6
Use of Machine Learning and Deep Learning in Healthcare—A Review on Disease Prediction System
Radha R.1* and Gopalakrishnan R.2
1Anna University, Chennai, Tamil Nadu, India
2K. S. Rangasamy College of Technology, Tiruchengode, Tamil Nadu, India
Abstract
The practice of adapting Machine Learning (ML) and Deep Learning (DL) methodologies for the exploration and identification of biomedical and health related issues has established unmatched response in the last few decades. A number of unearthing features that are meaningful are being recorded using these branches of Artificial Intelligence (AI) to achieve the difficult tasks that stood as challenge to human experts. The treatment processes, the devices used in treating patients, and the applications used are all capable in generating alarming amount of information. These information are technical data in the form of images, graph, test, and audio files; processing and getting the valuable insights from these data is a tedious task. The invention of ML and, lately, DL have paved way to access and analyze these data from the big data era in a smooth manner to predict, diagnose, and treat diseases effectively to save valuable lives of millions. DL, which has deeper (or more) hidden layers cascaded functions of similar quality, forms a network that is capable enough to dissect any magnetic resonance image in faster and accurate manner. The chapter discusses the basics related to DL and Ml methodologies and the related works where the impact of the same are high solicited. The implementation highlights of ML and DL are also presented with respect to pre-and post-treatment through healthcare systems. DL and ML find its application in every aspect of biological system, electronic health records related to patients, and image modalities as well. In addition to the above-mentioned, the chapter presents the inherent challenges of ML and DL affecting the medical domain as well the research scope on improving healthcare systems with focus to promote and improve health management system.
Keywords: Machine learning, deep learning, artificial intelligence, public health monitoring and reporting, storing, retrieval
6.1 Introduction to Healthcare System
The healthcare system is an essential component in the life of every citizen in every country. The healthcare policies in different countries have different rules and regulations incarnated into it. The needs of people in rural and urban areas differ and their by the policies related to healthcare system differs. A healthcare system that is universal faces many discrepancies in terms of quality treatment and medical coverage of a patient or the likely disease. The difference between urban and rural background paves way for many dissimilarities in handling and treating a patient. The natives of rural areas suffer a lot due to lack of physicians in required numbers for proper and timely treatment; they are the ones who access the healthcare system infrequently. Although the public healthcare system is prevailing the expanse of these fail to compete with the private healthcare providers. The cost and time taken to diagnosis a disease and treat the same differs from one provider to another. The advancement in technology is combined to provide a better treatment for anyone irrespective of the service providers.
Growing need and increasing challenges faced by the enormous population on mother earth presents the need for more healthcare professionals. Apart from this, the low insurance dispersion, insufficient access, and increasing deadly disease threats also add up to the need for a better healthcare system. Traditional healthcare systems or providers failed to provide the required necessities to general public in large scale. Technological advancement leads to expansion of infrastructure, process improvements, accessibility, storage, and retrieval process and also to provide timely decision. The need to access and store digital data related to a treatment or invention provided the opportunity to join hands with Artificial Intelligence (AI). With AI, the information related to a patient is extracted to the core which aids in better understanding and thus leads to a better treatment plan. A better healthcare system makes medical services understandable, cost effective, and accessible. The usefulness of a health-care system is undermined, and there are various reasons behind the failure of this life saving mechanism.
6.2 Causes for the Failure of the Healthcare System
One among the major reasons for failure in healthcare system usage in decision-making is characterized by mistrust, antagonism, and mostly skewed motivations. The consumers of the healthcare diagnostic system show an exemplified need for more facilities or features with less expenditure [1–3]. The concept behind using a system that could effectively treat a disease is diluted by the vicious notion of consumers to pay less and get more concepts. The concept of better tomorrow could be made possible only if the basic alterations are made in the healthcare culture. One other cause for failure is imparting the required knowledge among healthcare professionals as well. The motivation behind the usage of healthcare system should be care for patients rather than care for business.
The quality of such healthcare system has to be improved which was tempered by the overuse and misuse of such system by limiting the integration of structural design of such systems. One other cause of failure of any healthcare system is due to the inability in handling voluminous data generated in the form of digital facts and figures. With the ever increasing speed of data generation in the digital era, the need for a more accurate and fast diagnostic system is of high demand.
