Modeling Physical Activity Behavior Change
Edmund Seto1 and Ruzena Bajcsy2, 1School of Public Health, University of Washington, Seattle, Washington, USA, 2Electrical Engineering and Computer Science, University of California, Berkeley, California, USA
This chapter reviews the use of body sensors for physical activity behavior change modeling. It begins by presenting the need for individual-specific personalized strategies for motivating physical activity behavior change. Next, it discusses the current capabilities as well as challenges for body sensors to inform behavioral interventions, including presenting two existing models focused on understanding exercise performance. The chapter then discusses conceptual models for behavior change, focusing on the transtheoretical model of behavior change, health coaching, and motivational interviewing as examples. Current assessment approaches used to identify the stage in which a person belongs along the spectrum of adopting a behavior change are presented. Next, a study design and modeling framework are provided that utilize both questionnaire response and sensor data to estimate parameters associated with physical activity behavior change. The chapter finishes with a brief mention of remaining challenges in the field, including issues of usability and the risks associated with sensors and personal privacy.
Keywords
Body sensor network; behavior change; transtheoretical model; health coaching; personalized interventions
1 Introduction – Physical Activity Monitoring Capabilities
During the last twenty or so years, several groups, including ours, have used body sensors (a network of wireless accelerometers and other sensors that measure physiological parameters) on people during their physical activities, such as walking, falling, exercising, and the like. Most of these experiments were performed on small samples of the population, mostly on college students over relatively short time periods, and the scientific literature describing these studies is extremely scattered, distributed between engineering publications (IEEE Transactions on Biomedical Engineering, IEEE Transactions on Systems, Man, and Cybernetics, Journal of Biomechanics, etc.) and rehabilitation publications (Occupational Therapy, Sports Medicine, etc.). These small-scale studies of body sensors have rarely moved outside of the experimental laboratory to real-world practice.
Despite this, body sensors offer new possibilities to conduct increasingly detailed physical activity assessment. Beyond the simple waist-worn pedometer or accelerometer, using a variety of wearable sensors and different sensor modalities communicating with one another can provide a much richer perspective on a person’s physical activity (e.g., accelerometry at different body locations to assess posture and to recognize activity types; heart rate, respiration, and galvanic skin response sensors to assess fitness levels as exercise occurs; and GPS and other types of sensors to provide time-location measurements that offer contextual information for when and where exercise occurs).
Moreover, wireless technologies and integration of sensors with mobile phones are providing opportunities to communicate the results of these assessments in more creative, interactive, and meaningful ways so as to be more effective in motivating individuals to continue their progress toward adopting healthy levels of physical activity. There remain many challenges in integrating diverse sensor data, as well as challenges related to what to do with the information derived from these data. How should this information be fed back to the person, or communicated to a person’s social contacts (personal as well as health professional) so as to best help him continue exercising? Indeed, Clarke and Skiba [1] argue that there remains a “dearth of longitudinal studies to guide long-term training program designs.” This argument can be made for most of the current studies in observing human physical activities, and hence provide the proper guidance for intervention.
The challenge of how to provide information feedback is not simply a technology problem, but a human-centric technology problem. Technology is a way to collect data that ultimately needs to meaningfully inform a person’s ongoing process of adopting new behavior. Adopting new behavior is inherently a cognitive and psychological process that is more subjective and not as easily assessed as the more objectively measured changes in physical activity behavior. A number of theories have been proposed that govern how individuals adopt new behaviors. Indeed, these behavior-change theories – one in particular being the transtheoretical model [2] – have been applied to many health problems, including smoking cessation [3], problems with addiction [4], diet [5], and physical activity [6]. The challenge is how to integrate wireless body sensors with these theories.
The goal of this chapter is to examine these challenges. Specifically, we will consider:
• The need to utilize sensors to personalize behavior-change interventions to specific individuals
• The need to accurately quantify and model physical activities using body sensors in the context of interventions
• The transtheoretical model of behavior change and how it may be integrated with models of physical activity
1.1 Sensors can Inform Personalized Behavior-Change Interventions
In 2008, the U.S. Department of Health and Human Services issued its Physical Activity Guidelines for Americans report [7] that provides specific science-based guidelines for people of various ages to improve their health through physical activity. It recommends that children and adolescents obtain at least 60 minutes of physical activity per day, adults obtain at least 150 minutes of moderate or 75 minutes of vigorous intensity activity, and older adults try to obtain as much physical activity as younger adults. While these recommendations are based on scientific evidence of health benefits from population studies, on an individual level, a person may find such recommendations meaningless in terms of motivation to increase physical activity if he or she already meets the recommendation or feels that there is no hope of ever meeting the recommendation.
