CHAPTER 1
Healthcare Information Technology: Definitions, Stakeholders, and Major Themes
Kathleen A. McCormick, J. Marc Overhage, John E. Mattison, Brian Gugerty
In this chapter, you will learn how to
• Define the complex evolution of the computer network environment in healthcare information technology (HIT)
• Explain the fast uptake of HIT in the continuum of healthcare
• Describe how the increase in volume of HIT has expanded the capabilities to measure the value of healthcare
• Describe the need to prepare an adequate workforce aware of the unique HIT environment
• Define the roles of HIMSS and AHIMA in support of HIT credentialing, education, and training
This chapter provides an overview of some of the updated content in this second edition as well as new content pertaining to the rapid advances in healthcare information technology (HIT). These rapid advances will be briefly mentioned in this introductory chapter and further defined in later chapters. The evolution of HIT has occurred from simple systems to much more complex computer network environments.1 With this expansion, the technology has become a component of the entire continuum of care, which results in silos of information and data on individuals and communities of people. The need for integrated networks, standards, and security/cybersecurity has intensified as these systems are more commonly being used to increase the volume of HIT and monitor the value of healthcare.
The new generation of healthcare IT personnel must have adequate knowledge and skills to participate in the workforce delivering services and technology. Achieving certification is the best way for these technology and healthcare professionals to demonstrate proficiency with a standard body of knowledge endorsed by professional healthcare organizations. Two types of certification are the focus of this second edition. The first, Certified Associate in Healthcare Information and Management Systems (CAHIMS), is awarded by the Healthcare Information Management Systems Society (HIMSS). CAHIMS is a professional certification for emerging professionals who may not have a lot of experience in healthcare IT but seek a career in the field. The other is the Certified Healthcare Technology Specialist (CHTS) series from the American Health Information Management Association (AHIMA). This series originated with the Office of the National Coordinator for Health Information Technology (ONC) HIT Pro categories of exams and covers six IT roles for people in health information management. Both certifications will be described in more detail later in this chapter.
The Explosion of Healthcare Information Technology
During the past decade, the following factors have contributed to massive expansion in healthcare IT:
• A huge increase in the number of connected networks and network-enabled devices (commonly called the Internet of things [IoT])
• Access to healthcare through mobile devices, patient portals, and cloud services
• Critical cybersecurity threats
• Integration of healthcare networks
• The volume of genomics data
• The need to analyze big data
With this expansion in HIT, the healthcare informatics community has also come to realize that data standards are required to truly achieve interoperability and to mine the data for quality, efficiencies, effectiveness, and cost. In addition, the consumer has embraced direct-to-consumer genomics, mobile devices, portals, and the Internet. Consumers now demand secure and easy access to their healthcare information via healthcare apps on their mobile devices and via the Web on their home computers. When the authors defined the necessary components to understand healthcare IT in the first edition of this book, the enterprise architecture was fairly simple, consisting of a boundary, a network, a data center containing servers located in a defined, secure area, and desktop computers within a closed network. Contrast that to the time of writing of this second edition, and the architecture now contains mobile devices connected from any location, cloud services, and credentialed people accessing data in federated database infrastructures operated by business associates and other types of third-party providers. The hardware configurations that underlie the architectures for healthcare IT, the networks that support healthcare IT connections, and the services that provide diverse applications have become much more complex.
This contrast is depicted in Figure 1-1. The section on the left portrays the simpler healthcare information system that was developed 20 years ago and discussed in the first edition of this book. This second edition describes the current, more complex system depicted on the right. This highlights the rapidly evolving complexity of the computer network environment in which healthcare IT operates. Services are increasingly delivered through the Internet. Electronic health records (EHRs), for example, which historically were core applications running in a healthcare system’s data center, are frequently delivered as hosted services today. In addition, the rapidly expanding number of network-capable devices—whether mobile devices for accessing applications, communication devices, medical monitoring devices, or consumer devices such as fitness monitors and network-enabled scales—adds to the complexity and the requirements for various forms of federation and authentication. The regulatory framework for device manufacturers and importers comes from the Food and Drug Administration (FDA). The complexity of designing these systems becomes even greater when the corresponding requirements of privacy, confidentiality, security, and cybersecurity of systems and devices are taken into consideration.
