![]()
CHAPTER EIGHT
DIFFUSION OF E-MEDICINE
E-Medicine in Developed and Developing Countries
Joseph Tan, Mengistu Kifle, Victor Mbarika, Chitu Okoli
B. Challenges in Diffusing E-Medicine
C. Factors Driving the Diffusion of E-Medicine
B. Factors Affecting the Diffusion of E-Medicine in Ethiopia
4. Culture-Specific Beliefs and Values and Technological Culturation
C. Research on the Diffusion of E-Medicine in Developing Countries
IX. E-Medicine Development in Taiwan Case
Learning Objectives
- Define e-medicine in the context of the different periods in the development and growth of e-medicine as a concept, a discipline, and a practice
- Review challenges faced in the history of e-medicine
- Understand the significance of diffusing e-medicine in Canada
- Identify factors affecting the implementation and diffusion of e-medicine in developing countries, specifically Ethiopia
- Recognize the relationships among the factors that affect the transfer of e-medicine as well as their potential impact on the success of e-medicine implementation
Introduction
E-medicine can be defined as the diffusion of medicine and health care services through the use of information and communications technologies. In mainstream medical, public health, and health services research literature, terms such as telemedicine (which literally means medicine at a distance) and telehealth are often used interchangeably to refer to e-medicine services, with the understanding that telehealth encompasses not only telemedicine services but also important e-health administrative and support services (see Chapter Seven). The application of telemedicine to deliver e-health care and e-health education is not new (Bashshur, 1997). Throughout this book, however, the term e-medicine is often used not only in a broad sense because it corresponds elegantly to the notion of e-health diffusion but also in a more restricted sense because it refers to a specific aspect of e-health diffusion: the diffusion of various specialties and subspecialties within the telemedicine domain. Specific examples of e-medicine include teleradiology, teledermatology, telepathology, tele-ophthalmology, tele-oncology, telepsychiatry, telecardiology, telenursing, and tele-accident and emergency support. E-medicine contributes to the sociopolitical, cultural, and economic infrastructure and development of a country. It can help provide multidisciplinary perspectives in health care delivery to individual citizens, selected groups and communities, and even entire populations.
In this chapter, we provide an overview of e-medicine, focusing on the history of and the driving factors in the diffusion of e-medicine technology. Next, we discuss e-medicine in Canada, focusing on the work of the Canadian federal government, provincial initiatives, and investigations by university researchers. We then highlight the diffusion of e-medicine in developing countries, pointing out the critical success factors and challenges. Finally, we move on to discuss the diffusion of e-medicine in less developed countries, using the specific case of Ethiopia and examining the factors influencing success in the implementation of e-medicine applications.
E-Medicine Overview
As we discussed in Chapter Seven, e-medicine technologies have been and are being used for e-clinical services, e-diagnostic and information services, e-learning, and e-administrative applications in the health care sector. E-clinical applications support the access and delivery of clinical care at a distance and capture, organize, store, and share clinical information among providers as well as between providers and patients. The information collected is typically needed for e-patient assessment, e-diagnosis, and e-treatment.
One application of e-medicine for e-clinical services is telesurgery. In telesurgery, surgeons control a robotic device to perform an operation at a remote location. This work is still in the very early stages, with feasibility studies being conducted on pigs. Another popular form of e-medicine, illustrated in the case discussion in Chapter Ten, is teleradiology, in which rural hospitals can obtain readings of teleradiological images from urban centers that are more likely to employ senior and highly qualified radiologists.
Within e-diagnostic and information services, the four subcategories are teleconsulting, teleconferencing, telereporting, and telemonitoring. In teleconsulting, a patient uses an e-medicine service to consult with a health care provider. A teleconference entails two or more health care workers communicating over a video link to share responsibility for the patient, who is usually not present. Both telereporting and telemonitoring involve the transmission of relevant health information by a clinician to a remote center for interpretation. The analysis is then fed back to the clinician. The only difference between these two subcategories is that in telemonitoring the patient data are collected continuously or at intervals, whereas in telereporting, the transmission is usually done once.
E-learning applications provide on-line, Internet-based, and remote delivery of training and education services such as continued medical education for physicians and other health care professionals. These applications can also provide consumer health information. For example, one of the authors generated teaching materials jointly with a team of experts from the University of British Columbia (UBC) and the University of Cape Town (UCT) for health planning modules for the maternal and child health program for residents and medical students being trained in South Africa. The materials developed were delivered on-line. Several issues were immediately apparent. For example, due to cultural, socioeconomic, and political differences between the countries, the materials did not address real-life scenarios encountered by the medical students in their workplace. In other words, the perspectives and experiences of the experts in British Columbia were not ideally meaningful to the medical students in Cape Town. Collaborative learning had to occur between developers of the materials from the two countries. Such difficulties and challenges were quickly resolved among the team members through videoconferencing over satellite channels rather than expensive overseas travel. Some medical students located at UCT were also able to access materials via the Internet, cutting across geographical barriers and providing opportunities for a dialogue between the students and the experts. Both experts and students learned from this process.
E-administrative support is the exchange of e-health information among payers, providers, employers, and consumers—for example, through electronic health records, administrative data warehouses, and clinical databases, as well as through public health networks. On-line business-to-business and business-to-consumer billing; on-line claims made by e-consumers on e-businesses and between business entities; e-inventory management by suppliers and retailers; and e-financial transactions between vendors and third-party payers are all examples of e-administrative processes. Detailed discussions and illustrations of these e-technologies are available in Chapter Seven and elsewhere in this text. We will focus our discussion at this point on the history of e-medicine.
The History of E-Medicine
The roots of e-medicine can be traced as far back as 1876, when the telephone was invented. Even as early as the 1920s and 1930s, the concept of linking patients and doctors without the physical presence of the parties in the same location had surfaced publicly. In 1924, a picture of a patient interacting with a doctor on television appeared on the cover of the magazine Radio News, with the title: “The Radio Doctor—Maybe!” (Field, 1996). Interestingly, the first television transmission did not occur until 1927.
Today, the telephone is still an important component of e-medicine. During the days when telephones were reserved mostly for those who could afford them, physicians and pharmacists used them to teleconsult with one another. Wealthy patients also used them to reach their physicians for emergency services. Eventually, telephones were used to transmit basic clinical information; for example, in 1948, X-ray images were sent between New York and Pennsylvania through telephone lines (Viegas, 1998). However, e-medicine today encompasses more than low-cost telephone technology.
A critical phase in the development of e-medicine was the emergence of radio at the end of the nineteenth century and television in the early twentieth century. Radio was first used to provide medical advice for seafarers who required medical attention while at sea; it is still being used on board aircraft to provide medical assistance to passengers. As for television, physicians used it to aid in neurological examinations, as well as to teleconsult with other experts (Field, 1996). Among the first demonstrations of the capability of interactive video for e-medicine was the use of a two-way closed-circuit television system to link the Nebraska Psychiatric Institute and Norfolk Hospital with the University of Nebraska.
Subsequent significant breakthroughs in the diffusion of e-medicine can be divided into three historical periods. The first period covers the 1950s to the early 1970s. The 1950s and 1960s were marked by an effort to improve e-clinical care in specialty areas, including teleradiology, telecardiology, teledermatology, and telepsychiatry. In the early 1970s, longer distances were being covered through the use of satellite signals instead of phone lines. The majority of projects undertaken during this era before mass computing, however, were mainly proof-of-concept research in the form of technological feasibility studies. Most of these projects were attempts to provide medical services to astronauts. Governments picked up the substantial expense of staffing and directing projects operated with standard analog televisions. However, when the funds were exhausted, the projects similarly dwindled.
Fortunately, the second e-medicine period, from the late 1970s to the early 1990s, was characterized by the development of digital technology. During this period, computers became commonplace and digital communication methods emerged. Soon it was discovered that interactive videos could be distributed over wide area surface networks at a much lower cost than with analog television systems. During this period, e-medicine projects made use of computer-based, digital teleconferencing systems. Among the most significant projects of this period were those examining the feasibility of e-medicine for rural areas. Here, it was argued that real cost savings would materialize because of reduced travel costs; in addition, better health outcomes for e-patients would result from more timely diagnoses of illnesses.
Some very challenging barriers to the diffusion of e-medicine also became obvious during the second e-medicine period. Barrett and Brecht (1998) list these barriers as technology and standards; liability, licensure, and confidentiality; and reimbursement. Even so, the large number of images and data to be transmitted in teleradiology and telepathology led to the development of the Digital Imaging and Communications in Medicine (DICOM) guidelines, the first set of standards, by the American College of Radiology and the National Electrical Manufacturers. At the same time, Internet use and communications via e-mail were proliferating among physicians and other health professionals, who were exchanging text, images, and video around the world (Viegas, 1998). Concerns over escalating health care costs in both the United States and Canada, coupled with the diffusion of e-technologies, gave rise to renewed interest in e-medicine.
Today, the key challenges we are facing involve the need for improved standards; the use of wireless technologies; security, confidentiality, and privacy issues; legal questions about jurisdictions and reimbursements for e-medicine services; and the need for large-scale formative and summative evaluation of e-medicine initiatives.