In some cases, such group standards can do more harm than good. Individuals who do not meet healthy guidelines may be ostracized by society [8], and this may lead to negative emotions or ambivalence toward healthy behavior. This suggests that while national population-based guidelines may serve as crude goals for individuals, much greater attention needs to be placed on “personalized” behavioral interventions. Within intervention programs, people need to be thought of as individuals. The ability for one person to be more physically active than another relates to many factors, including their personal motivation and barriers toward exercise. Thus, personalized intervention plans are more likely to be successful compared to intervention programs that are simply based on blindly encouraging people to take action [6]. Indeed, recent “calls to action” within the cardiovascular health community recognize the importance of behavior-change interventions, and specifically the need to combine individual-level with population-based health promotion strategies [9].
Related to the concept of personalized behavioral interventions are “adaptive” interventions. Collins et al. [10] provide a conceptual framework in which interventions are not “fixed” – every subject receiving the same format and dose of intervention – but instead, the characteristics of the intervention are tailored to individuals. Moreover, this allows interventions to change in time for a person based on their individual-level characteristics.
Body sensors can play an important role in collecting measures of physical activity to better tailor interventions to the individual. Specifically, using body sensors over time can help monitor levels of physical activity at baseline pre-intervention, changes in physical activity that occur during an intervention, and the degree to which individuals maintain improvements in physical activity post-intervention. These measures may be useful feedback to the individual, or the people working with the individual, to encourage them to change their behavior. The use of sensors is increasingly being recognized as an important departure from traditional behavioral assessments that are based on only a few, infrequent, unclear concepts – often questionnaires or qualitative interviews – rather than continuous clearly defined objective measures [11]. Indeed, sensors may play an important role in moving away from a one-size-fits-all approach to interventions to a more patient/subject-centric form of adaptive behavioral intervention.
2 Physical Activity Body Sensor Technology
Let us now consider the necessary sensor hardware and software components that enable body sensor networks for behavior-change interventions.
Firstly, there are many currently available wireless body sensors, such as those that measure physical/kinematic and dynamic activities: accelerometers, force and position sensors; and physiological measures, such as skin conductivity, perspiration, breathing intensity, EMG, EEG, heartbeat, blood pressure, etc. Furthermore, we can have environmental measures, such as cameras, audio, pollution sensors, GPS, ultrasound, and social interactions of people using phones or the Internet.
The second issue relates to how these sensors will be used on the body reliably, including both technical as well as usability considerations. Considerations include the number of sensors and their placement on the body. Because sensors on the body move during physical activities, one needs to compensate for this movement, and realize that the location of each sensor may not be reliably identified. For real-world practicality we need to know the minimum number of sensors necessary for reliable measurement of specific activities. Also, if one uses existing sensors, e.g., those on a cellphone that a person might normally carry, what is the guarantee that the user will keep the sensor on the body in the correct (assumed) orientation? Furthermore, with all populations, and the elderly specifically, there may be problems with remembering to recharge the batteries for sensors periodically. Hence, the signal may not be reliably delivered, and it is not always obvious how to detect the reasons for missing data.
Third, as described in the previous section, we would like personalized subject-specific data on activities, but personalization leads to technical challenges. We need to understand the limits of individual motion. Different people have varied kinematic and dynamic ranges of motions. This implies that we need to calibrate the reachable space for each individual. This potentially requires more accurate measurements that need to be performed in more controlled conditions. This is a practical challenge since not every subject can be forced to come into a laboratory or be bothered with occasional re-calibration procedures.
Fourth, there are costs to consider. To be practical, activity monitoring at home or in general outside of research/experimental settings demands inexpensive sensors equipped with easy-to-use interfaces. We have found that using readily available low-cost sensors like those in common mobile phones, or commercial camera sensors for the home like the Microsoft Kinect, can affect the quality of assessment. The price one pays is in coarse resolution and inaccurate data. Thus, there is a need to quantify error and to infer the correct parameters for the physical activity modeling to inform proper intervention. Moreover, general-purpose technologies like the aforementioned phone and Kinect technologies may not be appropriate or accessible to all individuals (e.g., the really young, elderly, disabled, or impoverished).
