Testing bond strength: the case of dental biomaterials
Abstract:
The collection of laboratory data is often perceived as being driven by a desire to use such data as a predictor of clinical performance. Some experiments are designed to test the fundamental behavioural characteristics of a material and other experiments are designed to study their performance when in function. In this chapter, the various approaches to the laboratory-based assessment of dental adhesives will be explored. The chapter will take a critical look at the design of the experimental methods and clarify issues in relation to our ability to assess the performance of an adhesive.
Note: This chapter has been previously published in Dental biomaterials: imaging testing and modelling, ed. R. V. Curtis and T. S. Watson (Chapter 11 ‘Modelling bond strength in dental biomaterials’ by R. Van Noort), Woodhead Publishing Limited, 2008, ISBN: 978-1-84569-296-4.
18.1 Introduction
A considerable number of years ago, when I first joined the Dental School in Sheffield, I raised the question as to which was the best resin composite on the market. The only feedback I could get at the time was some comments about the relative merits of different materials based on personal experience and personal interpretation of a limited array of laboratory data about the products then on the market. In my naivety it seemed that a clinical study should be able to answer that question without too much difficulty. Ten years later I realized that things were not quite as straightforward as I imagined. By the time the work was published (van Noort and Davis, 1993), most of the materials that had been selected for the study no longer existed and thus, although it answered the fundamental question as to which material was best, the question itself had become irrelevant.
The presumption with an evidence-based approach to the selection of dental materials is that a material is developed and tried clinically and in time we receive feedback on its clinical performance. In the meantime, a new material comes along and as we receive clinical feedback on its performance we can then compare one with the other material and decide which is the better of the two (Fig. 18.1) (see www.cebm.utoronto.ca). In reality the life span of a dental material is probably no more than 3–4 years before it is modified in the light of clinical experience and with each change the gathering of an evidence base of performance has to start all over again (Fig. 18.2). The extrapolation of data from one material to its supposed improved version is fraught with danger and the path to better dental materials is littered with casualties where the new improved version did not live up to expectation. Thus, by the time we have the clinical data it is too late to use it in our decision making as the material has changed or disappeared from the market.
My reason for recounting this story is that as a consequence of the short life span of a dental material, enormous emphasis is placed on the properties of a dental material that can be measured in the research laboratory as the gathering of clinical evidence takes such a long time. Thus, the collection of laboratory data is often perceived as being driven by a desire to use such data as a predictor of clinical performance. It is important that this point is appreciated from the outset as this puts quite a different complexion on the reasons why many laboratory-based experiments are carried out on dental materials. Whereas the research of the clinically oriented scientist seeks to establish a link between experiments carried out in the laboratory and the potential clinical performance of a material, the materials scientist’s view of laboratory experiments is, generally speaking, quite different from this. The materials scientist will carry out experiments in the laboratory in order to understand how a material behaves and what factors control its behaviour. This allows the scientist to identify ways and means of improving the properties of a material. From their perspective, whether or not the material will meet the needs of a certain application may only be a secondary consideration. For example, the laboratory-based scientists may improve the properties of a fibre-reinforced resin composite but they would not even attempt to claim that this would make the ‘improved’ material suitable for making dentures or dental bridges. The point I am seeking to make is that some experiments are designed to test the fundamental behavioural characteristics of a material and other experiments are designed to study their performance when in function. It is important that we differentiate between these two types of experiments. For example, a micro-tensile bond strength test is designed to assess the fundamental behavioural characteristics of materials, whereas a microleakage test examines the performance of a material during function. The latter can generally be regarded as an attempt to test the material in a situation that simulates the clinical application of the material. One distinct difference between the two approaches is that, in the former, the variables can be reasonably carefully controlled, whereas in the case of the latter one has to deal with a multitude of variables that contribute to the outcome.
In this chapter, the various approaches to the laboratory-based assessment of dental adhesives will be explored. We will take a critical look at the design of the experimental methods and clarify issues in relation to our ability to assess the performance of an adhesive.
18.2 Rationale for bond strength testing
It is not unreasonable to take the point of view that if a material is to be used as an adhesive then one should test its adhesive qualities. However, that does not necessarily mean that we only need to look at the ability of the adhesive to bond to a surface, be it soft tissue, bone, enamel, dentine or any man-made material. One factor that is often overlooked is the requirement for the adhesive to act as a means of transferring load from one part of a structure to another. This generates stresses and strains within the adhesive and it is important that the adhesive has the necessary mechanical properties to withstand these stresses and strains. For example, one might happily use Blu-Tack to stick bits of paper to the wall but one would not do the same with a framed picture. The ability of the Blu-Tack to stick to the wall or the picture is not really the issue here, but its inability to carry load is a problem and is fundamentally the reason why it would fail as an adhesive. Thus, the assessment of an adhesive should be based not merely on its ability to stick but also its ability to carry load; that is, more often than not, the adhesive has to be able to contribute to the structural integrity of the whole unit. This requires one to differentiate carefully between the need to assess the integrity of an adhesive bond, on the one hand, and the requirement for a structure to carry load, on the other. Some experiments are designed to do the former, while others are designed to test the latter. Those designed to test structural integrity can be recognized as experiments that seek to simulate the clinical situation. Thus shear or micro-tensile bond strength tests are experiments that test the integrity of the adhesive bond, while the enamel debonding test for an orthodontic bracket is an experiment seeking to simulate the clinical situation.
