid collection of various patient-related information and knowledge elements to generate an aggregated, well-classified, and organized set of administrative and clinical information and knowledge that e-health providers (primarily nurses and clinicians) can retrieve, exchange, and disseminate as needed for e-clinical decision making, e-control, analysis, e-diagnosis, e-treatment planning and evaluation, and many other e-health-related cognitive activities.
Another core value proposition of most e-health domains and applications is improving two-way or multiple-party communications, thereby significantly improving access to e-health care, especially for those located in rural or remote areas. For example, technologies such as e-mail, Blackberries (wireless devices with organizer features providing access to email, corporate data, phone, and the Web ), secured Internet Web sites, personal data assistants (PDAs), virtual private networks (VPNs) and wireless cellular phones can enhance long-distance communications among e-health professionals or between e-health professionals and e-patients in different sectors, including communications between e-physicians and e-patients, laboratory test clinics and doctors, e-consumers and e-home care workers, e-physicians and e-pharmacists for verification of on-line prescription orders, and e-generalists and e-specialists for e-consultations on various subjects.
An additional core value proposition often cited as a rationale for adopting an e-health paradigm is user empowerment through tele-education and e-learning. Videoconferencing and on-line health learning and Web-based educational technologies, for instance, may assist long-distance medical training and permit tele-educational and multimedia educational dialogues among doctors, nurses, mental health and other specialists, and residents. The same videoconferencing and associated Web-based Internet training technology may be used for long-distance radiological consultations, remote medical consultations among doctors and specialists, and e-consultations by qualified doctors on emergency treatments that must be carried out by paramedics. Other e-health initiatives for tele-education and e-learning include on-line kiosks to provide software games and instructional materials for consumer education. Such e-health preventive initiatives, promoted to an entire population, can lead to huge cost savings in health care in the long run.
Benefits from the use of e-technologies in health care services should not be limited to direct patient care; in fact, use of these emerging technologies to improve health care communications and reduce costs may also result in greater user satisfaction. New approaches to the same old routines may improve the quality of health care services, while unnecessary inefficiencies and undesired bottlenecks in the traditional system are eliminated or minimized. Clinicians and doctors, for example, may find it more convenient to receive clinical test results on-line or via EDI, appropriately filed into the respective e-patient records. E-consumers or e-patients may be delighted to be able to connect directly with doctors, nurses, or other health professionals without having to travel a long distance, only to be told, perhaps, that their test results have yet to be received or validated. Both providers and consumers will also benefit from having the confidence that insurers are efficiently reimbursing co-payments or services that they have claimed on-line. The reimbursements can easily be posted directly into recipients' bank accounts rather than delayed for reasons ranging from missing information on physical claim forms to postal strikes.
Aside from e-data management capabilities, improved communications, and tele-education, other core e-health value propositions include knowledge dissemination, intelligent support, better health decision making, and improved personal and community well-being. The use of the Internet, as well as intranets and extranets, to promote community learning and e-learning communities (e-communities), to increase virtual interactions between e-health experts and non-experts within a virtual health network environment, and to build partnerships among community and health care leaders can improve health service delivery. In addition, more effective implementations and uses of emerging e-technologies such as specialized Web services for intelligent health decision analysis and support—for example, helping an employer or employee choose among competing insurers and health maintenance organizations (HMOs)—can be of great benefit.
Evidently, the core value propositions underlying e-health can make critical and significant contributions to reduced health care costs, improved access to health care, and even enhanced quality of the health care workplace and environment. Thus, e-health domains and applications, properly structured, can greatly benefit individuals, groups, organizations, communities, societies, and populations. Still, the question remains as to what the best next steps are and who should lead the effort to mobilize human and other resources to transform e-health from hype or a concept found only in textbooks and conference papers into a set of successful real-world e-business practices and documented cases.
E-Health Domains and Applications
Everyone interested in e-health should study the historical evolution and knowledge development not just of e-health domains and applications but also of the general computing, health informatics, and telemedicine revolutions that preceded the e-health revolution.
E-Health History
The genesis of health care computing can be traced as far back as the early 1950s, when only mainframes were available and only the major hospitals of G7 countries could afford to house and use these machines. In that period, even the processing of a routine batch of health-related information took a considerable amount of coordinated effort among various health professionals and computer experts. Despite the demand on expertise, the end results were mostly fraught with mechanical and programming errors. The failures of this first era of computing in health care were due mainly to the lack of active support from hospital administrators and top management, the lack of continuing funding, and the lack of knowledge and skill in the design and use of automated systems.
From the early 1960s through the 1970s, a new era of computing in health care emerged. A growing group of hospitals, including Akron Children's, Baptist, Charlotte Memorial, Deaconess, El Camino, Henry Ford, Latter Day Saints, Mary's Help, Monmouth Medical Center, St. Francis, Washington Veteran's Administration, and others throughout the United States, as well as Sweden's Danderyd Hospital and Karolinska Hospital, England's London Hospital and Kings Hospital, Germany's Hanover Hospital, and others in Europe began to agree on the need to advance a patient information management system prototype. Despite the risk of major system failures, these pioneering hospitals invested large amounts of money, time, and effort to move toward computerization. Seeing the sudden surge of interest among these hospitals and the potential market opportunities, large computer vendors such as Burroughs, Control Data, Honeywell, IBM, and NCR joined in an effort to support patient information systems. Lockheed Information Systems Division, McDonnell-Douglas, General Electric (GE), Technicon Corporation, and several other companies with a reputation for effective management of complex systems also collaborated. Nonetheless, many of the early projects were almost complete failures: the complexity of the information requirements of a patient management system was gravely underestimated. Companies such as GE and Lockheed had to withdraw their participation due to a lack of continuing funding, interest, and management support. Many pioneering hospitals also had to fall back on their manual systems to keep their facility operating smoothly, and several of the hospital administrators had to make the difficult choice to abandon their hospital information systems project at a huge loss.