Fifth, data from body sensors needs to be processed to be intelligible. The first challenge in signal processing is in identifying and filtering out outliers. The second challenge is that data is a composition of unreliable devices (including the hardware and software) and the unpredictable behavior of the user (including non-wear, non-compliance with usage instructions, and purposeful misuse of the sensors). In order to deal with unreliable devices one needs multiple measurements of the same phenomenon in order to detect and understand the reasons for the unreliable behavior. For example, if one detects missing data from the cell phone, one can try and understand this in the context of detecting possibly the loss of battery power on the phone or the capacity of the internal memory card if data is being stored locally, or whether the phone was traveling to a remote area without cell tower coverage if the data is being stored remotely. In these cases, other internal sensors on the phone can be useful to detect whether the technical side of the body sensor network is at fault.
In contrast, the unpredictable behavior of users is a harder challenge to understand. In part it can be verified by asking the user questions, such as, Have you exercised today? and What times during the day did you exercise?, but these answers might contradict the data, causing additional challenges. It is known from psychology that people sometimes have varied perceptions of their achievements/activities. There may be real memory recall problems. There may also be shame and embarrassment related to the aforementioned ethical issues around physical activity that lead to purposeful misreporting or misuse of the devices. The body sensors may be perfectly accurate, but because they are annoyingly so, an embarrassed user may throw it in the garbage! Finally, for more socially connected body sensors, users may not want to transmit data about their activities because of lack of trust and/or privacy concerns. Moreover, issues of trust may vary depending on if the data is being sent to a healthcare professional, a family member, friends, or the public at large.
3 Modeling Physical Activity
If we are able to address the above challenges there remains the challenge of integrating the data through the use of conceptual and/or numerical models for the physical activity of interest. While review of all such models is beyond the scope of this chapter, we highlight two such models as examples. We note that in calibrating models to sensor data, the Holy Grail is to find the “right” parameters that fit the data the best and most generally for the given population, and if these can account for individual-level factors, all the better.
Consider the aforementioned work of Clarke and Skiba [1], which describes and critically evaluates two performance models: critical power (CP) and the banister impulse-response (IR) model. They justify the inclusion of these two models in the curricula of both applied exercise physiology professionals (e.g., clinical exercise physiologists, personal trainers, and coaches) and research-focused exercise physiologists. We believe these models are equally applicable to the design of exercise protocols for different personalized rehabilitation and physical exercise programs because they are based on performance models, which in turn allow for the appropriate feedback and interventions. In theory, having such models and subsequently protocols that can monitor and supervise the progress of exercise can help lead to changes in the behavior of subjects.
Modeling, of course, depends on understanding the process, selection of parameters, how to extract them from the measurements, parameter fitting and optimization and simulation and sensitivity analysis. Indeed, the performance modeling literature features each of these aspects (some cited in [12,13]).
3.1 Critical Power (CP) Model
The CP model describes the capacity of an individual to sustain particular work rates as a function of time (t). In this way, the model represents the relationship between exercise intensity and duration for an individual. The CP is defined as the power that can be sustained without fatigue for a long time. Then we can further define power P=work/time and finally ![]() as the finite amount of energy that is available for work above the critical power:
as the finite amount of energy that is available for work above the critical power:
(1)
Morton [14] presents four assumptions of the CP model:
• Power output is a function of two energy sources: aerobic and anaerobic.
• Aerobic energy is unlimited in capacity (one can exercise at the intensity or below of CP for infinite duration), but it is limited in the rate at which it can be converted into work.
• Anaerobic energy is unlimited in the rate of conversion (i.e., maximal power output or speed is infinite) but is limited in capacity.
This model is useful for describing power duration for maximal exercise lasting from 2 to 30 minutes. As such, the CP model serves as a useful tool for devising pacing and tactical strategies in relatively short athletic competitions. But it can also provide a basis for individualized workout intensities during training, exercise, and rehabilitation procedures. Furthermore, the model is amenable to body sensor measurements. For example, exercise above or below CP results in differences in maximal oxygen consumption.
There are limitations to the CP model, especially when we need to account for intermittent exercises and need to optimize interval workout prescription. Morton and Billat [15] extended the 2-parameter CP model as follows:
(2)
where t is the total endurance time, n is the number of intervals, tw and tr are the duration of the work and recovery phases in each interval, respectively, and Pw and Pr are power outputs during the work and rest phases, respectively.