Limitation in data access and inadequate adoption to data in the form of electronic records and a proper data format to store them are also causes for the failure in healthcare system. The complex nature of healthcare system triggered another process, namely, evidence generation which become an acute task. The critical activities in healthcare units needed a wide range help from data analytics, engineers through the support from engineering principles. The point of focus here is right amount of knowledge at the correct time delivered to the right human to proceed further in assisting the right person with health related issues. All healthcare units either public or private need a sophisticated system that can provide the accurate and timely handover of potential knowledge about patient across healthcare units.
The most important factor that is a major reason behind the failure of healthcare predictive system is communication [4, 5]. The interpretation of patients’ opinion about the health concern or experience is intervened by the opinion of doctors which greatly influence the result or outcome of healthcare systems. Failure occurs in every step in providing treatment to a patient but the primary concern is with the fault in interpretation, interaction/communication between primary, as well as secondary healthcare units and with the specialists. The lack of information flow from primary to secondary health unit is also a cause of concern. The inadequacy in knowledge sharing about the diagnosis, treatment, and post-monitoring plans between hospitals is also a cause for failure of healthcare predictive systems. Elderly patients are the most who suffer from these inadequate communications between primary and secondary healthcare units and their lack of language compatibility [6].
The major criticism thrown on most of the primary healthcare unit and their supporting system is insufficient details available with respect to disease their causes, impediments their diagnosis and treatment when an alternate is required. These inefficiency leads to refusal of patient needs which makes them move from public service to private service. While with secondary healthcare units, their services are blamed because of inaccurate prognosis which focuses on acquiring an efficient healthcare support system. Because of their lack of accurate diagnostic report, they suffer from insufficiency in terms of information to be supplied to specialists.
The overall problem or failure in healthcare system which is used for identifying or predicting a disease is lack of proper communication between patient and the specialist/doctor [7–9]. The doctors, though try, may not be able to identify or gather the details with respect to the symptoms, its severity level, disorientation in sleep pattern identification, drug usage level monitoring, life style quality, and the lack of ability to overlook the patients’ incorrect way of projecting the cause, diagnosis, and post- and pre-treatment.
The health services like critical surgery with respect to life threatening diseases which happens at the disbursement of communication and followed through by clinical assistance post-surgery suffer a lot due to mis-communication. The routine questionnaires do identify the quality of the disease will also provide assistance in treating a patient again this causes issue if there is a language barrier [10]. The knowledge provided to patient with respect to the side effects of medication or surgery or treatment serves as a major cause of failure in healthcare service sector.
6.3 Artificial Intelligence and Healthcare System for Predicting Diseases
AI is a concept that made it possible to simulate the capabilities and behaviors of human in a machine. The voluminous data generated in this technological era made it difficult for humans to analyze these enormous data to provide insight about them. In a field where data are generated in exabytes, it needs a constant monitoring which is highly becoming an impossible activity for any human and the errors in prediction is also a major concern. The areas of critical activity like medicine, nuclear power plant activities, and forecast of disasters require accurate prediction. The advances in AI and its subsets made life more flexible and faster than ever; Siri in Apple, Cortana, and Alexa are smart enough to predict and provide the user with their needs in an interactive manner. These advances are utilized in the life saving industry to ease the diagnosis and treatment phase in terms of computational cost and time.
With advances in AI, the machines were able to handle things effectively like human beings but the concept of learning or gaining knowledge from data gathered was achieved only through Machine Learning (ML). AI is a field which works to make a system smart and intelligent and covers wide range of scope. ML is a subset of the above-mentioned term AI, which focuses on enabling a system to forecast and make decision for a specific domain based on the knowledge gained through past data. ML focuses on learning and self-correction, while AI focuses on the above along with reasoning.
To outdo human understanding in terms of interpreting, analyzing, and comprehending complex medical prognosis and medical data, AI-based algorithms are most pursued. AI is also pursued to eliminate the costly backend process related to management tasks and is used to cease the inefficiencies as well. It is used to drastically eliminate the 51% load of the medical staff who assist the physicians and remove nearly 16% load off physician activities. AI-based healthcare systems are widely appreciated and mostly look up for stream lining administrative activities as well as clinical care system.
While ML is a subcategory of AI, Deep Learning (DL) is a subsection of ML. DL mimics human brain by implementing the complicated nervous system of human being in assisting the decision-making or predictive system. DL procedures has a motivation on analyzing and identifying patterns with respect to information ingrained in the data collected with respect to medical images. These procedures recognise the patterns in the similar ways as how human brains processes the information provided based on already acquired knowledge. The moment from ML to DL helps process the enormous data generated on daily basis and also to prepare themselves on self-learning objective as well. Figure 6.1 provides the relationship between AI, ML, and DL.