Challenges in Diffusing E-Medicine
At present, there are more Internet hosts and servers in Los Angeles than on the entire African continent and more hosts and servers in Singapore than in Vietnam or the numerous Indonesian islands. In most developing countries, many suburbs and villages still lack basic telephone service. Despite our heralding the news that the Internet will provide one of the cheapest and fastest solutions to improving the health and well-being of world populations, the grim reality is that we are not going to easily close the gap and erase the inequities caused by the current digital divide. In fact, because of differences in the level of education between the haves and have nots, it is generally expected that the poor will have less accessibility to computing power and Internet capabilities. For example, there are many more high-speed Internet connections within a city in developed and developing countries such as Singapore or New York than the entire state of an underdeveloped country or even the country itself such as Ethiopia. The evolution of the Internet itself may therefore have further widened the divide.
As we have noted, prior research in e-medicine has focused on a number of important themes discussed throughout this and other chapters of this text. Key research areas include the following:
- E-medicine services
- Technical aspects of e-medicine
- Cost-effectiveness of traditional medicine versus e-medicine
- Clinical effectiveness and satisfaction with mainstream medicine versus e-medicine
- Diffusion, implementation, and impact of e-medicine
Of these themes, the last is the least developed but will perhaps provide the most valuable insights into the future development of e-medicine. To develop a comprehensive design model for e-medicine services, further research needs to be completed on the implementation and installation of e-medicine services and their general effects. Very little research has been done on the implementation and installation of e-medicine services, especially in developing countries. The questions that need to be answered relate to the difficulties encountered with actual implementations and how these challenges can be overcome.
The main focus of this chapter will be e-medicine diffusion. Before we look at the diffusion of e-medicine in developed countries such as Canada and in developing countries such as those in sub-Saharan Africa, we will discuss the factors underlying the diffusion of e-medicine.
Factors Driving the Diffusion of E-Medicine
From our historical knowledge of e-medicine technologies and applications, we see that the diffusion of e-medicine is fueled by many factors, including growth in e-home care needs, new trends in consumer health informatics, changes in legislation, increased competition, market expansion, new technological breakthroughs, as well as other socioeconomic factors. Given an aging population, closures of hospital beds, and reduced inpatient stays for operative procedures, the market for e-health care is projected to grow rapidly. Advances in medical technologies and pharmaceutical products are making a wider range of diagnostic, therapeutic, and surgical procedures and services for e-home care possible (see Chapter Nine). New legislation and rising health care costs are forcing payers and administrators to seek new and innovative ways to provide adequate levels of services at lower costs (see Chapter Twelve). E-medicine appears to offer an intelligent solution for the redistribution of medical services especially among the unprivileged because they may be in more urgent needs of such services and promises to bring about new opportunities for increased competition and commercial partnerships in the expanding e-health marketplace (see Chapter Thirteen).
E-medicine represents a dramatic shift from traditional thinking about medicine, which focuses on transporting the patient to the site of the health practitioners. Instead, e-medicine transmits expert knowledge and know-how to patients and practitioners; simply put, it moves the information rather than the patient. E-medicine services have therefore been used partly to replace and augment face-to-face home care visits with teleconferencing and video visits for the chronically ill and elderly. E-home care telemonitoring of heart conditions and vital signs, including blood pressure; the use of laptop computers by e-home care workers to document, review, and check medication and progress on patient charts; the ability to e-communicate with home care teams; and emergency or alert systems linking homes with clinics or hospitals are all developments in e-medicine diffusion.
Increasingly, e-consumers are demanding high-quality and reliable health information of all sorts on the Internet. This demand has also strengthened the e-medicine model. Rapid access to the World Wide Web has enabled the diffusion of e-medicine expertise to individuals whose access to such services used to be restricted. Increasing sources of medical and health care information have also led to demand for better medical information and knowledge, faster and more efficient means of accessing evidence-based medicine electronically, and improved on-line medical bibliographic resources and health research networks.
E-home care needs and consumer health informatics are not the only factors contributing to the diffusion of e-medicine. Rapidly rising costs of health care and increased competition among health providers have also contributed. In this regard, the politics and economics of the managed care approach to health care delivery have become some of the most important factors driving the diffusion of the e-medicine perspective. In a managed care setting, a certain population within a geographic boundary is expected to be covered for medical services regardless of their geographic location. Insurance companies in many U.S. jurisdictions were at first unable to reimburse physicians for e-consultations and e-medicine services. In managed care, where the fee-for-service practice arrangement is no longer prevalent, e-medicine can play a much more significant role. In other words, in a competitive environment, e-medicine applications will be readily accepted by insurance companies if such use results in overall cost savings and increased market share for the e-health provider organizations.
Another important question about the diffusion of e-medicine is the way in which the market for e-medicine is developing. Perednia and Allen (1995) state that the market share of a product or service can be increased in two ways: (1) increasing the size of the total market—for example, by expanding the demand for bandwidth suitable for e-medicine applications; and (2) increasing market share through extensive marketing and product differentiation—for example, by offering e-services at a higher discounted rate for Internet services among seniors and the underserved. E-medicine applications create new demands not only by introducing new medical technologies but also by requiring faster and higher bandwidths. This is why many telecommunication carriers who control the distribution of bandwidth have also entered the e-medicine market; they have a vested interest in the widespread use of their products.
Finally, several other factors play a role in the promotion of e-medicine services, including direct and indirect costs related to obtaining health and medical care—for example, travel costs, time lost from work, and the mental stress of dealing with physical visits to obtain health care services. The e-medicine approach cuts down on duplication of services and paperwork; helps to reduce the number of harmful drug interactions and inappropriate prescriptions; improves public safety, security, health, and well-being; reduces patient and professional travels; speeds up availability and delivery of key patient information in emergency as well as non-emergency situations, and enables shorter hospital stays by integrating assisted home care and community services through e-networks (see also Chapters Four, Five, and Six). Advances in computer hardware and telecommunications, along with improved high-capacity storage technology, will soon permit the integration of different e-medicine applications within a single network. Ultimately, this will translate into new and expanded opportunities for e-medicine technology transfer and commercialization.
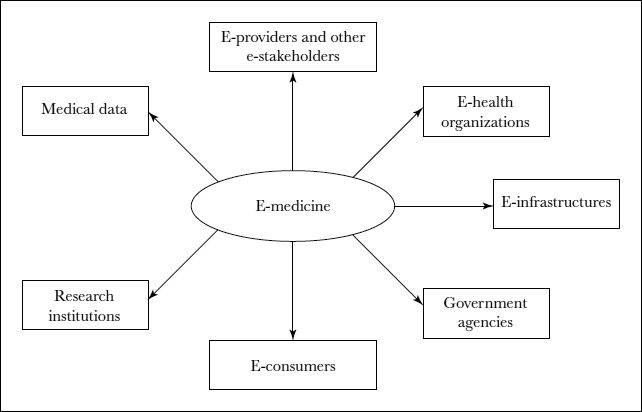
E-Medicine in Canada
In general, the technologies and systems used in e-medicine are designed to enable a two-way exchange of information between the general public on one hand and the health provider community on the other hand. The health care community essentially becomes an agent that gathers, processes, stores and disseminates data, information, and knowledge elements, using hardware and software components. These components include a device or mechanism for receiving signals; a means to transfer the information captured via communication or e-network technologies; and a device or mechanism for representing, storing, and presenting the output information (Industry Canada, 1998). Input signals can be represented in data, audio, or real-time video format, and output devices can include video monitors, computer file servers, and data recorders. Data, information, and knowledge elements collected and processed become valuable aggregated information or organized knowledge to be shared with the general public or for a specific purpose—for example, customized therapeutic interventions for a patient or a group of patients. While the general public provides most of the base data, instructions and critical information provided by experts will eventually be needed to sustain the health and well-being of the public. Figure 8.1 depicts this simple conceptualization of e-medicine as an exchange of information.
Despite the proliferation of new technologies and applications, Canada's e-medicine industry is still relatively small and underdeveloped. Canada has a land area of approximately 3.8 million square miles. The majority of Canadians live in urban cities located within 155 miles of the country's border with the United States, and the rest of the country is sparsely populated. Owing to the size of the country and the difficulties of traveling in remote areas due to geography and bad weather, Canadians need to develop expertise in e-medicine technology if Canada is to play a key role in the global e-health marketplace. In fact, Canada was one of the first countries to use telecommunications technology to assist in the delivery of health care. In 1956, a neurosurgeon in Saskatoon used closed-circuit television to transmit live electrocorticography tracings, and a Montreal radiologist pioneered teleradiology in 1958 (Elford and House, 1996).
FIGURE 8.1. E-MEDICINE AS AN INFORMATION CLEARINGHOUSE
Canada also launched its first domestic telecommunication satellite, Anik A-1, in 1972. From 1976 to 1982, the Federal Department of Communications sponsored a number of projects that evaluated the use of satellite technology for e-medicine. In these projects, although e-medicine was found useful, satellite systems were not found to be cost-effective. In the following ten years, although they participated in a few international e-medicine projects, Canadian researchers basically lagged behind. Lately, however, there appears to be renewed interest in e-medicine across Canada (Watanabe, 1998), perhaps due to the development of provincial and national infrastructures for the health information highway, as well as pressure to deliver health care at a lower cost and with increased technological capacity and speed (Wright, 1998).