3.2 Banister Impulse Response (IR) Model
In contrast to the use of CP for modeling individual exercise sessions or interval workouts, there is a need to model the effects of exercise over time, i.e., training. The IR model relates performance ability at a specific time to the cumulative effects of prior training loads. It describes the individual exercise dose-response relationship and handles the nonlinear time dependence and individuality in a single framework.
The model is basically a first-order differential equation describing a person’s change in performance as a function of time. The solution of performance p(t) is equal to the initial performance level p(0) plus positive training effect (PTE = “fitness”) minus the negative training effect (NTE = “fatigue”). Both PTE and NTE are expected solutions to first-order differential equation exponentials weighted with some coefficients that are specific to the activity task and the subject. The performance is a nonlinear function of training. Again, body sensors can play a useful role in monitoring changes in performance over time and successive training sessions to provide empirical data to fit such models.
In summary, both CP and IR models can be useful for guiding workout design and long-term planning, respectively. Performance models can serve as an avenue to guide professional reasoning and systematize the trial-and-error adjustments normally featured in exercise protocols. Moreover, these models also can help in identifying what feedback and intervention should be administered (e.g., Is the individual meeting the expectations of CP for a specific workout session? Is the individual training in a way that is most effective?).
Unfortunately, these models assume that individuals are motivated to optimize their exercises. For individuals just embarking on healthy lifestyle changes, or when a healthcare provider is prescribing behavioral intervention, such an assumption cannot be guaranteed. Hence, in the following, we discuss the issue of behavior-change modeling.
4 Behavior-Change Theories Relevant to Physical Activity Interventions
Although many theories exist for explaining the factors that influence individuals, and the cognitive and psychological changes that individuals go through as they adopt new behaviors, perhaps one of the more prevalent and integrative models is Prochaska’s transtheoretical model (TTM) [16]. The TTM is a conceptual (i.e., not inherently mathematical) model based on core constructs that describe the steps and ways that individuals adopt and maintain healthy behavior. The constructs describe how individuals move through six “stages” of change, and are influenced by ten “processes” of change [17], as well as some underlying assumptions about human behavior [18]. We define these briefly below.
The stages of change are ordered approximately in time. Individuals start at one of the stages, the earliest stage being “precontemplation,” and through intervention, progress to the last stage of “termination.”
1. Precontemplation: The individual is uninformed and not interested in the healthy behavior at all. He has no intention of adopting the healthy behavior at this time or in the near future.
2. Contemplation: The individual is aware of the problem, and has some intent to make a change in the near future (i.e., next 6 months). But perhaps at this stage the cons (e.g., too busy, too costly, not sure it will make a difference) outweigh the pros of adopting the healthy behavior.
3. Preparation: The individual is ready to make a change (i.e., in the next month). Perhaps they have created a plan, set goals, consulted with a trainer or have signed up for an intervention program. At this point, in his mind, the pros have outweighed the cons.
4. Action: This is when healthy behavior is observable. Changes in the person’s activities can be measured and quantified during this stage.
5. Maintenance: This is when an individual has transitioned from trying a healthy behavior, and doing it occasionally, to a state in which he does it routinely and naturally. During this stage, he may be tempted to “give up” and revert to their unhealthy behavior.
6. Termination: This is the last stage in the successful adoption of behavior change. The person is completely convinced that the behavior is healthy and good for him, and has no interest in reverting back to old unhealthy habits.
While the stages of change describe the temporal sequence of cognitive states that an individual goes through, there are a number of processes of change that individuals go through to govern the transitions between the stages of change. These “processes of change” are described as follows:
1. Consciousness raising: This relates to awareness of the problem and the potential for new behavior to address the problem.
2. Dramatic relief: This relates to the use of emotional experiences to convince a person to adopt a healthy lifestyle.
3. Self-reevaluation: This is relates to how an individual sees himself (self-image) with or without the unhealthy behavior.
4. Environmental reevaluation: This relates to how an individual sees himself affecting others around him because of his unhealthy behavior.
5. Self-liberation: This relates to how an individual believes he can change himself (will power).
6. Social liberation: This relates to the empowerment of disenfranchised populations who may benefit from advocacy, provision of services, and healthy alternatives and options.