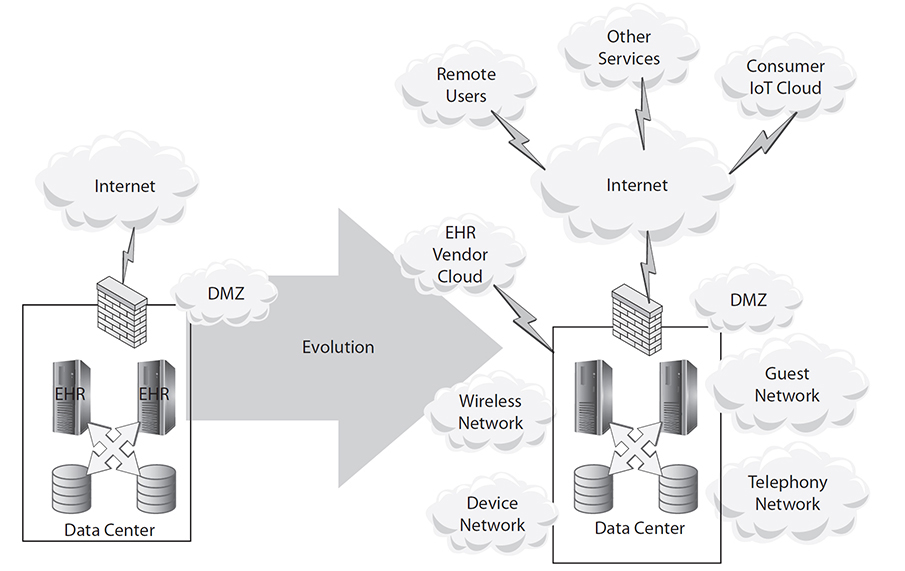
Figure 1-1 The evolving complexity of the healthcare information systems (DMZ = demilitarized zone, a network security layer)
This complexity has resulted in challenges of interoperability and interconnectedness mediated via a number of new resources. Through cloud services, mobile wireless devices, and the Internet of things, everything can be connected, requires nearly continuous updating, and requires a new understanding of how we defend, protect, and secure this new complex environment. Mobile devices now outperform the supercomputers of only 20 years ago. In this all-connected healthcare environment, the functionality is amazing, but the possibility of glitches, bugs, and exploitation from cybercriminals or mischief-makers is challenging and even formidable. Twenty years ago a handful of system administrators and software engineers managed the entire enterprise infrastructure, but now management is highly distributed across many interdependent networks. Keeping thousands of computers, tens of thousands of applications, and billions of records of all sorts properly functioning and secure in this new type of enterprise requires new healthcare IT skills.
In addition to the availability of more devices, healthcare professionals have more access to the Internet and cloud services from healthcare facilities and consumers have more access to healthcare information via the Internet (e.g., healthcare information on the Internet, mobile devices, and patient portals). The Internet was designed for universal open access and maximal participation. Security was not a priority when developing the Internet, but has since become the top priority. Migration from a low-security infrastructure to a high-security infrastructure is progressing slowly and painfully because of the conflicts between the competing objectives of “open” and “secure.” Those conflicts will require decades of ongoing negotiation and new skills in how to implement a balanced approach. The complexity of designing these systems becomes even greater when the corresponding requirements of privacy, confidentiality, security, and cybersecurity of systems and devices are taken into consideration.
New Network Complexity Requires New Standards for Data Sharing and Interoperability
The challenges of sharing data securely and achieving interoperability of the complex enterprises described in the previous section have led to the development of new open standards for authorization and integration. In 2014, Fast Healthcare Interoperability Resources (FHIR) was introduced as a new open standard for healthcare data, developed by Health Level Seven International (HL7), a nonprofit organization. FHIR is based upon developer-friendly application programming interfaces (APIs). FHIR provides for RESTful web service access (RESTful web services are one way of providing interoperability between computer systems on the Internet) to granular data elements that can be queried for individual patient data or in aggregate for population data while at the same time allowing data to be exchanged in health records in both human- and machine-readable XML and JSON data formats. FHIR also enables multiple data models and vocabularies used in healthcare.