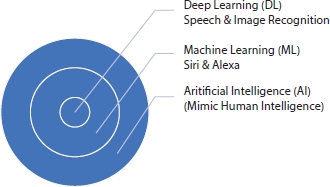
Figure 6.1 Relationship between AI, ML, and DL.
6.3.1 Monitoring and Collection of Data
The regular activity of collecting data on appropriate modules of health and the elements responsible for it is Public Health Monitoring and Reporting (PHMR). These activities are considered essential in a wide population or in a sample space, which are considered important to address the major health issues with respect to pattern, trends, topological cover, and number of occurrence in the geographical location along with its impact. The relationship between the elements responsible for outbreak of a pandemic and its health issues helps us in considering the contrivances of health and disease.
Without a proper health report, these public health monitoring activities are useless. Primary aim of public health recording is to support and to communicate the state of health of general public. These are also used to prepare the evaluation modules of policy making of healthcare plans. Data collection is an ongoing process of systematic collection, scrutinizing, and elucidation of innumerable types of information from countless sources. The accuracy of information is considered as a powerful tool not only to improve commerce but rather it is used to highly influence the decisions made. Most prevention strategies depend on these powerful tools [11–13].
Data pursuing and scrutiny are considered to change the universe for better in the healthcare industry. Reduction of workload, profit increase of medical agency and efficiency in the process of predicting epidemic outbreak, as well as providing the proper treatment plan for existing diseases are the merits of data collection. With AI in picture, a better view of affected persons’ interpretation of symptoms is achieved. Personalized treatments, advanced treatments, and improved communications between healthcare providers and disease affected persons and enhanced healthcare results are the boon of data collection.
Technological advances have enabled various modes of information collection from affected persons through wearable gadgets in collaboration with sensor devices. The information is processed by AI-based systems and ML algorithm to gain access to correlation between various data and is used to provide support to decision-making activity of physicians. In certain cases, these information services are based on predicting presence and absence of critical illnesses, and in some other cases, it predicts the possibility of occurrence of a disease or side effect of a treatment or relapse of an existing illness.
Chat bot therapy is used to collect the data of mentally instable person and their behavior; it is also used in the care taking process of elderly person by monitoring and understanding their daily routine. Use of AI in healthcare industry is the need of the hour but to make it possible enormous amount of information has to be gathered. The data collection comes with its own price in the form of privacy violation of a patient and is yet to find publicity in the society. The process of restructuring and implementing AI-based healthcare systems faces lots of hurdles due to lack of real-time data, since patients are not open minded in sharing their personal details related to treatment or causes or diagnosis.
6.3.2 Storing, Retrieval, and Processing of Data
In today’s world, the management of storage of medical record and the management of data stored in those records are the tedious activities. The healthcare sector is flooded with enormous volumes of data. The inter-net data center reveals that, in 2014, the amount of healthcare data generated was in terms of 153 exabytes, and now, in 2020, this has escalated to 2,314 exabytes. These data that are collected are in the form of structured, unstructured, and semi-structured data.
The data collected from various sources are put together in a single space and they need to be formatted in such a way that, when accessed from anywhere, they should provide the required information. In addition, 80% of these data are in unstructured format and considered a pressing issue in larger healthcare units where petabytes of such information are stored, processed, and maintained. Now, with advances in technology, these varied data can be stored in various locations using the organization strategies like Flash and Block chain even though cloud is considered the most widely used choice. The security and secrecy of the information stored in these locations are the major concern, which, in some cases, many healthcare units bend to comply with the legal mandatories of every country. Apart from storage of electronic health records (EHR), x-rays, and other imaging modalities, the process of retrieval of these data from storage unit also plays an important role in accurate and quick prediction of disease pattern [14, 15].
The storage location from fire proof, secure, and easy access and proper backup facilities in case of natural disaster must also be concerned. The medical care unit has a constant need of updating in terms of securing this information with minimal cost. The concern with space, cost, etc., can be overcome by usage of cloud services. Now, cloud is being replaced slowly by Flash storage technology which is viable alternative. These offers low delay in retrieval of information, and it provides instant access as well. Uptime with respect to these is also highly recommendable upto 100% and loss of data access is also negligible. Another technology is block chain, which address the interoperability and data exchange which are the two prominent challenges of healthcare industries.
Pre-processing of data is again a challenging activity since these data are in different format; the need to define a unique format is a need. The data are to the structured in a way which makes it feasible to be accessed across hospitals or any medical unit. AI-based system will be able to gain proper information through these data more easily when it is structured. Most of the medical data are in the form of images, the quality of the images depends or highly influenced by the environment in which they are obtained or acquired. The quality of the image has to be improved so as to find the defect or hidden information from these images.