7. Counterconditioning: This relates to coping or alternative behaviors to replace unhealthy behaviors.
8. Stimulus control: This relates to removing stimuli that prompt unhealthy behavior, replacing them with stimuli or reminders that promote healthy behavior.
9. Contingency management: This relates to the use of rewards and penalties for good and bad behaviors, respectively.
10. Helping relationships: This relates to having peer, family, or professional social support to encourage healthy change.
While the processes of change affect transitions between the stages of change, they are mediated by changes in cognitive and psychological variables. First of all, the processes affect how an individual weighs the “pros versus cons” of living a healthy lifestyle, i.e., decisional balance [19]. Also, the processes of change may alter a person’s “self-efficacy” – their confidence in making healthy behavior change [20]. Finally, the processes may affect one’s ability to cope with “temptation” to be unhealthy or resort to previous poor habits.
4.1 A Framework for Quantitative Modeling of Physical Activity Behavior-Change Interventions
Behavior change is inherently a difficult process due to the opposite of many of the aforementioned core constructs. Individuals may not progress linearly through the stages, but may move forward as well as backward through the stages as they change cognitively and physically. As previously mentioned, forward progression through the stages can be the result of a specific intervention program of some sort aimed at helping individuals change their behavior. In our research, we have been working with health coaches who help individuals change behavior through a process called “motivational interviewing,” which involves exploring a person’s readiness to change through communication and listen strategies, employing empathy, and collaborating to set goals for behavior change [21]. It is a method for achieving personalized adaptive behavioral interventions that we described at the outset of this chapter.
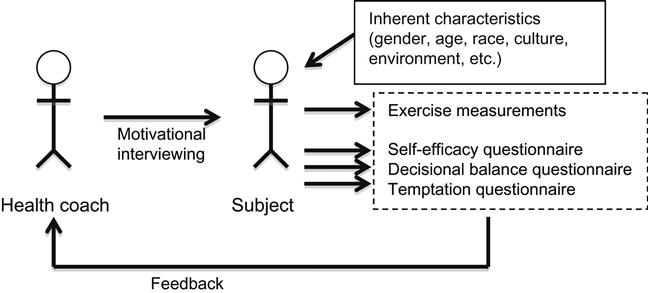
As an example, consider Figure 1, which illustrates a physical activity intervention program in which a health coach interacts with a subject using motivational interviewing techniques over some period of time (e.g., a 6-month period). During this period, there is a feedback cycle in which the health coach provides motivational interviewing to the subject who is conditioned by various inherent characteristics (e.g., gender, age, race, culture, environment, etc.), which in turn affects his exercise (measured by sensors) and cognition (self-efficacy, decisional-balance, and temptation measured by questionnaires). The results of changes in exercise and cognition affect the type of motivational interviewing that the coach performs with the subject. Hence, this sort of feedback enables the adaptive nature of this exercise intervention.
Also consider what data from this adaptive intervention may look like from a study design and a time series perspective (Figure 2). As the subject is recruited into the intervention study, they are given a baseline assessment before any intervention activities begin. The goal of the baseline assessment is to determine their cognitive state toward physical activity (i.e., to figure out where they are in the stages of change). Also, sensors may be worn during this baseline assessment period to determine the individual’s “normal” levels of physical activity and capabilities. It may take a few repeated measurements over a few weeks to obtain reliable baseline estimates. Let’s assume that the health coach finds that the individual has no interest in physical activity or in changing his levels of physical activity. The subject would be in the precontemplative stage. As the intervention begins, the health coach will start to provide feedback to the subject based on observations of body sensor data as well as the results of ongoing cognitive assessments using questionnaires. The use of body sensors to continually evaluate physical activity levels is novel and potentially more accurate compared to the bulk of prior transtheoretical model interventions that have only used self-reported exercise questionnaires (e.g., the 7-day Physical Activity Recall, PARQ) [6].