One reason that the Canadian e-medicine industry has grown very slowly over the years is that many potential users still have little knowledge about or experience in this field. Medicolegal, ethical, and administrative concerns also inhibit the growth of e-medicine. For example, telephone triage systems allow nurse practitioners to provide health care advice over the telephone, but there are potential liability issues such as medication errors due to human transcription errors. However, it is not clear what the legal implications would be if medication errors occur either because of nurse giving wrong advice or the patient having heard wrongly. As Blair and others (1998) point out, the issues of licensing and regulatory requirements for practicing across jurisdictional boundaries; responsibility for clinical care decisions and medical malpractice insurance coverage; and standards of care are all influencing the determination of physicians to practice e-medicine. In addition to these concerns, a number of ethical issues in regard to the health professional–patient relationship—such as privacy, confidentiality, informed consent, and security of transmitted data—are emerging. The Center for Bio-ethics at the Clinical Research Institute in Montreal is studying these issues (Industry Canada, 1997).
There is also a paucity of research showing the value of health care delivered via e-medicine. As a result, there is a need to assess the effectiveness of care delivery using various e-technologies, as well as the cost-effectiveness of these applications. A number of initiatives that focus on these topics are being undertaken by the University of Calgary in Alberta as well as the University of Victoria in British Columbia (see Tan with Sheps, 1998, Chapters Fifteen and Sixteen). In the United States, the National Academy of Sciences' Institute of Medicine (IOM) has also called on researchers everywhere to strengthen the evidence base for e-medicine. Field (1996) has suggested an evaluation framework for e-medicine applications in Canada and the United States that is based on the criteria of quality, accessibility, cost, and acceptability of health care services.
The Canadian Network for the Advancement of Research, Industry and Education is a government-funded initiative to help develop a national high-speed network and information-based technologies for many sectors, including health care. One ambitious project is the formation of a nationwide Asynchronous Transfer Mode (ATM) network (see Chapter Six). For this project, seven regional high-speed networks will be linked. The province of Nova Scotia has just implemented an e-medicine network, and other provinces—such as Quebec, Alberta, New Brunswick, and Ontario—are following in Nova Scotia's footsteps. Coalitions of private companies such as STENTOR are also working closely with provincial governments across Canada to research and develop advanced telecommunication and networking technologies, with an emphasis on e-medicine applications.
The Canadian Institute for Health Information (CIHI) has identified the need for standards in e-medicine, including standards for health information security and privacy, for information exchange and applications, and for linking provincial health care information systems (Industry Canada, 1997). British Columbia's Ministry of Health has instituted the British Columbia Health Information Standards Council (BCHISC). Comprising many stakeholder representatives from health care agencies, universities, governmental agencies, and user communities, the BCHISC identifies standards and sets guidelines to promote the effective and efficient sharing of health information in British Columbia. Joseph Tan, the editor of this text, was a member of this council for three years, participating in provincewide meetings on health information standards and related issues. In collaboration with the CIHI, the BCHISC works to improve the flow of e-health information to support new initiatives in different parts of the health care sector, including e-medicine. Although British Columbia has one of the most automated provincial health systems, including an on-line billing system for practitioners, PharmaNet/BC, and HealthNet/BC, the province still faces several challenges in developing and implementing e-clinical and e-medicine applications. Major barriers to the adoption of e-medicine practices are unresolved issues of professional acceptance, the ability and desire to change current practices, and reimbursement.
Watanabe (1998) argues that e-medicine will succeed in Canada only if “its development responds primarily to the needs of the health care sector and not simply to the availability of technology.” The Health Association of British Columbia (HABC) has identified several key factors that are necessary for the successful implementation of e-medicine systems.
- Leadership from e-medicine champions in health care practice and government to build partnerships and a vision for the field
- A coordinating body with representation from all levels of the health care sector and from academia, industry, and government to provide harmonization of activities, a forum for communication, and act as a pool of information resources
- Government funding for the implementation, ongoing maintenance, and evaluation of innovative diffusion of technology in various regions
It is often exciting to cover e-medicine from the perspective of a developed country such as Canada because of the growing number of initiatives and activities that are developing as e-medicine moves to the forefront of health informatics. Yet the greatest needs for e-medicine technologies and applications are not in developed countries, where health care standards are usually established and citizens can expect a certain level of support for their health and wellness. Canada, for example, subscribes to the vision of universal health care, and all citizens, regardless of race, ethnicity, or religious beliefs, have equal rights to access the health care system. In developing countries, however, even basic infrastructures for health care may be lacking, so e-medicine strategies may be able to provide quality medicare conveniently available at reasonable costs. Therefore, we now turn our attention to a country where an understanding of the e-medicine diffusion process would be especially helpful in designing future e-medicine programs.
E-Medicine in Ethiopia
For the last decade, Ethiopia has been planning a long-term national health care strategy to increase the number of citizens receiving care and to decrease the subsequent health care costs. However, health problems such as HIV/AIDS and malaria, combined with high population growth rates (2.6 percent in 2002), have increased the demand for health care services and have resulted in more expensive treatments. Moreover, slow economic growth and funding of the health sectors have not kept up with these rising health care costs. This is true not only of Ethiopia but of most developing countries, especially in sub-Saharan Africa.
In addition to financial scarcity, the shortage of medical specialists in many developing countries has led to a high mortality of patients suffering from various diseases. In the specific case of Ethiopia, the country's inadequate transportation infrastructure and large geographical area makes it more difficult than usual to provide health care services in remote and rural areas, where 85 percent of the population lives. Where clinics and hospitals do exist, especially outside urban areas, they are often poorly equipped and below the standards set by the World Health Organization (WHO). In addition, extended drought and famine have resulted in food shortages, illiteracy, and poor socioeconomic conditions.
Nevertheless, buildings, medical equipment, medical staff, and drugs are essential to good health care and require a high level of investment. To meet this challenge, the Ethiopian government and its international donors must supplement the existing human, infrastructure, and financial resources with modern technology. E-medicine has been identified as a possible solution.
As we noted earlier in this chapter, e-medicine involves delivering health care using telecommunication equipment as simple as telephones and fax machines or as complex as Internet-connected personal computers with full-motion interactive multimedia (Huston and Huston, 2000). There is a critical need to better understand the factors affecting the diffusion of e-medicine in developing countries. Services such as teleradiology, teledermatology, telepathology, telecardiology, and tele-ophthalmology can be extended to underserved communities and individuals in both urban and rural areas. In addition, e-medicine can help attract and retain health professionals in rural areas by providing ongoing training and collaboration with other health professionals. Although e-medicine, like all information and communication technologies (ICTs), was developed and tested in developed countries, it has successfully addressed some medical problems in developing countries. However, many of these initiatives have been relatively small and isolated. Wright (1998) suggests that while developing countries' priorities in most cases may not be to finance e-medicine activities, despite their known potential, the governments of these countries could at least facilitate the provision and flow of medical information and health care, thereby reducing unnecessary health care expenditures (for example, providing online training of nurses and doctors on how to share information resources and use teleconsultations). Experience in the developed world demonstrates that most successful e-medicine applications require a change in the organization of health care delivery.
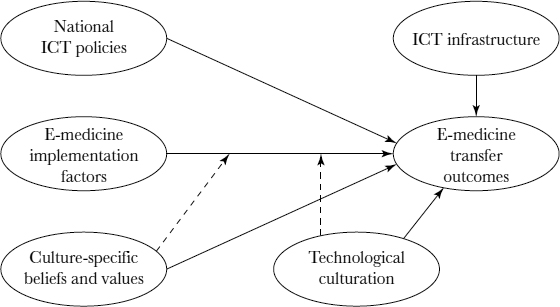
We address the lack of understanding of e-medicine diffusion in developing countries by focusing on a conceptual framework to measure e-medicine transfer outcomes relating to information technology, people, cultures, economics, and the social setting. The framework measures four areas: (1) ICT policies; (2) ICT infrastructure; (3) e-medicine implementation; and (4) culture-specific beliefs and values, and technological culturation. In explaining the framework, we present supporting arguments and insights on issues surrounding the diffusion of e-medicine in Ethiopia. We also highlight implications for research, practice, and other application domains.
Background on Ethiopia
Located in the horn of Africa, Ethiopia is the second most populous country in sub-Saharan Africa, with a population of 67.3 million. The country is made up of more than eighty ethnic groups who speak more than eighty languages. Ethiopia is not only populous, but it is a geographically large country (slightly less than twice the size of Texas). The geography and lack of transportation infrastructure is challenging. Eighty-five percent of the population is rural, with agricultural production as their primary livelihood activity. Ethiopia is bounded on the north by Eritrea, on the east by Djibouti and Somalia, on the south by Kenya, and on the west by Sudan. The country is among the poorest in the world, with an annual income of less than $100 U.S. per capita, 51 percent health coverage, 19 percent and 40 percent literacy rate among women and men, respectively, and a life expectancy of 43.4 years. The country scores low in almost all social and economic indicators. For example, in 2001, it ranked 158th out of 162 countries on the global human development index.
Social poverty is on the rise; the majority of the population does not have access to education, health care, or safe water. The high prevalence of HIV/AIDS and malaria has also put a significant pressure on the economy and the social infrastructure. Nevertheless, the Ethiopian government's openness to improving the situation, focusing on long-term development through agricultural development–led industrialization, has resulted in some prospects for increased productivity, improvement of rural infrastructure, growing private investments, and mobilization of external resources such as financial aids from other developed countries. The focus on rural areas and small households has led to expansion of agricultural extension in the sense of improved technology and credit schemes, primary education, primary health care, rural water supply projects, and rural roads. For example, the gross enrollment in primary education increased from 35 percent of eligible children in 1990 to 46 percent in 2000.