When one sets out to design a research project, the starting point is always to define the question one is seeking to address. Once one knows the question to ask one can then design the experiment that will seek to answer that question. This may all seem very obvious but it is noticeable in the ways that data are manipulated and presented that this fundamental point is often overlooked. When one considers this in the context of bond strength testing then it is important to appreciate that most bond strength tests are designed and conducted to answer a specific question. For example, a bond strength experiment may be conducted to determine the quality of the adhesion of a particular bonding system by examining the bond strength, and perhaps more importantly the mode of failure. Based on the information obtained it may be possible to suggest a means of improving the adhesion by overcoming any weaknesses that have been identified. You will note that this experiment would not provide an answer as to the clinical performance of the adhesive since that wasn’t the question that was addressed. Nevertheless we regularly see attempts to try to extrapolate from bond strength data to clinical performance. If one wants to ask the question: ‘What is the relationship between bond strength and clinical performance?’, then one must design quite a different experiment to answer that question. Conducting only bond strength tests will not answer that question. Thus, it needs to be made clear from the outset what is the purpose of the experiment being conducted. In summary, one can look upon adhesive interface testing as addressing different issues depending on how the experiment is designed. It is vitally important that the experiment undertaken matches the question asked such that one does not fall into the trap of making unjustified extrapolations to situations that the original question was not meant to address and for which the experiment was not designed.
18.3 Classification of dental adhesive testing techniques
The types of laboratory experiments that can be conducted on dental adhesives can be classified into two types, namely behavioural tests and structural integrity tests. In the behavioural tests one seeks to establish the fundamental material behavioural properties. Examples of the sorts of things one might measure are tensile strength, elastic modulus, fracture toughness, coefficient of thermal expansion and translucency. In structural integrity tests, one sets out to provide an experimental arrangement that simulates the usage of the materials. Typical examples of such tests in dentistry include strength and fatigue testing of crowns and bridges, wear tests and microleakage tests. It is important to appreciate the distinction between these two approaches to materials testing.
18.3.1 Behavioural tests
In the behavioural tests the focus is on understanding how the material behaves and how one might be able to change the properties of the material by changing such things as its composition. The critical feature of the design of these experiments is that one needs to ensure that the data gathered are correct and appropriate, otherwise they can very easily be misinterpreted and the wrong conclusion may be drawn. For example, in the compressive strength test of a cylinder, the failure of the materials is in fact a combination of shear and tension, and the calculation of the compressive strength by dividing the stress at failure by the cross-sectional area of the cylinder is actually not valid (Fig. 18.3).
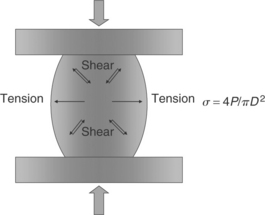
18.3 Complex tensile and shear stresses generated in a compressive strength test; σ, stress; P, load; D, diameter.
If one simply uses the test as a means of monitoring the setting process over time of a material such as a glass ionomer cement, or monitoring whether the compressive strength of the material is improved or made worse by a change in formulation, this does not matter, but if one were to try to extrapolate the data from the compressive strength test to a clinical compressive loading situation then this would be an erroneous use of this property of the material, since the stresses and strains generated under clinical loading conditions will be quite different from those in a compressive strength test.
18.3.2 Structural integrity tests
In structural integrity tests, the material is being applied in a situation in an attempt to provide some insight into how the material might respond to a clinical environment and to learn what makes the structure fail. This will be a complex interaction between material, design and environment. Thus, the structural integrity test is seeking to establish a link between the material and its performance in a clinical situation. How effective this is depends on the quality of the design of the structural integrity test and there will be a need to validate the simulation.
The testing of crowns and bridges under various loading conditions is an example of structural integrity testing. Some of these tests are designed to answer the question as to whether or not the structural integrity is compromised by a change in materials or design, of which a typical example is the so-called ‘crunch the crown’ experiment. Often such experiments are criticized for their lack of clinical relevance, but one has to remember that these experiments are designed to assess the complex interaction between materials and design. The question being addressed in such experiments is whether or not the structural integrity of the structure has been compromised to such a degree that there is little point in carrying out the much more complex and time-demanding experiments that test the durability of the structure. If one now adds the ingredient of environment along with those of materials and design, then the experimental design needs to reflect that and issues such as cyclic loading and corrosion become much more important (Fig. 18.4). One sees this for example in wear tests, which try to examine simultaneously the complex interaction between different loading conditions and environments, and where the validity of the clinical wear simulation will determine the popularity of the wear tester in terms of its ability to predict the clinical performance of a material or a device.
