I can’t stand our child’s crying another minute! This has been going on since he was born. He’s the baby from hell! My husband told me that if I didn’t fix his crying, he was leaving home. We can’t find any babysitters to take care of him because he is so irritable. I worry that someone else might abuse him because they wouldn’t love him like I do. I’m exhausted and at my wit’s end!
These words, spoken by a parent with an irritable child, are depictive of the tremendous impact that an irritable child can have on the parent–child relationship and family life. Parents become frantic in their attempts to console their child. When nothing works, parents often feel ineffective. They may worry why their child appears unhappy most of the time. For the child, it is an unsettling experience to be chronically unregulated when things like transitions in activities and small frustrations set them off. They learn to depend on their parents to soothe them because they lack strategies for self-calming. And because they are irritable most of the time, they may not experience pleasurable interactions with others.
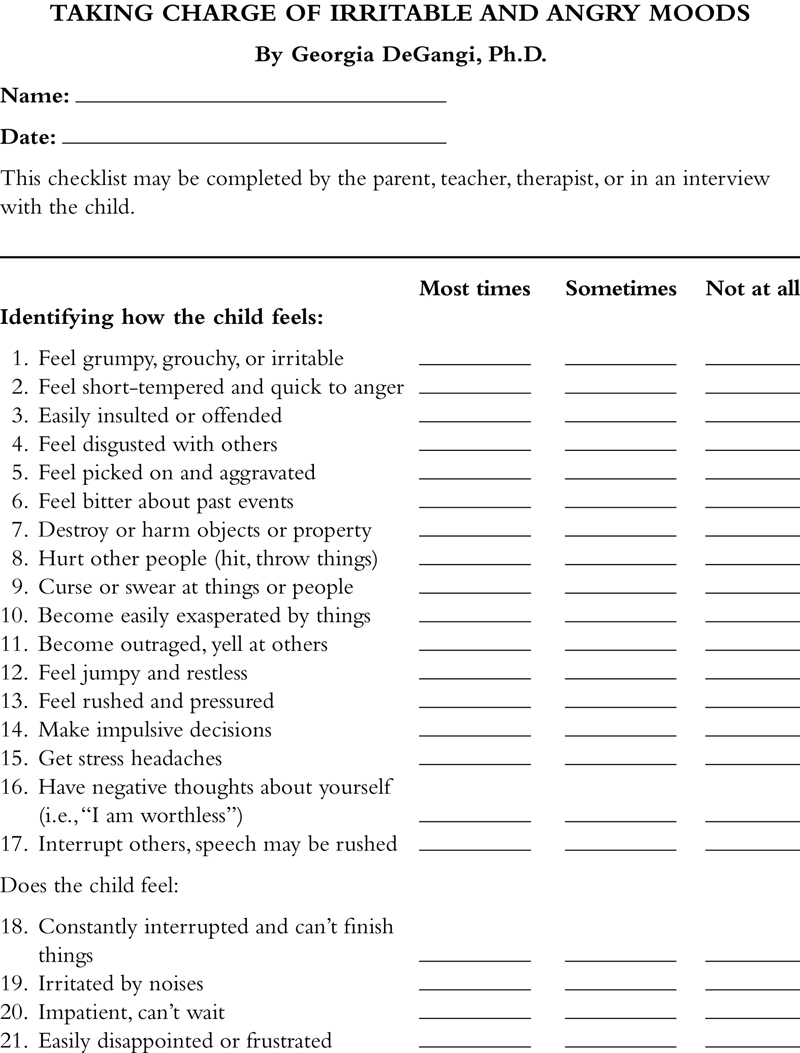
There are many reasons why a child is irritable or has mood regulation problems. To be most effective in treating these problems, it is important to understand the way in which emotion regulation develops in the young child. This chapter begins with an overview of different views of emotion to provide a framework for treating irritability and other disorders of mood regulation. Since a major aspect of mood regulation relates to how emotions are socialized, a developmental–structuralist framework is presented. Suggestions for treatment of different problems related to mood regulation and irritability are described along with several case examples of children at various ages. Lastly, a detailed checklist is provided that can help identify sources of irritability and target areas for treatment.
1. What is an emotion?
Emotions have a powerful impact on our experience of the world around us. Emotional expression provides a window into an individual’s internal experience of the world. They motivate our actions and affect the way in which we interact with others and our environment. Emotions provide life experiences with meaning. By guiding our thoughts and actions, emotions have a regulatory function, thus helping us to acquire adaptive behavior patterns and to motivate interactions with others (
Dodge & Garber, 1991). Through the expression of emotion, we can learn about how a person perceives him or herself and others, and how well they self-regulate when presented with challenging situations.
There are many individual differences in how people experience and express emotions and interact with others. Many people are predominantly happy, content, and curious. Others may be often withdrawn, sad, and depressed. Still others appear angry, destructive, and disorganized. Most people display different emotions and act differently depending upon the situation and their underlying mood at the time. But when a person is predominantly withdrawn, avoids other people, and has no interest in learning most of the time, it can affect their development and adaptability. Likewise, the child with a mood disorder who is angry, destructive, and overly aggressive will have difficulty engaging in appropriate interactions with others and in modulating their activity in everyday life.
Over the years, there has been considerable debate about what constitutes an emotion. Is it a subjective feeling state, such as feeling “depressed,” “content,” or “anxious?” Is it what motivates our interest in the world and guides our social interactions? Is emotion the outward motor expression of feelings—the smile, the scowl, the loud, stern voice, or the uplifted buoyant body posture? How much of emotion is affected by cognitive appraisal of a situation, event, or stimulus and how much by physical or autonomic responses (i.e., heart racing, cold clammy hands) that are experienced during anger, pleasure, or other emotional states? Most current views of emotion embrace all of these components. A broader view is generally accepted by emotion theorists who consider emotion to be the interface between the individual and his environment. Emotions mediate the individual’s capacity to adapt or respond to a variety of experiences. There are five major areas related to emotional regulation. These include:
1. Cognitive appraisal: Before, during, and after an emotion is experienced, the individual engages in cognitive appraisal. This process of evaluating the situation on a cognitive level determines what emotions are elicited. Some of the things that impact cognitive appraisal include:
a. Reading and understanding social cues: The irritable child may not be able to read and understand social situations and evaluate whether they should approach or withdraw. They may react in an unpredictable manner because of this difficulty.
b. Perception including face recognition and discrimination of affects: Some children have difficulty reading facial and gestural signals. As a result, they may misconstrue what a person is trying to convey. Often it is difficult for them to understand when firm limits are placed on them because of this problem.
c. Predicting one’s own behavior and that of others: A major goal for the child with mood regulation problems is to begin to predict their own behavior and modify it in response to different situational demands. Learning that certain behaviors have consequences is important to this process.
2. Physiological aspects of emotions: One of the things that help us to link meaning to emotions are physiological responses. As cognitive appraisal takes place, physiological responses activate arousal to allow the person to respond accordingly. This is important to prepare the person for action. For example, in dangerous situations, the person needs to be ready to flee. Without a physiological readiness, the person may not survive. Both neuroendocrine and autonomic states contribute to the physiological activation of emotions. Many irritable children are always in a state of hyperarousal and, therefore, do not have the typical physiological responses one needs to react in a calm and focused manner.
3. Expression of emotion: Communication of reactions, feelings, or intentions to others during social interactions is an important component of emotion. The motor expression of emotion is manifested through the neuromuscular system and consists of facial patterning, postures, and gestures. Often the irritable child expresses intense negative emotions (e.g., anger, distress, frustration). They have difficulty communicating more subtle ranges of emotions (e.g., express through words or facial expressions that they are beginning to feel frustrated vs. tantruming) and they may have little opportunity to express more positive emotions.
4. Socialization of emotions: As children develop, they are reinforced to express certain emotional displays. This process occurs first through the parent–child relationship, but if this relationship is affected by the child’s irritability and mood regulation problems, it is more difficult for the parent to provide positive social feedback. As the child grows older, they may have relationships that are negatively reinforcing. For example, others are likely to avoid them because of their bad temper, or they may have a history of bullying, being kicked out of play groups or school programs, and have few satisfying or rewarding relationships.
5. Modulation of emotion and mood states: Learning how to modulate emotions in response to internal states, situational demands, and the social context is a very important skill. How an individual perceives the experience of the emotion during and after its expression relates to the subjective feelings associated with emotions. Cognitive factors, such as memory and imagination play an important role in defining the subjective experience of emotions.
These components of emotion do not necessarily occur in this sequence; however, there is general agreement that the concept of emotion should include these five elements (
Scherer, 1984). Understanding the various elements of emotion regulation is important for treatment planning in working with children with regulatory disorders. In the next section, details about the different components of emotion regulation will be discussed with emphasis on how problems in each area may be observed and treated.
2. Cognitive appraisal
2.1. Reading of social cues
When faced with a situation, an individual makes a cognitive appraisal which affects the intensity and quality of the emotional reaction. The individual relies upon already acquired knowledge about similar situations, memories of past experiences, perceptual skills in reading signals or cues from the environment, as well as analytical skills in appraising the situation. This appraisal process is ongoing and may be manifested in a number of different emotional responses over time as the individual reflects upon past and current experiences. For instance, suppose the child thinks that a situation is very demanding. At first, the child may experience much apprehension and fear. If the child remembers that he was successful in a similar difficult situation in the past, he may feel challenged and excited after his initial response. However, if he experienced extreme frustration and feelings of incompetence in the past, he may seek to avoid another such experience and exhibit negative emotions. This is very common with performance anxiety.
How cognitive appraisal might impact a child with mood regulation problems is depicted by Owen, a 4-year-old child who was struggling at preschool. He often became irritable when there were transitions in activities, his space was invaded by other children, activities were more rambunctious, or when the classroom noise level became loud. He felt that he wasn’t ready to move on to the next activity when the children were expected to do so. Although he was a very competent child, he had trouble adjusting to change and would become distressed when expected to do certain tasks, such as share toys with other children or clean up his toys to get ready for snack. Usually after about 2 hours at school, Owen would begin to show his distress by hitting or biting other children or by withdrawing. His responses were very unpredictable with some good days, then followed by several days with multiple incidents. Each time he bit a child, he was sent home from school. Within a month, he was being sent home so frequently that his parents chose to keep him at home to give him a break from the stress of school. As we tried to work out a viable solution to the problem (e.g., getting a full-time aide to help him make transitions, to stop him before he bit another child, and to organize him when he appeared distressed), Owen began to make comments that he never wanted to go back to school again. In the next month that it took to find an aide, we saw Owen regress. With each day that he stayed home from school, he became increasingly more agitated, refusing to change his clothes, wanting to isolate himself in his bedroom, and screaming at his parents whenever they made the simplest of requests. As we reintroduced Owen back into school, we had to change his cognitive appraisal of school and himself to a more positive one. We were able to accomplish this by beginning with a short school day and a shortened week of school at first and using positive reinforcement from his aide for accomplishing tasks. We provided scheduled breaks during the day when he could reorganize himself (e.g., calming by sitting in a bean bag chair and looking at books, sucking on ice pops, or building a fort that he could go inside). We instituted a school and home program that reinforced good behavior and compliance, for playing friendly (e.g., not biting other children), making transitions (e.g., clean up toys when time for snack), and self-calming when agitated (e.g., asking for time alone in bean bag chair). Within a few months he became much more compliant both at home and school and was beginning to make more positive self-statements (e.g., “I want to go to school”; “I like doing this” instead of “I’m a bad boy,” “I’m angry”) and playing more with other children in a prosocial way.
2.2. Perceptual of facial expressions
Before a person can engage in cognitive appraisal, they need to be able to perceive signals and cues from the environment. One of the first ways that we learn to discriminate emotions is through understanding the meaning of various facial expressions. There are several important components that comprise this skill. These include:
1. Perceptual understanding of the face and its structural components: Discrimination of the face-hair outline develops as early as 4–7 weeks of age. By 5 months, infants become interested in the mouth and have a concept of “faceness” (features of the inner face as distinctive from the head shape). And by 7 months, the infant can detect different poses or angles of the face.
2. Recognition of affective expressions: The reading and understanding of different facial expressions (i.e., smiling or frowning faces) relies upon the integration of auditory and visual perceptual skills over time and space. It is the stopping and starting of facial movements that helps the infant to discriminate changes in facial expression. Between the ages of 3 and 7 months, the infant gradually acquires the ability to differentiate an increasing number of expression changes. For example, the 3-month-old can distinguish smiling, angry, or frowning faces. By 5.5 months, the infant can distinguish surprised faces and the 7-month-old can distinguish happy from fearful faces.
3. Simultaneous perception of vocal expressions, speech content, gestures, and body posture changes: This skill requires perceptual mapping of visual and auditory cues and their related meanings. The neonate is already attuned to characteristics of the human voice and can distinguish between the mother’s and a stranger’s voice. By 3–4 months, the infant can detect synchrony of voice with a moving face. Five to 7 month olds are able to distinguish when facial and vocal expressions match. A developmental task for all persons is to learn how to process both visual and auditory cues and their synchronization in reading facial signals. Children with autism spectrum disorder or nonverbal learning disability frequently struggle with this developmental task.
Sasha was a 10-year-old child with nonverbal learning disability who often misconstrued facial expressions in others and consequently attributed emotion to them that was inaccurate. In a group play situation, children were playing out a pretend play scenario where they built a fort to prevent the mean troll from scaring them. No matter how much facilitation she received from the therapist, Sasha would not join in the play with the other girls, and instead assumed the role of an angry monster who stomped around the room and roared. After the group was over, Sasha said, “The other girls were mean to me. They wouldn’t let me play with them.” Obviously Sasha had a completely different view of what happened in this play scenario and somehow projected her feelings into her role as the angry monster.
4. Understanding the meaning of facial expressions during interactions: This involves skills, such as differentiating a genuine smile from a forced smile or identifying different types of cries in a crying baby. Understanding facial expressions and their meanings begins through instinctual imitation when the infant reads and practices facial signals during interactions, such as mouth opening or tongue protrusion. By 6 months, the baby is responsive to the facial expressions of their mother. For example, if their mother looks sad, the baby will show more sadness, anger, and gaze aversion (
Termine & Izard, 1988).
Some children with mood regulation problems have difficulty in the perception of facial expression and in reading and understanding affective expression. They seem to become overwhelmed by emotional expression and may turn away to avoid eye contact or they may misconstrue the meaning of different facial expressions. One example of how this plays out is when parents report that no matter how clear their signals are when setting limits, their child does not listen or the child reacts by laughing at them. Suppose you present a picture of two children teasing another child to a 6-year-old child who has problems reading social cues. The child may misread the picture and say that it is a picture of three children playing ring around the rosey. There are also some children who have perceptual problems in recognizing different people’s faces and may react as if they have never seen the person before. Some children may be overwhelmed by anxiety or overstimulated by sensory input to the point that they cannot process verbalizations while also reading facial and gestural cues.