The health care infrastructure is spread thin and poorly equipped. Health care facilities, in the relatively few locations where they exist, are usually overcrowded and in need of physical repair. The human capacity problem is perhaps even more serious. There is one doctor for every 36,000 Ethiopians, and those doctors tend to be concentrated in Addis Ababa and the major towns. Ethiopia has three schools of medicine, 87 hospitals with less than 12,000 total beds, 257 health centers, and 196 private clinics. Although Ethiopia's medical schools are turning out trained personnel, too many graduates (about 60 percent) leave after their required in-country service due to low pay, difficult working conditions, lack of opportunities for professional development, and insufficient autonomy. For example, the International Organization for Immigration ranked Ethiopia first among African countries in the number of emigrant medical professionals.
Ethiopia is a typical developing country; its large proportion of children reflects high fertility rates and low life expectancy. The mortality rate for infants and those under the age of five started to decrease at the beginning of 1990s, but no further progress was recorded in later years. This may be due to the fact that HIV/AIDS is killing many children. Ethiopia has the lowest health progress in the region and around the globe, due to drought and famine, civil war, poor government, and political instability. Ethiopia has also the highest maternal mortality ratio in the world (800 per 100,000 live births), due to poor health infrastructure, scarcity of medical professionals and low rates of female education. Ethiopia is greatly affected by the HIV/AIDS epidemic, third in the world after only South Africa and India. Not only is this a serious health problem, but it is also becoming a developmental, social, psychological, and political problem. The problem is still increasing because of a lack of behavioral and lifestyle changes along with poor, voluntary counseling and testing. AIDS is sending Ethiopia's development backward and making a poor country even poorer.
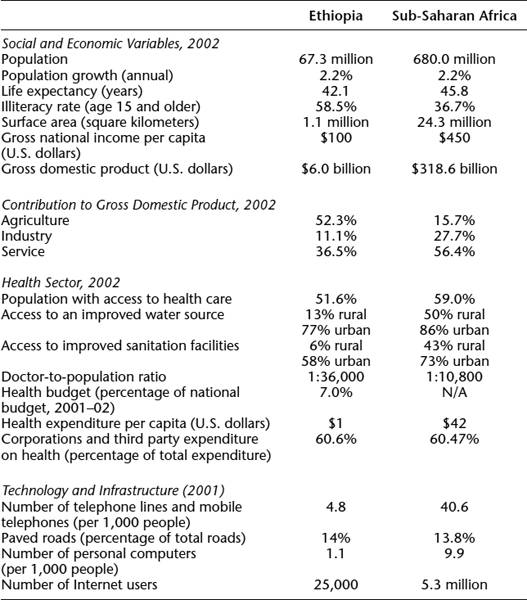
Despite the obstacles, Ethiopia's health care spending has been increasing, particularly since the launch of the health sector development program in 1997. The total spending on health increased from 1 percent of gross domestic product (GDP) in 1992–93 to 1.4 percent in 1996–97. It then dropped back to 1 percent before it picked up to 1.8 percent and 2.1 percent of GDP in 2000–01 and 2001–02, respectively. A moderate increase in health accessibility has been recorded, from 49 percent in 1995–96 to 52 percent in 2000–01. Table 8.1 shows the major comparative socioeconomic and health indicators of Ethiopia and sub-Saharan Africa.
Experts believe that the social and economic woes of Ethiopia are far from being resolved. Concerted efforts must be made to think out policies and strategies based on objective evaluation of the causes of rampant poverty, taking global dynamics into account. Agriculture, which contributes more than 50 percent of GDP, cannot save the country from poverty. Experts have argued that efforts should focus on untapped potentials such as tourism and ICTs. Introducing ICTs into health care services offers opportunities to improve the quality of care. Applications of ICTs not only will provide opportunities for Ethiopia to participate in the global economy but are also important in increasing people's ability to learn and change behavior.
The Ethiopian government has also shown its readiness to consider developing ICT policies and programs in order to address challenges in socioeconomic development. A broad-based national ICT policy development initiative began in early 1997. The first draft of an ICT policy was developed by a team of experts in June 2001 following a national workshop in November 1999. In early 2002, the Council of Ministers adopted the ICT policy, which emphasizes the need to harness ICTs in the health sector and build the necessary infrastructural capacity. The policy also discusses needs for human resource development and for building and strengthening institutions. A general description of ICT for health in Ethiopia is provided in Table 8.2.
E-medicine has been identified as a possible solution to some of Ethiopia's medical problems. Lessons from sub-Saharan African countries include some established standard practices for e-medicine diffusion (Mbarika and Okoli, 2003). E-medicine has already successfully addressed some clinical applications in Ethiopia, such as tele-ophthalmology, telecardiology, teleradiology, telepathology, and teledermatology. Following is a description of a teledermatology project.
TABLE 8.1. MAJOR SOCIOECONOMIC AND HEALTH INDICATORS OF ETHIOPIA AND SUB-SAHARAN AFRICA
Note: N/A = not applicable.
Sources: World Development Indicators Database, August 2003; WHO/UNICEF Joint Monitoring Program, 2001; African Human Development Indicators—United Nations Development Program, 2001.
TABLE 8.2. INFORMATION AND COMMUNICATION TECHNOLOGY FOR HEALTH IN ETHIOPIA
Positive Factors
|
Negative (Inhibiting) Factors
|
Source: SCAN-ICT Baseline Studies UNECA (Information and Communication Technologies, 2003).
In 1998, the Telecommunications Development Bureau (BDT) of the International Telecommunications Union (ITU) launched its first e-medicine project in sub-Saharan Africa. The connecting sites are the Tikur Ambessa hospitals, the Faculty of Medicine in Addis Ababa, and ten rural hospitals. The project was set up by a multidisciplinary group of partners that included the national e-medicine committee in close collaboration with domestic and international partners, including the WHO, European Community, United Nations Educational Scientific and Cultural Organization, E-Health Solution, WorldSpace, Tokai University of Japan, Addis Ababa University, Ethiopian Telecommunication Cooperation, and the Ethiopian Telecommunication Agency.
The project uses standard low-cost equipment, including e-networking via servers, digital cameras, and color scanners; e-medicine software; and telecommunication interfaces installed at the central studio and the remote hospitals. The Internet is used to connect hospitals, forming an e-medicine information network. The primary health care units will use e-mail to give the rural sites access to doctors' advice.
The teledermatology link between the teaching hospitals of Tikur Ambessa and ten regional secondary care hospitals throughout the country. The link allows the regional hospitals to exchange digital and video images of patients in rural areas who are suffering from skin disorders and then to send them, via the Internet, to doctors in the regional capital of Tikur Ambessa. The doctors consult among themselves and forward advice on treatment. These procedures considerably reduce patients' waiting time from six months to less than one week, and they also reduce unnecessary travel to a referral hospital. In addition, teledermatology has increased access to specialist health care.
Although these initial successes are promising, the projects are still relatively small and isolated. There is a critical need to better understand the factors affecting e-medicine transfer outcomes learned from the experience of other developed countries. In the next section, we present an ICT framework, identify and speculate on some of the positive and negative factors that have been found to influence e-medicine diffusion, and apply this thinking to Ethiopia.
Factors Affecting the Diffusion of E-Medicine in Ethiopia
For more than fifteen years, clinicians, health services researchers, and others have been investigating the use of ICTs to improve health care. E-medicine, representing an integration of the practice of medicine with the innovative applications of ICTs, is one area of such investigation. By drawing knowledge from various sources in technology diffusion research, we hope to develop an understanding of key factors that determine e-medicine transfer outcomes in a developing country.
Issues of technology transfer—that is, moving a given technology from creators to users—have been studied extensively, and the findings reveal major challenges, even in developed countries. Kwon and Zmud (1987), for example, argue that these challenges include difficulties in new technology implementation, which sometimes ends in failure. The problems become exacerbated when such transfers are attempted from developed to developing countries with significantly different socioeconomic and cultural environments.
We have identified four critical factors of e-medicine transfer to Ethiopia:
- National ICT policies
- ICT infrastructure
- E-medicine implementation factors
- Culture-specific beliefs and values and technological culturation—that is, cultural differences between the makers of the technologies, based in developed countries, and the users of the technologies, based in developing countries
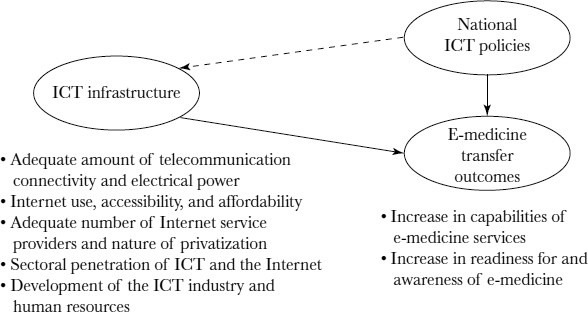
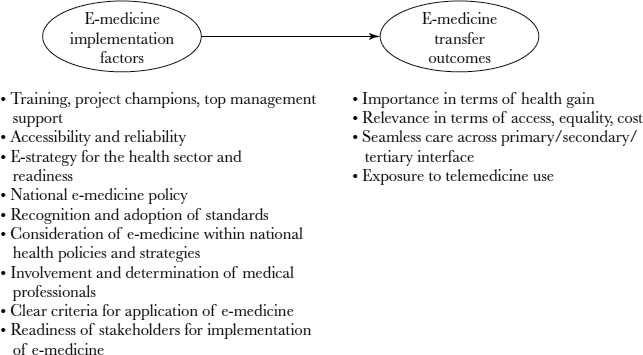
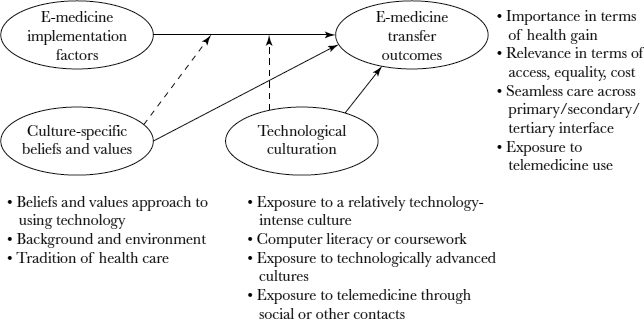
Figure 8.2 depicts the impact of various constructs on e-medicine transfer outcomes. Some of these relationships are positive, while others are negative.