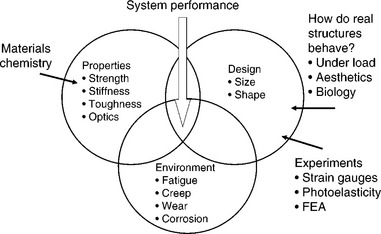
18.4 The factors influencing the performance of dental materials in the oral environment (FEA, finite element analysis).
As the experimental design becomes more concerned with asking questions about the potential performance in the clinical situation, so the experiments make a paradigm shift from the evaluation of the physical and behavioural characteristics of materials to what is more accurately described as system performance. It is important that this distinction is appreciated, otherwise one may fall into the trap of thinking that one is undertaking a test to determine fundamental materials properties whereas in fact one is conducting a structural integrity test. For example, the testing of the bond strength of orthodontic brackets is a structural integrity test, not a test of behavioural characteristics, and is potentially open to misunderstanding if one is unaware of this distinction (Eliades and Brantley, 2000).
It is important that the distinction between a behavioural test and a structural integrity test does not become blurred as the danger is that the experiment will not be able to provide valuable answers. Thus, the focus in the behavioural test must be on ensuring that the measurements undertaken provide genuine and reliable information on the behavioural characteristics of the material, while the structural integrity test must be so designed to provide a worthwhile simulation of the structure to be tested.
18.4 Behavioural adhesive tests
Next, I will explore some examples of what I consider to be behavioural tests and address some of the issues that arise in relation to how these tests are designed and conducted. However, before proceeding it is worth reiterating that in my view these experiments are not designed to assess the clinical performance of the materials used. Thus, it is pointless to enter into a discussion as to the clinical relevance of these experiments. What is important is that the experiments are designed such that the information obtained can be understood and is open to the correct interpretation. The focus of this discussion will be the methods used to assess the quality of adhesion between dentine and resins, although there are obviously other examples of fundamental tests of adhesion such as bone bonding to implants (Lin and Yen, 2004), resin bonding to fibre posts (Ferrari et al., 2006) or resin bonding to ceramics (Kern and Wegner, 1998; Della Bona et al., 2000).
18.4.1 Shear bond strength test
Of all the adhesive tests used in dentistry, the shear bond strength test has been one of the most popular bonding experiments ever devised. Its popularity has much to do with the simplicity with which this experiment can be conducted. When this experimental design was first introduced the quality of the dentine bonding agents was quite poor relative to the bonding agents available today. In those initial experiments the bond strength was so poor that failure would generally occur at the adhesive interface such that the bond strength, reported as a shear stress based on the ratio of load to bonding area, could be used as a measure of the quality of the adhesion achieved. As the quality of the adhesive bond improved then one would expect this to be reflected in an increase in the shear bond strength. However, it should be noted that this calculation of failure stress is in fact erroneous. The experimental design of the specimen and the manner of loading are such that the stresses experienced at the adhesive interface are extremely complex, as shown in Fig. 18.5. Failure is more likely to be due to interfacial tensile stresses generated as a consequence of the bending action rather than genuine shear (van Noort et al, 1989). In addition, these tensile stresses can be considerably higher than the calculated shear stress. When bond strength values were low this was not a problem and as long as the experimental design used was consistent in terms of size, shape and load application, different adhesives could be compared by calculating the nominal shear bond strength.
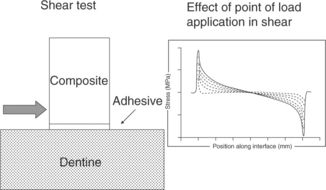
18.5 Interfacial stress distribution of the vertical stresses (σyy) for a shear bond strength test arrangement, showing high levels of tensile stress below the point of load application and compressive stresses on the side opposite to the point of load application.
Where one has to be really careful is in comparing shear bond strength data from experiments carried out in different laboratories. Minor modifications in the method used can potentially have a profound influence on the outcome of the experiment, such as, for example, the mode of application of the adhesive. Quite different results can be obtained if the adhesive is applied liberally over the dentine surface as compared with when it is constrained to the adhesive interface (van Noort et al, 1991). This problem is exacerbated by all the other variables that can come into play when bonding to dentine (Al-Salehi and Burke, 1997; Tay and Pashley, 2004).
Figure 18.6 shows that, for the unconstrained adhesive interface situation, the maximum stresses tend to occur at the adhesive/composite interface, while for the constrained condition the maximum stresses are at the dentine/adhesive interface, which invariably will produce different results. Thus, while it is reasonable to compare the adhesive performance of different dentine bonding agents within a laboratory, the comparison of data from different laboratories is fraught with danger, unless one can be sure that exactly the same experimental conditions were used.