At about the same time FHIR was introduced, an application platform for healthcare was developed called SMART Health IT. It is also an open standard (built upon the OAuth standard), and enables developers to create applications seamlessly within an EHR or on a data warehouse. This framework allows clinical care and technical IT support users in healthcare to more seamlessly draw upon the entire library of applications being used in clinical care, mobile applications, research, and public health.
SMART Health IT can be used in conjunction with the data models of FHIR to support the diverse use cases and third-party application services, to express medications, problem lists, laboratory data, and even genomic data. Currently, SMART libraries are available for HTML5/JavaScript, iOS, and Python. The libraries comprise a gallery of applications not restricted to a single EHR platform. In addition, the technology can host multiple commercial (typically requiring payment) and open source (free) applications.
System interoperability must be capable of data sharing, interoperability of data elements, and compliance with vocabulary, terminology, and messaging standards. Without common standards, boutique terms used in clinical practice have to be mapped and harmonized to national and international standards in order to measure value, monitor quality, determine if outcomes have been met, and assure safety of care. We continue to suffer from more terminology standards than warranted by the variety of use cases. Every “harmonization” effort suffers from some degree of semantic degradation, and hence a smaller set of terminologies is highly desirable.
Having surpassed the 25th anniversary of the launch of the Human Genome Project, the United States is embarking on a new journey called the Precision Medicine Initiative (PMI), a major component of which is the All of Us Research Program, the goal of which is to enroll 1 million Americans in a study of their genetic and genomic information with patient healthcare and lifestyle data using the EHR and mobile applications and sensors.2, 3 A genetics analysis of one patient is estimated to produce about 1 terabyte of data in a single encounter.4 That is considered big data, a topic explored in detail in Chapter 23. The influences of genetics and genomics across the continuum of care begin in preconception/prenatal care and continue through diagnosis and screening of disease, and monitoring therapeutic decisions of disease and recurrence.5 New evidence guidelines that predict the uptake, metabolism, and excretion of drugs are known for at least 36 common medications at the time of writing.6 Roadmaps, workflow pathways, and algorithms are being developed to include these new types of data into the EHR.7, 8 Together with telehealth utilization, these innovations will be discussed more broadly in this book. The role of social media and the personal health record will also be discussed in this second edition.
The organization of the book has changed in this edition so that more pages could be dedicated to these new advances in healthcare IT. In subsequent chapters, these concepts will be defined and the major themes will be expanded. A new Glossary defines the important terms used in this edition. The major stakeholders in healthcare IT are defined in a new appendix based upon the Standard Occupational Classification (SOC) codes for the United States. Please see Appendix C for how to access this content.
The Role of HIT in the Continuum of Healthcare
The continuum of healthcare today goes from conception to death. Depending on the circumstances, most healthcare in the United States begins either prior to conception (fertility counseling, genetic screening, etc.) or upon discovery of pregnancy. Often, prenatal care includes genetic and genomic studies of the parents and the fetus. This starts the healthcare record for many individuals today. A person born in the United States typically is delivered in a hospital and then becomes a consumer of ambulatory care. Unless emergency room visits are required, a healthy child or adolescent sees healthcare providers only for vaccinations, school and camp physicals, and regular check-ups. More recently, a nurse practitioner or pharmacist in a retail clinic or pharmacy might also see the child or adolescent. Telehealth may be available if online consultation is required for services not rendered by the nurse practitioner. When hospitalized, consumers (whether children, adolescents, or adults) become patients in community health practices in small, medium, or large healthcare facilities. As the consumer advances in age and develops chronic or acute healthcare conditions, they may be seen in specialized laboratory settings, diagnostic and treatment settings, or in a day hospital. With advancing age, a consumer may develop more serious chronic and acute healthcare conditions and require hospitalization, followed by rehabilitation in a center or as an outpatient. Advancing further, some consumers may require care for functional disabilities (that is, the inability to engage in activities of daily living [ADLs] such as walking, dressing, eating, or toileting themselves). This may require healthcare workers (and robots) to provide care in their home, or it may require assisted living, skilled nursing care, or nursing home care. In the late stages of life, hospice care may be appropriate, which focuses attitudes and resources on dying with dignity, quality, and comfort.