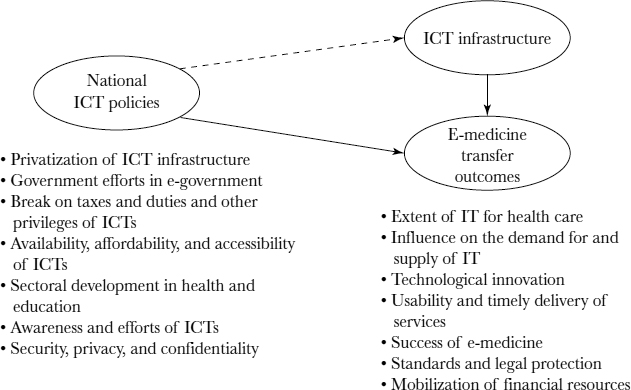
National ICT Policies.
National ICT policies are both general policies and specific health and security policies tailored to e-medicine. Government policies have been found to be highly instrumental in the diffusion of computing within a society (Gurbaxani and others, 1990). In Ethiopia, the formulation and implementation of policies in the ICT sector is still very rudimentary. An integrated set of laws, regulations, and guidelines to shape the generation, acquisition, and utilization of ICTs does not yet exist. Nonetheless, the government controls most of the ICT infrastructures and upholds policies that influence the acquisition and use of these infrastructures by private organizations. Policies such as these, which encourage computer ownership and investment, encourage the transfer of ICT to all segments of the population.
FIGURE 8.2. CONCEPTUAL FRAMEWORK OF ISSUES IN TELEMEDICINE TRANSFER IN ETHIOPIA
Another aspect of ICT policy issues in Ethiopia is privatization of ICT infrastructures. In Ethiopia, the government owns and manages the telecommunications operator that provides phone lines for Internet, fax, and e-mail access, which are important infrastructures for the transfer of e-medicine technologies. However, because Ethiopian government policies forbid or restrict privately owned telecommunication and Internet service provider services, lack of competition makes such services expensive and usually poor in quality. Hence, a policy that is not specific to e-medicine significantly affects e-medicine transfer through its effect on ICT infrastructures.
Like other health care systems, the health care system in Ethiopia deals with very sensitive and private data. Given that these data systems are increasingly interoperable yet the primary demands are that the data be correct, not corrupted, relevant, complete, and accessible only to authorized persons, the data systems must be secure. This gives rise to the need to address technological, legal, regulatory, ethical issues not only within a national context but also at the international level. A key strategic issue in any health care system is the technical, communications, and data standards, although in most instances these standards are not specifically directed at health care.
Figure 8.3 depicts the impacts that national ICT policies can have on e-medicine transfer outcomes.
Based on our understanding of national ICT policies in Ethiopia, we propose the following national policy directions in order to effect positive e-medicine transfer outcomes:
- Policies that favor the development of ICTs, to increase the level of ICT infrastructures and increase e-awareness in society, thereby encouraging foreign investment
- Policies that favor the development of e-health and technical standards and favor legal protection of providers
- Policies that favor the development of security, confidentiality, and privacy measures
ICT Infrastructures.
ICT infrastructures are the telephone and telecommunication infrastructures, the information technology (IT) sector, electrical power, the Internet, and the extent of ICT penetration and ICT industry that facilitates data and image communications.
To enable the use of e-medicine, a country needs a solid ICT infrastructure. In the past, telecommunications infrastructure has usually been measured in terms of teledensity, the number of telephone landlines per capita (for a review, see Mbarika, Musa, McMullen, and Byrd, 2002). However, with the spread of wireless telecommunications, a broader perspective should be taken in identifying ICT infrastructure. Figure 8.4 depicts the impacts that ICT infrastructure can have on e-medicine transfer outcomes.
FIGURE 8.3. EFFECTS OF NATIONAL ICT POLICIES ON E-MEDICINE TRANSFER OUTCOMES
FIGURE 8.4. EFFECTS OF ICT INFRASTRUCTURE ON E-MEDICINE TRANSFER OUTCOMES
Due to various socioeconomic and political problems, Ethiopia has been reported to have the lowest levels of most types of ICT-related infrastructures in the world (Goodman, 1991; Mbarika, 2001; Mbarika, Byrd, McMullen, and Musa, 2002; Mbarika, Byrd, and Raymond, 2002). Ethiopia's ICT infrastructure problems include a huge gap between supply and demand; a strong distribution imbalance that favors urban over rural areas; poor-quality service; long waiting times for new services; and peak traffic demands that exceed network capacity (Mbarika, 2001). One result is an extremely low level of basic telephone penetration: less than one phone line per 100 people (International Telecommunications Union, 2001).
Three aspects of how ICT infrastructures affect e-medicine diffusion should be addressed: (1) what ICTs are currently being employed in the practice of e-medicine; (2) what other ICTs could be employed in this effort; and (3) what enhancements to current infrastructures are necessary to enable other e-medicine practices. We propose that the following factors will have favorable impacts on e-medicine transfer outcomes in Ethiopia:
- More advanced and available telecommunication and electrical power infrastructure
- A more advanced and available IT sector
- More penetration of ICT in the health and IT sectors
- More advanced and available Internet infrastructure
Implementation Factors.
E-medicine implementation factors include the involvement of technology champions or institutions, e-medicine policy, interoperability, e-standards, e-awareness, e-readiness, and e-acceptance.
Figure 8.5 depicts the potential impacts of key implementation factors on e-medicine transfer outcomes (Checchi, Sevcik, Loch, and Straub, 2002; Mbarika and Byrd, in press; Rogers, 1983).
Information systems researchers have identified a number of implementation factors for ICTs in general, including user training, project champions, and top management support (Checchi, Sevcik, Loch, and Straub, 2002; Culnan, 1986; Kwon and Zmud, 1987; Loch, Nelson, and Straub, 2000; Lucas, 1978; Robey and Zeller, 1978; Rogers, 1983). Traditionally, information system introduction failures are correlated with how the systems were implemented. For example, after researching user training in sub-Saharan Africa, Aynu, Okoli, and Mbarika (2003) argue that ICT training or human capacity development can play an important role in structuring sustainable ICT transfer. They further argue that although the development of ICT infrastructure is a fundamental need for effecting sustainable economic development in Ethiopia, the presence of substantial infrastructure is insufficient to yield economic development without the trained human capital to effect this conversion.
FIGURE 8.5. EFFECTS OF E-MEDICINE IMPLEMENTATION FACTORS ON E-MEDICINE TRANSFER OUTCOMES
Factors that specifically affect e-medicine implementation include policies that maintain e-medicine initiatives, integration of e-medicine into mainstream health care services, and interoperability standards at all levels including technical, human, and operational. Many interfacing standards—for example, Health Level Seven (HL7), Digital Imaging and Communications in Medicine (DICOM), picture archiving and communication systems (PACS), ITU telecommunication standards (the H320 family), International Organization for Standardization standards (ISO 9000)—as well as safety regulations must be considered. In addition, relevant clinical application criteria such as health gain, volume, cost, access, and equity can all influence e-medicine implementation. Further, human factors—mainly awareness and acceptance of technology as well as willingness and e-readiness on the part of stakeholders—can also contribute to implementation success.
While efforts have been made to assess the level of a community's e-readiness, including issues of digital divide, based on available indicators (Dutta, Lanvin, Paua, and Cornelius, 2003), much information is still lacking on issues such as ICT use and health. However, it seems safe to assume that assisting a country's e-readiness will help maintain and develop the implementation of e-medicine.
We propose that the following implementation factors will have positive impacts on e-medicine transfer outcomes in Ethiopia:
- Factors that favor e-readiness and e-medicine implementation in general
- National health policies that favor the development of e-medicine
- Stakeholder awareness of, readiness for, and acceptance of the use of e-medicine services
- The presence of criteria for selecting clinical applications
- Clinical applications that have matured in technologically advanced nations
- Clinical applications that involve medical images
Culture–Specific Beliefs and Values and Technological Culturation.
Culture-specific beliefs and values refers specifically to the effects of practitioner and patient attitudes toward e-medicine implementation, while technological culturation has to do with the influence of technologically advanced cultures on an individual's attitude toward technology. Culture is a complex notion that is usually assessed in terms of multiple variables. Its potential impact on e-medicine transfer outcomes in Ethiopia is shown in Figure 8.6.