The resolution, color contrast, and noise removal are some of the pre-processing activities related to the image medical data. In case of data stored in the form of text and numerical format, redundancy and incomplete data are of great concern. The text data are processed using NLP (Natural Language Processing) technique which is one of the extensions of AI. This helps in translating the regional language information related to patients and diseases in to another language so as to assist the physician in identifying the cause, symptom, and treatments provided to a patient. Language barrier is broken using these AI and ML advancement. Further, it aids in communication between patient and physician even without worrying about language barrier. The chat bots are trained in such a way that it identifies the language of the patient and raises question in their native language to assist the patient upon analyzing their previous medical records.
6.4 Facts Responsible for Delay in Predicting the Defects
The facts responsible for delay in prediction systems are used earlier are non-AI based, which purely rely on the observations of the radiologists. The true state of the distribution of radiologist per 1,000 patient ratio is not convincing, thus resulting in delay in predicting the disease or the spread of an existing ailment. The delay in the prediction is deadly in critical diseases; in rural areas, the places where the medical facilities or staffing are insufficient and these delay are always blamed for high death rate in these regions. With the use of AI- and ML-based prediction system, the possibility with increase in speed of detecting the disease is high.
Communication is also a barrier which is yet another root cause for the failure of these systems. The lack of information related to a particular disease, its origin, symptoms, severity, and speed of spread are also missing in most cases which makes it difficult in designing and training an AI-based healthcare system. The AI system depends on the past history and ML learns from these previous data to train itself to handle the new incoming data, so the data shortage is also a major drawback.
Connectivity is also to be considered; the internet access in rural area is also a bottleneck in delay in predicting the disease or pattern. The images taken from patients in rural areas could be compared with existing images to find a match in them to identify the disease when a proper network supply is available within seconds. In most of developing countries where the population in rural areas suffer mostly with lack of facilities for testing and knowledge sharing among medical practitioners is limited could also be taken into consideration for delay in diagnosis of diseases.
6.5 Pre-Treatment Analysis and Monitoring
AI-induced predictive systems provide more information to clinicians with an abundance of insight about patient and the root cause of the disorders experienced by the patients. The AI-based systems help immensely to assist physicians in making accurate decisions in terms of diagnosis and also in planning the treatment. There are many systems effectively designed for treatment assistance for patients of need used in many healthcare units, but the most sought among them is the system for cancer detection. ML approaches are used in application including analysis of various image modalities for effective identification of presence of cancer cells, type of cancer, area of spread, and, in some cases, the remaining life of an organ [16, 17].
The pre-treatment process involves analyzing the image which involves pre-processing like enhancing the image quality and segment the image, finding the region of interest, and identifying the presence of cancer cell and cancer type by training the system. The pre-treatment process reduces the false positive or false negative issues faced during manual evaluation and could also be used in reducing the (invasive) testing done on patients. There are many advancements and systems designed for the purpose of assisting the physicians like VIZ which recognizes difference in the image modalities related to brain. The brain health is evaluated based on AI- and ML-enabled system neural analytics (robotics). The diseases like cardiovascular diseases, lung disorders to eye disorders are identified through Voxel cloud, a computer aided detection system. Many such startup systems showing interest in AI enabled development in these areas like Nines, Botkin.AI, Prognica and Jiva.ai are to name few.
For example in pre-treatment phase of brain tumor, the detection process that uses ML- and DL-based computer-aided diagnostic (CAD) system plays a vital role in identifying the tumor region successfully than the radiologist with minimal time duration. Here, the image of the patient is fed to the system which pre-processes the image to enhance its contrast to define the boundaries of the components of the brain cavity. Upon enhancement, the image is fed to segmentation approach that sections various regions of the brain cavity based on the intensity of pixel value. Figure 6.2 shows the flow of the segmentation process flow of the computer-aided system using DL and ML [18–20]. The segmented image is then further processed to identify the features that are vital to indicate the incidence or non-appearance of tumor using various classification algorithms [21].
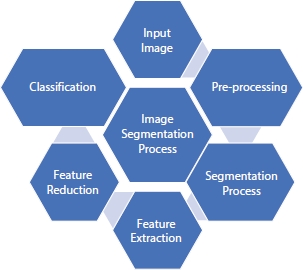
Figure 6.2 Image segmentation process flow.