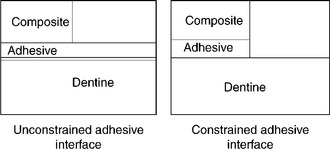
18.6 Finite element analysis of the stress distribution for an unconstrained adhesive interface and a constrained adhesive interface.
As dentine bonding agents improved so another problem came to light, namely fractures no longer occurred at the adhesive interface but would tend to be cohesive in nature, more often than not involving the dentine. The reason for this is that the stresses generated by the bending action will predispose any crack that forms to deviate into the dentine when confronted with a strong adhesive bond. In shear bond strength tests this deviation of the fracture mode from the interface into the dentine tends to occur at a nominal shear stress of some 20 MPa. This has led some people to suggest that the bond strength exceeds the cohesive strength of the dentine and that the maximum bond strength that can be achieved to dentine is of the order of 20 MPa, which seriously misunderstands the actual situation. This interpretation does not fit comfortably with the observation that the ultimate tensile strength of dentine may be as high as 100 MPa (Bouillaguet et al., 2001). It is much more likely that the transition from an interfacial failure to a cohesive failure of the dentine is as much a consequence of the improved adhesion as it is of the design of the experiment. A similar problem arises with shear bond strength testing of resins to ceramics, where fractures are frequently cohesive in the ceramic (Blatz et al., 2004), which has been shown to be an experimental artefact (Della Bona and van Noort, 1995). The correct way to interpret the situation is that when cohesive failure of the dentine becomes the dominant mode of failure, it is no longer possible to differentiate between the different dentine bonding agents and an alternative test needs to be used. One such test that is gaining in popularity is the micro-tensile bond strength test.
18.4.2 Micro-tensile bond strength
The micro-tensile bond strength test has been gaining in popularity since it was first introduced in the early 1990s (van Meerbeek et al, 2003). The most important difference between the micro-tensile test design and the shear test design is the potential ability for the micro-tensile bond strength test to be able to calculate the average tensile stress at the adhesive interface. The concept is the same as one that has been used in engineering for decades whereby the stress–strain behaviour of a material is assessed using a dumbbell specimen design (Fig. 18.7). The idea behind this design is that all measurements are taken in the central part of the specimen, well away from the clamping site, such that a uniform stress field is generated and the local tensile stress can be calculated simply from the load divided by the cross-sectional area. The wider section of the specimen at each end is there to ensure that the specimen could be easily gripped and to avoid failure within the clamping zone as this would invalidate the experiment.
What this means is that it is then possible to assess the quality of the adhesion by comparing the tensile stress at failure for different bonding agents, evaluate the mode of failure and maybe identify the weakest link in the system, without this being influenced by geometric design features. The two notable differences that should strike one immediately when examining micro-tensile bond strength data: firstly, the 20 MPa ceiling observed for the shear bond strength test has disappeared and tensile bond strengths in excess of 40 MPa can be achieved; secondly, cohesive failure of the dentine is a much less common occurrence. Thus, the constraints imposed by the design of the shear bond-strength test have been removed.
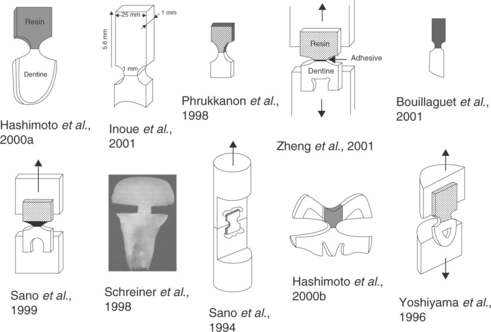
As with all new tests, within a very short time of its introduction, various forms of the micro-tensile bond strength test have appeared (Fig. 18.8). There is a danger with these alternative designs that the original premise of producing a uniform stress at the interface is lost. The sorts of designs now used include the simple stick, dumbbell and various re-entrant designs. It is the latter that have become the main area of concern, since the interfacial stress will be affected by the degree of the re-entrant design. This means that we could again find ourselves in the situation where it becomes impossible to compare the results from different laboratories because of the use of different specimen designs.
Recently published work has shown that the micro-tensile bonds strength for the stick, dumbbell and parabolic designs are pretty much the same, but that sharp re-entrant shapes underestimate the stress at failure due to the stress-concentrating effect of such designs, which would suggest that one might as well use the stick specimen design since it is the easiest to produce (Betamar et al., 2007a,b).
However, using the same design is not yet the complete answer to producing results that can be compared from one laboratory to another. There is also the issue of size and results will not be comparable if widely different specimen sizes are used, despite them having the same shape. Since the days of Griffith’s experiment on glass fibres it has been known that smaller specimens are stronger and that this is simply a consequence of the reduction and removal of inherent flaws in the system (Gordon, 1968). The same applies to the specimens used in the micro-tensile bond strength tests and a valid comparison is only possible if specimens are of a similar size or, better still, of the same cross-sectional area (Sano et al., 1994).