The Technicon system was the light that was eventually found at the end of the long tunnel of hospital-based patient information system failures. This particular system, initiated by Lockheed for El Camino Hospital in Mountain View, California, and later acquired and improved by Technicon Corporation under the leadership of Edwin Whitehead, became the successful prototype that laid the foundation for all future hospital patient information management systems throughout North America and Europe. The major lessons learned in the El Camino project were the importance of focusing on user information needs and the need to change user attitudes, particularly to overcome resistance from physicians and nurses. Owing to the success of this project, large-scale data processing applications in medicine and health record systems also began to take hold during the early and mid-1970s as the use of computers began to result in continuing gains in productivity and evidence of increased efficiency.
Nonetheless, these early successes were achieved at very high costs. Johns Hopkins Oncology Center, for example, acquired their first computer system in 1976 for a quarter million dollars; its processing power was only a fraction of today's desktop computers. Other successful early patient record systems include the Computer Stored Ambulatory Record System (COSTAR), the Regenstrief Medical Record System (RMRS) and The Medical Record (TMR). COSTAR, a patient record system developed at Massachusetts General Hospital by Octo Barnett in the 1960s, was later extended to record patient data relating to different types of ailments (for example, multiple sclerosis [MS-COSTAR]) and is used even today in several teaching hospitals and research universities across the globe. RMRS was a physician-designed integrated inpatient and outpatient information system implemented in 1972, and TMR is an evolving medical record system that was developed in the mid-1970s at Duke University Medical Center. Together with the success of the Technicon system, the efficiencies of these automated record systems soon provided considerable motivation for the integration of computing into health care systems.
As soon as health administrators and practitioners began to realize the efficiency and data processing power of computers, which increased when minicomputers were introduced during the late 1970s and early 1980s, computerization began to be seen as a magic bullet for controlling and managing the large and increasing volumes of medical and other administrative data processed on a daily basis. Medical data range from demographics of patients to clinical and health services data to epidemiological and health population statistics, such as the prevalence and incidence of tuberculosis (TB) along with statistics on TB morbidity and mortality. Health administrative data encompass health administrative and patient financial data and inventories of drugs and medical equipment, as well as routine transactional data, including the management of patient billing, insurance co-payments, accounts receivable and payable and general ledgers. By the early 1980s, computer miniaturization and cost reduction simultaneous with increases in processing power resulted in a dramatic move away from massive health data processing using mainframe or minicomputers to new and more efficient forms of health management information system (HMIS), office automation (OA), and networking technologies.
Whereas HMIS automates routine management reporting to support administrative and patient care applications, OA designs health office systems and processes to reduce time and effort expenditure on the part of health knowledge workers such as doctors, pharmacists and nurses. Networking technology is a relatively new aspect of computing and refers simply to the electronic transmission of data, text, or voice information from one computer (source) to another (destination). Each of these “islands” of health computing technologies comprise hardware and software components interacting with humans to provide a catalyst for change—in particular, a move toward greater ease in managing information flow between or among health care stakeholders. Early experiences led to awareness that integrating HMIS, OA, and networks would change how work processes needed to be “informated” in the different areas of health service delivery. Users at all levels also realized that the key to unlocking the usefulness of these technologies rested in successful design of the human-computer interface—that is, the information display interface that the users see as the computer.
Health networking and telecommunications were soon discovered to be the most powerful pieces in the puzzle of an integrated health care information system, bringing together the different technological islands. The focus on these two technologies opened up interest in e-clinical decision support and e-medicine applications in the early 1990s. E-medicine was first tried in the 1970s via low-cost telephone technology, but interest in this area dwindled quickly due to lack of funding. In the mid-1990s, however, advances in health computing and networking technologies rekindled interest in e-medicine and other areas of e-health administrative, clinical, and financial applications, including e-commerce applications, e-clinical decision support and expert systems, e-nursing support systems, and other e-health applications such as e-home care systems. Intelligent medical information systems and health decision support systems (HDSS), it was thought, should be able to mimic the thinking processes of clinicians. Researchers have always wanted to add intelligence to computer systems, and the extension to remote medical diagnostic systems was soon considered a valuable and noteworthy medical computing application domain, foreshadowing the e-health era.
In light of new technologies and the massive infusion of investment money provided by corporate businesses and venture capitalists in the late 1990s and also in the process of protecting health care assets from the Y2K threat, researchers, businesses, and end users all began to shift attention to Internet connectivity. Whereas Internet use had previously limited to academics, its sudden widespread diffusion and the discovery of e-mail as a convenient technology among end users led to the dissemination of e-commerce and e-business concepts among young entrepreneurs.
E-consumers and young risk-taking entrepreneurs began using current and emerging Internet technologies, giving rise to extended e-technologies and applications, including intranets, extranets, virtual public and private networks, e-business networks, Web-based businesses, community networks and learning communities, and Web development and maintenance services, all of which ultimately blossomed and extended into various e-health perspectives, domains, technologies, and applications.
While e-health constitutes only a tiny part of the lengthy history of the life and medical sciences, which, according to Jordan (2002), date back as far as 3,000 B.C., the wave of interest in and consumer-driven requests for e-health services on employers, clinicians, doctors and pharmacists in just the last several years is mind-boggling. In the context of the e-business revolution, e-health is seen as a paradigm shift from a physician-centered care system to a consumer-driven care system (see Chapter Sixteen). In other words, e-health systems place the e-consumers rather than the caregivers at the center. As one example, these systems are used primarily by e-patients to connect with member physicians when they want and wherever they want; patients are no longer limited by time and space. Further, if the quality of services or products or the level of health knowledge provided by a certain e-care provider or HMO does not meet the e-consumer's expectations, he or she has a convenient means of switching e-care providers. More significantly, the flow of e-health data, information, knowledge, and even wisdom will eventually empower e-consumers to take on new roles, not just seeking alternative care services from the best available and accessible sources but also educating themselves in evidence-based medical practices, in integrative (holistic) and gene-based medicine, in alternative and complementary clinical modalities, and in health-promoting lifestyles, activities, and behaviors. Eventually, these actions and changes in e-consumer health and lifestyle behaviors will result in new and creative forms of consumer-driven health information therapies.