In each of these areas in the continuum, the expanding role of healthcare IT has driven the use of technology in all environments (ambulatory, inpatient, long-term care, and even home to the consumers themselves). There are four transformative catalysts in present-day healthcare throughout the United States that are driving changes in the way healthcare IT supports the health of the public:
• A focus on population health with services and the use of mobile technologies to support wellness and disease prevention
• Self-management for those with chronic disease and transitioning of resources and services from acute care to community and home care
• A person-centric focus in care delivery and services for consumer empowerment
• Healthcare system reform using EHRs and other technologies that extend across all levels of services and care settings, including the person’s home
The Increasing Volume and Shift to Value of Healthcare IT
The Health Information Technology Economic and Clinical Health (HITECH) Act of 2009 and its funding focused on increasing the volume of EHRs in hospitals and ambulatory care. Provisions of the HITECH Act incentivized the measurement of value and the adoption of Meaningful Use (MU). Currently the measurement of value is focused on MACRA and MIPS. These concepts will be described in the following sections.
Increasing the Volume of EHRs
As of 2011, the adoption of comprehensive EHRs in U.S. hospitals was only 8.7 percent according to a report of the results of a 2012 Robert Wood Johnson Foundation survey.9 Basic EHR adoption was 18 percent, and those reporting use of any EHR was 26.6 percent. Adoption of the EHR was a key objective of the HITECH Act, and that objective is increasingly being met. In a more current briefing from May 2016, the ONC describes a huge increase in the adoption of the EHR by non-federal acute-care hospitals from 2008 to 2015 (based on data from the American Hospital Association). In 2015, nearly all reported hospitals (96 percent) possessed a certified EHR technology (compared to 72 percent in 2011, the first year certification began), and 84 percent of hospitals adopted at least a basic EHR system (compared to 9.4 percent in 2008).10 The certification of EHR systems began in 2011 to recognize EHRs that meet technological capability, functionality, and security requirements adopted by the Department of Health and Human Services (HHS). (Notably, the report identifies two subtypes of hospitals that still had basic EHR adoption of 55 percent or less in 2015: children’s hospitals and psychiatric hospitals.10) Of those that have adopted EHRs, they are moving to optimization and updates of the systems, measuring value from the systems, and securing the infrastructure.

NOTE Also with the enactment of the HITECH Act in 2009, cybersecurity became a priority moving forward with the anticipated increase in the number of electronic health records to secure. One of the issues is that HIPAA currently does not include security risk analysis that covers personal health information (PHI) cybersecurity in medical devices, even though many devices include PHI. The issues that revolve around cybersecurity will be further discussed and described in Chapters 30 and 31.
The previously mentioned Robert Wood Johnson Foundation study also reported that the percentage of office-based physicians in 2011 who had a basic EHR was 33.9 percent, and 57.0 percent for any type of EHR.9 As of 2015, according to an ONC report, 87 percent of office-based physicians have adopted any EHR, and 78 percent have adopted a certified EHR. Over half, or 54 percent of office-based physicians, have adopted a basic EHR.11 While this represents a significant doubling of office-based physicians using an EHR, survey results indicate that a majority of offices with fewer than five physicians are still struggling to adopt an EHR.
Measuring the Value of Healthcare
Concurrent with this second edition, reimbursement changes are pushing for wider value-based care with Comprehensive Primary Care (CPC and CPC+), and the Medicare Access and Chip Reauthorization Act (MACRA) of 2015 rewards healthcare providers for providing quality care. The MACRA quality program proposes two paths for reimbursement based upon quality: the Merit-based Incentive Payment System (MIPS) and the Alternative Payment Models (APMs). These will be further discussed in Chapters 3 and 16.
The concept of value-based healthcare that is dependent upon an interoperable healthcare IT system became evident in the recent passage (December 2016) of the 21st Century Cures Act, the previously mentioned All of Us Research Program of the Precision Medicine Initiative,3 and in bipartisan statements of the U.S. executive and legislative branches of government. The 21st Century Cures Act (“Cures Act”) provides $4.8 billion of new funding for advances in PMI research into variations of disease ($1.5 billion), the Cancer Moonshot to speed cancer research ($1.8 billion), and investments in the BRAIN initiative to study brain diseases, including Alzheimer’s ($1.5 billion).12 In addition, the Cures Act incentivizes the FDA to utilize flexible approaches in reviewing medical devices that represent breakthrough technologies, and adds $500 million regulatory modernization of the development of new drugs and devices. The Cures Act will also ensure EHRs are interoperable for seamless patient care.