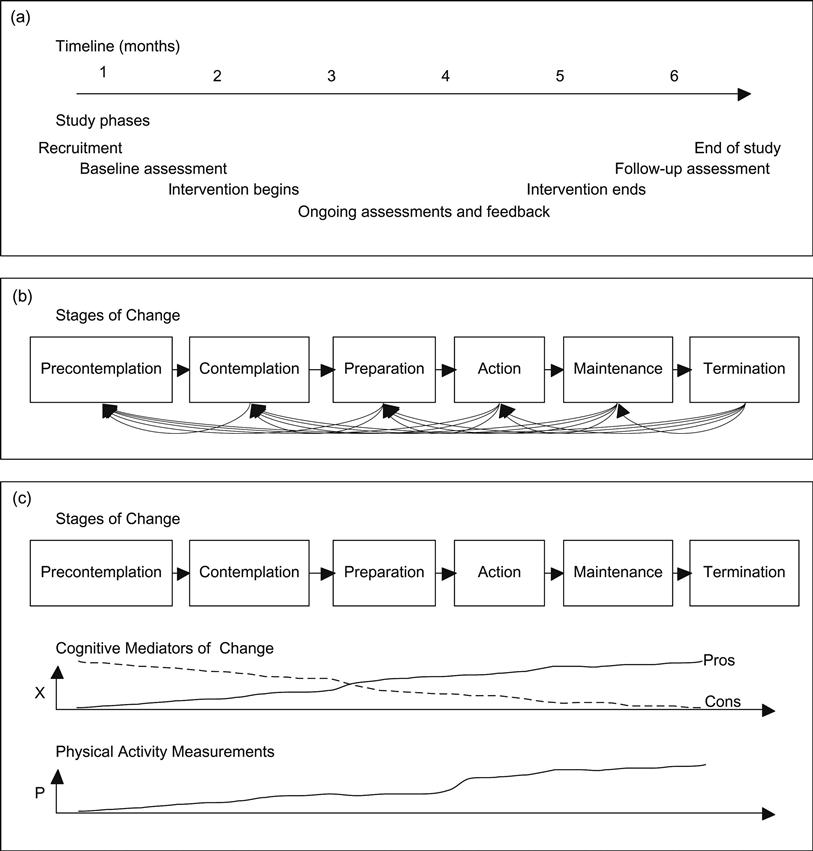
Based on the stage of change in which the person is at, a health coach may conduct motivational interviewing to help the person identify one or more processes of change that could be used to help the individual transition to the next stage of change. Questionnaires may be used to assess the stage of change to which the individual belongs. Additionally, cognitive assessments may be used to assess changes in the mediators (self-efficacy, pros versus cons, and temptations). Specific questionnaires and assessments are presented later. The interviewing provided by the coach could be tailored to the results of the assessments. Over time, through such personalized and stage-specific intervention, the coach may help the subject establish an exercise plan, which would place the subject in the preparation stage. And when the subject begins to exercise, the various improvements in physical activity would be measureable using the body sensors. Ultimately, the study would assess changes in physical activity during the intervention and at follow-up at the end of the intervention compared to the levels of physical activity at baseline.
4.2 Assessing Stages of Change
In order to monitor a person’s progression through the stages of change we need some way to assess his stage. Various algorithms have been developed for exercise-related stages of change, including Marcus and Simkin [22], who created the Stage of Exercise Behavior Change (SEBC) questionnaire to assign people into stages. A related approach called the Stage of Exercise Scale (SOES) developed by Cardinal et al. [23–25] asks individuals to place themselves on a 5-rung ladder, which determines their stage. The validity of these questionnaires has typically been evaluated if exercise increases as individuals progress through their assigned stages. This correlation between physical activity and stage change over time is consistent with the framework we have described in Figure 2.
Aside from assessment of stage of change, other questionnaire-based assessments of mediating factors have been developed. For instance, assessments have been developed for decisional balance [17], self-efficacy [26], and temptations [27]. These questionnaires may be used to estimate the probability of transitioning between stages based on each of these factors, respectively.
In all cases, results of such questionnaires, as is common in psychological studies, are variables that are either binary or ordinal ratings. Moreover, despite having undergone various validation studies, when applied at the individual person level, they should be viewed as only indicators, subject to error, rather than absolute assessments [28].
As a concrete example, consider the following questionnaire adapted from Marcus, Rossi et al. [17] aimed at assessing stages of change:
Please respond with how much you agree with the following statements:
I am currently physically active.
0=Strongly Disagree, 1=Disagree, 2=Neither Disagree or Agree, 3=Agree, 4=Strongly Agree
I intend to become more physically active in the next 6 months.
0=Strongly Disagree, 1=Disagree, 2=Neither Disagree or Agree, 3=Agree, 4=Strongly Agree
I currently engage in regular physical activity.
0=Strongly Disagree, 1=Disagree, 2=Neither Disagree or Agree, 3=Agree, 4=Strongly Agree
I have been regularly physically active for the past 6 months.