18.5 Structural adhesive tests
It is important to appreciate the distinction between a behavioural adhesive test as described above and a structural adhesive test. Whenever a dental device is used in an experimental design that mimics its use clinically this is a structural integrity test. For example, pull-out tests for fibre posts (Giachetti et al., 2004), debonding of orthodontic brackets (Vicente et al., 2006), debonding of resin-bonded bridges (van Dalen et al., 2005) and crown retention tests (Palacios et al., 2006) are all structural integrity tests. The experiment involves the testing of the whole system and thus one is looking at a system response. A consequence of this is that it generally turns into a multi-factorial problem that needs very careful analysis. If appropriately constructed in terms of the question the test is trying to address then such tests can be very enlightening. One obvious concern with structural integrity tests is the validity of the experimental design used and its ability to answer the question it is seeking to address.
18.5.1 Structural integrity tests for cantilever resin-bonded bridges
As an illustration of how a structural integrity test can be used to acquire useful information on the behaviour of a complex system, I would like to take a closer look at the cantilever resin-bonded minimum preparation bridge. Numerous shear and tensile bond strength tests have been conducted with bond strengths typically being in the region of 30–40 MPa. This would suggest that a debonding force of some 300–700 N would be required to debond a cantilever resin-bonded bridge if based simply on the area of bonding provided, which obviously is absurd (van Noort, 2005). Thus it was proposed that a peel test along the lines shown in Fig. 18.9 would be more realistic for the assessment of the adhesion of the bridge.
The debonding force for the beams was found to be no more than 25 N in this experimental design, which is considerably more realistic (Northeast et al., 1994). Perhaps this is not surprising since the design produces a highly significant stress concentration at the point where the beam attaches to the base, as shown in the finite element analysis (FEA) of the system in Fig. 18.10. One concern in such a test is always whether or not the correct loading condition has been considered. Further experiments were conducted to assess the failure load in what would be the occlusal direction and it was found that the failure loads for occlusal loading were some seven times higher than those for the peeling condition (Bhakta et al, 2006). Similar observations have been reported by van Dalen et al. (2005) and thus it is reasonable to assume that failure is most likely to occur by a peeling action.
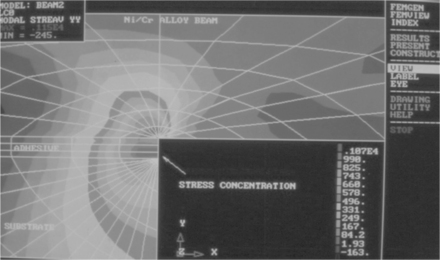
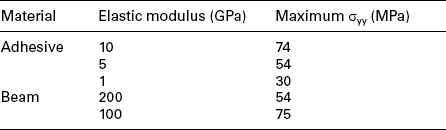
18.10 FEA model of the local stress distribution for the vertical tensile stress (σyy) for a cantilever beam.
The benefit of combining the experimental work with FEA modelling is that it provides an opportunity to interrogate the system and get an idea of what would happen if certain parameters were changed. For example, one can change the elastic modulus of the adhesive or the beam and see how this influences the peak stress in the system. The results for such an analysis are shown in Table 18.1, which would indicate that a combination of a high-stiffness beam material and a low-stiffness adhesive would provide the best outcome. This idea that a low elastic modulus adhesive provides a better resistance to failure by peeling forces deserves further study, especially since this fundamental material property has not previously been considered as a parameter for the selection of a resin-bonded bridge adhesive.
Another material parameter that may have an influence on the outcome is the fracture toughness of the adhesive, which is based on the observation that the fracture is initiated in the adhesive. As it happens, Knobloch et al. (2000) had carried out a series of experiments on the fracture toughness of luting agents and so this afforded us the opportunity to compare the peel strength of these adhesives with their fracture toughness. The results of this comparison are shown in Fig. 18.11 and there appears to be a very close correlation between fracture toughness and peel strength (Al-Ghananeem and van Noort, 2004). This would suggest that a combination of low elastic modulus and high fracture toughness is required for an adhesive for cantilever resin-bonded bridges. Thus, it may be possible to link the material’s fundamental behavioural properties to those of the system and point us to a possible solution to a problem.
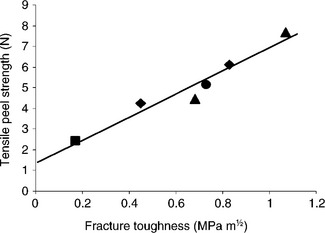
18.11 The relationship between tensile peel strength and fracture toughness of a range of luting agents.
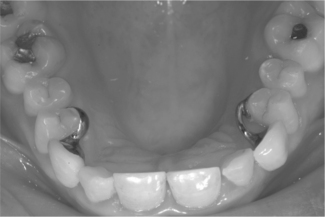
An alternative approach that can help to improve the performance of the system is to consider a change in design. The fundamental weakness is the stress concentration that arises at the point of attachment of the tooth. One way of dealing with this is to change the position of the attachment, as shown in the clinical case study in Fig. 18.12. A comparison of the peel force between the cantilever and lingual bar designs showed a peel force for the old design of 7 N as compared with 38 N for the new design (Bhakta et al., 2006). There is no doubt that there are potential problems with the proposed design, but the important point that I wish to illustrate with this example is that sometimes we need to take a step back and consider the whole system and how we may change its behaviour rather than focusing on the materials that make up that system.