Culture is a system of attitudes and traditions that are transmitted from one generation to another through learning. The health sector must take into account the issues of an individual's ethnic and cultural context. The poverty in Ethiopia means that many people simply cannot afford to expect, let alone demand a basic standard of health care. As a result, there is no standard of care, or the existing standard of care is inaccessible to the public at large. In summary, the health care situation in Ethiopia encompasses vulnerability marked by increasing poverty, and primitive sociocultural traditions with high illiteracy such as the dependency on village chiefs or priests rather than medical doctors to provide a cure; little health care treatment is therefore available. Participating in a clinical trial may be considered a privilege because trial patients are given the benefit of significantly better health care than the rest of the population.
Two levels of beliefs and values should be considered in e-medicine diffusion. On an individual basis, the issue is a person's beliefs and attitudes toward treatment providers and health care institutions. From an organizational standpoint, the focus is on a social system that involves different physician group behaviors as well as outcomes and performance of the wider health system. The nature of e-medicine is in networks—networking of both people and technology. Networking works well with developed power structures in which people have clear roles and responsibilities.
In Ethiopia, there are no clear job descriptions for physicians or other workers. Beliefs and values ingrained in people by their cultural context significantly affect their thinking and perspective, including their approach to using technology, for example, a stubborn preference for face-to-face interactions. In Ethiopia, as elsewhere, physicians working in an organization are often subject to cultural shock when networks replace hierarchies and when relationships become predominantly contractual rather than collegial. Hence, fear of change becomes a major factor in how physicians in Ethiopia may react to a specific project or need. It is easy to see that cross-cultural analyses are important in planning e-medicine systems, because what may work in one culture may not be appropriate in another.
FIGURE 8.6. EFFECTS OF CULTURE ON E-MEDICINE TRANSFER OUTCOMES
Straub and others (2002) divided the construct of “culture” into two subconstructs:
- Culture-specific beliefs and values that a person might hold because of the influence of their cultural background
- Technological culturation, which describes a person's exposure to a relatively technology-intense culture
In the context of studying ICT diffusion in developing countries, technological culturation could indicate the degree to which a citizen of a developing country has been exposed to more technologically advanced cultures (Checchi, Sevcik, Loch, and Straub, 2002). Specifically looking at technology adoption at the individual level of analysis, McCoy (2002) tested a comprehensive model of the moderating effects of national and cultural dimensions on technology transfer. Researchers (for example, Checchi, Sevcik, Loch, and Straub, 2002; Straub and others, 2002; Straub, Loch, and Hill, 2001) have found that both of these cultural subconstructs have a mediating effect on ICT implementation. Put simply, beliefs, values, and technological culturation affect the effectiveness of ICT implementation, in addition to their direct effects on ICT outcomes.
Based on the above analysis, we identify the following cultural effects on e-medicine transfer outcomes in Ethiopia:
- Culture-specific beliefs and values consistent with e-medicine practice in technologically advanced nations will yield favorable outcomes.
- Social culture and behavior consistent with risk assessments, care-seeking experiences, and medical decisions within e-medicine practice will positively affect outcomes.
- Taking patient preferences and knowledge into account and building patient-provider relationships within the health service will yield favorable outcomes.
- Technological culturation of citizens will enhance the favorable effect of e-medicine implementation factors on transfer outcomes.
Research on the Diffusion of E-Medicine in Developing Countries
The study of e-medicine diffusion in developing countries should focus on national ICT policies, ICT infrastructures, e-medicine implementation factors, culture-specific beliefs and values, and technological culturation. National ICT policies reflect the aspirations of government policymakers in prioritizing ICT for national development. They reflect both general ICT policies and those specific to e-medicine. ICT infrastructures include computers, telephones, wireless networks, and telecommunication infrastructures that facilitate communications and data collection and storage. We expect both national ICT policies and ICT infrastructures to have a direct effect on e-medicine transfer outcomes, and we also expect national ICT policies to also have a direct effect on ICT infrastructure. E-medicine implementation factors refer to a set of antecedents, such as training; health policies; selection of e-medicine applications based on accessible technologies and needs; e-awareness; e-acceptance; e-readiness; and e-management support. This set of factors affects the effectiveness of e-medicine transfer. In regard to culture-specific beliefs and values and technological culturation, our analysis shows that cultural factors affect e-medicine transfer directly and also through their moderating effect on e-medicine implementation.
E-medicine outcome measures for projects in developing countries, like outcome measurements for any health technology or service, are essential for several reasons. Reviewing outcomes gives government policymakers the opportunity to form new insights into the effectiveness of various national ICT policies on e-medicine transfer to developing countries. Such insights could help policymakers fine-tune their policies in a bid to encourage further e-medicine investments by stimulating infrastructure development, increasing financial resources, mobilizing e-medicine programs, reducing policy barriers, as well as informing health managers about the feasibility, cost-effectiveness, and acceptability of clinical e-medicine and helping those who have invested in e-medicine identify problems and improve programs.
E-medicine infrastructure providers, such as equipment manufacturers and service providers, need an understanding of where the needs are and how best to base organizational practices strategically for both local and multinational organizations. For example, e-medicine equipment manufacturers (which are mostly based in Europe and North America) can develop systems that fit within the cultural and educational context of developing countries.
The requirements for e-medicine in developing countries are not the same as in developed countries, and the telecommunication infrastructure and resources also vary dramatically. The greatest need for e-medicine is in countries where a majority of rural community residents are deprived of efficient health services due to their location. For example, in Ethiopia there is a digital divide between the capital region and the rest of the country. Addis Ababa is comparatively well equipped with ICTs, but the rural areas are generally cut off from most information and communication facilities.
Moreover, four major trends are driving the need for and increasing the significance of ICTs in the health care sector for developing nations: (1) the need to curtail health care costs in general; (2) infectious diseases such as HIV/AIDS and malaria, with their more treatment dependent patients and higher care needs; (3) increasing focus on preventive care; and (4) political changes in the structure of health care systems. E-medicine may not solve all medical problems, and technical, clinical, organizational, behavioral, and cultural obstacles to e-medicine technologies will remain, as will policy impediments and uncertainties related to reimbursements, standards, security measures, licensure, medical liability, and other concerns. However, research on the transfer and diffusion of e-medicine is a starting point in efforts to reach Africans who live in areas with limited medical facilities and personnel. E-medicine research with a focus on developing countries could have far-reaching positive outcomes.
Conclusion
Rogers' studies revealed five major characteristics of an innovation that affect its diffusion: the innovation's relative advantage, its compatibility with mainstream technology, its complexity, the ability to apply the innovation, and the opportunity to effectively observe the innovation (Rogers, 1983). In the case of e-medicine, the diffusion process will affect not just individuals, groups, and communities but countries and continents. Hence, in addition to the significance of e-medicine's technological characteristics, we must also become aware of individual, group, community, and national characteristics, communications, and contextual factors (such as regulations and economics).
Chapter Questions
- What is meant by diffusion of e-medicine? What is the significance of studying the diffusion process in the context of evolving e-health systems and environments?
- How does e-medicine development in the United States and the United Kingdom compare with that in Canada?
- What can developing countries learn from the diffusion process of e-medicine in developed countries? What differences between developed and developing countries should be considered when implementing e-medicine as a system of knowledge transfer?
- In what ways is the diffusion of e-medicine similar in developed and developing countries? In what ways is it different? What are the reasons for these differences?
- What do you think are the critical success factors for e-medicine diffusion in a country such as the one you live in? Have any of these factors changed over the years?
- Imagine that you are the minister of health for a large geographical region. You have been allotted a large sum of investment money to develop e-medicine in your area. How would you go about planning, designing, and evaluating the success of an e-medicine program—for example, a tele-ophthalmology program?
References
Aynu, B., Okoli, C., & Mbarika, V.W.A. (2003, June 8–10). IT training in Sub-Saharan Africa: A moderator of IT transfer for sustainable development. Paper presented at the 4th Annual Global Information Technology Management World Conference, Calgary, Canada.
Barrett, J. E., & Brecht, R. M. (1998). Historical context of telemedicine. In S. F. Viegas & K. Dunn (Eds.), Telemedicine: Practicing in the information age (pp. 9–17). Philadelphia: Lippincott-Raven.
Bashshur, R. L. (1997). Telemedicine and the health care system. In R. L. Bashshur, J. H. Sanders, & G. W. Shannon (Eds.), Telemedicine theory and practice (pp. 5–36). Springfield, IL: Thomas.
Blair, P., Bambus, A., & Stone, T. H. (1998). Legal and ethical issues. In S. Viegas & K. Dunn (Eds.), Telemedicine: Practicing in the information age (pp. 49–60). New York: Lippincott-Raven.
Checchi, R. M., Sevcik, G. R., Loch, K. D., & Straub, D. W. (2002, December 1–3). An instrumentation process for measuring ICT policies and culture. Paper presented at the International Conference on Information Technology, Communications and Development, Kathmandu, Nepal.
Culnan, M.J. (1986). The intellectual development of management information systems, 1972–1982: A co-citation analysis. Management Science, 32(2), 156–172.
Dutta, S., Lanvin, B., Paua, F., & Cornelius, P. (2003). The global information technology report 2002–2003: Readiness for the networked world. Oxford, England: Oxford University Press.
Elford, R., & House, M. (1996). Telemedicine experience in Canada (1956–1996). Report of the Congress International Conference, Montreal, Canada. St. John's, Canada: Telemedicine Centre, Faculty of Medicine, Memorial University of Newfoundland.
Field, M. (1996). Telemedicine: A guide to assessing telecommunications in health care. Washington, DC: National Academy Press.