Since we are now more aware of the numerous possibilities and channels through which e-health can be intelligently applied and practiced, we can turn our attention to the e-health application clusters that have been or can be implemented.
Domains of E-Health Applications
In general, e-health domains and applications can be divided into two primary clusters based on two key dimensions of systems integration characteristics (Raghupathi and Tan, 2002).
On one hand, systems that are characterized by a high degree of internal integration include applications such as the following:
- Virtual patient records (VPR)
- Document management (DM)
- Geographical information systems (GIS)
- Group health decision support systems (group HDSS)
- Executive information systems (EIS)
- Data warehouses (DW)
- Data mining
We define internal integration as the degree to which systems and technologies are integrated with one another within an organization.
On the other hand, systems that are characterized by a high degree of external integration include the following:
- Telecommunications, wireless and digital networks such as asynchronous transfer mode (ATM) networks
- Community health information networks (CHIN)
- The Internet
- Intranets and extranets
- Health informatics
- Telemedicine or e-medicine
External integration is defined as the degree to which systems and technologies interface with outside organizations and agency computer systems.
VPR technology houses uniquely identifiable information about an individual patient from various isolated sources. Accordingly, diversified data coded in different formats for use with different platforms can be converted for use with a common virtual platform. This is not just the creation of a massive traditional database but the design and development of a common network via a system which permits various components to interact and operate together (an open system) for the conversion and transmission of media-rich medical data from multiple distributed sources to support multiple users. TeleMed, a collaborative VPR prototype project created by researchers at Los Alamos National Laboratory and physicians from the National Jewish Medical and Research Center in Denver, supports real-time interactive uses of media-rich graphical patient records among multiple users at multiple sites. VPR technology is ideal for telemedicine practitioners.
Document management technology aims to put clinical and financial data online. DM applications can include document imaging, workflow optimization, electronic form processing, mass data storage and computer output to laser disk, among other possibilities. Many hospitals and health organizations use DM technology to handle the otherwise paper-intensive process of collecting and filing patient information. For example, notebook computers and customized software can allow busy nurses to rapidly and accurately update all patient and insurance records electronically instead of handwriting and later transcribing many documents and forms between their regular visits to patients. This technology frees up time for nurses to focus on patient care.
A geographical information system (GIS) is a powerful tool for collecting, recording, storing, manipulating, and displaying spatial data sets. A GIS uses spatial data such as digitized maps and can represent a combination of text, graphics, icons, and symbols on two-dimensional and three-dimensional maps. GIS technology might be used for digital mapping of a certain epidemic—for example, HIV infection among a subpopulation across various counties in a province or state. This knowledge can then be used to effectively target interventions for specific population groups.
A group health decision support system combines analytic modeling, network communications, and decision technology to support group decision-making processes such as group strategic thinking, problem formulation, and generation of goal-seeking solutions. Use of a group HDSS can reduce not only the cognitive burden but also the mental effort associated with group meetings. This technology also has the potential to increase the efficiency, effectiveness, and productivity of group interactions through asynchronous board meetings, on-line forums, or special group meetings in which board members and executives can network and share information with one another without being completely constrained by separation in time and geographical distance.
In the context of an e-health provider organization, an executive information system (EIS) collects, filters, and extracts a broad range of current and historical e-health-related information from multiple applications and across multiple data sources, both external and internal. This provides the organization's executives and other key stakeholders with the necessary information to identify key problems and strategic opportunities. A common EIS application entails an HMO executive using it in long-distance strategic planning sessions to determine the challenges and potentials of various business strategies. One popular feature is the ability of an EIS to narrow or expand information from one level to another, enabling executives to conveniently retrieve answers to special or ad hoc queries. For example, a DSS that allows a health manager to know who and why a group of people are “frequent” users of the organization's emergency services let the organization implement appropriate policies to prevent resource abuse or misuse. Another important feature is the ease with which EIS technology can be integrated with related technologies such as a geographical information system, an expert system (ES), an HDSS, or a group HDSS.
Data warehousing architecture for integrated information management simply provides an integrated source of aggregated, organized, and formatted data. The data in a DW are designed to support management decision making and strategic planning. Accordingly, these data may sometimes be stratified (categorized in various forms), and most likely have already been aggregated and filtered after coming from legacy systems. Again, a DW can be combined with an EIS, an ES, an HDSS, a group HDSS, or a GIS not only to increase data analytic and processing power but also to develop new and complex forms of e-health technologies.
Today, the most prominent use of a DW in e-health care is the automated collection of massive amounts of linked data from diverse sources for use in data mining (sometimes referred to as data dipping) techniques. Data mining techniques explore the data for hidden trends and patterns. Data mining tools include artificial neural networks, case-based (analogical) reasoning, statistical methods, genetic algorithms, and explanation-based reasoning. The opportunity for an HMO to explore and discover best practices by comparing and contrasting physician practice patterns for different treatment protocols corresponding to groups with specific case mixes is one benefit of applying DW and data mining technologies. The unraveling of the human genome to provide treatments for various challenging ailments is another noble example of DW and data mining technology applications.
Turning now to e-health systems and applications characterized by a high degree of external integration, we will start with e-health networking technologies. These essentially are applications that speed up large-scale movement and exchange of media-rich health information from one point of a network to another. The architecture of such a network may be a hub-and-wheel communication configuration; an open system configuration, including the use of the Internet, electronic data interchange (EDI), and extranet; a groupware application; or an intranet configuration (see Tan, 2001).