6.6 Post-Treatment Analysis and Monitoring
DL approaches benefit most of the post-treatment analysis process of patients and helps reduce the time spent on patient analysis almost upto 15% from the physician end. The cut down of man power invested by physician on understanding and analyzing the background of their patient history and getting knowledge from the current image modalities of the patients help radiologist to a great extent. The images are analyzed by the DL-enhanced system and these procedures gets an insight about the image and assists the clinicians in determining the amount of radiation to be provided or the extend of exposure or the area to be re-operated in case of relapse in cancer patients. DL and ML being subsets of AI help in developing expert systems that questions patients and able to remotely access any patient’s data similar to it, thus making the required suggestions to doctors in attending to the patient. The insight about the previous treatment provided for a similar kind of disease may help to treat the patient more accurately and quickly thus time and cost are optimized to a maximum.
Expert systems designed based on AI or computer-aided healthcare systems based on DL or ML are designed in such a way that they acquire the knowledge from the clinicians and train themselves based on those stored data. During treatment of critical illnesses, the dosage of medicine recommended for any patient is monitored and along with other vital information or fed to these systems which monitors to find the possibilities of occurrence of any other ailment during the post-treatment phase. These above activities require constant man power monitoring and increasing the expense on medicines as well, thus contributing to increase in the cost of treatment. The design of effective post-treatment procedures based on AI, ML, or DL could be employed to bring down the cost considerably. Thus, an effective healthcare system in rural areas of developing countries around the world is provided.
6.7 Application of ML and DL
6.7.1 ML and DL for Active Aid
Elderly people mostly rely on the support of others to meet their daily activities; AI provides an answer to overcome this dependency in the form of AI-based Active Aid. This is powered by the concepts and technologies like robotics and NLP. AI-based applications to help support these elderly people through home smart automation software, which uses the data generated by sensors along with wireless sensor network and some of the data mining tools is presented in [25] recently. Moreover, a part of AI, which is Neural Networks, is trained with specific input image modalities to identify the expressions displayed by humans in various scenarios and the modulations in their voices. These NNs are capable to interact with the humans and help them with their needs specifically for specially abled persons and persons affected by paralysis. These neural networks further assists people using wheelchair to monitor and control its moments without any gadgets mounted on them [26].
The AI-based RUDO helps blind people to have a comfortable work life along with others even in the field of electronics as well as informatics [27]. The system based on AI to detect fall and categorize them to identify the complication level in elderly people helps immensely in treatment plan. The activities of elderly people who are on their own in any environment can be monitored and the details are recorded, these records serve to identify a possible disorder that may cause an alarming situation [28]. The above-mentioned devices, tools, and software based on ML and DL help in improving the life style of differently abled person to a great extent. Many researches have collected enormous amount of information from the environment as well as from the users to device expert system that interacts with the radiologist or with the physicians to assist them in planning the treatment (post or pre), the systems are trained in such a way that they monitor the side effects of the medication based on the pathology report of any patient as well [29].
ML and DL cover wide range of applications in the medical domain. Processing of signals from various sensors and the image produced by various imaging techniques used to project the anatomy of human being for diagnosis or prediction of diseases uses these technologies that bubbled out from AI. They are widely used because of their capability to identify interlink between the factors and the diseases caused by these factors [30]. The issues related with enormous data that are generated on daily basis suffer with quality issues, inconsistency, as well as incompleteness along with ethical issues. Accessing these data from various domain and coming out with a meaningful insight is a complex task by itself. These technologies address all the disease related issues but still they majorly focus on data from three important domains: cancer [31], neurology [32], and cardiology [33]. Figure 6.3 shows the flow of data generation from clinical observations to NLP data and its enhancement which boost the analytics process done using ML and DL approaches.
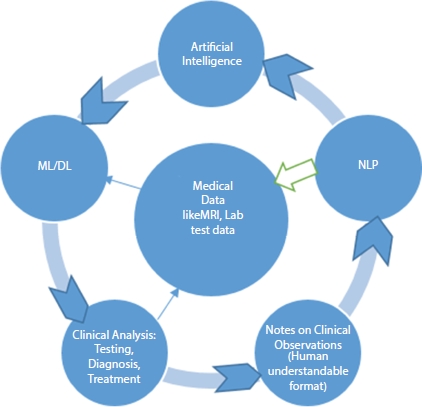
Figure 6.3 The visual representation of clinical data generation to natural language processing data enhancement, to machine learning data analysis, and to clinical decision-making.