Goodman, S. E. (1991). Computing in less-developed countries. Communications of the Association for Computing Machinery (CACM), 34(12), 25–29.
Gurbaxani, V., Kraemer, K. L., King, J. L., Jarman, S., Dedrick, J., Raman, K. S., & Yap, C.S. (1990). Government as the driving force toward the information society: National computer policy in Singapore. Information Society, 7(2), 155–185.
Huston, T., & Huston, J. (2000). Is telemedicine a practical reality? Communications of the ACM, 43(6), 91–95.
Industry Canada. (1997). Telehealth in Canada: Challenges on the road ahead. Retrieved from http://strategis.ic.gc.ca
Industry Canada. (1998, September 18). The definition, many applications. Retrieved from http://strategis.ic.gc.ca
Information and Communication Technologies (ICT) Team of the Development Information Services Division (DISD), Third Meeting of the Committee on Development and Information (CODI 3), Addis Ababa, Ethiopia, from April 10-17, 2003.
International Telecommunications Union. (2001). African telecommunication indicators. Geneva, Switzerland: International Telecommunication Union.
Kwon, T. H., & Zmud, R. W. (1987). Unifying the fragmented models of information systems implementation. In R.J. Boland & R. A. Hirscheim (Eds.), Critical issues in information systems research (pp. 227–251). New York: Wiley.
Loch, K., Nelson, G., & Straub, D. W. (2000). NSF project summary: IT transfer to Egypt: A process model for developing countries. Unpublished manuscript.
Lucas, H. C. (1978). Empirical evidence for a descriptive model of implementation. MIS Quarterly, 2(2), 27–41.
Mbarika, V.W.A. (2001). Africa's least developed countries' teledensity problems and strategies. Yaoundé, Cameroon: ME and AGWECAMS.
Mbarika, V.W.A., & Byrd, T. A. (in press). Stakeholders' perceptions of strategies to improve the technological infrastructure for e-commerce in Africa's least developed countries. European Journal of Information Systems.
Mbarika, V.W.A., Musa, P., McMullen, P., & Byrd, T. A. (2002). Teledensity growth constraints and strategies for Africa's LDCs: “Viagra” prescriptions or sustainable development strategy? Journal of Global Information Technology Management, 5(1), 25–42.
Mbarika, V.W.A., Byrd, T. A., & Raymond, J. (2002). Growth of teledensity in least developed countries: Need for a mitigated euphoria. Journal of Global Information Technology Management, 10(2), 14–27.
Mbarika, V.W.A., Byrd, T. A., Raymond, J., & McMullen, P. (2001). Investments in telecommunications infrastructure are not the panacea for least developed countries' leapfrogging growth of teledensity. International Journal on Media Management, 2(1), 133–142.
Mbarika, V.W.A., & Okoli, C. (2003, January 6–9). Telemedicine: A possible panacea for sub-Saharan Africa's medical nightmare. Paper presented at the 36th Hawaii International Conference on System Sciences, Waikoloa Village, Hawaii.
McCoy, S. (2002). The effect of national culture dimensions on the acceptance of information technology: A trait based approach. Unpublished doctoral dissertation, University of Pittsburgh, Pittsburgh, PA.
Perednia, D. A., & Allen, A. (1995). Tele-medicine technology and clinical applications. Journal of the American Medical Association, 273(6), 483–488.
Robey, D., & Zeller, R. L. (1978). Factors affecting the success and failure of an information system for product quality. Interfaces, 8, 70–75.
Rogers, E. M. (1983). Diffusion of innovations. New York: Free Press.
Straub, D. W., Loch, K. D., Evaristo, R., Karahanna, E., & Srite, M. (2002). Toward a theory based definition of culture. Journal of Global Information Management, 10(1), 13–23.
Straub, D. W., Loch, K. D., & Hill, C. E. (2001). Transfer of information technology to developing countries: A test of cultural influence modeling in the Arab world. Journal of Global Information Management, 9(4), 6–28.
Tan, J., with Sheps, S. (1998). Health decision support systems. Sudbury, MA: Jones & Bartlett.
United Nations Development Program (UNDP). (2001). The World Development Report—African Human Development Indicators. New York: Author.
Viegas, S. F. (1998). Past as prologue. In S.F. Viegas and K. Dunn, (Eds.), Telemedicine: Practicing in the information age (pp. 1–8). Philadelphia: Lippincott-Raven.
Watanabe, M. (1998). Telehealth in Canada [Editorial]. Telemedicine Journal, 4(3), 197–198.
World Development Indicators Database, World Bank, Washington, DC. August 2003; WHO/UNICEF Joint Monitoring Program, New York, 2001; African Human Development Indicators—United Nations Development Program, 2001.
Wright, D. (1998). Telemedicine and developing countries. Journal of Telemedicine and Telecare, 4(2, Suppl.), 1–88.
E-Medicine Development in Taiwan Case
Paul Jen-Hwa Hu, Chih-Ping Wei, Tsang-Hsiang Cheng, Joseph Tan
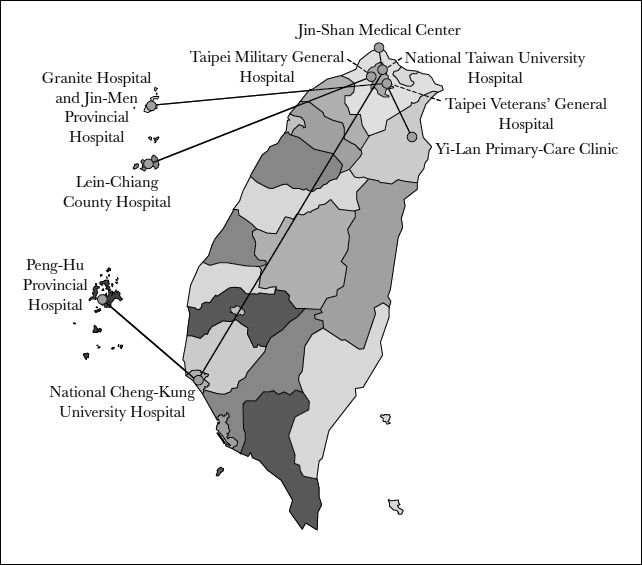
E-medicine is an essential form of e-health, as is indicated by its inclusion as a core application in the Taiwan's National Infrastructure Initiative (NII), which was launched in 1995, and in similar national initiatives, including the National Broadband Experimental Network. Technology-enabled e-medicine allows service delivery and collaboration beyond geographic and temporal barriers. Government participation, particularly that of the Department of Health (DoH), Taiwan's supreme health authority and policymaker, is critical to the dissemination of e-medicine. According to DoH, the overarching goal of e-medicine in NII is to design, establish, and evaluate a wide array of services that jointly constitute a nationwide infrastructure for remote diagnosis and e-patient management.
The diffusion of e-medicine programs has been initiated and propelled chiefly by leading acute tertiary care centers and teaching hospitals, including the National Taiwan University Hospital, the Taipei Veterans' General Hospital, and the Taipei Military General Hospital. Initial motivation for e-medicine programs included enhancement of access to services and quality of care, particularly through vertical service integration that connects care providers in primary, secondary, and tertiary care sectors. Over time, additional services and support activities have been incorporated, including support for e-clinical training and continuing education.
At the time that this case study was completed, all existing programs were still largely in an experimental stage. In spite of adequate technology bases, the continued operation and services of most of these programs is greatly dependent on external resources and the voluntary participation of individual physicians and specialists, technologists, and academic or clinical researchers. While these programs have demonstrated clinical value and resulted in encouraging evaluations of the technical feasibility of e-medicine for patient care and service collaboration, efforts to make the transition from the current experimental stage to real-world clinical settings raise important challenges in program management. As Perednia and Allen (1995) commented, the ultimate success of an e-medicine program requires an adopting organization to address key challenges pertinent to both technology and management.
Major E-Medicine Programs in Taiwan
In 1995, the DoH released the first national blueprint for e-medicine in Taiwan, high-lighting the use of adequate and available information and telecommunication technologies to enhance service accessibility, quality, timeliness, and cost-effectiveness. Both horizontal service extension to remote areas and vertical care integration to seamlessly connect care providers in the primary, secondary, and tertiary care sectors were identified as important e-medicine applications. Support for nonclinical services or activities was also emphasized. With partial funding by NII, the DoH provided pilot e-medicine programs with financial assistance for technology acquisition. Technologies supporting both synchronous and asynchronous services were targeted.
Videoconferencing systems with multimedia capability were commonly used with synchronous services, including real-time patient assessment, e-diagnostic services, and e-consultation. On the other hand, medical imaging transmission and display systems and electronic patient record systems were used with asynchronous services or consultations. A review of the services rendered found a mix of diagnostic, prognostic, and consultation services using medical images, particularly in such specialty areas as neurology, dermatology, and internal medicine.
Exhibit 8.1 highlights the major e-medicine programs in Taiwan. As shown in the exhibit, most Taiwanese e-medicine programs are based in Taipei, with the exception of the program housed at National Cheng-Kung University Hospital. All existing programs share an emphasis on enhanced patient care and management through vertical service integration. Typically, the e-medicine programs are housed at and managed by a tertiary or teaching hospital with a direct service link to a primary or secondary care facility; for example, an outpatient clinic or a regional general hospital. The point-to-point service arrangement is common, although it is not effective for creating a service network or community because of the increasing number of nodes needed to service a growing community. The existing programs focus primarily on the clinical aspects of e-medicine, although other services or activities are also supported.