A community health information network (CHIN) may be conceived as a network that links health care stakeholders throughout a community or region. Such an integrated collection of telecommunication and networking capabilities can facilitate communications with patients as well as the exchange of clinical and financial information among multiple providers, payers, employers, pharmacies, and related health care entities within a targeted geographical area. Central to a CHIN's success is the practical implementation of a computerized patient record system at the community or regional level. Figure 1.2 shows the Wisconsin Health Information Network, an example of a participating CHIN. In this figure, WHIN connect software provides various business task applications to participating users. Whereas WHIN switch controls the mode and rate of access among the various users, WHIN processing ensures that data input provided by the users are cumulated to generate the required output (reports).
CHIN technology has become an important interactive research and communication tool, aiding both medical professionals and health consumers in search of health-related information and knowledge.
Intranets and extranets extend the concept of the Internet as a complex web of networks. Intranets and extranets use the same hardware and software as the Internet to build, manage, and view Web sites. Unlike the Internet, however, these virtual networks are private; they are protected by security software known as “firewalls” to keep unauthorized users from gaining access. An intranet supports Internet-based services only for organization members, whereas an extranet extends network access privileges to certain partners, giving them access to selected areas inside the private virtual network, thereby creating a secure customer or vendor network. A simple example of integrated Internet, intranet, and extranet use in health care is providing users such as e-patients, e-physicians, and other e-providers with access to on-line insurance service data. Electronic filing of insurance benefits and claims via an extranet dramatically cuts agency and other labor costs while increasing the accessibility of the information for both patients and providers as well as providing administrative insights into health care trends and medical best practices. The use of intranets and extranets ensure the security and the accuracy of these transactions as the information is encrypted and transmitted over secure lines to ensure confidentiality. Whereas the intranet are used to share the internal data of an organization, the Internet and the extranet connect users from outside the organization primarily to information that may be released to the public.
FIGURE 1.2. WISCONSIN HEALTH INFORMATION NETWORK (WHIN)
The chief emphasis of health informatics and telemedicine is clinical and biomedical applications of e-health technologies. At the clinical level, e-health decision support systems (e-HDSS), e-clinical decision support systems (e-CDSS), and e-expert decision support systems (e-EDSS) are being developed to assist physicians and other medical specialists in diagnosis and treatment. An example of an e-CDSS is an interactive videodisk system that helps a client enter personal health data in order to weigh the pros and cons of surgery. HDSS is a generic term used among the administration staff whereas e-CDSS denote a clinical focus and are systems used by health providers. In contrast, e-EDSS are domain specific systems used amongst specialists (see Tan and Sheps, 1998). Other examples include systems that monitor heart rates and alert care providers if they are abnormal, that guide prescribing pharmacists to potential adverse drug interactions, and that educate patients on preventive health care and health-promoting activities.
Finally, e-medicine, which is a more generic term, unlike traditional “telemedicine” thinking, is the use of digital networks to perform virtual diagnosis of disease and disorders. In teleradiology, among the first successful applications of e-medicine, X-rays or scanned images of patients are digitized and stored electronically so that they can be shared among multiple health providers at geographically distant sites. Other e-medicine applications include teleconsultation—for example, in teledermatology and telepathology; telesurgery, including telegastroscopy (see Chapter Ten); robotics and virtual reality (see Chapter Sixteen); telelearning—for example, using videoconferencing or on-line medical education; and telecare (see Chapter Nine).
E-HEALTH STRATEGIES AND IMPACTS
Among the most critical aspects of e-health systems are planning e-health business strategies, e-health care technology management and diffusion, e-health system implementation and evaluation, and envisioning and monitoring the impacts of e-health technology.
The planning aspect involves building a strategic vision to align the goals of senior management with the changing needs of the e-health marketplace. Technology management and system implementation relate to managing the diffusion of e-health innovations, redesigning work practices so that both workers and users can work virtually (e-work), and addressing issues of user acceptance or failure arising from the implementation and evaluation of an e-health system. Not only is it important to focus on the impacts of e-health systems on individuals, groups, communities, and societies, but it is also critical to realize how the implementation of an e-health system may ultimately affect the larger context of our health care delivery system both nationally and globally.
Planning E-Health Strategies
Planning e-health strategies includes identifying e-consumer needs and business requirements, applying systems theory and decision theory, materializing telemarketing and virtual network management concepts, planning e-data warehouse mining and e-technology strategies, and championing sound methodologies for growing new and complex e-health applications. Most important, the mission of the system analyst group should reflect the vision of the system creator and should serve as a thematic rationale for integrating individuals and virtual group teams toward the achievement of planned goals and objectives.
A major trend in planning e-health strategies is shifting responsibilities and power from traditional health providers and health system analysts to e-consumers, the people who ultimately determine the survival, use, and growth of the e-health business ventures. Traditional approaches have concentrated on satisfying business needs with little attention paid to e-consumers. The decisions of leaders and system analyst groups should echo and reflect more appropriately the active participation, expressed needs and recorded feedback of e-consumers. This trend reflects growing acceptance of the notion that e-health data, information, and knowledge are shared resources and that the acceptance of any e-health business model and the accompanying interface design requires a consensus of e-health providers, payers, and consumers. Given the rapid shifts in the e-technology marketplace and the lengthy delays often experienced between the vision of a new e-health system and its realization, it is generally wise to revisit the decisions made during planning sessions and to conduct intensive market research and prototyping before implementing an actual e-health system.
More recent approaches call for shorter gaps between system strategic planning sessions and more attention given to the changing marketplace (see Chapter Twelve). In addition, an environmental assessment must always be conducted before formulating a strategic plan. Scenario planning is one approach to system strategic planning. Here, competing futures are envisioned, and strategies are developed and tested against these possible futures. The e-technology vision is then determined on the basis of the scenario results, taking into account current technological and system capabilities. For example, if the e-technology vision calls for handheld devices to be employed by all the e-health home care workers, who currently use only cell phones, then the transition to the new e-technology will call not only for changes in work practices and habits but also for finding new ways for patients to connect with workers, examining how workers monitor their patients remotely, and determining how workers are to be monitored and managed virtually (see Chapter Nine).