As this second edition goes to press, Donald J. Trump has recently become the 45th President of the United States and has appointed Dr. Tom Price as the new HHS secretary. Both have strongly advocated repealing the Affordable Care Act (ACA). It is unquestionable that the ACA regulatory burden and format may change and take a new vision for care delivery and measuring the value of healthcare. Indications are that there will not be a diminution of efforts to build infrastructure for interoperability, to improve quality monitoring, and to deliver more cost-effective and efficient healthcare embracing the new technologies and science of genetics and genomics.
A draft white paper on patient-generated health data (PGHD) policy prepared by Accenture was recently released by the ONC.13 With the increase in consumer technologies, including mobile applications and wearables, the white paper addresses the prospects and challenges for clinicians and researchers going forward through 2024.
The increase in the volume and complexity of healthcare IT requires personnel who demonstrate a standard of knowledge that distinguishes them from others in this competitive HIT workplace environment. By becoming certified in healthcare IT, you demonstrate that you have mastered the knowledge and gained the skills and tools to work in this healthcare environment. In addition, you become more valued in this competitive and expanding marketplace, thus expanding your career opportunities.14
Preparing a Critical Mass of Certified Healthcare IT Technicians and Professionals
The new and evolving complex healthcare information technology environment requires building a new type of HIT workforce.15 To help meet the growing demand for HIT professionals, the ONC facilitated the enactment in 2009 of the HITECH Act, which funded nearly $33 billion between 2011 and 2016 to subsidize adoption of HIT in the United States.16 Part of this money funded the Health IT Workforce Development Program, the goal of which was to train a new workforce of skilled HIT professionals who are able to help providers implement electronic health records and achieve meaningful use of EHR systems.
Employment of healthcare IT professionals is expected to increase by 20 percent through 2018, according to the Bureau of Labor Statistics. The U.S. government estimates that we will need more than 50,000 healthcare IT workers to help medical providers with electronic medical records—a number expected only to grow as the American population ages. A more recent Bureau of Labor Statistics report has identified that there were 188,600 jobs available in 2014 for medical records and health information technicians. This includes the category of employees who need a postsecondary certificate to enter the healthcare information technician job, and some may need an associate’s degree. The job outlook for this category has been updated for 2014 through 2024, with an estimated 15 percent growth (much faster than the average of all other job categories). Between 2014 and 2024, the expected increase in the number of jobs over the current number of jobs is 29,000.17
The Bureau of Labor Statistics currently has ten categories of computer and information technology occupations (excluding management): computer and information research scientists; computer network architects; computer programmers; computer support specialists; computer systems analysts; database administrators; information security analysts; network and computer systems administrators; software developers; and web developers. According to the Bureau’s 2015 Occupational Outlook Handbook (OOH), the median annual salaries for 2015 for these occupations range from $51,470 for computer support specialists (typically requiring an associate’s degree) to $110,620 for computer and information research scientists (requiring a doctoral or professional degree). The median salary for computer and IT occupations requiring a bachelor’s degree range from $77,810 for network and computer systems administrators to $100,690 for software developers.18
The 2015 OOH reports for the category of computer and information systems managers (which includes chief medical information officers and chief nursing information officers) a median wage of $131,600 per year. The growth in this category is expected to be 15 percent from 2014 to 2024. The Bureau estimates an increase of 53,700 new jobs during this same timeframe.19 This category also includes project managers who plan, coordinate, and direct the computer-related activities.
The 27th Annual HIMSS Leadership Survey reflects the opinions of IT professionals in U.S. healthcare provider organizations regarding the use of IT in their organizations.20 This study puts a finger on the pulse of healthcare IT annually and is reported at the Annual HIMSS meeting. This study covers a wide array of topics crucial to healthcare IT leaders, including IT priorities, issues driving and challenging technology adoption, IT security, as well as IT staffing and budgeting plans. Based on the feedback of 282 healthcare IT professionals, nearly three-quarters of the participants in the 2016 survey reported that their focus will be on clinical integration (73.8 percent), primary care provider efficiency (72.3 percent), mandated quality metrics improvement (68.4 percent), and care coordination (67.4 percent). This compares to previous HIMSS Annual Leadership Surveys, which indicated that federal mandates, including meeting Stage One, Two, and future versions of Meaningful Use requirements and a conversion to ICD-10, would be the issues driving their efforts in the years ahead.