For example, 11-year-old Walter appeared very stiff and uncertain when interacting with others. He was frequently so anxious that he claimed that he couldn’t hear what others said to him, as if his ears were plugged up with fuzz. In fact, the middle ear muscles do constrict when a person is anxious causing this phenomenon. Not only that, but Walter would be so overwhelmed by crossing the street in front of my office building as he walked from his mother’s car, that he usually began his therapy session asking me to be very quiet and calm for at least the first 10 minutes to help him transition into “interactive” mode. I was aware that I had to keep my facial expressions as unanimated as possible and even to speak with less inflection. We practiced different styles of interacting (i.e., slower paced, benign topics to more animated, emotionally evocative topics) in addition to talking about his understanding of my facial and gestural cues and his internal state of overload.
In working with children with mood regulation problems, it is important to determine if the child is struggling with the perceptual aspects of facial expression and/or reading and interpreting social or affective cues. It is important to observe how much the child can process and to provide the right amount of stimulation that allows them to take it in without becoming overwhelmed. For example, Nina, a 6-year-old child with problems reading facial cues, enjoyed playing dress-ups. She particularly liked playing “Super-Girl,” putting on a gold cape and silver leggings. Nina liked to play out disasters, such as having cookies burning in the kitchen, little animals stuck in crevices, or babies getting lost in the woods. It seemed that she liked seeing the therapist express exaggerated expressions of alarm or surprise. She would play Super-Girl who would come to the rescue of the therapist in the burning block house. At first Nina needed the therapist to do the same script each time so that she could predict and understand what affective expressions went with which scenarios, but after a while, Nina liked it when the therapist made other things happen that might be silly or novel (i.e., a stuffed animal purposely sets the fire just so he could ride down Super-Girl’s fireman ladder). It was important to move from more expressive emotions to more subtle ones and from predictable events to ones that were less predictable. The dress-ups and fantasy play were ideal ways of helping Nina to learn how to read social cues.
5. Neural mechanisms underlying perception of facial expressions: The processing of emotional expression involves complex pattern recognition and coordination of visual (e.g., facial expressions) and auditory inputs (e.g., voice intonations). Studies of patients with hemispheric dysfunction have shed light upon the role of the right and left hemispheres in the perception and comprehension of visual and auditory stimuli related to emotional expression.
Generally, the right hemisphere is dominant in the recognition of visuospatial and auditory patterns and is important in integrating holistic perceptual properties. Some of the specific functions of the right hemisphere include the following:
a. Mediation of attention and emotional behavior,
b. Face recognition,
c. Discrimination of emotional expressions,
d. Comprehension and expression of affectively intoned speech,
e. Judging the quality of an emotion (e.g., positive or negative),
f. Recall of facial expressions from a model or picture,
g. Inhibition of inappropriate positive affects (pathological laughing).
The left hemisphere also plays an important role in cognitive appraisal of emotion. The left hemisphere is important for the following functions:
a. Verbal mediation and verbal labeling of emotional faces,
b. Motor planning of facial expressions (i.e., smile, show gums),
c. Inhibition of negative affective expression (pathological crying),
d. Comprehension and memory of emotionally charged stories.
There are some functions, however, that are attributed to both hemispheres. These include the following:
a. Perception of humorous content of pictures,
b. Naming and selecting emotional faces, although this tends to be a right hemisphere function more than left.
Understanding what neural mechanisms might be compromised for a child is useful in treatment planning. For example, some children with significant language impairments struggle with labeling emotions and may repeatedly ask questions, such as “Are you happy?” when they see your smiling face. In contrast, children with nonverbal learning disabilities may need concrete verbal labels to help them interpret social interchanges (i.e., “watch for when Michael looks away from you and stops playing with the ball, then ask him if he wants to do something else with you”).
Jeanie was an 11-year-old child who often smiled or laughed when talking about a distressing event (i.e., being bullied at school for using a rolling backpack). She seemed unaware that her facial expression was a mismatch with her verbal content. Interestingly, as she became more aware of this behavior, she became more in touch with the depth of her feelings. It was only then that she could process how angry she was by the bullying events at school. Sometimes she would crush bubble wrap in her sessions with me as she talked about these events, thus giving her a physical outlet for her anger and helping her body to process the anger she felt inside. We used a variety of techniques to help her gain more of a match between her internal mood state and her outward expression of emotion. It was useful to link verbal interpretations of visual feedback by videotaping her and watching the tape together to discuss what she was feeling in the moment. She also learned to check her expression in the mirror to see how she presented herself to others and to see if there was a match between her face and her internal emotions.
2.3. Predicting one’s own behavior and that of others
Social situations provide many cues that assist the individual in integrating perceptual and cognitive meanings. When a situation is highly novel or the person lacks experience or skill in interpreting meanings, the individual tends to rely heavily upon feedback from other people, particularly those who are important to them (i.e., peers, parents), as well as cues about a situation. A classic example is that of the 9-month-old infant who is crawling on a clear plastic platform that presents the illusion of a visual cliff. The child at this age does not have the perceptual understanding that he might fall off a cliff, therefore, he relies upon his mother’s expression. Whether his mother smiles and encourages him to crawl or expresses fear will affect his appraisal of the situation as one that is safe or dangerous.
The young child is more dependent upon facial cues of individuals experiencing the event, but as children grow older through the school-aged years, they rely more on situational cues. As children mature, they are also better able to integrate both facial and situational cues (
Hoffner & Badzinski, 1989). We see this in many everyday situations with adults as well. Suppose you are invited to attend a social gathering of persons from a highly different socioeconomic and cultural background. Most individuals would watch others who are comfortable with the situation to determine what behaviors are expected. Men and women may talk together in segregated groups. It may be expected that jokes will be received with modest chuckling versus loud laughing. The hostess may be offended if the guests do not eat second and third helpings of food.
3. Physiological aspects of emotion
Descriptions of emotion often involve both physiological responses (e.g., peripheral autonomic nervous system) and facial expression. The physiological component of emotion may involve changes, such as increased sweating, throbbing or racing of the heart, pupillary dilation, facial flushing or blanching, and gastric motility. These autonomic responses (i.e., heart rate) often parallel facial expressions associated with emotion (
Darwin, 1872). Darwin suggested that there were specific neural pathways that provide communication between the brain and the periphery associated with emotions. When emotional states occur, heart rate changes occur which in turn influence brain activity.
3.1. Mediation of emotion via autonomic responses
There has been considerable debate about whether the emotion or the autonomic response occur first.
James (1884) described emotion in terms of afferent feedback from the viscera to the brain. Different emotions were caused by highly specific changes in
the autonomic nervous system. For example, an individual may experience heart racing and increased sweating in a stressful situation. These autonomic responses would help the person to label feelings of fear.
In contrast,
Cannon (1927) argued that autonomic changes occurred in response to brain processes which defined the experience of emotion. A person would first assess a situation as one evoking fear, then would experience the associated autonomic responses.
The question posed by these two theorists is an interesting one. How would a lack of afferent feedback influence the ability to experience emotions? Imagine the patient with an artificial heart who would not experience shifts in heart rate during different emotional experiences. Would this individual feel emotions in the same way as previously experienced before heart surgery?
3.2. The specificity of emotions
Although there seem to be differences in opinion about the role of afferent feedback in the experience of emotion, research shows that different emotions elicit distinct autonomic responses.
Ekman, Levenson, and Friesen (1983) have demonstrated a degree of specificity between autonomic activity and facial expressions. It appears that there are intimate links between the neural mechanisms controlling the facial muscles and the autonomic nervous system. When emotions occur, specific facial expressions and unique patterns of autonomic activity are elicited depending upon the emotional state. Ekman and his colleagues suggest, unlike the James theory, that peripheral feedback from the autonomic nervous system to the brain is not required in order to experience emotion.
But what happens when a person assumes a facial expression by simply contracting different facial muscles that are part of that particular expression? Do they experience the emotion as well? Here is an experiment for you to try. Raise your brows, hold them raised, and pull your brows together, now raise your upper eyelid and tighten the lower eyelid, and stretch your lips horizontally. What does your face look like? Your face should look as if you are experiencing fear. Did you feel any autonomic changes that were related to fear?
In an experiment where subjects assumed different facial expressions in the same way that you just did, the subjects experienced different autonomic changes, such as changes in skin temperature and heart rate (
Ekman et al., 1983). Of course, the autonomic changes are mild in contrast to when the emotion is actually experienced. These results may explain why some people who are feeling low can pick up their mood by “putting on a happy face.” The act of smiling may actually elevate the way we feel even if it starts out as deliberate rather than spontaneous.
3.3. Autonomic responses associated with discrete emotions
Fear and sadness result in cooler skin temperatures while angry faces result in increased skin temperatures. Heart rate generally increases with negative emotions (e.g., anger, fear, and sadness) but decreases with other emotions, some of which are positive (e.g., happiness, disgust, and surprise).
3.4. The Polyvagal Theory of Emotion
The link between autonomic nervous system activity and social communication is described in the Polyvagal Theory of Emotion (
Porges, 1995). In this theory, there are three phylogenetic stages of neural development. The first stage represents the primitive unmyelinated vegetative vagal system. It is characterized by immobilization responses. The vagal system functions in the capacity of helping the body digest food and to reduce cardiac output when the person is confronted with either a novel or threatening situation.
In the second stage, the spinal sympathetic nervous system is activated which serves in increasing metabolic output while inhibiting primitive vagal influences. This stage is one of mobilization and is represented in the person’s capacity to engage in “fight or flight” when confronted with threatening stimuli.
The third stage is characterized by the myelinated vagal system that helps to regulate cardiac output and to foster engagement and disengagement with the environment. It is brain stem mediated and it controls facial expression, sucking and swallowing, breathing, and vocalization. This system has an inhibitory effect on the sympathetic nervous system, effects on cardiac function, and promotes physiological calming.
Porges (1995) theorizes that this is the system that provides the neurological basis for early mother–infant interactions, as well as the development of complex social behaviors. Some of the social behaviors that this system impacts are emotional expression, vocal communication, and contingent social behaviors.
In treatment we frequently use deep breathing exercises to help calm states of agitation, anger, or other dysregulated mood states. The polyvagal theory helps to explain the neural mechanism behind why deep breathing helps calm the nervous system to allow for better social engagement and attachment to others.
3.5. Neural mechanisms underlying physiological changes
Afferent feedback from the facial and postural muscles plays an important role in modulation of emotion. When these afferents were severed in an experiment with cats (reticular formation left intact), the cats became mute and completely lacking in facial expressiveness and purposeful behavior. They also became hyperexploratory but lacking in intentionality (
Sprague, Chambers, & Stellar, 1961). It seems that afferent feedback mechanisms are important to self-monitor emotional expression and to organize purposeful exploration.
Developmental shifts are observed in neurophysiological control of facial expressivity. With maturation, the infant displays a greater range of expressivity but, at the same time, can self-regulate affect in response to situational demands, thereby showing a trend toward greater cortical control of facial expressions. There is also greater control of autonomic functions with age. As the individual matures, they are less likely to respond with high variability in autonomic responses (i.e., heart rate and respiration) as they learn to adapt to various novel or stressful situations. Therefore, in normal development, there is greater myelinization of the brain in conjunction with greater regulation of autonomic functions that parallels the affective expressivity and control.
Some individuals seem to have a great deal of difficulty in recognizing the autonomic responses that accompany emotions. As a result, they may not perceive that they are getting angry or upset until they suddenly blow up. This has important implications for parents who may be at risk for abusing their children. It is important to teach them how to recognize the bodily signals that mean they are getting angry (e.g., stiffening of muscles, skin getting hot, stomach churning, and so on) so that they can cool off before they explode at their child. By tuning into these body signals, the person can learn to control their behavior better.
The task of learning how to read body signals was a major piece of intervention with 9-year-old Alexis. She had a short fuse and would explode, screaming at her parents and throwing things whenever she experienced the slightest bit of frustration. Her tantrums would go on for several hours which resulted in the whole family being up to all hours of the night trying to console her. Her parents thought that Alexis looked like a wild animal with hair falling in her face, her body slumped over, and hands clawing at the air like a tiger. Alexis would also shut down when she became depressed, hiding under a table or sitting inside her closet for hours on end. These mood changes would come on suddenly and once in an intense mood state, Alexis had considerable difficulty coming out of them. Although she was a child who was helped by medications, through therapy Alexis began to be able to recognize when she could feel her mood shifting to anger, frustration, or sadness. When she felt herself becoming upset by things, she could focus on what her body was telling her, then take steps to soothe herself before her mood state progressed too far. Doing things like jumping on a trampoline, kicking a soccer ball, or playing piano helped her to self-calm. Alexis also talked with me about her “Tantrum Warning Device,” (a rainbow colored semicircle ranging from red for anger, orange for agitated, yellow for frustrated, green for calm, and blue for sad) a concept that we used to help her predict what situations caused her to become upset. For instance, doing homework almost always caused her warning meter to go up to a “medium sizzle.” Not getting to stay up late and play Nintendo would make her get “boiling mad.” The object of the warning device was to recognize when her mood was moving from mild to mild-medium or medium anger and get it back down again by calming herself.
4. Expression of emotion
The expression of emotion involves facial expressions, gestures, posture, movements, and vocal responses. This outward display of emotion, also called “affective expression,” is linked to our inner emotional experience. The expression of emotion is primarily facial. Since the facial musculature has greater sensory and motor innervation than postural muscles or visceral organs (i.e., heart), expression of emotion through the face is much more specific. Facial expressions provide information or meaning about the emotional experience of the sender to other persons. They also provide internal feedback to the person emitting the facial expression.
In order for an emotional signal to capture someone’s attention, it should involve as many dimensions as possible. The toddler who sees his parent frown, stomp his foot, point with his finger, and firmly state “NO!” knows that his parent means business. In contrast, parents who have difficulty setting limits may display weak or even discrepant signals that are difficult to read and are confusing to the toddler. An ambivalent parent may smile as they say, “Now, don’t throw your food, honey!” Some toddlers may be confused by this mismatch of signals. Others may know what is expected of them, but continue on with their disruptive activity suspecting that there are no consequences to their actions.
4.1. Universality of emotional expression
For many years, there has been an argument about whether facial expressions are universal or specific to cultures. One way to study this is by observing cultures that have had little contact with other cultures. Although people in such cultures do not display any facial expressions that are not observable in other cultures, there are certain standards or norms that individuals follow in expressing emotions.
Ekman and Friesen (1969) have termed these “display rules.” These are cultural norms that are internalized about when, where, and how an emotion is displayed. Therefore, affective expression will vary considerably depending upon socialization and cultural norms. For example, in Western cultures, males are not expected to cry and females are generally expected not to display anger. In some societies, joy may be expressed through an uplifted body posture, laughing, large body movements, and loud vocal exclamations while in others, a simple smile may be all that is observed. Regardless of culture, there are certain facial expressions of emotion that are universal (
Izard, 1971). The facial expressions that are universal to all cultures are fear, surprise, anger, disgust, distress, and happiness. There is less universality for interest, contempt, and shame.
4.2. Developmental differences in affective expression
Neonates are capable of expressing a wide range of emotions including interest, distress, disgust, and pleasure (
Izard, Huebner, Risser, McGinnes, & Dougherty, 1980). Young infants are able to express positive affects including interest and enjoyment. They can also express negative affects including distress, disgust, fear, anger, and shame.