18.6 Future trends
It seems to me that there are a number of avenues that still need to be trodden before we can make the connection with clinical performance. With regard to the assessment of the fundamental behavioural properties of adhesive interfaces, there is more we can do. In the case of dentine bonding, with the micro-tensile bond strength test we have an effective means of assessment of the tensile bond strength of resins to enamel and dentine and the technique can be applied to a variety of other materials. However, it is generally accepted that failure in shear occurs at lower stresses than failure in tension and therefore we could do with a shear bond strength test that genuinely assesses the resistance of the adhesive interface to shear stresses and would be as widely accepted as the micro-tensile bond strength test. Perhaps the push-out test deserves closer examination (Dhert et al., 1992) or some form of torsional shear test. Also a fracture mechanics approach to the assessment of adhesive interfaces can potentially provide more insight (Lin and Douglas, 1994; Tantbirojn et al., 2000; Armstrong et al., 2001; Della Bona et al., 2006).
Another aspect of the performance of dental adhesives that requires more attention is the durability of the bond under the aggressive conditions of the oral environment. This could range from examining the effects of long-term storage in water, or perhaps some more aggressive medium such as artificial saliva, in order to test hydrolytic stability (Carrilho et al., 2005; De Munck et al., 2006), to cyclic fatigue loading of the interface (Attia and Kern, 2004; De Munck et al., 2005).
Structural integrity tests can play an important role in the identification of potential weaknesses in a system. However, by their nature such tests are more complex and thus the results are generally speaking more difficult to interpret and also more prone to misinterpretation. Thus, it is important that these tests are designed in such a way as to be able to address the question that is being asked, and no more or no less.
Alongside the experimental testing of the structural integrity of a system, computational modelling of the system is gaining more popularity, be it an implant replacing a missing tooth (Pilliar et al, 2006), an orthodontic bracket (Katona, 1997), a veneer (Magne and Douglas, 1999) or a filling (Borkowski et al., 2006). One can approach this from the concept of benign design, by which I mean how the interfacial stresses can be minimized (Richardson et al., 2001; Bhakta et al., 2006). This is hard enough and an even greater challenge is to try to link the data from behavioural tests, such as the micro-tensile bond strength test, to the interfacial behaviour of a bonded structure under load (Fennis et al., 2005). This would provide us with the potential to make a prediction as to where and at what load an adhesive interface in a dental structure, such as a restored tooth, will fail and what we may have to do to prevent this from happening. If that were possible then we would have a seamless transition of understanding from the fundamental laboratory test to the clinical performance of our dental adhesives and we would begin to bridge the gap between dental engineering and the other engineering disciplines.
18.7 Conclusion
We have a challenge to develop behavioural and structural tests for dental adhesives that are relevant to their clinical application (van Meerbeek et al., 2003). If we are prepared to accept that our starting point is to use such tests to understand better how the materials we use and the structures we create work in practice, then such understanding and knowledge can be used to improve the system behaviour. In due course we may begin to move closer to the goal of being able to carry out laboratory-based experiments that will inform the clinical performance of the materials and systems being evaluated.
18.8 References
Al-Ghananeem, M.M., van Noort, R. Tensile peel strength versus fracture toughness of luting cements. BSDR Annual Meeting, Birmingham, UK, April, 2004. [(abstract)].
Al-Salehi, S., Burke, F.J.T. Methods used in dentin bonding tests: An analysis of 50 investigations on bond strength. Quintessence Int.. 1997; 28:717–723.
Armstrong, S.R., Keller, J.C., Boyer, D.B. The influence of water storage and C-factor on the dentin–resin composite microtensile bond strength and debond pathway utilizing a filled and unfilled adhesive resin. Dent. Mater.. 2001; 17:268–276.
Attia, A., Kern, M. Influence of cyclic loading and luting agents on the fracture load of two all-ceramic crown systems. J. Prosthet. Dent.. 2004; 92:551–556.
Betamar, N., Cardew, G., van Noort, R. Influence of specimen designs on the microtensile bond strength to dentin. J. Adhesive Dent.. 2007; 9(2):159–168.
Betamar, N., Cardew, G., van Noort, R. The effect of variations in hour glass specimen design on the microtensile bond strength to dentin. J. Adhes. Dent.. 2007; 9(5):427–436.