The following sections describe few typical case studies, which enlightens the usage of ML and DL in medical domain.
6.7.1.1 Bladder Volume Prediction
The failure of bladder activities like urination and storage is prominent in many patients suffering from spinal cord injuries or by other diseases caused by neurological ailments. The bladder activity is regained by medicines in some cases and in many usages of sensors to monitor and trigger alarm to indicate the need to empty it is achieved. The data from these sensors in the form of digital values are processed along with the other factors recorded and observed in any patients body is processed by smart neuroprostheses. These are composed of two components, internal unit available inside the patients’ body, and external unit is a wearable one. The internal unit records signals and these are processed by external unit with complex algorithms to activate the simulation commands related to the required neurological activity [34].
The existing mechanism is improved by including the activities of the external unit into the implantable device (internal unit), for this pressure sensor along with volume sensors are used. The ML-based quantitative and qualitative are used to achieve the required outcome. The neural activities are recorded, identified, and categorized as level 1, 2, and 3. The use of ML-based mechanism greatly reduced the cost involved with hard used and also reduced the usage of power to a great extent. The quantitative and qualitative mechanisms initially undergo a learning phase while in offline mode; the sensors learn to detect the factors responsible for real-time monitoring [35]. The learning phase deals with digital data conditioning, matching the closely related neural activity with that of the bladder status, background activity monitoring, volume curve analysis, and pressure prediction. In this, linear regression is used in predicting the level of bladder status as 1, 2, or 3, as well as regression method is used to analysis volume and pressure estimation. On-the-fly spike sorting algorithm is used on DSP which shows significant improvement than existing works.
6.7.1.2 Epileptic Seizure Prediction
As a neurodegenerative disease, Epilepsy is characterized by sudden, unpredictable and almost instantaneous seizures [22, 23]. Long-term intake of medicines or surgery is the solutions to control this degenerative disease. Surgery is still considered less as an option since it has a marginal success rate; this motivated the researchers to find a better practice. The earlier works were not able to present the region of onset of seizures. The AI-based approach made it possible to withstand the skewness in data distribution. One of the major issues in identifying seizures is the high density analyses required to be performed on iEEG signals. The spectrum-weighted adaptive directed transfer function (swADTF) [24] based on ML concepts helps in identifying generators of seizures and sinks. Further research in prediction of seizures is carried out in tracking features that enhances the outcome along with ML and DL techniques.
6.8 Challenges and Future of Healthcare Systems Based on ML and DL
Like any other expertise, ML and its subset also faces numerous bottlenecks and challenges. Enormous high quality dataset is the challenging requirement of these healthcare systems. Even though amplification of these data sets are done to increase size of the existing data reserve and by allowing the new images to maintain their original attributes helps to some extent. These new data are considered as training sets by these complicated neural networks.
Every medical image has many underlining information hidden init. A radiologist may view a medical image and identify many findings and produce different diagnosis report based on the image, but a CAD system will provide insight with respect to a specific focus only. A need for multi-purpose algorithm that effectively identifies multiple defects in a single image is the greatest expectation from the on lookers. These procedures are not generalized (one algorithm for all disease diagnosis) as well as they are not equipped to provide the underlining reasons for the incidence like a radiologist.
Lack of usage of 3D image is still a great issue while proceeding with DL approaches as well standardization of data format used while collecting data is still a challenge. Large data set processing needs more precise training along with specific algorithm to provide accurate outcome. These enormous data sets make these procedures more problematic and delicate. The wrong interpretation leads to legal issues is also a major concern.
The future healthcare system based on AI and its subsets will render a path that makes it possible to diversify hospitals as one place to treat critical illnesses while clinic are used to treat less urgent cases. A centralized hub of data is connected to all units irrespective to location but they are connected with respect to expertise in the treatment and disease domain, thus directing the patients to the exact service provider and practitioner for quick and accurate treatment with common to all payment schemes.
These procedures help clinicians as well by reducing the rate of burnout they face while attending to patients with minimal resources to dispense. These improve the workflow and work pattern by cutting down the human effort required in the administrative sector. The knowledge acquired with respect to disease symptoms, pattern, diagnosing procedure, and treatment plan provided to every individual, the models train themselves to assist the clinicians as well as patients, too.