Baby cries are heard in the first few minutes of life, however, different types of cries and cry expressions related to different negative affects (sorrow, fear, anger, pain) develop as the child matures. This differentiation in emotional expression occurs for all emotions and relates to the individual learning to attach different meanings to events.
5. The socialization of emotions
Some primary emotions appear to be innate, however, they become adaptive over infancy, particularly through socialization. Affect is learned very early in life and becomes appropriate according to demands placed upon the individual. For the infant, this occurs
in parent–infant interactions. Up to 6 months of age, the infant’s facial expressions are highly changeable or labile, changing every 7–9 seconds (
Malatesta & Haviland, 1982;
Malatesta, Culver, Tesman, & Shepard, 1989). This high variability in expression gives the caregiver many opportunities to respond and shape emotions. Mothers actually respond to about 25% of their infant’s facial expressions with a lag time of less than 0.5 second. This is the time most optimal for instrumental conditioning. Most mothers will show a dissimilar affect than their babies and imitate their baby’s expression only 35% of the time. Mothers tend to reinforce positive emotional expressions through smiling and talking to their infants, particularly in younger infants (i.e., 3 month olds). By 6 months, mothers do less nonverbal acknowledgment of their baby’s affect.
This information is important in our work with children. We need to be aware as therapists that our facial expressions are highly changeable and that we only reinforce about 25% of our client’s facial expressions. As a result, in treatment of some individuals, we may purposely slow down our affective expressions so that the child is better able to process our affect and we may choose to remark on certain emotional expressions in our client at helpful moments. Noticing subtleties in affect, such as a tearful eye, a fleeting grimace, a choked voice, or the child sipping water to soothe themselves may be clues to the person’s true emotional core.
Facial expressions of infants are signals to their caregivers to communicate with them. The competent infant becomes adept at providing clear signals to the caregiver when expressing needs, but the caregiver must also be sensitive in reading and reacting to these signals. When an infant displays a high-intensity expression, parents tend to engage in more stimulating interactions with their babies.
What happens when the infant is less capable of expressing affect because of motor problems? Mothers of Down’s syndrome infants tend to compensate for low-intensity expressions by becoming more stimulating in their interactions with their babies. Parents of infants who appear less alert or less responsive may try to compensate for their infant’s diminished emotional expressions by overstimulating them (
Sorce & Emde, 1982). These types of infants are less emotionally available and tend to be less rewarding for the parents.
In contrast, what happens to the parent–child interaction when the infant is irritable? In our study of mother–infant interactions, we found that mothers of regulatory disordered babies were likely to engage in more anticontingent responses (e.g., doing opposite of what baby was seeking) and tended to overstimulate their baby by talking a lot rather than engaging in active play (e.g., symbolic play or rough housing). The mothers also appeared depressed by showing flat affect (
DeGangi, Sickel, Kaplan, & Wiener, 1997). It seems that these mothers were more comfortable using distal and verbal modes of communication than proximal, gestural, or sensory modes of communication. They seemed to have difficulty reading their infants’ signals, in responding in a contingent manner, and in facilitating their infant’s representational capacities. In everyday situations, this
may affect the mothers’ capacity to support their children’s abilities to self-regulate or organize planned actions to manage distress. The infants with regulatory disorders had difficulty responding in a contingent manner and in providing effective gestural, affective communication during sensory play situations (e.g., play with textured toys). Their behaviors and communicative signaling may evolve around their experience of distress, sensory hypersensitivities, and the ability to cope with heightened levels of positive and negative emotions. The result is a miscoordinated interaction between mother and child that includes asynchronous, disengaged behaviors.
5.1. The inhibition of affective expression
It is possible for a person to inhibit expression of emotions when trying to conceal their reactions. Usually the person cannot totally inhibit the internal feelings recruited by an emotion although they may be able to combat a bad mood by engaging in certain activities (i.e., exercise, exciting activities). Oftentimes, the person’s voice will reveal their true emotions even if they manage to keep a poker face. For instance, a person may be telling you about a very stressful event in their life and saying that it no longer bothers them, but you can detect a quivering or a cracking in the voice even though they are smiling as they talk. It is also harder to inhibit signs of emotion in the face than it is in the body. A person who is feeling depressed and sad may be able to keep an uplifted body posture, but their face will often give away their sad mood.
5.2. Neural mechanisms mediating affective expression
Affective expression does not suddenly emerge, but rather it is the integration of cognitive, perceptual, and motor skills. This occurs as the result of increasing functional connections between specific brain regions instead of emergence of specialized localized brain centers. The right hemisphere is specialized for voluntary facial expressions, such as posing for a picture. These types of deliberate or voluntary facial expressions involve visual–spatial skills (i.e., knowing what a smile looks like, then assuming one). Interestingly, deliberate facial expressions that are expressed without the corresponding emotion are usually asymmetrical as opposed to spontaneous ones. For instance, a deliberate smile tends to be stronger on the left side of the face in right-handed subjects (
Ekman, Hager, & Friesen, 1981). Timing also differs. For instance, the expression may be too short or too long and the onset and offset may be abrupt. Think of the person who is trying to be cheerful but feels depressed. They may put on an exaggerated smile of the lips but without the wrinkling around the eyes that goes with a spontaneous smile. Or the person may have a fake laugh that is too loud and too long.
A number of studies have reported that the left side of the face dominates affective expression—that is, the left side of the face shows greater facial movement and is more intense than the right side during spontaneous emotion. Most investigators have attributed this to right hemispheric lateralization for emotion (
Fox & Davidson, 1984).
Both hemispheres contribute differentially to the experience and expression of positive and negative emotions. States of positive emotion are associated with left frontal activation while states of negative emotion are associated with right frontal activation (
Davidson, 1984). The left hemisphere also plays an important role in the inhibition of negative affects by suppressing right hemispheric activity. This inhibition begins when children develop verbal fluency, around 18 months of age.
The emergence of different emotions also follows a developmental progression that relates to neural maturation. The emotions of interest and disgust appear to be under unilateral hemispheric control and are present in the newborn at a time when there is little functional interconnection between the hemispheres. Fear and sadness usually do not emerge until the end of the first year when interhemispheric communication is developing. However, a child who has been maltreated by caregivers, or hospitalized for a serious illness, or whose caregiver is seriously depressed may suffer from an anaclitic depression in the first year of life. The onset of locomotion, a behavior associated with commissural communication, also occurs with the emergence of fear. The baby is not only able to experience fear but can escape fear-provoking events with efficiency. Expression of sadness usually develops in the second year of life and is associated with alternation between approach and withdrawal, thus implicating interhemispheric communication (
Fox & Davidson, 1984).
Feedback from the body may serve to help regulate affect. Certain body postures give more feedback than others. For example, a “sad” body posture with collapse into flexion causes the least firing of proprioceptors in the neck and trunk. A “happy” posture causes a high degree of proprioceptive discharge from the extensors. It is used therapeutically when we use muscle relaxation techniques on the highly anxious or hyperaroused individual. Through a change in body posture, the goal is to help the person to unblock negative emotions or to alter arousal for more focused purposeful attentive behavior.
Children with sensory integrative dysfunction, especially problems related to muscle tone and motor planning, are likely to have difficulty in modulating affective expression because their bodies do not provide accurate feedback related to postures that accompany facial expressions. Sometimes there are major implications for the child. The following case example depicts how these problems might play out.
Patricia was a very bright 6-year-old child with severe motor planning problems. She appeared happy and content, but experienced enormous frustration that she was so accident prone and slow to learn things that should be automatic (e.g., riding a bicycle). She was just beginning to dress herself and was still struggling with tasks like tying her shoelaces and buttoning her clothes. Patricia had developed high anxiety, behavioral resistance, and learned helplessness related to any task that required motor planning. For example, Patricia was afraid of heights that affected her ability to climb stairs. When she would climb a flight of stairs at home, school, or other places, such as a museum, she would become overwhelmed with fear. Instead of using her words to say she was afraid, she would cling to her mother or father and say she had to go home right away, saying that she was going to vomit. She did, in fact, sometimes become motion sick in the car and would experience autonomic reactions to movement (e.g., feeling like she would vomit after swinging on a swing). Patricia did not like to take any risks and appeared to derive satisfaction from activities when she was involved vicariously. For example, she would command her parents to dress her dolls in certain outfits, changing their clothes several times in a row, then she would want them to set up her doll house in a particular way, often changing her mind and wanting them to set it up all over again. If they did something different than she wanted, she would yell at them loudly and begin to throw tantrums. Patricia was a child who often assumed a watchful role in her life activities, but when she engaged with others, she would often become intense and verbally aggressive. It seemed that the lack of adequate sensory feedback that she experienced from her body coupled with severe motor planning problems contributed to her strong sense of inadequacy and inability to modulate affect. She seemed to function at two ends of the spectrum—either passive and submissive or screaming and intense. Becoming more attuned to feedback from her own body while working on appropriate ways to control others and the environment were emphasized in her therapy program.
6. Modulation of emotion and mood states
The modulation of emotion is intimately connected with the process of “self-directed regulation” (
Tronick, 1989,
2007). When a person is developing a new skill or lacks prior knowledge of the meaning of a situation, they tend to rely upon others for cues to communicate emotional meanings. For example, an infant is reaching for an out-of-reach toy. Soon the infant feels frustration, fusses, and is on the verge of quitting. However, the father, observing this activity, encourages the baby to continue reaching until he has successfully attained the toy. The father’s encouragement served to motivate the baby’s persistence while deterring frustration, tantruming, or other negative behaviors in this example.
As the child develops, self-directed regulatory behaviors emerge (
Gianino & Tronick, 1988). These involve the individual’s internal capacity to shift negative emotions to more positive ones to allow for goal-directed activity. The infant who engages in self-calming techniques, such as sucking his thumb, or looking away momentarily before resuming the activity may be able to persist in reaching for the toy on his own without the father’s encouragement.
6.1. Regulation of negative affects
Kopp (1989) has further delineated the development of emotion regulation. It involves the use of an action or behavioral scheme, such as vocalizing, self-distractions, manipulating an object, or removing oneself from a situation. These actions help to diminish the individual’s state of arousal that are related to distress. The child gradually learns a variety
of adaptive mechanisms that help organize and monitor the child’s actions and regulate negative emotions. For example, when presented with a challenging situation, a person often uses strategies that worked before. If the strategies are successful, the person is able to inhibit feelings of frustration and anger that would occur otherwise. An adaptable infant may close his eyes and avert his head when having his face washed instead of crying. A toddler may hold his hands together or put them in his pockets when told that he cannot touch a fragile object, thus inhibiting himself in an adaptable way. A child struggling to master a very difficult task may take a break to refresh him or herself mentally and physically, thus avoiding a tantrum.
6.2. Emotion regulation and adaptation
The emotions that an individual experiences while engaged in activity further serve to regulate the individual’s ability to adapt and respond to the situation or activity. Suppose a person experiences interest, pleasure, or mild anxiety while engaged in a task or social interchange. The experience of these emotions will help to support persistence and continual engagement. If, on the other hand, the person experiences intense or negative emotions, such as anger, fear, extreme frustration, or high anxiety, these emotions will interrupt or disturb the individual’s ability to engage further in the task or they may seriously impede the person’s performance.
Another important way that we regulate emotions are in relation to our own internal goals. They help us to evaluate our success in accomplishing our goals and motivate our activity in further pursuit of our goals. Internal goals may be immediate in nature and relate to security and basic homeostasis. For example, a high-risk family may be faced with putting food on the table and finding shelter. Another internal goal may be sharing interactions with others. For example, the young child may bring a toy to his father hoping that he will play a game with him. We also have internal goals for mastery and accomplishment of skill. While learning a new skill, a person may experience frustration and anger. Picture the person learning to play golf who continually misses the ball and hits the ball into the woods and sand traps. On the other hand, a person may feel a positive emotional state while learning a new skill—such as joy and interest—which further motivates engagement in the activity. Take the young child who is learning how to crawl or walk and practices this skill over and over again. But if there is a block or an obstacle in the way that is too difficult to overcome, such as a gate blocking entry to the stairs, the infant may become distressed and angry. After a while, if the infant cannot overcome the obstacle or an adult does not respond to the baby’s expression of distress, the infant may feel defeated, sad, and eventually withdraw from the situation.
6.3. The role of arousal in the socialization of emotions
The infant’s first goal is to learn to tolerate the intensity of arousal and to regulate his internal states so that they can maintain the interaction while gaining pleasure from
it (
Sroufe, 1979). This has been described as “affective tolerance,” that is, the ability to maintain an optimal level of internal arousal while remaining engaged in the stimulation (
Fogel, 1982;
Fogel & Garvey, 2007). The parent acts to help regulate this arousal, then works to facilitate the infant’s responses once the infant can regulate himself. If the infant does not develop affective tolerance, withdrawal from arousing stimuli may lead to a pattern of disengagement with resulting insecurity in attachments.
Brazelton, Koslowski, and Main (1974) have observed how the mother attempts to adjust her behavior to be timed with the infant’s natural cycles. For example, mothers generally reduce their facial expressiveness when the infant gazes away, but will maintain their expressiveness when the infant looks at them (
Kaye & Fogel, 1980).
Field (1977,
1980) has proposed an “optimal stimulation” model of affect and interaction. If the mother provides too much or too little stimulation, the infant withdraws from the interaction. The optimal level varies considerably from one infant to the next and depends upon the infant’s threshold for arousal, tolerance for stimulation, and ability to self-control arousal. If the mother maintains the infant at an optimal level, an interchange of smiling and gazing occurs. An increase in the infant’s attentiveness may relate to the mother becoming less active and more attentive to the infant’s gaze or when the mother engages in imitations of her infant’s behaviors. When the mother becomes more active, the infant tends to be less attentive. Adults also seek to modulate their arousal during interactions in similar ways. For example, two friends talking in a highly stimulating environment, such as a crowded shopping mall may look away intermittently from the person speaking.
6.4. Mood regulation
What is the difference between emotions, feelings, and moods? Emotions are brief in duration—most last only a few seconds. Most facial expressions are also brief except when they are very intense (e.g., crying, laughing hysterically). The autonomic nervous system changes that occur during an emotion may last longer than the emotional expression but do not persist for more than a few minutes. For example, when a person becomes very angry, they may feel “angry” after they have expressed their anger. The visceral responses associated with anger usually last longer than the actual expression of the emotion. The longer an emotion is experienced, the stronger the person reports the feeling of a particular emotion. When angry feelings last for a duration of time, perhaps an hour or more, then it becomes a mood. In emotional disorders, duration becomes important. In addition, the individual becomes prone to being flooded by a particular emotion—depression, anger, anxiety. Flooding is the phenomenon when almost any event will elicit the emotion. Sometimes the emotion will reappear without any particular stimulus. When this happens, the emotion is intense and interferes with everyday functioning (e.g., sleep patterns, eating, work tasks, social interactions). The person will also have difficulty dampening the emotion and shifting to more positive, productive emotions.
Moods do not have a facial expression. For example, a person who is feeling irritable may become angry very easily and stay angry longer than a person who is not irritable. The irritable mood though does not have a distinct facial signal. When a person has a predominant mood, such as feeling depressed, they will typically show a high frequency of sad expressions (
Ekman, 1984).