0=Strongly Disagree, 1=Disagree, 2=Neither Disagree or Agree, 3=Agree, 4=Strongly Agree
Note that the questions lead to ordinal, scored responses. Asked over large numbers of people, we would generally find the scored responses to each question fit normal distributions. Thresholds may be specified such that those scoring low in questions 1 and 2 would indicate subjects in the precontemplation stage. Those scoring low in question 1 and high in question 2 would indicate subjects in contemplation. Those scoring high in question 1 and low in question 3 would indicate subjects in preparation. Those scoring high in questions 1 and 3, but low in question 4 would indicate subjects in the action stage. And those scoring high in question 4 would indicate those in maintenance.
Although these assessments have traditionally been conducted fairly infrequently over the course of an intervention, new technologies may play an emerging role in more frequent (e.g., daily) assessments. Approaches like Ecological Momentary Assessment [29], in which subjects are asked in-the-moment during random or fixed-interval times about their feelings and attitudes, can be conducted on more pervasive technologies, such as personal computers, phones, and tablets.
4.3 Opportunities to Use Behavior-Change Models to Guide Intervention Programs
Over the last several years, progress has been made toward applying engineering control theory approaches to the challenges of understanding behavior-change interventions. As we have alluded to in Figure 2, data from behavioral interventions can be viewed as time series. Moreover, particularly for adaptive interventions, in which intervention characteristics change over time, more formal modeling of the feedback process (Figure 1) can benefit from more generic studies of feedback for control systems. Notable literature includes the work of Rivera et al. [30], who applied ordinary differential equations to an adaptive behavioral intervention, and Böckenholt [28], who examined the use of a Markov model in cases where there are stages (i.e., states) associated with the behavior-change process.
Because the stages of change are essentially states, they are amenable to implementation via a Markov model, whereby a person belongs to a given state at any given point in time, transitions between states are governed by probabilistic processes, and future state depends only on current state. Böckenholt [28] combines two main components to end up with a continuous-time latent Markov (CT-LM) model for behavior change. The first component considers that binary or ordinal responses to typical behavioral surveys depend upon a latent (not directly observable) state to which a person belongs. Second, changes in responses over time are modeled by a stochastic process that governs transitions between states. Detailed derivations of the model are presented in Böckenholt [28], which are discussed briefly below.
Based on prior work by Samejima [31,32], Böckenholt describes the probabilistic nature of binary or ordinal responses to questionnaires as being a function of the latent state in which a person resides:
(3)
where the probability that a variable ![]() (i.e., a question in a questionnaire) takes on a response
(i.e., a question in a questionnaire) takes on a response ![]() is conditional on the characteristics of the latent state
is conditional on the characteristics of the latent state ![]() , and is related to the difference of two normal cumulative distribution functions
, and is related to the difference of two normal cumulative distribution functions ![]() defined by the mean
defined by the mean ![]() and standard deviation
and standard deviation ![]() , for a set of lower and upper thresholds
, for a set of lower and upper thresholds ![]() and
and ![]() , respectively.
, respectively.
Due to the challenges of collecting and processing body sensor data that we described earlier, physical activity data are also subject to error. Thus, they may also be amenable to such a probabilistic treatment as questionnaire response data, in which physical activity levels determined from sensor measurements are ranked into ordinal levels.
Next, because the responses are dependent upon the state ![]() to which an individual belongs, we need to define switching probabilities between states. A person can belong to only one state at any time. In the CT-LM model, states are discrete, defined by the above parameters
to which an individual belongs, we need to define switching probabilities between states. A person can belong to only one state at any time. In the CT-LM model, states are discrete, defined by the above parameters ![]() and
and ![]() . Switching between states follows a Markov process and depends upon time within a given state:
. Switching between states follows a Markov process and depends upon time within a given state:
(4)
where (0<![]() <1) and (
<1) and (![]() >0), such that the probability of switching
>0), such that the probability of switching ![]() is small if the duration
is small if the duration ![]() of the time interval spent in a state has been short. These are called transition probabilities.
of the time interval spent in a state has been short. These are called transition probabilities.