6.9 Conclusion
An innovative approach to decipher medical data and understand the information provided by those modalities as well as statistical data AI provides a better path. With the benefits, there comes the bottleneck with these approaches which are to be tackled effectively in future to make human life better than the existing one. Proper training and by providing adequate knowledge to clinicians in terms of AI will provide a better network to handle these medical data. In future, data from various foundations will be used to uncover similarity factors in identifying diseases, and it will be used to predict the risk value of any individual, reduce waiting time for patients, and thus increase productivity in hospitals and healthcare systems. The healthcare systems are equipped in such a way that they predict risk development in a human being before it gets worse. These predictions will be projected not only based on health records of an individual rather based on the demographic details; thus, it helps to break the notion of SDOH (Social Determinants of Health). Networking models based on DL with generalized algorithm to analyze any kind of data to predict any type of disease is the need of the hour.
References
1. Lundell, L., Attwood, S., Ell, C., Fiocca, R., Galmiche, J.P., Hatlebakk, J., Lind, T., Junghard, O., Comparing laparoscopic antireflux surgery with esomepra-zole in the management of patients with chronic gastrooesophageal reflux disease: a 3-year interim analysis of the LOTUS trial. Gut, 57, 1207–1213, 2008.
2. Liker, H.R., Ducrotte, P., Malfertheiner, P., Unmet medical needs among patients with gastroesophageal reflux disease: a foundation for improving management in primary care. Dig. Dis., 27, 62–67, 2009.
3. Jones, R., Armstrong, D., Malfertheiner, P., Ducrotte, P., Does the treatment of gastroesophageal reflux disease (GERD) meet patients’ needs? A survey-based study. Curr. Med. Res. Opin., 22, 657–662, 2006.
4. Nocon, M., Labenz, J., Jaspersen, D., Leodolter, A., Richter, K., Vieth, M., Lind, T., Malfertheiner, P., Willich, S.N., Health-related quality of life in patients with gastro-oesophageal reflux disease under routine care: 5-year follow-up results of the ProGERD study. Aliment. Pharmacol. Ther., 29, 662–668, 2009.
5. Olberg, P., Johannessen, R., Johnsen, G., Myrvold, H.E., Bjerkeset, T., Fjosne, U., Petersen, H., Long-term outcome of surgically and medically treated patients with gastroesophageal reflux disease: a matched-pair follow-up study. Scand. J. Gastroenterol., 40, 264–274, 2005.
6. Dent, J., El-Serag, H.B., Wallander, M.A., Johansson, S., Epidemiology of gas-trooesophageal reflux disease: a systematic review. Gut, 54, 710–717, 2005.
7. Kripalani, S., LeFevre, F., Phillips, C.O., Williams, M.V., Basaviah, P., Baker, D.W., Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA, 297, 831–841, 2007.
8. Jiwa, M., Coleman, M., McKinley, R.K., Measuring the quality of referral letters about patients with upper gastrointestinal symptoms. Postgrad. Med. J., 81, 467–469, 2005.
9. Garasen, H. and Johnsen, R., The quality of communication about older patients between hospital physicians and general practitioners: a panel study assessment. BMC Health Serv. Res., 7, 133, 2007.
10. Halpern, R., Kothari, S., Fuldeore, M., Zarotsky, V., Porter, V., Dabbous, O., Goldstein, J.L., GERD-related healthcare utilization, therapy, and reasons for transfer of GERD patients between primary care providers and gastroenter-ologists in a US managed care setting. Dig. Dis. Sci., 55, 328–337, 2010.
11. Jones, R. and Ballard, K., Healthcare seeking in gastro-oesophageal reflux disease: a qualitative study. Eur. J. Gastroenterol. Hepatol., 20, 269–275, 2008, http://www.biomedcentral.com/1472-6963/11/111 Page 5 of 6.
12. McColl, E., Junghard, O., Wiklund, I., Revicki, D.A., Assessing symptoms in gastroesophageal reflux disease: how well do clinicians’ assessments agree with those of their patients? Am. J. Gastroenterol., 100, 11–18, 2005.
13. Flook, N.W. and Wiklund, I., Accounting for the effect of GERD symptoms on patients’ health-related quality of life: supporting optimal disease management by primary care physicians. Int. J. Clin. Pract., 61, 2071–2078, 2007.
14. Tytgat, G.N., McColl, K., Tack, J., Holtmann, G., Hunt, R.H., Malfertheiner, P., Hungin, A.P., Batchelor, H.K., New algorithm for the treatment of gas-trooesophageal reflux disease. Aliment. Pharmacol. Ther., 27, 249–256, 2008.
15. Tandel, G.S., A review on a deep learning perspective in brain cancer classification. Cancers, 11, 1, 111, 2019.
16. Bauer, S., Wiest, R., Nolte, L.-P., Reyes, M., A survey of MRI-based medical image analysis for brain tumor studies. Phys. Med. Biol., 58, 13, R97, 2013.