Moods may be produced in different ways. Changes in biochemical balances, such as diet, disease, fatigue, exertion, or a stimulating sensory experience can produce different mood states. For example, if a person is tired, they may be more irritable. Or a child who rides on a series of carnival rides may become very hyperexcitable and happy. If a particular emotion is elicited repeatedly over the course of a short period of time, it may produce a biochemical change that causes a mood state to prevail. If a person has experienced a series of maladies in a row, they may become angry and irritable over time.
The feelings that are associated with emotions may be anticipatory in nature, such as anticipation of an exciting event (i.e., opening a birthday present). It may also be anticipatory dread or fear (i.e., presenting a speech in front of a large audience or an upcoming piano lesson after not practicing for a few weeks). Feelings also occur while an emotion is being expressed. Oftentimes, we hear people express these verbally while engaged in an activity. For example, we hear children exclaim, “This is fun!” Feelings may be elicited by memories of the event. Certain words, smells, or places often evoke strong feelings of past events. Sometimes children reared in institutional settings, such as an orphanage in Russia remember things from their very early childhood based on certain sensations or smells. For example, 5-year-old Katarina cried and stated, “You’re not going to tie my hands down, are you?” when her parents went to a hotel and showed her a spring mattress that she would be sleeping in. Evidently the spring mattress must have reminded her of her early days in the orphanage when she was restrained in bed.
7. A developmental–structuralist approach to organizing sensory and affective experiences
In this next section, the developmental–structuralist approach is presented. This approach incorporates the organizational tasks and adaptive and maladaptive infant and caregiver patterns observed in the first few years of life (
Greenspan, 1979,
1989,
1992;
Greenspan & Lourie, 1981;
Greenspan, Wieder, & Simons, 1998). It emphasizes the link between sensory and affective-thematic experiences which help the child to organize and regulate emotional processes.
In this model, there are three essential levels of emotional development. In the first level, the child learns to become socially engaged, but in doing so must learn how to self-regulate by developing homeostasis and forming an attachment to the primary caregivers. The next level is one in which the child develops intentional organized behaviors. The important milestones of this level include development of flexible reciprocal interactions, purposeful communication, an understanding of causal relationships, and development of self-initiated organized behaviors. The last level involves representational capacity, its elaboration and differentiation. In this level, the child shifts from organizing concrete behavioral patterns to symbolic representations of events, objects, and persons. The child begins to learn how to label feelings and emotions and elaborate upon them, and expressing emotions related to themes, such as dependency, pleasure, assertion and autonomy, anger and control, empathy and love. These three levels of psychosocial development are described in this next section.
7.1. Level of engagement: homeostasis and attachment
The infant’s first task is to take interest in the world and regulate himself in terms of states of arousal and feeding and sleep cycles. Self-regulatory mechanisms are complex and develop as a result of physiological maturation, caregiver responsivity, and the infant’s adaptation to environmental demands. In the early stages of development, the caregiver soothes the young infant when distressed and facilitates state organization. Early sensory experiences are important in helping the infant to differentiate pleasant and unpleasant experiences. For instance, being fed and cuddled is usually a comforting experience whereas wearing a wet diaper is not.
The capacity for engagement and attachment has to do with both physical capacities of the infant, such as the ability to modulate and process sensory experiences (including visual, auditory, tactile, olfactory, vestibular, proprioceptive), and the ability to coordinate simple motor actions, such as reaching for the caregiver’s face. The infant learns to engage in mutually satisfying experiences with the affective world. For example, the parent may play reciprocal cooing games with his or her baby. As the infant learns to regulate states of arousal, he can focus attention to take interest in the world while also adapting to a variety of sensory stimulations experienced in everyday life (i.e., being held and carried, fed, or bathed). As the caregiver provides soothing and organizing sensory and affective experiences for the baby, the infant forms a special emotional interest with the caregiver.
Problems at this early stage can have wide-reaching implications life-long. For instance, Sylvia was distraught when a favorite aunt offered her 7-year-old child a birthday present, something that delighted her daughter but upset Sylvia very much. She couldn’t seem to explain her emotional reaction, but she felt furious at the aunt for giving a gift to her daughter with such warmth and caring. Sylvia had suffered from emotional deprivation growing up and never experienced being given to and nurtured in pleasurable ways. On a cognitive level, she knew that she should be happy that her daughter was receiving something she didn’t get as a child, but on a visceral level, it made her feel neglected.
7.2. Level of intentional, interactive, organized behavior, and affects
This level spanning from 8 months through 18 months includes the stages of somatopsychological differentiation (intentional communication) and behavioral organization. This level lays the foundation for formation of a complex sense of self. The baby becomes increasingly more purposeful and organized in interactions with the object and person world. The child begins to attach emotional meanings to different sensory, interactive, play, and caretaking experiences. For example, the 8-month-old may reach out to be picked up, then smiles when his wishes are met. By 18 months, the toddler begins to understand that their mother or father are sometimes loving and nurturing, sometimes firm or even angry, and other times playful. The child still relies on concrete experiences and is oriented on here and now experiences because he has not yet developed the capacity to represent his thinking, emotions, and behavioral experiences.
An important hallmark of this stage is the development of intentional organized communication to human interactions. We observe the child engaging in interactive signaling with others through gestures, words, and actions. For example, a 9-month-old often enjoys the game of tossing his cup and plate onto the floor while sitting in the high chair. At first it may become a playful game, the infant gesturing toward his cup on the floor and smiling as his father returns it to his tray. But if the dad tires of the game and ignores baby’s wishes to continue the game, the baby begins to clench his fists and look angry, even banging on the lap tray to show his anger. Through these interactive exchanges, the baby begins to organize and communicate emotions, such as assertiveness, curiosity, anger, dependency, and pleasure. By 15–18 months, interactive signaling becomes more organized. The toddler can communicate not only in proximal space, but also in distal space. The toddler may toddle across the room to knock down a large block tower, then look over to see if his mother noticed him. If the mother smiles admiringly and tells him, “What a big boy!” the toddler interprets her words and gestures as encouraging. This distal connection with the mother, also known as social referencing, enables the toddler to continue playing from across the room without having to go back to sit on mom’s lap. He can feel her reassuring presence through her approving nods. He can gesture to her about feelings of frustration or anger when he can’t successfully build the block tower, such as throwing the block and scowling.
During the level of intentional organized patterns, the toddler learns to use complex preverbal gesturing and sounds to engage with his world in a new way. Communications become reciprocal in nature and the toddler learns that he can give and receive information from others through different channels (e.g., gestures and words, as well as sensory and motor experiences, such as rough housing with father). The toddler communicates emotional meanings through these channels. For example, he may challenge the limits of safety by testing whether he can touch an electrical outlet at home or unbuckle his seat belt while riding in the car. He may look for reassurance and acceptance by putting away her book on the shelf. Many of the important life messages are learned during this stage including love and approval versus hate and rejection, safety versus danger, and a respect and empathy for self and others versus impersonal detachment.
Many children with mood dysregulation including those with autism spectrum disorders, ADHD, or those who have suffered abuse, neglect, or trauma often do not develop the capacity for interactive signaling, reciprocity, and the ability to integrate thoughts and feelings for adaptive social behavior. They may lack a sense of self and be unable to differentiate the range of emotions, such as assertion and needs for dependency, self limit setting, or empathy.
7.3. Level of representational elaboration and differentiation
During the representational stage occurring between 18 and 30 months of age, the child creates mental images from actions, events, and sensorimotor experiences and internally manipulates them through thoughts, communication, and new actions. The child begins to represent ideas through pretend play and articulation of abstract ideas. The emotional meanings of life that were previously explored through two-way communication now become symbolized. The child can explore the meanings of different emotional experiences including dependency, pleasure, assertiveness, anger, and self limit setting. The child is now able to attribute affective meanings to objects, people, and events. For example, the child learns that weekday mornings have a different pace to them because mom and dad are bustling about. He may resist getting dressed to avoid having to go to the babysitter’s but on the weekend, he quickly helps his dad get him dressed to go to the park. The child begins to express complex emotions, such as empathy and an internalization of love for self and others. These emotions become stable and survive emotionally upsetting experiences, such as separations and tantrums. Later on, the child develops the ability to experience loss, sadness, and guilt.
During this stage, the child attaches meaning to concrete events. For example, the toddler can label pictures (e.g., “D.W. is happy. She found the ring.”) and describe objects in affective terms (e.g., the scary monster, the favorite stuffed animal). He can also describe his own feeling states (e.g., “I want that,” “my turn”). As the child moves into pretend play, he or she can enact simple to complex dramas that reflect everyday sequences and their meanings to the child, such as feeding the dolls, going to the store, then coming home to sleep. Older children do the same thing through story telling, poetry, or art.
As emotions become differentiated and the child has a stronger sense of himself and others, experience becomes categorized into functionally relevant patterns. As the child can communicate through words and pretend play, wishes and emotions are expressed. The child can shift between fantasy and reality in play (“that’s pretend, isn’t it?”). He also learns to understand his impact on others (i.e., saying sorry when he spills his juice on another child).
8. Application of developmental–structuralist model
This last section focuses on the functional application of the material presented in this chapter. In the first part, different emotional problems of children are discussed from the point of view of the three levels of somatic-affective experience described by Greenspan. A case example is used to depict problems that may occur at each level and how the clinic could intervene. Following this, concrete suggestions are provided for working with different problems related to mood regulation and irritability. Three case examples are provided that integrate the components of the model spanning from infancy through early adolescence.
Dr. Greenspan’s seminal work in the field of ego psychology has provided mental health and early intervention professionals, as well as families with children with special needs an important way of conceptualizing the child’s emotional and developmental needs and how to translate this into treatment. For example, is the person engaged or not engaged, in what situations do these occur and how do they engage or disengage? How does the person communicate—through gestures, affective expressions, and words? Does the person organize affective experience symbolically? By observing individuals along dimensions of engagement, intentional behavioral patterns, and representational elaboration, the clinician can conceptualize how to address the person’s difficulties. For example, if the child has a fundamental deficit in the capacity for engagement or gestural communication, one may concentrate on these more basic areas. If the child has the capacity for representational thinking, one would work on building a foundation for interactions while also fostering the child’s symbolic capacities.
8.1. Level of homeostasis and engagement
Infants who are unable to process sensory experience in a normal fashion cannot utilize the range of sensory experiences available to them for learning. These infants oftentimes have maladaptive responses in forming affective relationships. For instance, an infant who is hypersensitive to touch, sound, and movement may avoid tactile contact, being held and moved, and may avert his gaze to avoid face-to-face interactions.
The ability to engage can be compromised by several things. There may be difficulties in sensory modulation or processing, such as the baby who is sensitive to touch or high-pitched sounds and who avoids or withdraws from the human world. Difficulties with muscle tone or coordination can affect the infant’s ability to signal interest in the world. For example, the young infant who arches away from the mother’s breast during feeding due to oral hypersensitivities or an imbalance in muscle tone will affect the level of engagement that occurs during feeding. These problems in the infant will affect the caregiver’s ability to respond, particularly when they do not understand what the baby’s responses mean. The mother whose baby arches away when he is held may feel that she is being rejected or that she is not a good mother, particularly if the baby’s tactile hypersensitivities or increased muscle tone are not understood.
Even when the infant is competent from a sensorimotor standpoint, a caregiver might fail to draw a baby into a relationship (e.g., a caregiver who is depressed or who is self-absorbed may not woo their new infant). This can have lifelong implications for the person. For example, Carol’s mother was an alcoholic who was more concerned about her own social life than raising her three children. The father traveled and was rarely home. Carol’s mother frequently abandoned the children to go out to parties and left the house in chaos with no food for the children to eat. As Carol grew up, she observed the horrible disrepair of the household, the stark neglect from her mother, and felt that she was worthless, undeserving, and unlovable. When Carol became a mother, she was constantly getting into battles with her husband, children, and family members, not knowing how to be in a mutually rewarding and reciprocal relationship. She struggled with how to provide a nurturing and stable home environment for her own children which was the focus of our work together.
Physical traits, temperament, ability to self-regulate, sensorimotor capacities, and interactive capacities can have a significant role in the baby’s capacity for engagement. Variations in the capacity for engagement are often a central aspect that underlies different types of psychopathology in later childhood and adulthood. Difficulties that are encountered at the level of engagement, may be evidenced by a lack of relatedness to the human world. For example, the child may appear aloof or distant, “beating to their own drummer” as Greenspan describes, or they may be autistic-like. One can observe the quality of engagement in terms of its stability and how well it is maintained when challenged by stress or demands. For example, a child may remain engaged in play as long as it is the child’s agenda, but as soon as the adult requires the child to follow a routine, make a transition, or adhere to any other demand, such as cleaning up, the child may become disengaged. For some individuals, the stress that causes them to disengage may be certain types of sensory stimulation (e.g., loud noises, someone touching them in an effort to be close). The qualities of the engagement may also vary depending upon the challenges that confront the child. For example, the child may appear mechanical in their interactions, emotionally labile, or very demanding of attention from others.
8.2. Level of intentional, interactive, organized behavior, and affects
A child with difficulty at this level will have disorganization with gestural signals and intentional behaviors. The child may interact but not purposefully. For example, play may be stereotypic, perseverative, or appear unfocused or aimless in quality. The child may not respond to the caregivers’ signals, ignoring or misreading communications from others. Temper tantrums or withdrawal from interaction may occur if the caregiver does not respond to the child’s signals.
8.3. Level of representational elaboration and differentiation
Disorders in this phase include children who remain concrete and have difficulty using representational thinking. Impulsive or withdrawn behavior often accompany such a limitation. The child’s relationship patterns may be fragmented or there may be an overdependence, clinginess, and inability to separate from the caregiver. The child may also show little range of affective elaboration. For example, play may focus exclusively around aggression and the child may appear solemn, stubborn, or angry. Some children may be highly impulsive with acting out behaviors as observed in conduct disorders. The following section presents a case example of a child with difficulties in the various emotional stages described earlier.
9. Case example of a child with difficulties in various emotional stages
Philip was a very verbal and imaginative 6-year-old child. He was charismatic and liked dramatic play, sometimes dressing up in hats to be policeman, fireman, or superman. Philip had difficulties with social skills. He played well with peers as long as the play went his way, but when it didn’t, he would bully the other children and say, “Nobody can touch any of these toys!” He often misconstrued social signals (e.g., confusing accidental and purposeful touching) and would become aggressive with other children. He was anxious about making friends, yet he could be outgoing, introducing himself to others in a friendly way.
Philip was a hypersensitive child. If he got hurt, he overreacted strongly, screaming at his parents not to touch him. He showed signs of tactile defensiveness, such as hating haircuts, avoiding new food textures, and preferring long sleeved garments and pants even in warm weather. When in a group of children, Philip tended to withdraw. He was sensitive to loud noises and seemed to have difficulty focusing at school, going from one thing to the next. When not engaged in an activity, he often zoned out watching TV. There were subtle indicators of motor planning problems. For instance, Philip was fearful of riding a bicycle. He did not like unexpected movement, was frightened of falling, and disliked trying new movement activities.