EXHIBIT 8.1. MAJOR E-MEDICINE PROGRAMS IN TAIWAN
The National Health Insurance Scheme (NHIS) and the NII will both reimburse the cost of providing an e-medicine service. Specifically, the NHIS reimburses the services of on-site (local) attending care providers, while the NII partially reimburses services performed by the remote tertiary or teaching hospitals. Connection services are provided free of charge by the Bureau of Telecommunications, Taiwan's largest telecommunications service provider, which is primarily owned and controlled by the Ministry of Transportation. Depending on the requirements of the specific project, different connection services are available, including an integrated service digital network (ISDN) and a high-speed digital exchange network that supports frame relay and asynchronous transfer mode (ATM) transmissions.
Videoconferencing Project at National Taiwan University Hospital
Officially launched in 1995, this program connects the National Taiwan University Hospital (NTUH) and the Jin-Shan Medical Center, a primary care clinic located in rural Taipei County. Using a state-of-the-art videoconferencing system in conjunction with a medical imaging transmission and display system and a multimedia patient record retrieval system, NTUH provides both synchronous and asynchronous services to patients located in the connected medical center. The services in high demand include remote patient assessment, diagnosis, and diagnostic or therapeutic consultation across a wide array of specialty areas.
In 1997, NTUH expanded its e-medicine program by connecting directly with National Cheng-Kung University Hospital, the most important e-medicine center in southern Taiwan. The connection between two major centers supports peer-to-peer consultation, collaborative patient management, and clinical case discussions among physicians and specialists located at different tertiary hospitals. In addition, this link will be the backbone of the nationwide e-health service network envisioned by the DoH.
Around-the-Clock Consultation Project at Taipei Veterans' General Hospital
Taipei Veterans' General Hospital (TVGH) is a modern tertiary hospital that serves both the military community and the general public. TVGH joined the NII e-medicine scheme in 1995, operating a direct service link to Granite Hospital, the largest military hospital on Jin-Men Island. Using the same designated ATM-T1 line, TVGH also offers services to patients at Jin-Men Provincial General Hospital. The e-medicine suite is located in Granite Hospital, so patients from the provincial hospital have to travel there. By design, the program uses integrated information and medical imaging technologies, including a videoconference system, a medical image transmission and display system, and the existing patient information systems and image archive database systems housed at TVGH. TVGH offers around-the-clock e-diagnostic and therapeutic consultation services to patients located at both of the connected hospitals on Jin-Men Island, especially to those in need of immediate medical attention or emergency care. In 1997, TVGH launched a second service link, providing similar services to a public primary care clinic in Yi-Lan County in eastern Taiwan.
Emergency Support at National Cheng-Kung University Hospital
National Cheng-Kung University Hospital (NCKUH) is the only tertiary teaching hospital that joined the NII e-medicine scheme at its commencement. Operating a direct service link to Peng-Hu Provincial Hospital, a general hospital located on the island of Peng-Hu, NCKUH provides mainly remote consultation and diagnosis support for emergency care. This program's technological requirements include a high-resolution image transmission and display system and a videoconferencing system. In addition to its primary concentration on emergency medicine, the program provides scheduled virtual outpatient clinic sessions to patients not in need of urgent care, as well as clinical case discussions and continuing education programs for health care professionals. Judged by the service volume and the range of activity supported, this program is arguably the most active e-medicine program in Taiwan, offering about six hundred remote clinical sessions and delivering continuing education to over five hundred individuals in a typical year.
Military Acute Care at Taipei Military General Hospital
Taipei Military General Hospital (TMGH) provides acute tertiary care to the military community. TMGH joined the NII e-medicine scheme in 1997, operating a direct ISDN line that connects to Lien-Chiang County Hospital on Ma-Tsu Island. The program is supported by a mid-range videoconferencing system and a medical image transmission and display system. Use of this program, which is mostly restricted to urgent patient care, has been limited.
Program Evaluation and Management Issues
A survey of the major e-medicine programs in Taiwan suggested several key issues and observations concerning program evaluation and management. Overall program planning has mostly been centralized, with the DoH playing a critical role in program (need) assessment and coordination. Each program is highly autonomous with respect to particular services and medical specialty areas offered. At the same time, the programs share a fairly sophisticated technology base that integrates the relevant information, telecommunication, and medical imaging technologies to different degrees. Typically, while each program acquires technologies from external vendors, technology transfer, testing, evaluation, enhancement, and integration are mostly undertaken and managed by in-house IT staff, especially in the tertiary (teaching) hospitals.
Most, if not all, of the existing programs concentrate on serving patients in rural or offshore areas and focus primarily on vertical service integration by connecting care providers in primary, secondary, and tertiary care sectors. The target service recipients and service focus are largely consistent with those commonly found in U.S. programs but distinctly different from those of urban-based programs in Hong Kong as these programs are centrally controlled and administered through the Hong Kong Health Authority (Sheng and others, 1997, 1998). Program and service financing is mostly supported by the NHIS or the NII.
Several issues pertinent to program management deserve highlighting. First, the provision of routine technology-enabled e-medicine services may require considerable learning or training on the part of physicians and specialists. That is, user training is essential. Kleinke (2000) surmised that physician resistance is a significant bottleneck in the adoption and diffusion of technology innovations in health care. Training should not be confined to technology use and operations but, when and where appropriate, should include training in verbal communication skills and in detecting or using important nonverbal expressions or cues in a virtual setting.
Technology management represents another key challenge, commencing with technology acquisition. Both system integration and interoperability are relevant and need proper attention. Integration includes interfacing with existing (legacy) systems and with multiple sources of information or data. The importance of system interoperability significantly increases when scaling services from a point-to-point configuration to a networked setting in which participating organizations use heterogeneous technologies. For instance, a medical image system whose storage format follows a Digital Imaging and Communications in Medicine (DICOM) standard is desirable. Similarly, transmission of medical images between or among service participants can be greatly supported when all connecting organizations have implemented a picture archiving communications system (PACS). Cross-platform system interoperability is also required in order to preserve the confidentiality of patient information at both the algorithm level (for example, encryption software) and in a particular communication layer (for example, Secure Socket Layer).
Service configuration is also important. In a nutshell, e-medicine should generally be network-based because the value of an e-medicine service may be perceived to be higher when it includes more participants, patients, or care providers. In this light, expanding e-medicine services from a point-to-point configuration to a network-based service community is desirable, especially when connecting a network of service providers (for example, physicians and specialists) with a network of service consumers (the general public). An expanded service configuration is also economically appealing because of the resulting economy of scale and probable economy of scope.
Finally, service diversity is also critical to the success of an e-medicine program. An organization that chooses to concentrate on the clinical aspect of e-medicine services nonetheless should not exclude alternative or expanded service applications. Basic clinical training and continuing education are fundamental nonclinical activities that may be better supported and enhanced in an e-medicine setting. Diversity in medical specialty areas is a useful goal. In short, e-medicine services may differ considerably in their respective requirements, but including more services in an e-medicine program contributes to the program's overall value and its likelihood of success.
Conclusion
In this case study, we have surveyed the development of e-medicine in Taiwan and highlighted some major and representative programs. Several implications for program evaluation and management are identified and discussed. Overall, we suggest that not only should program champions work to convince physicians and specialists in general about the clinical value and technical feasibility of e-medicine programs, but they should also demonstrate the common benefits of e-medicine services and their implications for professional authority or autonomy, together with adequate strategies for protecting stakeholders. In addition, concerns about service delivery, physician-patient relationships, system integration and interoperability, legal liability, and payment for services must be addressed in order for e-medicine programs to continue and grow.
Case Questions
- Would you consider the dissemination of e-medicine in Taiwan similar to or different from that of other developed countries in Asia, Europe, or North America? Why or why not?
- Based on this case, identify and discuss common barriers to the diffusion of e-medicine services within a health care system.
- What are the core technologies that support e-medicine services in Taiwan?
- Compare and contrast the different e-medicine programs highlighted in this case. Does one program appear to be more effective and successful than others? If so, which one, and why?
- How are the surveyed e-medicine programs funded? What challenges do these programs face? What do you project for the future of these programs?
References
Kleinke, J. D. (2000, November–December). Vaporware.com: The failed promise of the health care Internet–Why the Internet will be the next thing not to fix the U.S. health care system. Health Affairs, Vol 19, Issue 3, 57-71.
Perednia, D. A., & Allen, A. (1995). E-medicine technology and clinical applications. Journal of the American Medical Association, 273(6), 483–488.
Sheng, O.R.L., Hu, P. J., Au, G., Higa, K., & Wei, C. (1997). Urban teleradiology in Hong Kong: Lessons learned and implications. Journal of E-Medicine and Telecare, 3(1), 81–86.
Sheng, O.R.L., Hu, P. J., Wei, C., Higa, K., & Au, G. (1998). Organizational adoption and diffusion of e-medicine technology: A comparative case study in Hong Kong. Journal of Organizational Computing and Electronic Commerce, 8(4), 247–275.
The authors would like to acknowledge the contributions of students, research assistants, and colleagues from their various universities, particularly graduate students at the University of British Columbia and Wayne State University, who have contributed to the literature searches and materials used in this chapter. Any omissions or errors remain the responsibility of the authors. This work was partially supported by grants provided to Joseph Tan by the Office of the President of Wayne State University.