Successful e-health system planning also requires effective e-health care technology management (e-HCTM). Briefly, e-HCTM is management of the entire e-health technological infrastructure and the information processing capacity of the virtual business system. Top management must work to ensure that information resources and e-technology are best adapted to meet the needs of the marketplace. In many cases, the necessary work process restructuring for efficient e-health information processing and effective decision making will not happen without significant leadership at the executive level, including extracting past experiences and expertise within the e-business community (see Chapter Thirteen). Moreover, the increased complexity of the e-health care environment and the rapid rate of change in technological capabilities make the process of e-HCTM increasingly complex and difficult.
E-Health Implementation and Evaluation Issues
E-health system implementation and evaluation include responsibility for overseeing the integration of e-technologies, the incorporation of e-health transactional activities into the virtual e-health system, the incorporation of security and privacy mechanisms to ensure user acceptance and satisfaction, and the training and education of users migrating from legacy systems to the e-health system. Not only should e-technologies be integrated with old and new equipment within the existing virtual network configuration, but system transactional procedures must also be integrated into existing administrative procedures. Administrative issues may also include the privacy, security, and confidentiality of virtual patient and e-patient records; legal and ethical considerations regarding data collected, analyzed, and distributed electronically; and policies regarding security and network standards (see Chapter Fourteen). Among other important goals and objectives of e-health system implementation and evaluation are the following:
- To achieve significant operational cost savings
- To generate revenues without sacrificing quality patient care
- To project an improved professional image by relieving health care workers of tedious physical reporting activities so that they can concentrate on patient care
- To achieve user satisfaction, especially for e-consumers who will be relieved of travel costs and other inconveniences
One significant goal of e-health system implementation and evaluation strategy for a virtual system is to ensure that top management gives adequate attention to ensuring a smooth interface between the technological and human elements. Such interfaces occur at two levels: first, the human-computer interface (HCI) between the individual users and software applications, and second, the system technology interface (STI) between the various users and organization technologies as a whole, including human considerations involved in work processes and transactions, and the e-technology. STI focuses on the overall alignment of technology and human resources in pursuit of the overarching business goals, while HCI emphasizes building applications to augment specific functions for users. Many problems faced in system implementation and evaluation have to do with inadequate HCI design or poor STI configuration. The significance of these interfaces cannot be overemphasized, because the users, whether e-workers or e-consumers, do not have face-to-face interactions but conduct their businesses completely through these interfaces.
The challenges of e-health system implementation and evaluation are therefore interwoven with many other factors, including the integration of quality planning, quality control, and quality improvement processes to evolve a secure, well-managed, and quality-focused e-health care environment and the integration of network technology management, organization technology management, and user-interface technology management to build efficient, enterprisewide system infrastructure and interfaces. Integrating electronically gathered data, model, and knowledge elements to design effective applications is key to sharing these resources. Together, these challenges point to the need to integrate environmental, technological, and administrative components in order to successfully drive and direct the implementation and evaluation of various e-technologies and applications within the larger context of Web services and the Internet, intranets, and extranets.
Finally, any e-health system implementation and evaluation will lead to suggested system modifications and changes—for example, to the e-networking infrastructure; to the level of computing competence required of current and future e-workers; in the information flow processes and business processes; and in the belief systems, ethics, lifestyles, and behaviors of e-workers and users. To ensure that these workers and users will have the critical knowledge, skills, and attitudes to address concerns arising from these changes, the system should also address staffing, training, and education issues. For example, attracting and retaining valuable technical staff calls for aggressive recruitment and telemarketing programs, new opportunities for staff training and development, and the employment of e-learning strategies for sharing knowledge among workers.
E-Health Impacts
E-health will have an impact on the individual user, the workgroup, and the forms of emerging health systems—for example, virtual alliances, virtual work management, virtual group interactions and networking capability, collaborative decision-making effectiveness, and shared intelligence and expertise. Aside from the government and venture capitalists, several other major e-stakeholder groups are involved in e-health care systems: e-consumers, e-providers, e-employers, e-vendors, and e-insurers. Each of these groups has a set of interrelated needs and desires that are not being met by the traditional health care information and network infrastructure.
At the individual level, for instance, users want to know if the introduction of an e-health system will result in better productivity and decision-making effectiveness for them. For example, a traveling health manager equipped with a personal data assistant (PDA) that acts both as a cellular phone with an automated directory and an Internet appliance with the ability to access e-mails and Web sites will probably be able to better perform his or her duties irrespective of his or her whereabouts.
At the workgroup level, e-health will affect the ability of group members to share data, to coordinate activities, and to network effectively. A virtual health record system used by multiple care providers, for example, will integrate all the information from different care providers regarding a single patient.
At the system level, we have noted that e-health will create change on many fronts—for example, system structure and culture. E-health will improve managerial productivity, increase control of information flow, flatten reporting hierarchies, increase the power of decentralized units, change the power and status of individual workers, and open up possibilities for new units and services. E-health systems will result in new cultural expectations for system behavior. In keeping with the e-health diffusion phenomenon, for example, automated intelligence, on-line training capabilities, and virtual networking may completely change the way a given system performs health care services.
The impacts that e-health systems have at the level of a single isolated system may be extended to the entire health care delivery system at a societal level. For example, the use of the Internet to transfer massive amounts of media-rich patient data and the availability of knowledge systems such as robots and automated intelligent systems may engender legal and ethical questions about privacy, security, and individual and institutional property rights. One such question that is frequently asked is “Who owns all the different pieces of stored medical information about a particular patient?” Other questions may be “What information should or should not be kept on-line about an individual, and who has priority access to the information?” Follow-up questions to those could be “How accurate and secure is the information being stored, and what prevents the on-line information from being misused?” Other societal impacts of advances in e-technology include the following:
- Changes in employment levels for mainstream health workers and how their work may be performed (for example, telecommuting)
- Changes in the role of disabled, women, and minority workers in the health workplace
- New opportunities for cybercrime and misuse of power
- New ways for e-consumers to purchase health care products and services
- New ways to prevent injuries from work in hazardous environments
- New gadgets and automated devices to help seniors and the disabled
- New modalities and ways of reaching distant consumers and the underserved
- Improvements in e-medicine and e-home care services, societal well-being, and the quality of life in general
Conclusion
By the last half of this new millennium, hospitals and other health service organizations will face increasing pressures to move toward an e-health model, due to changing demographics, changing governments, a changing e-technology marketplace, and changing health care environments. We have already seen how a young discipline such as the e-health field can grow and expand quickly to affect every aspect of daily health care—particularly our acute care systems and our public health systems.