Philip had many problems related to self-calming and mood control. Up until he was 4 years old, he seemed to be a fairly easy child. He never went through the terrible twos, but became fussy and irritable at 4 years of age. The event that seemed to stand out in his parents’ mind was when they removed his pacifier. At the time, Philip was only using the pacifier at night to fall asleep. He picked a day shortly after his fourth birthday and gave his “binkies” to his mother for a “binky funeral.” Although he seemed ready to do this, he viewed the event as traumatic. The next day after they threw the binkies out in the trash, and watched the trash truck drive away, Philip went up to his teacher and told her, “There’s nothing bad going on, but there are no binkies in my house.” Shortly after this, Philip did not want to go outside and seemed depressed, expressing worries about safety. Since then he had difficulty controlling his mood and became easily angry. He would often lash out verbally toward his parents, calling them names or being bossy. He wanted to be in control and to be the center of attention. He balked at complying with requests and had trouble waiting his turn both at home and school. Generally his tantrums ranged from brief to lasting for an hour. At school he had difficulty complying with the teacher’s requests and would tell the teacher that he was the boss. Sometimes he would hit the teachers or do things like tear paper, throw sand, or break toys.
When I met Philip, I noticed that he rarely looked at me or his parents, even when he was talking with us. He glanced at me briefly, but only when he was across the room rather than at close range. I speculated that Philip might be overwhelmed by affective cues from others, that he had difficulty reading facial cues, or that he had difficulty coordinating looking at objects and a person while interacting at the same time. The treatment focused on activities where Philip and his parents communicated with one another from across the room with things like walkie talkies or long tubes that they could look through. His love for dressing up and constructing buildings around himself is an example of how he did better when he could create a physical distance between persons. Eventually a goal would be to help Philip tolerate closer proximity with others while remaining engaged.
Philip seemed to have a high need to discharge energy through physical play and to create excitement, yet at the same time, he seemed to become overwhelmed with stimulation and needed to quieten himself, retreating to enclosed spaces (e.g., going inside a small playhouse in a busy waiting room). He loved playing with stimulating toys like pushing over an inflatable Bop man or flying and crashing airplanes in the air. He liked varying these activities, watching the airplanes do flips or watching them travel to different planets. He also enjoyed aggressive play that involved superheros attacking the bad guys. Despite these needs to discharge aggressive energy, Philip liked retreating to enclosed spaces. He liked to go inside my pup tent which had pillows and a soft bin filled with plastic balls inside it. He crawled inside the ball bin and wished to be zipped up inside it. While inside he wanted to play that he was a baby, asking me to be his mommy. His need for self-soothing was demonstrated by his wish to pretend to drink from a bottle, then be put to sleep. It seemed that Philip operated at two ends of the continuum—showing a high need to discharge intensity while also needing to retreat when he became overwhelmed with stimulation or the demands of the situation; however, he was able to express his needs well, seeking out self-soothing or making play choices to discharge tension that he experienced (e.g., through aggressive play). Philip is an excellent example of how one might work on self-soothing and the need to discharge aggressive impulses through a combination of representational play and sensorimotor experiences. Giving up the pacifier was a traumatic event in his life; however, the fact that he did not learn how to assert himself until later in life suggests that he had not negotiated the earlier stages of homeostasis, assertion, and autonomy.
Philip showed a good capacity to construct pretend play patterns of several ideas, although he didn’t show this capacity until after he discharged physical energy in play, such as that with the airplanes. He was able to link ideas into a logical sequence but he could not always explain what was happening as he enacted things with objects, thus showing inconsistent consolidation of the stage of combining representational ideas with emotional thinking. He was only sometimes able to elaborate verbally on his play ideas when asked questions related to causality (i.e., “why,” “what,” or “how” questions), but this occurred whenever he became more organized in his play. Philip showed a vivid imagination and created many different scenarios in his play, calling upon his imaginary friend “Wishing Well Willie” to watch us and give us advise as we played. It appeared that Philip had some good play capacities but needed facilitation from an adult to obtain his best performance. At other times, he seemed to become self-absorbed and needed to be drawn back to remain interactive. His parents were very sensitive in facilitating his play, yet were able to back off when Philip showed needs to self-soothe or withdraw.
Philip seemed to have a high need to control situations, in part because of problems tolerating unpredictable events that might occur. He could express his needs for assertiveness and aggression through play, but also showed a high need for calming and containment. Although he had some good play capacities—connecting two or more ideas in a logical sequence and could use language to describe causality (why, what, where questions), he could only do these skills with adult facilitation and after he had had the opportunity to organize himself through high-intensity physical play. It appeared that Philip had some difficulty expressing feelings and thinking through problems and how they are solved.
Mr. and Mrs. T. received parent counseling to help them in managing Philip’s aggression, his problems around self-calming, and noncompliance. Emphasis was placed on helping Philip to read social cues, to problem solve in social situations, and to anticipate and predict his tantrums. A plan for managing aggressive behavior was enforced that used ignoring for name calling, time outs for tantrums, while reinforcing positive behaviors, such as complying with demands or “playing friendly” with others. We discussed better ways to self-soothe than to control the situation with his mood (e.g., going inside a pup tent filled with pillows and listening to music; building forts to go inside). He also needed to develop more flexible ways of responding to others’ requests and to respond to less predictable situations. We used pictures of upcoming events, checklists with pictures of sequences he had to do, such as getting dressed and riding in the car to school. The parents were successful in helping Philip to read facial cues and to sustain eye contact in games like charades.
Philip received developmentally based individual psychotherapy to develop his capacities to problem solve, to control his impulses, to cope with anxiety and stress, to develop the ability to comply with situational demands, to read and respond to social cues, to predict mood changes, and to signal others and himself when he was becoming disorganized. He also needed to develop a better sense of competency in his ability to control himself and to self-organize in a range of situations. A combination of cognitive-behavioral, and play therapy was useful for Philip in resolving these issues. Due to his high need for tactile-proprioceptive input, objects selected for play therapy incorporated this sensory component to provide him with better physical organization.
Philip also received short-term occupational therapy to address his tactile hypersensitivities. A sensory integrative therapy approach helped him with some of the constitutional issues that seemed to underlie some of his mood and behavioral problems. Activities focusing on proprioceptive input helped to diminish his need for aggression and withdrawal in social situations.
10. Identifying causes of mood dysregulation
There are many causes of mood dysregulation. It is important to determine which problems might underlie the disorder. A list of potential causes is given as follows. A checklist appears at the end of this chapter to help identify specific aspects of the child’s irritable and angry moods.
1. Medical problems: Common medical problems that might induce high irritability are thyroid disease or other medical illnesses causing chronic pain. Certain medications can cause irritability as a side effect. Allergies to milk and gluten products agitate the nervous system. Chronic insomnia or other sleep disturbances may be the culprit.
2. Constitutional problems: Sensory hypersensitivities are often associated with high irritability. A child may have aversions to being touched by others, even when the tactile input is not construed as irritating by most persons. Janice was constantly agitated when tapped or touched by persons in her family or friends. She had a history of abuse that seemed to compound the problem, therefore, it was difficult to distinguish how much of her problem was emotional or sensory.
Auditory hypersensitivities can cause chronic irritability. A child who lives in a noisy household with kids making loud noises in play, vacuums running, or other irritating machine noises can be constantly on edge. The child may not be able to function in everyday life unless he minimizes loud noises by wearing noise-cancelling headphones or by going to wooded parks to avoid the cacophony of life.
Visual hypersensitivities are common, especially in individuals with attention deficit disorder. Rose would become agitated with too much visual clutter, but created her own visual clutter by not cleaning up as she did projects, or leaving things out and not cleaning up as she did the activity. She felt overwhelmed by stacks of clothes and objects lying about her bedroom and felt that there were never ending homework and chores awaiting her attention. Her state of overwhelm quickly translated to an irritable state.
Another source of high irritability is the loading effect of too much sensory stimulation. This can be in any of the sensory channels—movement, touch, sound, sights, or smells. Rachel was a college student with bipolar illness who found that she had to limit her exposure to too many activities or places in a given day, otherwise she went into a state of complete shutdown. She had to live alone in a dorm room because of her inability to tolerate too much stimulation. If forced to continue her day through multiple activities, she sometimes became so anxious and distraught that she could only manage if she took antianxiety medication.
In addition to sensory dysregulation, the person may be temperamentally wired to be fussy, irritable, and intense. Harrison was, such as person. His parents joked about how he was the hard one in the family to raise. But as he grew older, his irritable nature continued. He could be pleasant for short periods of time when social convention required it, but at home, he was tense and agitated with the slightest thing. His requests were unreasonable and he was unable to adapt to any change in his life, insisting things had to be his way or the highway.
3. Environmental or life stressors: There are many individuals who are irritable for a period in their life because of environmental or situational stress. Worries about having enough food or money, being subjected to grossly unfair situations, failing a grade in school, doing boring or hateful tasks, or being forced to live in a less than acceptable living surrounding are some examples. Once the bad circumstance improves, the child usually resets their mood to a better place, but it may take at least 6–12 months to recover from these kinds of stressors.
Time pressures are a very common source of irritability for many children. Having too much work to do in too little time, having no chance to restore oneself with breaks or soothing activities, and feeling overwhelmed by too many demands on one’s time can create irritability. Internet stress is often reported when the person feels that they have to answer and respond immediately to texts, emails, or research things online. This is an extra demand on time for many teenagers. Once the person creates time in their life for a more balanced schedule without the need to hurry through tasks and space to breathe, the irritability usually abates.
Trauma can be a cause of irritability. A child who has been bullied, teased, or has been chronically abused physically, sexually, or emotionally will not only become irritable, but depressed. The constant hypervigilance induced by the trauma results in a flight or fight state of arousal which places the individual in chronic irritability and agitation.
4. Family stressors: There are numerous family stressors that can induce irritability in a person. Living with a person who has highly irritating habits can be extremely difficult. For example, Maria’s mother had severe obsessive–compulsive disorder and was constantly checking Maria to see if she was clean enough. Another common family stressor is when a couple divorces or separates or when the couple adopts a child, has unplanned pregnancies, or the couple blends step-children into their existing family. This had a profound effect on Rebecca whose parents adopted a child when she was 10 years old. The adopted child was violent and kicked and beat both Rebecca and her parents, inducing a state of trauma for the entire family.
5. Accommodations in emotional development: It is important to ascertain whether a person’s irritability relates to mood dysregulation associated with attention deficit disorder with hyperactivity, bipolar disorder, depression, anxiety, and/or trauma. It is helpful to use the model discussed in this chapter to identify which levels of emotional development are compromised and why.
At the level of homeostasis and engagement, a person may be easily overwhelmed by the affect of others and misinterpret and be irritated by others’ vocal and gestural cues. For example, Tim lived with his father and younger brother and found their way of interacting to be gruff, loud, and overwhelming. Tim felt that both his father and brother were always angry at him, when in fact, they were astonished to find out that was how Tim felt. Tim’s father and brother were large men with deep voices who could be rather imposing to others, especially to Tim who was the smallest and still in middle school.
At the engagement level, a person may not have had rewarding early attachments in their life. Denise felt that her own parents were very formal and never expressed affection toward her. As she grew older she felt that she was unlovable and not deserving of others’ affections or attention. This dynamic coupled with the fact that Denise experienced tactile defensiveness gave her ample reason to shrink from any form of tactile contact. She developed a hands-off interactive style and avoided any physical activity that might bring her into close proximity to peers (i.e., sports). Others often found her stiff body posture and withdrawal pattern off-putting which resulted in Denise adopting a more isolated social profile. As she entered the teen years, Denise became a loner, eating lunch by herself in the counselor’s office, and relating best to animals over people.
A person who lacks the capacity to self-soothe will be at sea in knowing how to regulate his own distress. They may be overly reliant on others to soothe them, or once angry and distraught, they become incapacitated by their own distress, remaining so for many days after an event. Louise reported that she felt like a black cloud followed her around when she went into her foul moods and nothing could break the cycle. Louise would obsess about what others had done to make her feel this way, never seeing how her own mood had contributed to her state of mind. She couldn’t let go of this thought, blaming others, especially her parents, mercilessly. She took things out on her parents, banging on their bedroom door when they wouldn’t sit with her to help her feel better. She wanted them to comfort her constantly to the point that they could never get space from her. It led to a bad cycle whereby Louise felt abandoned and unloved by her parents, unable to comfort herself, and stuck in a bad mood with no solution.
If a person never develops emotionally during the stages of assertion and autonomy, they are apt to have difficulty knowing how to assert themselves properly, knowing how to self-control their impulses, or they may end up being highly controlling of others. Jack was such a person. As a growing boy, he lived alone with his father after his parents separated when he was 10 years old. His father had obsessive–compulsive disorder and bipolar illness which caused him to be extremely controlling of Jack. He grew up as a good boy who never rocked the boat to avoid any conflicts with his volatile father. When his father was hospitalized, Jack needed to be cared for by his estranged mother. He suddenly changed from being docile to extremely angry all the time. He started to boss his mother and sisters around and constantly yelled that everything they did was all wrong.
11. Treatment approaches
There are a number of excellent resource books that are available which provide guidelines for parents and professionals in managing infants and children with irritability and mood regulation problems. These are provided under “Suggested Readings” at the end of this chapter. The reader is referred to the books on this list for specific guidelines around behavioral management techniques which are not addressed in this chapter.
Before embarking on a treatment program to address the child’s irritability, a complete history of when and where crying and irritability occur and for how long is useful in determining the causes of the behavior. In some cases, a crying infant or irritable child may be responding to tensions in the parent who may respond to the child by handling the baby briskly or in ways that are not conducive to calming. In addition, excessive crying may be related to emotional issues, such as separation anxiety, and for some children, it may occur whenever changes are introduced in the everyday routine or activity. Once it is more apparent what might be underlying the child’s irritability, a treatment plan can be introduced.
An important aspect in treating the child is to develop a consistent plan in approaching different behaviors. The treatment plan should include helping the child learn to self-calm, to solve problems, and tolerate distress and frustration. At the same time, the parents need help in understanding the child’s distress and their own feelings while at the same time, learning how to set limits and redirect the child to purposeful activity. A number of guidelines that can be used in treating the child with irritability are given as follows.
11.1. Rule out medical problems
When an infant or child is inconsolable, it is important to determine if the child has medical problems that may be the primary reason for the crying (e.g., colic, chronic ear infections, reflux, severe allergies, urinary tract infections). Milk intolerance or a diet heavy in gluten can sometimes contribute to irritability (
Rapp, 1991). A referral to a nutritionist is often helpful in managing diet.
Eating healthy at regular times (e.g., 3 meals per day plus two snacks for young children) and avoiding a diet high in carbs, sugar, and fried food is highly beneficial to the child’s physical health. In addition, getting a good night’s sleep and keeping a regular sleep schedule is very important. Without these basics in place, the child is apt to be irritable.