Bhakta, S., van Noort, R., Cardew, G. Improved retention of anterior cantilever resin bonded fixed partial dentures by design alteration: An experimental and finite element study. J. Prosthet. Dent.. 2006; 95:209–217.
Blatz, M.B., Sadan, A., Maltezos, C., Blatz, U., Mercante, D., Burgess, J.O. In vitro durability of the resin bond to feldspathic ceramics. Am. J. Dent.. 2004; 17:169–172.
Borkowski, K., Kotousov, A., Kahler, B. Effect of material properties of composite restoration on the strength of the restoration – dentine interface due to polymerization shrinkage, thermal and occlusal loading. Med. Eng. Phys.. 2006; 29:671–676.
Bouillaguet, S., Gysi, P., Wataha, J.C., Ciucchi, B., Cattani, M., Godin, C., Meyer, J.M. Bond strength of composite to dentin using conventional, one-step, and self-etching adhesive systems. J. Dent.. 2001; 29:55–61.
Carrilho, M.R., Carvalho, R.M., Tay, F.R., Yiu, C., Pashley, D.H. Durability of resin-dentin bonds related to water and oil storage. Am. J. Dent.. 2005; 18:315–319.
Della Bona, A., Anusavice, K.J., Mecholsky, J.J., Jr. Apparent interfacial fracture toughness of resin/ceramic systems. J. Dent. Res.. 2006; 85:1037–1041.
Della, A., Anusavice, K.J., Shen, C. Microtensile strength of composite bonded to hot-pressed ceramics. J. Adhes. Dent.. 2000; 2:305–313.
Della Bona, A., van Noort, R. Shear versus tensile bond strength of resin composite bonded to ceramic. J. Dent. Res.. 1995; 74:1591–1596.
De Munck, J., Braem, M., Wevers, M., Yoshida, Y., Inoue, S., Suzuki, K., Lambrechts, P., van Meerbeek, B. Micro-rotary fatigue of tooth-biomaterial interfaces. Biomaterials. 2005; 26:1145–1153.
De Munck, J., Shirai, K., Yoshida, Y., Inoue, S., van Landuyt, K., Lambrechts, P., Suzuki, K., Shintani, H., van Meerbeek, B. Effect of water storage on the bonding effectiveness of 6 adhesives to Class I cavity dentin. Oper. Dent.. 2006; 31:456–465.
Dhert, W.J.A., Verheyen, C.C.P.M., Braak, L.H., De Wijn, J.R., Klein, C.P., De Groot, K., Rozing, P.M. A finite element analysis of the push-out test: influence of test conditions. J. Biomed. Mater. Res.. 1992; 26:119–130.
Eliades, T., Brantley, W.A. The inappropriateness of conventional orthodontic bond strength assessment protocols. Eur. J. Orthod.. 2000; 22:13–23.
Fennis, W.M., Kuijs, R.H., Barink, M., Kreulen, C.M., Verdonschot, N., Creugers, N.H. Can internal stresses explain the fracture resistance of cusp-replacing composite restorations? Eur. J. Oral. Sci.. 2005; 113:443–448.
Ferrari, M., Goracci, C., Sadek, F.T., Monticelli, F., Tay, F.R. An investigation of the interfacial strengths of methacrylate resin-based glass fiber post-core buildups. J. Adhes. Dent.. 2006; 8:239–245.
Giachetti, L., Scaminaci Russo, D., Bertini, F., Giuliani, V. Translucent fiber post cementation using a light-curing adhesive/composite system: SEM analysis and pull-out test. J. Dent.. 2004; 32:629–634.
Gordon, J.E. The New Science of Strong Materials, 1st. Princeton, NJ: Princeton University Press, 1968.
Hashimoto, M., Ohno, H., Kaga, M., Endo, K., Sano, H., Oguchi, H. In vivo degradation of resin-dentine bonds in humans over 1 to 3 years. J. Dent. Res.. 2000; 79:1385–1391.
Hashimoto, M., Ohno, H., Endo, K., Kaga, M., Sano, H., Oguchi, H. The effect of hybrid layer thickness on bond strength: Demineralized dentine zone of the hybrid layer. Dent. Mater.. 2000; 16:406–411.
Inoue, S., Vargas, M., Abe, Y., Yoshida, Y., Lamberchts, P., Vanherle, G., Sano, H., van Meerbeek, B. Microtensile bond strength of eleven contemporary modern adhesives to dentine. J. Adhes. Dent.. 2001; 3:234–237.
Katona, T.R. Stresses developed during clinical debonding of stainless steel orthodontic brackets. Angle Orthod.. 1997; 67:39–46.
Kern, M., Wegner, S.M. Bonding to zirconia ceramic: Adhesion methods and their durability. Dent. Mater.. 1998; 14:64–71.
Knobloch, L.A., Kerby, R.E., Seghi, R., Berlin, J.S., Lee, J.S. Fracture toughness of resin-based luting cements. J. Prosthet. Dent.. 2000; 83:204–209.