Chapter Questions
- Do you feel that e-health phenomenon is a temporary fad or that it will become a permanent reality? Why?
- What is the significance of understanding the basic components of e-health? Why is it important to understand the major themes of the e-health field?
- Compare and contrast the e-health system with the mainstream health care system. What key factors distinguish e-health care from conventional health care?
- Imagine that you're living in the age of mobile health where wireless connections prevail. How might you choose among a list of available mobile physicians? What criteria will you use? Cost? Response time? Other measures? How would you go about determining and measuring these criteria?
References
Jordan, T.J. (2002). Understanding medical information: A user's guide to informatics and decision making. New York: McGraw-Hill, 2002.
Raghupathi, W., & Tan, J. (2002). Strategic IT applications in health care. CACM, 45(12), 56–61.
Tan, J. (2001). Health management information systems: Methods and practical applications (2nd ed.). Sudbury, MA: Jones & Bartlett.
Tan, J., with Sheps, S. (1998). Health decision support systems. Sudbury, MA: Jones & Bartlett.
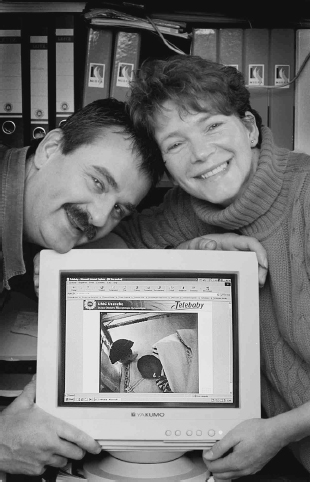
The Telebaby® Case
Ronald Spanjers, Anne F. Rutkowski
New information technologies can be efficiently used to fill the human need for communication during the difficult time when a family member is hospitalized. The Telebaby® project, designed and supported by the University Medical Centre Utrecht, links parents at home to their newborn receiving intensive, high, or medium care. Tele-baby is simple enough to be easily adopted by parents; however, implementing Telebaby in a hospital environment proved to be a real challenge.
Background
The concept of attachment is central to most discussions of parenting. The purpose of bonding may sound paradoxical: the natural phenomenon of bonding enables a child to develop feelings of security in strange environments and later to separate from the main caregiver (Bowlby, 1969, 1988). If skin-to-skin contacts are recognized as primordial in the development of healthy premature newborns, any separation of a mother and her child affects not only the child but also the mother (Klaus and Kennel, 1976, 1985). Attachment is gradual, not automatic, immediate, or to be instantly expected of the mother; however, caregivers often experience traumatic stress and anxiety when separated from their newborn.
The idea of an Internet facility to link premature infants with their parents was conceived in order to support parents during the difficult period of separation. The researchers assumed that it would give caregivers a feeling of greater control of their relationship with their newborn and thus reduce their anxiety. Reviewing previous experiences in linking mothers with their hospitalized children encouraged the researchers to persevere (Bialoskurski, Cox, and Hayes, 1999; Lupton and Fenwick, 2001; Woollet and Phoenix, 1991).
Sponsorship by the “Friends of the Wilhelmina Children's Hospital” made it possible to implement a system that allows a mother to view her newborn on the intensive, high, or medium care unit from her hospital bed through an internal video circuit. Later, the concept of Telebaby originated from the idea that video images could be distributed over the Internet. Technology that provided a connection between the hospital and patients' homes was built: Telebaby was born. Parents were enthusiastic about using the Telebaby facility as a complement to their regular visits at the hospital. Telebaby was surely an appealing concept. More important, Telebaby contributed to the well-being of the caregivers and thus the health of their newborns.
This case study begins with a description of the project and the supporting technologies used. The results of monitoring parents' login activity and the preliminary results of a parent survey questionnaire are also presented. We then conclude by examining some research limitations and suggestions for future developments.
Project
The Perinatal Center of the University Medical Centre Utrecht consists of two wards, Obstetric Care and Neonatal Care. The center has four hundred employees and an annual budget of 20 million Euros. Obstetric Care handles 10,000 new cases per year, with 30,000 follow-up consults. Of 4,500 admissions, 2,500 are adults and 2,000 are newborns, of which 1,000 need low care, 500 medium care, and 500 intensive or high care. In total, the admissions and 600 short-stay days generate 30,000 nursing days in eighty to one hundred beds and cribs.
In the planning stages of Telebaby, several issues concerning privacy and safety were raised. Given their nature, only practice could prove the extent of their relevance. More practical issues such as costs and image quality were dealt with before the project started. One major concern was the “gimmick effect,” the fear that the system, once developed, would have a short-term appeal for its concept and innovation but would not be appreciated for its contribution to the well-being of patients and families.
The Telebaby project started small and experimental. An exploratory team of three persons was formed, covering all necessary skills such as programming, financing, and understanding the medical and nursing activities of a perinatal center. Managers assigned a minimal and recoverable budget of 7,500 Euros. If the project had failed, most of the computer equipment could have been used elsewhere. The goal of the team was to test the concept and the technology. Within half a year, the team decoded and transmitted the signals required for transmission using standard Internet technology. Exhibit 1.1 presents a picture of a baby that was transmitted through the internal video circuit and that was used in a corporate campaign on innovation within the University Medical Centre Utrecht. Physicians, nurses and parents became curious.