11.2. Address sensory hypersensitivities that may contribute to irritability
Inconsolability may be related to hypersensitivities that the child has to environmental stimulation or constitutional problems in the child that causes them to be highly reactive to touch, movement, sights, or sounds. The child’s sensory hypersensitivities should be addressed through particular activities or techniques described in
Chapter 9 and in the
Skill Sheet #2: Activities for problems of touch. Whenever possible, it is very helpful to integrate these activities into play, preferably in the context of the parent–child relationship. Activities that provide deep pressure or proprioception are useful (e.g., sitting in beanbag chair with weighted blanket on lap; rolling up like a “hot dog” in heavy comforter). If the child is hypersensitive to sounds, the child should be encouraged to engage in activities that allow the child to make their own sounds (e.g., drumming objects on different surfaces to see what sound they make). In addition, vestibular responses should be normalized by providing linear movement activities (e.g., forward–back rocking).
11.3. Avoid overstimulating the child
A common problem confronting the parent who is trying to console a crying infant is a tendency to become frantic when consistent efforts do not seem to work. One may observe the mother rocking vigorously forward and back for a short period of time, then shifting to swinging the baby in the air when crying resumes. It is important in the therapy to console the parent and to help them to avoid overstimulating their child. It may be helpful for the therapist to model how to calm the child by trying certain techniques with the parent, then talking them through how to do it with their child. For example, if it appeared that a pillow hug (e.g., taking pillow, holding it against child’s back, then squeezing it firmly) was a strategy that might help, the therapist might first do it with the caregiver, then teach them to do it with their child. It is also important to help the parents to remain calm while trying to console their crying infant and to try a technique long enough to evaluate its effectiveness. Sometimes the caregiver’s tolerance for their child’s fussiness is very low. These parents try many different techniques for a brief period of time, then feel that “nothing works.”
It is important in the therapy to find ways to decrease stimulation at home and school environments, as well as streamlining the number of activities that the child is doing. The mantra is “less is better” and “one thing at a time.” It is very useful to eliminate or scale back on activities that create a state of urgency or rushing around. The therapist should model calmness and practice meditation and relaxation techniques with the child in session (see Skill Sheet #7: Mindfulness: stilling the mind). In addition, the child should find healthy escapes or self-distractions that give them an opportunity to leave a situation that is overwhelming or overstimulating. This is often an educational accommodation for school-aged children when they are issued a pass to take a short break in a quiet room to regroup, practice deep breathing, and calming their mind.
11.4. Soothe both parent and child
It is often necessary to find ways to soothe both parent and child. This may be done by having materials in the environment that provide containment, holding, and soothing. For example, both parent and child can have a calming experience if both of them are made to sit inside a large inner tube or a pup tent filled with soft pillows while engaged in interaction together. By using these types of techniques, the therapist is providing both physical and emotional holding to both parent and child.
11.5. Create opportunities for the child to learn how to self-calm
Parents of very young infants should be encouraged to calm their crying baby, but once a baby reaches 6–9 months, the infant should be given the opportunity to self-calm and to learn to solve problems that are sources of frustration through support and encouragement from the parents. When crying persists beyond 5 or 10 minutes even after the parents have encouraged the infant to self-calm (i.e., presenting the baby’s pacifier or a favorite toy), the parents should seek to calm their baby by holding and rocking or other effective means. For older children, the parents may need to help the child to self-calm at first, then redirect them toward a calming activity that they can do on their own. Over time, the parent may direct them immediately toward the calm-down activity, gradually withdrawing the child’s dependence on the parent as a soothing device.
Many preschool and school-aged children respond well to a calm-down area that both provides containment and offers them activities to regroup. Pup tents or a small designated area of the house may work well for this purpose. For example, the parents may place a table cloth over a card table and fill it with pillows or create a space between the back of the sofa and the wall where the child can retreat when overstimulated. In this space, there should be a box of calm-down materials that help the child (e.g., puzzles, books, squeeze balls, or other calming materials). To install the calm-down area, the parents should practice going there with the child at moments when they are calm or dysregulated. Since many children who are irritable fall apart during transitions, the parents may have several calm-down boxes that can be used for different situations (e.g., a box in the glove compartment of the car for car rides).
An important aspect of parent guidance is to help the parents help the child to develop self-calming. Children who are fussy often depend upon others to calm them rather than calming themselves. Self-calming should be introduced in two ways: through environmental modifications and through objects, interactions, and play that support self-calming. However, it is important to determine the best ways for a given child to soothe himself. For example, some children quieten when looking or listening to something novel. Others respond better when helped to organize their own movements.
Oftentimes the parents need to begin by providing sensory inhibition through firm deep-pressure and linear movement. For instance, bringing the hands to midline, touching the palms to body parts, or helping the child to suck on his own fingers are simple ways to accomplished this. Once an infant develops self-calming behaviors, the infant should be helped to use these on his own rather than constantly being organized and calmed by others. With older children, the child may learn a variety of “heavy work” activities like pushing a chair or heavy box across the room. It is useful to combine a calming activity with one that is purposeful. The child may also respond well to a collection of fidgets in a “sensory box” (i.e., squeeze toys, putty, chewing fidget, and so on).
Finally, the child should learn to find ways to soothe in multiple settings. This may be done by structuring the environment to provide a feeling of containment and enacting soothing activities at certain times of the day (
see Skill Sheet #1: Self soothing). Using the Symptom Checklist from
Chapter 1, one may glean which types of soothing activities are right for the child. For example, the child may self-calm with intense movement, noise reduction, dimming of lights, and firm pressure to the abdomen and hands. The child may take 3–10 minute movement breaks during the school day, doing certain yoga exercises in a dimly lit room with the door closed. While sitting at his desk, he may place a heavy weighted blanket or other weighted toy on his lap and wear noise-cancelling headphones. While listening to the teacher, he might squeeze a stress ball or resistive putty.
11.6. Help the child to learn how to make transitions from one activity to the next
There are a number of tricks in helping children to learn how to make transitions in activities. Making transitions in activities requires the child to shift attention from one activity to the next, to anticipate and plan the next activity, and to make changes in activity, eventually without the help of a parent or teacher. Gaining a sense of autonomy and the capacity to tolerate separations from the parent is important in helping the child in making transitions. Therefore, objects need to be provided that help the child self-organize to transition from one activity to the next, but also represent the connection between parent and child.
The parent may carry a keychain with a picture of them and their child on it or use a blanket, stuffed animal, or other symbol representing the connection between parent and child. When making transitions, the parent can signal the child, “Don’t forget your stuffed animal.” Giving the child advance warning that a transition is about to occur is often helpful. The parent should help the child finish what they were doing, then give them an object to hold that represents the next activity. For example, the parent may say, “We’re leaving for the store. Can you bring along your shopping list too?” and give the child a pad of paper and crayons to scribble on while riding in the car. Some children respond well to photographs or picture cards that show the child doing the next activity. The parents will need to take photos of the child doing different activities, such as riding in the car, swinging on a swing at the park, getting dressed, etc. to implement this method.
11.7. Provide clear limits, rules, and structure
A problem-solving approach is useful in helping parents arrive at strategies for limit setting. When the child challenges the parents with something that he shouldn’t be doing, the parents should say “no” firmly coupled with a gesture. If he still doesn’t stop what he is doing, the child should be removed from the room or the object taken away even if it results in a tantrum. It is useful for both the caregiver and child to acknowledge the child’s anger and frustration. Sometimes a child can be redirected to another activity before the crying escalates too far. If it is at the point that the child is inconsolable, the caregiver should move the child to a time out or calm-down corner, then as soon as the child has calmed, they should be redirected to a positive activity. It is helpful to think about how different situations might play out—a tantrum in a restaurant, when the parents are in a hurry, in a parking lot, etc. and how they would handle a tantrum in public situations. Both caregivers should come up with a consistent way of handling the tantrum and enforce it. If possible, it is a good idea to keep visits short to public places, such as the grocery store, a restaurant, or shopping mall so that the trip ends successfully rather than in a meltdown. When unanticipated tantrums occur, parents should avoid reinforcing the tantrum by buying a toy, or giving the child a bottle or lollipop. It is usually better to remove the child from the situation and as soon as he or she is calm, then offer a calming toy or stuffed animal to hold while telling their child, “I like how you calmed yourself down.”
Parents should pick a few key behaviors that will be the ones they wish to work on with their child. For example, sitting at the table for eating, turning off the TV when it’s time to go to school, and getting dressed for bedtime may be the three targeted behaviors. Although it is difficult to do, other behaviors that don’t fall into the targeted behaviors should be deemphasized. For example, if the child chooses to dress themselves in odd clothing and it is not one of the top three or four target behaviors, the parents should leave it alone, letting the child do it their way. Compliance and good behavior should be reinforced with praise. Some families like using praise coupled with tangible reinforcers, such as stickers, checks on a chart, a cookie, or a visit to the “Mommy Treat Bag” at the end of the day.
Teaching the child how to problem-solve is very useful in helping them to arrive at strategies for limit setting on their own behavior. The first instinct for the irritable child is to explode or react without thinking. There is a detachment between the thinking mind and the emotional mind. What we are seeking is for the two to merge into a wise
mind, as described in dialectical behavioral therapy (
Linehan, 1993). In the small child, he learns how to stop himself and internalize limits from the parent who firmly says “no” coupled with a gesture. Similarly, the child needs to identify what behaviors are not OK to continue doing, to visualize something that denotes a visual gesture to stop (i.e., a stop sign, road block, red light), and perhaps even a tactile cue that signals him (i.e., squeezing arm firmly or a firm touch on the leg coupled with saying “stop” in the mind). If the child can’t stop yelling or whatever negative behavior it is, they need to remove themselves from the situation immediately. It is useful for the child to verbally acknowledge their anger and frustration and seek validation from others. This can be very powerful in quieting the irritability. The child needs to feel that others understand their point of view, even if it is distorted or inappropriate for that situation. For example, the child may say,
“It is really irritating to me every time I eat with you and you eat food loudly and spill food all over the place. If you don’t mind, I will eat in the kitchen so that I don’t upset either you or me. I hope you can understand that this is something that sets me off.” See Skill Sheets #9: Giving and receiving validation; #14: Observing your own limits; and #20: Communicating effectively with others.
The child needs to understand when their behavior is out-of-control and what limits they will need to impose on themselves. It is helpful to think about how different situations might play out—becoming rageful at kids on the playground when they don’t do what you want, when the family is in a hurry, or the child is in the middle of a video game and has to shut it off, etc. and how they will handle their irritability at home and in public situations. The child and suitable family members (i.e., parents, siblings) should come up with a consistent way of handling the irritability and enforce it. For example, if large family gatherings are apt to set the child off, it is a good idea to keep visits short and successful rather than resulting in an angry outburst.
The child should pick a few key behaviors that will work on. List behaviors that are apt to be problematic and prioritize which ones should be tackled first. For example, sitting at the family dinner table and not arguing, turning off the TV to create less stimulation at nighttime, and getting enough sleep and getting up on time to avoid being rushed may be the three targeted behaviors. Although it is difficult to do, other behaviors that don’t fall into the targeted behaviors should be deemphasized at first until the first three are mastered. It often helps motivate the child to have some form of self-reward if they can consistently accomplish these changes over the course of a month. For example, the child may reward themselves with a meal at a nice restaurant, going to a sporting event, or buying some new music (see Skill Sheets #13: Increasing personal effectiveness and #19: Installing structure and organization in your life).
11.8. Help the child become more self-reliant
Many parents complain that their child is constantly whining and demanding their attention. To help build the child’s capacity to organize themselves and decrease reliance on the parent to entertain themselves, the caregiver should try playing with their child for about 10–15 minutes, using the child’s favorite toys. After the child is playing well, the parent should encourage the child to keep playing while they do a small chore or activity in the same room. Every few minutes, the parent should reassure and praise the child, “Good playing alone!” Mom or dad may try to keep the connection between them and their child by singing a song from across the room while they work.
Whenever the parent is involved in a task, such as cooking a meal, it is wise to offer the child some pots and pans, plastic containers, and small objects to use in filling, dumping, stirring, etc. so that the child can play and imitate them while the parent cooks. If the child complains, the parent should try to redirect him physically or verbally. The parent should be clear to their child about when it is time to pick them up and when it isn’t because their hands are tied up. As soon as mom or dad are finished with their chore, they should reward their child by sitting with them to read a story or playing with them briefly to reward their playing alone. For young babies, they may be carried about in a sling or backpack while the parent does household chores so that he or she can see what mom or dad is doing.
With preschool and school-aged children, it is helpful to teach the child to label their emotions and to read bodily signals so that they can implement calm-down strategies on their own. Sometimes children respond to ideas like a traffic light or mood meter. Red colors denote either time to put on the brakes or mad or angry feelings. Green or blue colors may be used for calm and focused states. Other children respond well to thinking about how their engine is running. A good resource book for therapists is the program developed by
Williams and Shellenberger (1994) on “How does your engine run?”
11.9. Develop tolerance for frustration and a sense of mastery
Using child-centered play, parents can work with their child to develop the capacity to tolerate frustration. For example, suppose the child is trying to fit a toy into a container and is getting frustrated. The parent might reflect, “Yes, it doesn’t fit!” rather than immediately help the child to solve the problem. Mom or dad might gently reposition the container for better success, but should avoid taking the object from the child and solving the problem for him. It is a good idea to wait for the child to look to the parent for help. In this way, the child learns to coordinate communication with others when frustrated. The parent may want to first reassure the child, “You can do it, keep trying.” If this is not enough, the parent may help the child to solve the problem through physical or verbal guidance.
Developing a sense of mastery is important for the child who is irritable to feel that they can overcome frustrations and gain pleasure from their own accomplishments. This can be done by giving the child small “jobs,” such as turning the lights on and off when leaving or entering the room, closing the dishwasher, or pushing a drawer shut. If these things are done everyday, it will help the child feel that he contributes to the family and is a big help. The child should also be encouraged to do age-appropriate activities that he can master, such as stirring with a spoon to make pudding, or pull-apart toys like pop beads.
11.10. Help the child tolerate distress, predict precursors of irritability, and self-calm before exploding
A major goal for children suffering from irritability is to predict what sets them off while also learning to solve problems that are sources of frustration. Many individuals with irritability cannot tolerate distress of any kind. It is very helpful for the child to acknowledge that they are in a situation that is annoying to them or that they are already irritable and the slightest irritant will set them off. Several strategies are useful for children. One is for them to think about whether this is a situation that allows for a healthy escape to redirect themselves, leave to stabilize mood, then return to the situation to cope with what lies ahead. Healthy escapes may be to take a short break, get a drink of water, go to the restroom, etc. During this “time off,” the child should engage in deep breathing exercises (see Skill Sheets #5: Distractions for emotion regulation; #7: Mindfulness: Stilling the mind; and #8: Systematic relaxation: stilling the body) while refocusing one’s thoughts in a positive direction (e.g., “I can do this,” “This won’t be so bad.”). If a healthy escape is not possible, deep breathing and positive cognitive reframing in the moment is essential to endure the distress of the situation. One can count breaths while breathing deeply, reach into one’s pocket for a keychain or fidget that soothes their hand, glance out the window at the greenery, or find some other momentary distraction that can help to regroup them. All of these kinds of techniques should be practiced in session with the therapist to help the child access the strategies when needed in everyday life.