Lin, C.M., Yen, S.K. Characterization and bond strength of electrolytic HA/TiO2 double layers for orthopedic applications. J. Mater. Sci. Mater. Med.. 2004; 15:1237–1246.
Lin, C.P., Douglas, W.H. Failure mechanisms at the human dentin-resin interface: A fracture mechanics approach. J. Biomech.. 1994; 27:1037–1047.
Magne, P., Douglas, W.H. Porcelain veneers: Dentin bonding optimization and biomimetic recovery of the crown. Int. J. Prosthodont.. 1999; 12:111–121.
Northeast, S.E., van Noort, R., Shaglouf, A.S. Tensile peel failure of resin-bonded Ni/Cr beams: An experimental and finite element study. J. Dent.. 1994; 22:252–256.
Palacios, R.P., Johnson, G.H., Phillips, K.M., Raigrodski, A.J. Retention of zirconium oxide ceramic crowns with three types of cement. J. Prosthet. Dent.. 2006; 96:104–114.
Phrukkanon, S., Burrow, M.F., Tyas, M.J. The influence of cross-sectional shape and surface area on the microtensile bond test. Dent. Mater.. 1998; 14:212–221.
Pilliar, R.M., Sagals, G., Meguid, S.A., Oyonarte, R., Deporter, D.A. Threaded versus porous-surfaced implants as anchorage units for orthodontic treatment: Three-dimensional finite element analysis of peri-implant bone tissue stresses. Int. J. Oral, Maxillofac. Implants.. 2006; 21:879–889.
Richardson, C.J., van Noort, R., Howard, I.C. The influence of elastic modulus of restorative materials on the stress distribution in a canine tooth with an abrasion-erosion lesion. In: Middleton J., et al, eds. Computer Methods in Biomechanics and Biomedical Engineering – 3. London: Gordon and Breach Science Publishers; 2001:595–604.
Sano, H., Shono, T., Sonoda, H., Takatsu, T., Ciucchi, B., Carvalho, R., Pashley, D.H. Relationship between surface area for adhesion and tensile bond strength – evaluation of a micro-tensile bond test. Dent Mater. 1994; 10:236–240.
Sano, H., Yoshikawa, T., Pereira, P.N.R., Kanemura, N., Morigami, M., Tagami, J., Pashley, D.H. Long-term durability of dentine bonds made with a self-etching primer, in vivo. J. Dent. Res.. 1999; 78:906–911.
Schreiner, R.F., Chappell, R.P., Glaros, A.G., Eick, J.D. Microtensile testing of dentine adhesives. Dent. Mater.. 1998; 14:194–201.
Tantbirojn, D., Cheng, Y.S., Versluis, A., Hodges, J.S., Douglas, W.H. Nominal shear or fracture mechanics in the assessment of composite-dentin adhesion? J. Dent. Res.. 2000; 79:41–48.
Tay, F.R., Pashley, D.H. Resin bonding to cervical sclerotic dentine: A review. J. Dent.. 2004; 32:173–196.
van Dalen, A., Feilzer, A.J., Kleverlaan, C.J. The influence of surface treatment and luting cement on in vitro behavior of two-unit cantilever resin-bonded bridges. Dent. Mater.. 2005; 21:625–632.
van Meerbeek, B., De Munck, J., Yoshida, Y., Inoue, S., Vargas, M., Vijay, P., van Landuyt, K., Lambrechts, P., Vanherle, G. Buonocore memorial lecture. Adhesion to enamel and dentin: current status and future challenges. Oper. Dent.. 2003; 28:215–235.
van Noort, R. An overview of the clinical use of resin-to-metal bonding. In: Roulet J.-F., Vanherle G., eds. Adhesive Technology for Restorative Dentistry. London: Quintessence Publishing Co.; 2005:153–169.
van Noort, R., Davis, L.G. A prospective study of the survival of chemically activated resin composite restorations in general dental practice: Five year results. J. Dent.. 1993; 21:209–215.
van Noort, R., Cardew, G.E., Howard, I.C., Noroozi, S. The effect of local interfacial geometry on the measurement of the tensile bond strength to dentin. J. Dent. Res.. 1991; 70:889–893.
van Noort, R., Noroozi, S., Howard, I.C., Cardew, G.E. A critique of bond strength measurements. J. Dent.. 1989; 17:61–76.
Vicente, A., Navarro, R., Mena, A., Bravo, L.A. Effect of surface treatments on the bond strength of brackets bonded with a compomer. Am. J. Dent.. 2006; 19:271–274.
Yoshiyama, M., Carvalho, R., Sano, H., Horner, J.A., Brewer, P.D., Pashley, D.H. Regional bond strengths of resins to human root dentine. J. Dent.. 1996; 24:435–442.
Zheng, L., Pereira, P.N.R., Nakajima, M., Sano, H., Tagami, J. Relationship between adhesive thickness and microtensile bond strength. Oper. Dent.. 2001; 26:97–104.