EXHIBIT 1.1. VIDEO IMAGE OF A BABY AS TRANSMITTED THROUGH THE TELEBABY VIDEO CIRCUIT
The hospital's automation department, working with Infoland, an Internet streaming company, ensured the stability of the technology. Providing maximal support to the users (parents and nurses) was recognized as the most important factor for success or failure (Oudshoorn, Brouns, and Van Oost, 2005). A budget of 75,000 Euros was acquired through the Friends of the Wilhelmina Children's Hospital. The largest part of the budget (55,000 Euros) was used for hardware and software, including the server, encoders, laptops, adaptation of the internal video circuit, and customized software. An estimated 400 hours were spent developing and implementing the concept (excluding software development by Infoland), for a total of 20,000 Euros in personnel costs.
Hardware and Software
The internal video circuit consisted of twenty analogue Panasonic cameras, mounted on a standard equipment rail on the crib with a fixed focus. They were connected to an internal coaxial network with an XLR plug that also provided power. Because the camera was located outside the crib, the image sometimes lost quality when the plastic top of a crib produced shimmering. The cameras were routed to the television in the mother's hospital room (or an Internet stream) using a patch bay that connects specific cribs with specific destinations inside and outside the hospital. This way, fifty cribs could be connected to fifty different beds.
The internal video circuit had to be adapted for Internet video streaming. An encoder transformed the analogue signal of the internal video circuit into a digital video stream. The encoding was done on-line in real time with a delay (buffer) of five seconds, and the frame rate was ten frames per second. A 56K modem on an average bandwidth network was able to adequately handle the data flow. A higher-quality modem did not provide a better image of the newborn, because the load of encoded data was relatively low: changes in light intensity were few, the newborn hardly moved, and movement around the crib was limited. Sound was not encoded because of privacy considerations rather than technical limitations; the microphone of a newborn in one crib could transmit speech from physicians or nurses providing care to another nearby newborn. Furthermore, it is was feared that parents might misinterpret sounds on the ward, such as the audio control signals from respiratory equipment, thus raising instead of lowering their anxiety.
The streams are offered to a server that distributes them to the viewers. The server is a standard Compaq PC (800 MHz, 16 GB, 522 MB). The four encoders are also standard Compaq PCs, all with four Osprey 200 Codec cards. The software used is the Windows 2000 operating system with Windows Media Encoder and customized I-stream software from Infoland. Telebaby is accessible through a standard browser on the hospital's Web site. The login screen includes a “thank you” page that lists the sponsors and a disclaimer page that covers legal issues. The four types of users—the administrator, the automation department, the nurse, and the parent—have different menus. The administrator (supervisor) has access to all menus, including the system users menu (where types of users can be set), the camera control menu (which holds IP settings of the streams) and the general fields menu (where the patient data fields displayed along with the stream can be defined). The automation department and the nurses can access the menu where streams are assigned to patients and predefined patient data fields are filled in. The camera overview menu gives a thumbnail page of active streams (Exhibit 1.2). The parents (Exhibit 1.3) have access only to the parents' menu, which displays the stream of their newborn and some patient data fields such as name, unit, bed, the unit's telephone number, and the name of the primary nurse. No other menus were accessible from outside the hospital.
EXHIBIT 1.2. TELEBABY CAMERA OVERVIEW MENU
EXHIBIT 1.3. PARENTS AT HOME, WITH ON-LINE TELEBABY CONNECTION
Implementation
A team of nine “Ambassadors of Telebaby” nurses was formed. This team was given extra training so that they could facilitate the implementation process and provide basic support for parents. Over 50 percent of the parents had Internet access at home. Five preconfigured laptops, each with an Internet account, were available for those who did not have a personal computer. Parents had to fill out an intake form, which requested information such as their address and which type of Internet connection they used (cable, phone, ISDN). Nurses used the intake sheet to add the newborn's data in the patients' menu and assign a stream. Parents (and other users) were given a hard-copy manual that was comprehensive in terms of navigating the software and system and had step-by-step screen shots.
An extensive, more technically oriented software manual was accessible via the Web site. Parents were asked to log in on a demonstration stream first, to reduce anxiety when logging in to see their newborn for the first time. Only after they had successfully logged in on the demonstration stream were parents given the login name and password for their child's video stream. More than one viewer can access the stream for a given infant at one time; parents were free to pass on the login name and password to relatives. Once parents could see the demonstration stream, almost no technical barriers could keep them from logging in to see their newborn. A blue or black stream indicated that the camera had been unplugged or covered at the unit; for example, parents who visit the unit will not need the camera, or the camera may be physically in the way when providing care to the newborn.
Implementing an externally oriented information system in a hospital triggers safety issues, particularly when this system crosses the boundaries of the hospital's networks. Hospitals have tight security policies. In this case, the streams were rerouted through the completely separate and more open network of the medical faculty. Acceptance of the system by physicians and nurses was obtained by relating it to the perinatal center's basic philosophy of keeping mother and child as close together as possible in a clinical setting. Telebaby extends this philosophy when the mother is discharged. Physicians and nurses had the basic right to switch the camera off when providing care to the newborns. However, it was stressed to parents that the quality of care was the same regardless of whether the camera was switched on. The twenty-four-hour nature of perinatal care, combined with the fact that some of the nurses only took night shifts, made the training difficult to plan and demanded a clear instruction manual.
Results
The login activity of the parents was closely monitored. The log file contains data such as duration and frequency of use (Exhibit 1.4) such as via a unique viewer identifier generated by the Windows Media Player. Usage was high between 11 A.M. and 3 P.M. A clear pattern of “anxiety visits” can be discerned. These short but frequent visits at 2 P.M. and 9 P.M. offer parents a feeling of control. They quickly see their newborn and log off, most likely after seeing the baby moving. At 10 P.M., the unit's lights dim and image quality drops, so usage is minimal after that hour.
System use over time varied and depended on the admission and discharge of patients and parents. Mothers who used the internal video circuit usually applied for the Internet streaming facility when they were discharged and their newborn stayed in the hospital. Average frequency of system use usually drops after the first few days and picks up shortly before the newborn is discharged, exceeding the initial use. System use on the weekends is low because parents visit the hospital more frequently on weekends. One important finding was that parents with access to the Telebaby system did not visit their newborn less frequently. Physical visits were always parents' first choice.