Often children who are irritable expect others to fix the situation rather than self-calming themselves and coping with the situation in adaptable ways. Self-calming should be introduced in two ways: through environmental modifications and through objects and interactions that support self-calming. However, it is important to determine the best ways for a given child to soothe himself. For example, some people quieten when looking or listening to something novel (i.e., listening to music or book on tape). Others respond better through the sensory channels of movement or touch (i.e., sitting in a vibrating massage chair or sitting in a rocking chair). Some children organize by doing “heavy work” activities, such as moving furniture or lifting weighted toys. It is useful to combine a calming activity with something purposeful (see Skill Sheet #1: Self-soothing).
In therapy sessions, the child may be directed toward recognizing the physiological underpinnings of their irritability. These precursors might be noticing heart rate and breathing patterns which tend to become rapid and irregular when angry or irritable. The person may experience a jittery, nervous edge in their hands, body, and feet. Other signs may be hypervigilance, inability to sustain eye contact, and projecting a scowl or irritated facial expression. These will impact interactions and cause the child to receive social feedback that they are unpleasant to be around. Once the child is self-aware of these bodily signals, the therapist can guide the child in learning deep breathing exercises, stilling the mind, calming the body, and focusing vision on a steady object or person to change the irritability within the body and mind.
Another powerful technique is for the child to learn how to project a half-smile facial expression. This serves the purpose of changing both internal and external feedback that the person receives. The half-smile provides direct feedback to the limbic system and hypothalamus that a positive emotion is being experienced, even if the presiding emotion is irritability. In essence it tricks the brain and helps redirect the emotional valence of the mind from irritability to a more positive emotion. Not only that, the social feedback that a half-smile generates from others versus a scowl helps the child to receive better social reinforcement
11.11. Help the child set goals, become flexible, and cope with change
Most children who are irritable struggle with change and relinquishing control. One way to begin work on flexibility is to focus on the ability to make transitions in activities. This requires the person to shift attention from one activity to the next, to anticipate and plan for the next activity, and to be flexible with changes that occur as the activity is taking place. Making lists of upcoming activities and checking them off as they occur is organizing and gives the person a sense of control. Setting reasonable goals for oneself is important. Some children derail themselves by setting unrealistic goals, then they become angry and frustrated when they fail. For example, the child may decide to build a toy roller coaster in his basement that is very elaborate and beyond the scope of his skills or the space available. One solution might be to set an amount of time that they can dedicate to a particular activity, stick with that time designation, then mark down where they are in the process for the next time they resume the task.
Being mindful of how one is controlling and rigid in everyday life is helpful, then to think through what changes one needs to make so that they are an easier person to live with. For example, the child may need to do certain chores at specified times and days to contribute to the family life (i.e., walking the dog, empty recycle and trash). If this works for them and their family, there is no need to change. However, they may be rigid about certain rules or activities that negatively affect the whole family. Select one or two that upset others in the family and find a better way to manage it, allowing breathing room for everyone in the family. For example, if the child insists that everyone in the family do certain activities in a specified order and in a certain place in the house, this should be opened up for discussion with some way to allow for change (see Skill Sheets #12: Changing how you think and #15: Taking control of your own behavior).
11.12. Develop tolerance for frustration and installing a positive self-worth
It is important to find ways for the child to develop the capacity to tolerate frustration. It may be useful to list frustrating or distressing events or activities in the child’s life, then beginning with the least frustrating. Practice or discuss the task and identify how to tolerate the distress while solving the problem at hand. When points of frustration are felt, the child should take a deep breath, think through what options are available to him in solving the problem, and visualize breaking through the distress threshold. The child may visualize running through a finish line, jumping over a hurdle, or arriving at a train station. Often the irritable child rushes through tasks when they feel agitated or frustrated rather than slowing down, working carefully, and keeping present in the moment.
It may be helpful for the child to have another person validate their frustration by acknowledging their distress, yet not solving it for them. Getting help at difficult points in the task may be essential for some problem situations. For example, the child may have a physical limitation and cannot write their homework without having mom scribe for them. Positive self-talk is very helpful to persistence. The child should try different mantras, such as “I can do it if I keep trying.” Working for short increments of time (i.e., until a timer goes off) is also helpful in working through the threshold of frustration (see Skill Sheet #6: Positive self-talk).
Developing a sense of mastery is important for the child who is irritable to feel that they can overcome frustrations and gain pleasure from their own accomplishments. Feeling pleasure or excitement will motivate a child’s activity, therefore, it is important to find things that the child wants to learn that can help mediate sustained attention and focus during potentially frustrating activities (see Skill Sheet #11: Creating positive life experiences).
11.13. Overcome feelings of isolation and create positive interactions with others
Individuals who are irritable often feel very isolated because their interactional styles can be so negative and nonreinforcing to school mates, friends, and family members. Often people avoid them or interact with them in hostile, aggressive, and angry patterns. For example, the child may not be invited to social gatherings, or people avoid them at all costs because of their negativity. This not only leads to a profound sense of isolation, but the child often feels unloved by others and unworthy of positive attention. Usually the child has few friends and is viewed negatively by peers.
There are several important strategies to help the child with social interactions. Practicing how to listen to others, to take in others’ point of view without disagreeing, and to wait in conversations rather than interrupting impulsively are important skills. Often the child needs something to do to help them remain patient while listening, especially if they are feeling agitated or flooded with emotions during the interaction. Deep breathing and practicing the half-smile can be very useful to this process. The child may benefit from giving themselves a break before they explode at the other person (e.g., leave the room to step outside and calm oneself). It is also very helpful to keep social interactions short until the child learns how to interact in positive ways without erupting or becoming negative and irritable (see Skill Sheets #10: Finding pleasure and making connections; #16: Keeping track of positive behaviors; and #20: Communicating effectively with others).
Increasing one’s self-awareness that their irritability is contagious and creates a negative interaction cycle with others is a major task for the moody person. They may need to restrict what topics they speak to others about, sticking with noninflammatory topics, funny stories, or playful games. This will require the child to let go of things that they may feel passionate about that agitate themselves and others, for example, some children are fixated on certain topics, such as curse words or provocative subjects that might combust the conversational exchange.
11.14. Develop better problem-solving and coping skills
Many individuals with irritability have very poor problem-solving and coping skills, especially in knowing how to stop themselves from responding rapidly and in thinking through viable alternatives in solving the problem. Many struggle with integrating their perspective about a problem with what other people may consider a good solution. At the heart of good problem solving and coping is the ability to integrate one’s thoughts and feelings, to digest other’s perspectives on the problem, and to generate several good solutions. The child needs to be able to clearly describe the problem in his mind, to express feelings about the problem situation so that others can understand them, to assert what they want and need for a good problem resolution, and to think through what others will gain if they see the problem their way. It requires negotiation skills and practice (see Skill Sheet #12: Changing how you think).
Skill sheets are provided, in the appendix, that may be used in treatment to help the child with self-soothing, self-distractions, validation, problem solving, and stilling the mind and body.
11.15. Support the parents in feelings of isolation and provide respite
Parents of irritable children often feel very isolated because normal parenting experiences are often precluded. For example, many parents report that they cannot take their child to play groups, birthday parties, or other family gatherings because their child will fall apart. Parents often express the fear that other caregivers may abuse their overly distressed baby, thus resulting in the parents never leaving their child with other caregivers when respite is sorely needed. When parents must cope with an infant who cries in excess of 2 hours per day or a child who is highly irritable, respite should be explored to help parents restore their capacity to deal with their overly fussy infant. The caregivers should give themselves a break before they explode at their child. Parents should be encouraged to put their child in a safe play area (not the crib or bedroom where he sleeps), leave him for a few minutes so that he can calm down while the parents take a break for themselves as well.
11.16. Address the parent’s anxieties about the child’s behavior
It is important to talk with the parents to address their own anxieties/perceptions as to why their child is crying or is irritable. For example, one set of parents believed that their young baby felt abandoned when she cried despite the fact that her parents were by her side almost constantly. As we explored this, it became apparent that both parents had issues around being emotionally neglected by their own parents. Once they learned ways of maintaining healthy connections with their child and became comfortable separating from their child, both parents and child became less anxious when together and apart.
It is often useful to help the parents become more attuned to their own reactions to their child’s irritability. For example, if the child is anxious or angry, some parents may resonate to the child’s emotion, becoming almost contagious to the same emotion. Instead of organizing or calming the child, the parents’ reactions may cause emotions to escalate. As a result, sometimes irritable children end up having irritable parents and the irritable mood pervades the household.
11.17. Help the parent to differentiate what the crying or irritability means
Part of the therapy should focus on helping the parent to observe when the child’s cry or irritability is changing and to recognize when and how the child self-soothes. Sometimes parents misconstrue normal babbling sounds as whining or they may view the child as constantly irritable when in fact they are not. The therapist should empathize with how bad the crying or whining feels for the parents, then help them to read their child’s signals. For example, the therapist might guide the parent “Let’s listen and see if we can tell what your child is telling us right now.” By taking on a “watch, wait, and wonder” stance, the parent can step back from the experience momentarily to be better able to read the child’s vocal and gestural signals. The therapist can then help the parent to distinguish between frustration, poor self-consoling, and expression of negative affects (e.g., aggression, discontent). In addition, the therapist should try to help the parents in grieving that they didn’t get the child they might have wanted and instead have one who is difficult, irritable, and demanding. Sometimes it is important to help the parents to learn to accept that their child will always be more demanding and irritable in nature than other “easy children.”
12. Case examples
12.1. A young child with irritability
Tommy was a toddler with extreme high irritability who would cry uncontrollably most of the day. Nothing seemed to soothe him. Even when spoken to softly by his mother, he would restart his crying again inconsolably. Tommy was recognized as different soon after birth. On his second day of life, a nurse from the newborn nursery approached his mother saying, “Mrs. G., you are going to have to do something about Thomas. He’s keeping all the other babies awake.” When he first came home from the hospital he was sleeping approximately 12 out of the 24 hours, and screamed most of the time that he wasn’t asleep.
Earliest interventions were with a pediatrician who diagnosed the baby as having “colic” and prescribed a sedative when he was 4 weeks old. Neither parent wanted their baby to be medicated, so the mother instead got a referral to a nurse practitioner. She explained that Tommy was very easily overstimulated—even by things, such as faces, lights, and noises. She recommended decreasing stimulation by doing things, such as holding him facing away from mother when feeding and sound-proofing his sleep environment.
In Tommy’s first year, he had otitis several times which was used as the explanation for his persistent crankiness. By the time I saw Tommy, there was no current evidence of chronic ear pathology and the remainder of his medical history was negative. He had good weight gain on breastfeeding, but was weaned at 3.5 months of age because he kicked and punched, which his mother interpreted as his way of fighting being held. Once on bottle feedings, he slept through the night.
Tommy’s mother tried to return to working part-time when he was 3.5 months old. He was placed in a family daycare, where he was with two other children. The babysitter described Tommy as “sensitive” and often said that he was cranky all day long. When the babysitter decided to take in more children, Mrs. G. decided to stay home with Tommy. She felt that Tommy’s fussiness could cause a caretaker who didn’t really love him to abuse him. The parents had a limited support system to provide respite.
Mr. G. seemed to have the best luck in soothing Tommy, seemingly because he was better able to rough house with Tommy in ways that his mother was unable to do. Whenever she felt frustrated with Tommy, she gave him to her husband. Mr. G. pointed out to his wife that she often acted irritable and tense with Tommy which he thought contributed to the problem. Mrs. G. admitted having a great personal struggle with her current feelings about this child. She often doubted her capacity to be a mother, and even had these thoughts before Tommy was born, mainly because she felt she lacked the experience to be a good mother. She felt publicly embarrassed by his unsoothable crying.
12.1.1. The diagnostic work-up
Developmental testing showed that Tommy was functioning at age level but there seemed to be definite evidence of an expressive language delay but no receptive language difficulties. He was unable to sit and play with toys and he had difficulties initiating planned and purposeful actions, both indicators of motor planning problems. We also noted that Tommy seemed slow in processing information during attentional tasks. On the Test of Sensory Functions in Infants, Tommy demonstrated severe hypersensitivities to touch and movement and difficulties motor planning simple motor actions. He much preferred gross motor tasks, but he showed some interest in looking at pictures and magazines. Tommy had poor balance and often fell as he maneuvered around the room. He also had low muscle tone and sat with a slouch. Our test findings and observations showed that Tommy had delays in expressive language and balance, low muscle tone, and hypersensitivities to touch, sound, and movement, as well as attentional difficulties.
In spite of the mother’s feelings of inadequacy, we noticed how gentle and supportive she was of her son. When she played with Tommy, mother tended to be rather understimulating and at times somewhat withdrawn, especially when Tommy played quietly. Mrs. G. was aware of this to the extent that she described not wanting to “rock the boat” when he was calm. Most of her interactions with Tommy centered around assisting him obtain an out of reach toy or to introduce a new toy when he became fussy or distracted. No symbolic play or reciprocal interactions were observed. When he handled toys, it tended to be more stereotypic like taking toys in and out of boxes or shaking and banging toys.
12.1.2. Treatment process
In our early sessions, we focused on decreasing the tension between Tommy and his mother, and in the context of unpressured play with her, on developing initiative, reciprocal interactions, purposeful manipulation of toys, regulation of mood state, and desensitizing responses to touch and movement. During the child-centered activity, Tommy spent a considerable amount of time lifting heavy push carts, pounding and pushing them on the floor, thus providing himself with heavy proprioceptive input and desensitizing his responses to loud noises. His mother discovered that when she gently imitated him, his pleasure and length of playing time increased. In the first week of treatment, we encouraged Mrs. G. to play with Tommy in a large bin of styrofoam chips and to explore textured objects (i.e., slinkies, stretchy toys), tactile activities that Tommy soon began to crave.
Within a very short period of time, Tommy developed a strong interest in interacting with both his parents. He seemed to gain enormous pleasure engaging in reciprocal interactions with both of them which delighted his parents. By the third week of treatment, Tommy’s crying behavior was significantly diminished. The critical break appeared to occur once Tommy was able to express himself through gestures and he could tolerate touch, sounds, and movement. Tommy became much less reliant upon his close to the ground positions, including the W-sitting posture, and fell much less often when walking. Moreover, he became very interested in looking at pictures and wanted to know the names of everything.
After 3 months of our focused intervention on facilitating Tommy’s development through play and addressing the foundations of the parent–child relationship, Tommy was referred to an early identification program where he received individualized speech and language therapy and occupational therapy. As Tommy improved, his mother began to talk about the contribution her self-doubts and depression had made to their difficulties.
12.1.3. Follow-up
By the time Tommy was 4 years of age, he had made substantial progress in all areas of development. Upon testing, we found Tommy to be a very bright and verbal child. He was sociable and engaging. At school he had friends and home life was going well although his mother found that she needed to adhere to predictable routines and avoid introducing too many changes. The only intervention that was needed at the time was sensory integration therapy to address problems with motor planning, coordination, and balance. When Tommy reached third grade, the demands of school and homework became difficult for him and he needed tutoring, but overall did well in his development as he grew older. Tommy is an example of a child who was highly irritable at birth and how with good intervention in the first 2 years of life, we might have prevented long-term serious emotional and developmental problems.