Since there is no category of nursing informatics in the Bureau of Labor Statistics, HIMSS conducts a survey of compensation for nursing informatics certifications. In 2014, a nurse with an informatics certification made an average of $121,830 annually, compared to $106,537 for comparable registered nurses without certification.21
The Roles of HIMSS and AHIMA in Support of Healthcare Information Credentialing, Education, and Training
As indicated in the chapter introduction, the professional organizations currently certifying in HIT are HIMSS (CAHIMS certification) and AHIMA (CHTS series). The AHIMA CHTS certifications support the continuation of the previously described ONC objective to prepare a critical mass of healthcare IT technicians and professionals. (Until very recently, CompTIA also offered HIT certification through its Healthcare IT Technician certification exam, but it has retired this certification as of February 28, 2017, and does not plan to renew or replace it.22)
Healthcare Information and Management Systems Society (HIMSS)
HIMSS is a global, cause-based, not-for-profit organization with more than 50,000 members focused on better health through information technology (IT). HIMSS conducts surveys of its members, including CIOs and other executive leaders, and the results of these surveys serve today as the primary source for understanding the evolving roles, responsibilities, and professional background of informatics professionals. HIMSS has offered certification to members since 2002 when it established the Certified Professional in Healthcare Information and Management Systems (CPHIMS). A more recent certification, Certified Associate in Healthcare Information and Management Systems (CAHIMS), focuses on emerging professionals who may not have experience with HIT.
The CAHIMS exam is focused on leadership, technology environment, analysis, and privacy and security.23 The content of the exam is meant to demonstrate professional knowledge in healthcare information and management systems. It provides the person obtaining the certification a solid foundation upon which to strengthen their abilities, acquire more experience, and advance their career path.
In addition to certification, HIMSS offers broad educational programs, resources, and training in healthcare IT in a variety of formats. These include conference sessions, virtual events that provide access to a series of digital educational programs including webinars. HIMSS has regional chapter-sponsored courses that provide credits that can be applied for CPHIMS/CAHIMS certification.
American Health Information Management Association (AHIMA)
Since March 2013, AHIMA has been administering the exams for healthcare IT previously available from the ONC. AHIMA is the member association for health information management (HIM) professionals and offers certification of coders and health professionals for information management. AHIMA focuses on roles specific to HIM fields, including privacy and security, diagnosis and treatment coding, electronic health records, reimbursement, regulatory compliance, healthcare information technology, and information governance.
AHIMA serves 103,000 HIM professionals. In addition to HIM professionals, AHIMA members also include companies and consultants, individuals, and academic institutions with a focus on HIM programs. The AHIMA certification exams focus on individuals trained through short-duration, nondegree healthcare IT workforce development programs, as well as on members of the workforce with relevant experience and various types of training and academic preparation. The U.S. Department of Veterans Affairs (VA) has approved all AHIMA certification exams for reimbursement for active-duty military and veterans. Pearson VUE offers the AHIMA exams in multiple locations throughout the country. AHIMA offers a variety of education and training programs for certification, through conferences and webinars.
The AHIMA CHTS series includes the following six exams: Clinician/Practitioner Consultant (CHTS-CP); Implementation Manager (CHTS-IM); Implementation Support Specialist (CHTS-IS); Technical/Software Support Staff (CHTS-TS); Trainer (CHTS-TR); and Practice Workflow and Information Management Redesign Specialist (CHTS-PW).24
The next six sections are taken from the AHIMA web site: https://my.ahima.org/certification/getcertified.24
Certified Healthcare Technology Specialist-CP Exam (CHTS-CP)
The Clinician/Practitioner Consultant Examination conveys the background and experience of a licensed clinical and professional or public health professional. Workers in this role will:
• Suggest solutions for health IT implementation problems in clinical and public health settings.