A questionnaire (n = 31) was distributed to parents after they had used the system. Parents were asked to rate the Telebaby system on a five-point Likert scale from −2 (not useful at all) to +2 (very useful). In preliminary results, parents rated the system very useful (M = 1.84, SD = 0.38). The parents were positive about the value that Telebaby added to the general level of health care provided to their newborns (M = 1.70, SD = 0.67). When using the system, parents worried less about their newborns (M = 1.26, SD = 0.82).
EXHIBIT 1.4. DURATION AND FREQUENCY OF TELEBABY USE
Parents were slightly less enthusiastic about the quality of the picture but generally satisfied (on a ten-point scale, with 10 as the maximum score, M = 6.35, SD = 1.10). Parents who used the hospital's internal video circuit found the streaming image quality less satisfactory, while parents who had never used the internal video circuit rated the overall image quality (both refresh rate and size) higher.
Conclusion and Limitations
Parents were enthusiastic about the possibility of using Telebaby as a complement to their regular hospital visits. The login activity of parents showed that using standard Internet technology to distribute multimedia images allowed parents to visit their newborn more often than they could have without the technology and markedly reduced the anxiety associated with the mother-child separation. The preliminary results of a questionnaire administered to parents (n = 27) indicated that Telebaby gives the parents a feeling of control in regard to knowing the state of their newborn. Parents of newborns are preoccupied; lack of a working system lowers their feeling of control over the state of their newborn and raises anxiety.
A system like Telebaby could become standard for perinatal centers. However, more investigations into experimental, ethical, legal, cultural, medical, and developmental issues should be conducted. For clear ethical reasons, we could not design a control group of parents who did not benefit from the Telebaby system. Monitoring of the login activity of parents revealed that the parents did share the password and login information to allow family members and friends to virtually visit their baby. If this trusting attitude toward such technology generalizes to other similar systems, ethical considerations of privacy and security should be given serious consideration. It would be interesting to see how people from different cultures react to such a project. Adding dynamic medical data such as saturation and heart rate could make the system more useful for physicians and nurses (Gray and others, 1998; Halamka, 2001). Because research suggests that the mother's voice plays an important role in the mother-child bonding, an auditory expansion to allow babies to hear their mother's voice would be worth investigating. Broadband Internet could make the transfer of sound from a parent's home to a hospitalized newborn more feasible (Dekkers and others, 2002).
In conclusion, valuable contributions to the quality of patient care can be made by applying standard information technology. While a system like Telebaby cannot replace the skin-to-skin contact of a baby with his or her caregivers, it nonetheless contributes to the relaxation of the parents. Spitz (1945) would surely agree that such a system can only be favorable for the hospitalized newborn's well-being. With health care moving toward a much more patient-orientated approach, we suggest that a relatively simple and low-cost application such as Telebaby can also contribute to the well-being of the caregivers and thus of their newborns.
Case Questions
- How feasible would it be to apply the Telebaby system in your country or work-place?
- Can you envisage improvements in the hardware and software integration of the Telebaby system?
- If you were involved in implementing Telebaby, how would you ensure, evaluate, and even enhance its effects and effectiveness?
- What are the psychosocial aspects and benefits of Telebaby? Can you identify any negative aspects? If so, how would you go above resolving these challenges?
References
Bialoskurski, M. Cox, M. C., & Hayes, J. (1999). The nature of attachment in a neonatal intensive care unit. Journal of Perinatal and Neonatal Nursing, 13, 66–77.
Bowlby, J. (1969). Attachment and loss: Vol. 1. Attachment. New York: Basic Books.
Bowlby, J. (1988). A secure base: Parent-child attachment and healthy human development. New York: Basic Books.
Dekkers, L., Dijkhuizen W. J., Van Geelen, N., Golder, T. J., Huizinga, H., & De Jager, M. (2002). Een Toekomst van Glas: Vooruitlopen op de Doorbraak van Breedband-technologie [A future of glass: Being ahead of the broadband breakthrough]. Stichting Maatschappij en Onderneming [small promotional book on broadband that uses Telebaby and similar applications as an example]. Den Haag.
Gray J., Pompilio-Weitzner, G., Jones, P. C., Wang, Q., Coriat, M., & Safran, C. (1998). Baby CareLink: Development and implementation of a WWW-based system for neonatal home telemedicine. Proceedings of the AMIA Annual Symposium (pp. 351–355).
Halamka, J. (2001). Inside a virtual nursery. Health Management Technology, 6. Retrieved from http://www.healthmgttech.com
Klaus, M., & Kennel, J. (1976). Maternal-infant bonding. St. Louis, MO: Mosby Press.
Klaus, M., & Kennel, J. (1985). Parent-infant bonding. St. Louis, MO: Mosby Press.
Lupton, D., & Fenwick, J. (2001). They've forgotten that I'm the mum: Constructing and practising motherhood in special care nurseries. Social Science & Medicine, 53, 1011–1021.
Oudshoorn, N., Brouns, M., & Van Oost, E. (2005). Diversity and distributed agency in the design and use of medical video-communication technologies. In H. Harbers (ed.), Inside the Politics of Technology. Amsterdam: Amsterdam University Press.
Spitz, R. (1945). Hospitalism: An inquiry into the genesis of psychiatric conditions in early childhood. In A. Freud (Eds.), Psychoanalytic Study of the Child, (Vol. 1, pp. 53–74). New York: International Universities Press.
Woollet, A., & Phoenix, A. (1991). Psychological views of mothering. In Motherhood: Meanings, practices and ideologies (pp. 28–46). London: Sage.
All photos containing individuals in this case study are subject to the privacy policy of the University Medical Centre Utrecht and have been cleared for use in this publication. Reproduction of these photos without the explicit authorization of the authors and the University Medical Centre Utrecht is prohibited.