17. Menze, B.H., The multimodal brain tumor image segmentation benchmark (BRATS). IEEE Trans. Med. Imaging, 34, 10, 1993, 2015.
18. Giulia Clementi, D.S., Paoluzzi, A., Università Roma Tre, Scorzelli, G., Pascucci, V., Progressive extraction of neural models from high-resolution 3D images of brain, in: Proceedings of CAD’16, pp. 348–351, 2016.
19. Talo, M., Baloglu, U.B., Yıldırım, Ö., Acharya, U.R., Application of deep transfer learning for automated brain abnormality classification using MR images. Cognit. Syst. Res., 54, 176–188, 2019.
20. Emblem, K.E., Predictive modeling in glioma grading from MR perfusion images using support vector machines. Magn. Reson. Med., 60, 4, 945–952, 2008.
21. Marshkole, N., Singh, B.K., Thoke, A., Texture and shape based classification of brain tumors using linear vector quantization. Int. J. Comput. Appl., 30, 11, 21–23, 2011.
22. Wiebe, S., Eliasziw, M., Bellhouse, D.R., Fallahay, C., Burden of epilepsy: the-Ontario health survey. Can. J. Neurol. Sci., 26, 4, 263–70, 1999.
23. Fisher, R.S., van Emde Boas, W., Blume, W., Elger, C., Genton, P., Lee, P. et al., Epilepticseizures and epilepsy: definitions proposed by the international leagueagainst epilepsy (ILAE) and the international bureau for epilepsy (IBE). Epilepsia, 46, 4, 470–2, 2005.
24. Bou Assi, E., Rihana, S., Nguyen, D.K., Sawan, M., Effective connectivityanalysis of iEEG and accurate localization of the epileptogenic focus atthe onset of operculo-insular seizures. Epilepsy Res., 152, 42–51, 2019.
25. Dahmani, K., Tahiri, A., Habert, O., Elmeftouhi, Y., An intelligent model of homesupport for people with loss of autonomy: a novel approach, in: Proceedings of 2016 International Conference on Control, Decision and Information Technologies, St. Julian’s, Malta, 2016 Apr 6–8, pp. 182–5, 2016.
26. Rabhi, Y., Mrabet, M., Fnaiech, F., A facial expression controlled wheelchair forpeople with disabilities. Comput. Methods Programs Biomed., 165, 89–105, 2018.
27. Hudec, M. and Smutny, Z., RUDO: a home ambient intelligence system for blindpeople. Sensors, 17, 8, 1926, 2017.
28. Wu, Q., Zhang, Y.D., Tao, W., Amin, M.G., Radar-based fall detection based onDoppler time–frequency signatures for assisted living. IET Radar Sonar Nav., 9, 2, 164–72, 2015.
29. Lloret, J., Canovas, A., Sendra, S., Parra, L., A smart communication architecture forambient assisted living. IEEE Commun. Mag., 53, 1, 26–33, 2015.
30. García-Vázquez, J.P., Rodríguez, M.D., Tentori, M.E., Saldaña, D., Andrade, ÁG, Espinoza, A.N., An agent-based architecture for developing activity- awaresystems for assisting elderly. J. Univers. Comput. Sci., 16, 12, 1500– 20, 2010.
31. Esteva, A., Kuprel, B., Novoa, R.A. et al., Dermatologist-level classification of skin Cancer with deep neural networks. Nature, 542, 115–8, 2017.
32. Bouton, C.E., Shaikhouni, A., Annetta, N.V. et al., Restoring cortical control of functional movement in a human with quadriplegia. Nature, 533, 247–50, 2016.
33. Marr, B., First FDA approval for clinical Cloud-Based Deep Learning in Healthcare, 2017, https://www.forbes.com/sites/bernardmarr/2017/01/20/first-fda-approval-for-clinical-cloud-based-deep-learning-in-healthcare/?sh=2b55eea161c8
34. Mendez, A., Sawan, M., Minagawa, T., Wyndaele, J.J., Estimation of bladder volume from afferent neural activity. IEEE Trans. Neural Syst. Rehabil. Eng., 21, 5, 704–15, 2013.
35. Mendez, A., Belghith, A., Sawan, M., A DSP for sensing the bladder volume through afferent neural pathways. IEEE Trans. Biomed. Circuits Syst., 8, 4, 552–64, 2014.
- *Corresponding author: [email protected]