If the average time that a person spends in a state ![]() is
is ![]() , then
, then ![]() is the termination rate of the state per unit of time, with transition rates between specific states
is the termination rate of the state per unit of time, with transition rates between specific states ![]() and
and ![]() denoted as
denoted as ![]()
(5)
And state-switching generally following these probabilities:
(6)
Assuming that responses and physical activity are tracked over time longitudinally for a number of subjects, data are available to parameterize the CT-LM model. Böckenholt combines the above relationships into the CT-LM model of the probability of observing a particular response pattern over time from the ![]() -th subject at times
-th subject at times ![]()
(7)
where ![]() is the probability of switching from state
is the probability of switching from state ![]() to
to ![]() between times
between times ![]() and
and ![]() ,
, ![]() is the probability of being in state
is the probability of being in state ![]() at time
at time ![]() , and
, and ![]() is the probability of observing the response at time
is the probability of observing the response at time ![]() given that the
given that the ![]() -th person is in state
-th person is in state ![]() .
.
This leads to a log-likelihood formulation from which parameters of interest (![]() ) may be estimated using maximum likelihood estimation techniques given sufficient data observations from subjects’ responses tracked over time as they transition between states.
) may be estimated using maximum likelihood estimation techniques given sufficient data observations from subjects’ responses tracked over time as they transition between states.
Within this framework, there are two remaining challenges. The first is how individual-level factors are considered. In the absence of individual-level covariates in the maximum likelihood estimation, population average parameters based on the provided data will be estimated. These can be useful if the data provided are already for a specific population group. However, for larger and more general population data, if individual-level covariates are provided, e.g., related to the transition probabilities or duration of time within a state, parameters related to these individual-level covariates may also be estimated.
The second question is how feedback with the health coach is implemented. We may assume that the health coach has no state. Consistent with the concept of motivational interviewing, the coach responds simply to the state of the subject. Hence, the motivational feedback ![]() that a health coach provides to their subject – the processes of change that they prescribe to the subject – is modeled as a function
that a health coach provides to their subject – the processes of change that they prescribe to the subject – is modeled as a function ![]() :
:
(8)
where ![]() depends upon the expectation of the subject’s state
depends upon the expectation of the subject’s state ![]() , and results in a vector of binary (yes/no) outcomes as to whether the subject should or should not work on each of the 10 processes of change as a specific intervention strategy to encourage movement to subsequent stages of change. Evidence from the successes of stage-matched intervention studies in which individuals are matched to specific processes of change based on the stage they belong to may help define function
, and results in a vector of binary (yes/no) outcomes as to whether the subject should or should not work on each of the 10 processes of change as a specific intervention strategy to encourage movement to subsequent stages of change. Evidence from the successes of stage-matched intervention studies in which individuals are matched to specific processes of change based on the stage they belong to may help define function ![]() . Moreover, if this function is parameterized, it may be included into the transition probabilities above and subject to maximum likelihood estimation.
. Moreover, if this function is parameterized, it may be included into the transition probabilities above and subject to maximum likelihood estimation.
While the calibration of such models to real-world body sensor data has not been fully realized, the conceptual and methodological underpinnings as described by these studies will soon allow for more widespread application of numerical modeling to sensor-enabled behavioral intervention studies. For instance, assuming behavioral intervention studies lead to data from which parameters of such models can be estimated, it would be possible to estimate the expected state to which an individual belongs with greater certainty, thereby informing greater personalization of health coaching.
5 Conclusion
In this chapter we have explored the motivation for personalizing behavior-change interventions using body sensors. We have discussed the opportunities and challenges of using body sensors to inform exercise models. We have also presented the need to think beyond performance-oriented exercise models to those based on psychological and cognitive aspects of behavior change.
Still there remain numerous issues to be explored that are both practical and ethical in nature. For one, we have only explored a limited set of feedback options. One may be feedback just to the subject himself. Another type is feedback between a subject and a health coach. There are many other scenarios including feedback between peers undergoing interventions as well as feedback to family and friends who may provide social support. As we mentioned in the introduction of this chapter, new wireless communication capabilities have enabled all these forms of feedback. However, we have not addressed the issues of the format for such feedback (temporal frequency, symbolic/textual/verbal, computer-automated, or humanistic). With all of these forms of feedback, accurate and timely data from body sensors will play an important role in tailoring the messages to encourage behavior change. However, there are trade-offs between the breadth and depth of sensing needed to improve behavior-change programs and what can be tolerated in terms of risk to personal privacy and usability. As body sensor systems are increasingly moved from the research world into the practical world, we will need to continue to explore such practical and ethical issues.