12.2. A school-aged child with irritability
As a baby, Ceci was very fussy, suffering from reflux. The only thing that seemed to calm her was vigorous swinging, bouncing, and bear hugs. She was very tiny for her age, and at age 9, she looked more like a 6-year-old. Her 6-year-old sister and her friends loved to pick her up and would swing her around like a baby doll. Ceci craved sugar, avoided proteins, and ate mainly vegetables and salad. Ceci did not like to be touched, kissed, or stroked, but frequently wanted her parents to sit next to her. Tantrums were a daily occurrence in the T. household. Ceci could be easily set off, and usually awakened screaming “I hate you!” to her parents when they went in to waken her for school. The mother found that giving Ceci a squeeze hug helped organize Ceci, but they had fallen into a bad pattern where both parents did everything for Ceci to avoid conflict.
Despite Ceci’s tiny size, she was ferocious when she kicked or hit her parents. Mom’s shins were constantly bruised from these assaults. Ceci also had the instinct to throw everything from remote controls to food that she didn’t want to eat. If mom or dad tried to contain Ceci’s physical outbursts or throwing behavior, she would scream, “You hit me!! Stop pushing me!” The rages were unpredictable and could occur over the slightest change in routine. Once upset, Ceci often did things like dig her fingernails into herself or bang her head hard against the wall exclaiming “I hate myself. I wish I were dead.” She sometimes would find sharp objects like a safety pin to push into her arm. Threats to self-harm always brought attention and concern from her parents who constantly worried that Ceci would become a cutter one day. Sometimes Ceci ramped up the self-harm to taking out a screen window in her second story bedroom and attempting to jump out. Once upset, Ceci would follow her parents around, wanting them to witness her distress. She would walk around the house knocking into furniture and lamps, thrashing wildly. When these incidents occurred, her father would take her for a car ride with the windows open, the cool air and change of scenery usually working to calm Ceci down.
Nothing seemed to be fun for Ceci, but she loved her pet cats and guinea pigs, and enjoyed drawing and playing school or grocery store. On play dates, she liked building forts and playing hide and seek.
A week didn’t go by without a major event happening. Due to Ceci’s jealousy about her younger sister, she would often do terrible things to Ellen while she slept. One night she snuck into her sister’s room and poured baby powder all over Ellen’s face, taped her eyelids shut with duct tape, and doused her comforter with catsup. Ellen woke up screaming from the burning on her face and eyes. On other occasions Ceci would booby trap Ellen’s bedroom door, putting a cup of pee on the top of the door that would spill on Ellen as she opened the door. On another occasion she poured toilet bowl cleaner on Ellen’s pillow. Ellen was a major trigger for Ceci. Ceci tried to ruin Ellen’s homework by pouring water all over it, or taking a gift that Ellen received on her birthday and smashing the picture frame and glass. In the same week, she threw a booster seat at Ellen’s face and cut her eye so badly that they had to go to the emergency room. Ellen lived in constant fear of her sister and felt abused by her. Her younger sister often flinched when Ceci walked into the room and sometimes hid behind a book shelf to avoid getting hit or punched by Ceci.
Sometimes these acts of aggression were directed toward her parents. She was known to take dog’s poop and put it on her parent’s bedsheets. It was a common occurrence that Ceci would fall apart on car rides to and from school or after-school activities. Things in the back seat became flying missiles projected at mom’s head. If mom told her to stop, she would grab mom’s hair and pull it as hard as she could while mom was driving, or Ceci would kick wildly on the seat back behind her mother’s seat. The whole time these tantrums were occurring, Ceci would scream things like, “You don’t love me! You wish I were dead!” When her parents might restrain her to prevent her from harming herself or others, it only reinforced Ceci’s view that she was unloved.
Due to Ceci’s strong urge to discharge tension through movement and pounding her body against people and things, we put together a calm-down box. Inside were things, such as wood hammers to pound soft clay into shapes, bubble wrap to squeeze in her hands or to stomp on with her feet, and newspapers to rip up. Ceci loved an inflatable Bop Man that she could kick and punch around in her bedroom. Jumping on a trampoline in the backyard was also an effective outlet. We made an Angry Box for all the members of the family to write down things that made them upset or angry. Ceci loved the idea that others could also be angry besides herself. She was wonderful at coming up with suggestions for others, and frequently wrote in things that bothered her to get advice. This worked better in my therapy room where it was anonymous and she could read about other kids’ problems.
Maintaining routines and sequences in everyday life was very important to Ceci’s mood regulation. We made charts with sequences from getting dressed in the morning all the way through bedtime. She could win a prize for getting enough checks in the day and if she didn’t win the minimum, the consequence was to lose electronics or screen time. Ceci craved having time with her parents to do art projects or to go to the park. She wanted “I love you” moments and time that they played with her. This was very important to improving Ceci’s behavior. We also had to equalize the Ellen–Ceci tension. We set up a system of fairness so that even days, Ceci went first on things; odd days Ellen went first. We also did several sibling sessions in therapy so that the two girls could learn how to play well together and start to enjoy one another’s company.
Another effective treatment for Ceci was to learn to signal her parents that she had “Tornedo Feelings.” This meant to not touch her or hold her down, but to either completely ignore her screaming, and if she was unsafe, to take a large pillow, give her a big hug and help her to calm down. She was allowed to throw beanbags in her bedroom if she was angry. After she calmed down, she then wanted her parents to talk to her about what made her mad and what she could do next time that type of incident came up. We redecorated a part of her bedroom to be a calm-down space where she could write down her “Tornedo Feelings.” We also developed a warning system that her parents could use with her. When she was in Yellow Alert, a problem was cooking up and Ceci was urged to tell her parents what she was feeling and to try to solve the problem with their help. If she was able to turn around a Yellow Alert feeling to the Green Calm Zone, then Ceci received a star on her chart. If, however, her mood entered the Red Alert zone and Ceci lost control, hurt people, or wouldn’t go to her room alone or with the help of a pillow hug to guide her there, then she got two strikes and lost all screen time.
During these episodes of Tornedo moments, Ceci believed that she was the “devil child.” We talked about how everybody gets mad. She was prompted to think “I had a burst through moment. I am lovable and I can be in control. My family will help me.” What also seemed to anchor Ceci was when her mother gave her a quartz crystal to carry with her, when she was at school, home, or with friends, that she believed had positive healing powers for fear, sad, or negative feelings. Every morning she and her mother would say a blessing for the day focusing on positive feelings. This provided Ceci with a mantra that she could hold onto and chant in her mind when she felt that her feelings were sliding south.
In addition to these various strategies, we also had to address Ceci’s anger at the fact that she was such a small child and that people thought her sister, Ellen, was older than her. Ceci expressed how she felt minimized by others and tossed around when kids would pick her up on the playground. She wanted people to think about what she knew and could do and not focus on her size. Practicing a script of how to talk to friends and family who talked about her smallness helped Ceci to take control. One of these scripts was “I know I am small for my age, but guess what I learned to do? I rode a horse the other day and I’m learning to knit.” We also practiced Confident Walking (i.e., runway walk with dress-ups, and so on) so that she looked like she was in-charge of her body. Practicing yoga and deep breathing accompanied by ammunition of what to say when people focused on her size helped Ceci to be less concerned about her size.
Ceci had made great strides in her therapy as a result of this integrated treatment program. She had also received medication for anxiety that had quieted her explosiveness. Although she continued to need support for her mood regulation at age 10, she viewed therapy as a wonderful place to solve problems and to feel supported and cared for.
12.3. A middle school–aged child with irritability
Laila at the age of 13 years had longstanding problems with her mood. Laila was a dichotomy—there were times when she was extremely irritable, angry, and explosive, then other times when she was quite compassionate and loving. Things usually escalated rapidly when mom or dad made a demand on Laila to review her math for a test, practice her piano, or walk the dog. Laila would typically respond with a snarky remark which quickly led either parent to blow up at her. Sometimes the end result would be hours of yelling, door slamming, and either the parents or Laila locked in their bedrooms to avoid being with one another. Usually when Mr. and Mrs. D. resorted to going to their bedroom, Laila would sit outside their door crying for hours, pleading with them to forgive her. Laila was constantly asking for one more chance, and often had either her phone or iPad taken away for punishment.
As an only child, Laila always needed the companionship of one of her parents. She got bored easily and wanted her parents to play games with her, watch movies with her, or take her places. When she did her homework or piano practice, she insisted on her parents being in the room with her. Her parents tried creating a calm-down space for Laila, but she wouldn’t go there on her own to calm down and ended up escalating her screaming to the point that she hyperventilated.
Over the 3 years of my work with Laila, I was struck by her intense need for loving attention. In our sessions, she would gaze at me with an intense look of love and caring. I used this connection with her to validate her distress, but to help her understand her ruptures in mood and to figure out what she could do to help herself. It seemed that even when Laila had a perfect day of relaxation, she still got overwhelmed easily. What set her off was the slightest denial of what she wanted. Small arguments began when she felt that her parents promised her something, then said no, or if they wanted her to do something for the family like fold the laundry and she was not in the mood. A typical kind of argument might start over Laila feeling that she had nothing to wear for the choral concert, then she would find her white shirt and black skirt dirty in the hamper because she hadn’t planned ahead. Occasionally the fights between Laila and her mother could be over Laila choosing to wear something that mom didn’t approve of. Mom’s tendency to be blunt and too honest toward Laila would completely trigger her. For instance, one time Laila was wearing a skirt that rode high on her waist. Mom said that she should pull it down onto her hips and untuck the blouse because it made Laila “look fat.”
Laila thought about how she would like to go in a time machine and change the past. She regretted her behavior and wished that she was different, but she was constantly on the verge of a burst. She felt enormous shame about her mood, but also felt that nobody understood her and that she was alone with this internal state of distress. Part of the problem, too, was that Laila had no best friend and usually alienated her friends by her reactivity and by making highly judgmental comments. For instance, a girl came to school one day with tissue paper stuck in her bra to augment her breasts. Laila confronted her and said, “I know what you’re doing! You’re not fooling us.” She would frequently roll her eyes or get huffy when anybody at school annoyed her, including her teachers.
As we look more closely at the emotional underpinnings of Laila’s mood dysregulation, there are several things that seem to load the deck. She had an intense need to be soothed and loved by others. For instance, she couldn’t go to sleep unless she hugged her parents and was reassured. There were times that she expressed to me worries that her parents would die and she would be left alone. She quickly went to worries about being abandoned. On the flip side, her parents felt that she was suffocating to be with, never-ending with her neediness. She became intensely overfocused on something that she wanted for herself like getting a particular shampoo at the store, then couldn’t let it go, harping on it until her parents gave in or took away her privileges. She also did not seem to have any understanding of how her tantrums impacted others. When her mother said that she had had enough and put in earplugs to muffle out her screaming, or went into her bedroom to get away from Laila, Laila interpreted it as complete rejection. Laila always needed to have the last word on everything. She often pried into her parents’ personal lives to find out secrets. Sometimes she went through their bureau drawers to find whatever she thought they could be hiding. Mrs. D. felt that she had no privacy whatsoever from her daughter, feeling constantly intruded upon.
As Laila entered the teen years, problems arose with phone and internet usage. On a few occasions, Laila would post derogatory remarks about another girl, hoping that she would leave the school because Laila disliked her so much. Once she posted a photo of her breasts that was circulated around the school and resulted in the police coming to school to confront her. She sometimes signed up for apps that were for 18 years and older, then would lose her phone privileges for several months. Her parents put parental controls on all her devices and felt that they had to constantly monitor her.
Proper diagnosis was important to Laila’s treatment plan so that we could assess if she needed medication to help stabilize her mood. Through systematic observations and comprehensive evaluation of mood, we determined that Laila was suffering from bipolar mood disorder. She was helped by medication, but with the unfortunate side effect of weight gain. She also had weekly therapy in addition to participating in group psychotherapy to gain feedback from peers about her behavior.
What has worked for Laila? Because of her high need for validation and connection with others, it was very important that the therapy have this as a foundation. Fortunately Laila felt very nurtured and cared for by me and was open to talking about her mood ruptures without feeling ashamed. She loved to write poetry and stories about her moods and drew beautiful pictures that depicted how she felt. This expressive mode was very useful as a medium between therapy sessions. To help Laila handle her internal state of distress, we constructed two plans—one for home and the other for school. Finding healthy escapes to calm down that she could absorb and make use of was very important. At home her safe place was her bedroom where she would go and hug her stuffed animals, listen to music, or look at one of the meditation apps on her phone, such as Head Space or Soul Buddy. I encouraged Laila to write down what was upsetting to her to share with me in the next session. Sometimes she would call me in an agitated moment and just talking with her for a few minutes helped to deescalate the terrible mood.
Out of the home, Laila was coached to move away from the conflict at hand, to step out in the hallway, or go to the bathroom and take deep breaths, chant a mantra in her head, distract herself with calming thoughts, and think through what would be a good resolution before returning to the situation. I encouraged Laila to quiet the part of the brain that was “on fire” and to not let her feelings take over. It helped her to think about how the planning and thinking part of her brain had gone “off-line” and that she was allowing her emotional brain to take over. I emphasized that she needed to build a highway between the planning center of her brain and her mood center, to take charge of her feelings and quiet the terrible mood to a calm place. Unsticking her negative thoughts was also important. If she was stuck on a negative cycle, I practiced with Laila how to switch topics to something less volatile, then return later in the conversation on what agitated her so. Usually this channel switch helped her to unstick the negative thinking. Laila was also very responsive to body techniques to organize her body and release anger. She liked pounding a pillow or squeezing bubble wrap when enraged. Two good outlets for Laila were marching up and down the steps while pounding her feet or playing a loud, percussive piece on the piano. I also taught Laila yoga and tai chi movements that facilitated movement with breath control. If she could breathe deeply and move while focusing her mind and vision on a beautiful object, she felt much better.
It was very important to teach both Laila and her parents various dialectical behavioral techniques to help them communicate better with one another, to tolerate the distress state that they all felt, and to do calming activities together as a family like something as simple as enjoying a cup of tea together. Equally important was the need to shore up the attachment between Laila and her parents through mutually satisfying activities that gave them pleasure. It was important that they begin to enjoy one another again. The most successful activities tended to be ones outside of the house like going shopping or to interesting places, but I encouraged them to make mealtimes special when they could talk about their days and topics that were fun or compelling. I also encouraged them to spend time together just being in a calm space without arguing (i.e., reading together with music playing in the background, watching a movie together).
13. Summary
In this chapter, the different ways that constitutional and emotional factors contribute to emotional disorders were described. As demonstrated by the review of the literature and case scenarios, it is important to take into account the various ways that emotion regulation occurs and is manifested. The developmental–structuralist model described by Greenspan suggests that both adaptation and psychopathology can be described by the way in which sensory and affective-thematic experiences are organized. A comprehensive treatment model incorporates how the individual functions in his environment while focusing on helping the child develop the capacity to engage and self-regulate, to organize purposeful social communication and interactions with others, and to express emotional ideas and feelings while also learning how to self-monitor and evaluate the appropriateness of their responses. Therapeutic approaches need to address the child and family functioning, environmental modifications that support self-calming and organization, as well as parent–child interactions.