• Address workflow and data collection issues from a clinical perspective, including quality measurement and improvement.
• Assist in selection of vendors and software.
• Advocate for users’ needs, acting as a liaison between users, IT staff, and vendors.
Certified Healthcare Technology Specialist-IM Exam (CHTS-IM)
Implementation Manager Examination demonstrates a candidate’s ability to provide on-site management of mobile adoption support teams throughout the implementation process of health IT systems. Prior to training, workers will have experience in health, IT environments, and administrative or managerial positions. Workers in this role will:
• Apply project management and change management principles to create implementation project plans to achieve the project goals.
• Interact with office/hospital personnel to ensure open communication with the support team.
• Lead implementation teams consisting of workers in the roles described above.
• Manage vendor relations, providing feedback to health IT vendors for product improvement.
• Apply project management and change management principles to create implementation project plans to achieve the project goals.
• Interact with office/hospital personnel to ensure open communication with the support team.
• Lead implementation teams consisting of workers in the roles described above.
• Manage vendor relations, providing feedback to health IT vendors for product improvement.
Certified Healthcare Technology Specialist-IS Exam (CHTS-IS)
Implementation Support Specialist Examination tests a candidate’s ability to provide on-site user support throughout the health IT system implementation process. Previous background in this role includes information technology or information management. Workers in this role will:
• Execute implementation project plans, by installing hardware (as needed) and configuring software to meet practice needs.
• Incorporate usability principles into design and implementation.
• Test the software against performance specifications.
• Interact with the vendors as needed to rectify problems that occur during the deployment process.
Certified Healthcare Technology Specialist-TS Exam (CHTS-TS)
Technical/Software Support Staff Examination assesses a candidate’s ability to maintain systems in clinical and public health settings, including patching and upgrading software. Candidate backgrounds include information technology or information management. Workers in this role will:
• Interact with end users to diagnose IT problems and implement solutions.
• Document IT problems and evaluate the effectiveness of problem resolution.
• Support systems security and standards.
Certified Healthcare Technology Specialist-TR Exam (CHTS-TR)
Trainer Examination conveys the ability to design and deliver training programs to employees in clinical and public health settings. Previous background includes experience as a health professional or health information management specialist. Experience as a trainer is desired. Workers in this role will:
• Be able to use a range of health IT applications, preferably at an expert level.
• Communicate both health and IT concepts as appropriate.
• Assess training needs and competencies of learners.
• Design lesson plans, structuring active learning experiences for users.
Certified Healthcare Technology Specialist-PW Exam (CHTS-PW)
This Exam portrays the skills needed to reorganize a provider’s work to effectively use health IT to improve health care. Candidates may have backgrounds in health care or information technology, but are not licensed clinical professionals.
Workers in this role assist in reorganizing the work of a provider to take full advantage of the features of health IT in pursuit of meaningful use of health IT to improve health and care. Individuals in this role may have backgrounds in health care (for example, as a practice administrator) or in information technology, but are not licensed clinical professionals. Workers in this role will:
• Conduct user requirements analysis to facilitate workflow design.
• Integrate information technology functions into workflow.
• Document health information exchange needs.
• Design processes and information flows that accommodate quality improvement and reporting.
• Work with provider personnel to implement revised workflows.
• Evaluate process workflows to validate or improve practice’s systems.
Chapter Review
This chapter described the evolution that has occurred in the HIT computer network environment in the past few years. This evolution has resulted in a much more complex environment that presents technical challenges in several areas that are mentioned in this chapter and described in depth in this new, second edition. Among the challenges introduced in this chapter are the need to navigate new and updated data standards intended to help the United States achieve interoperability in healthcare; actually achieving interoperability among the wave of new consumer health apps and devices; and improving security and cybersecurity in systems and devices to match the greater complexity of today’s network environment. The emerging IoT, more service-oriented architectures, and cloud services also present challenges in this new environment. This chapter also defined the workforce that needs to be prepared to meet these challenges. Finally, this chapter defined the roles of the major organizations that certify individuals for working in HIT.
Questions
To test your comprehension of the chapter, answer the following questions and then check your answers against the list of correct answers at the end of the chapter.
1. What has incentivized the uptake of healthcare information technology in the United States?
A. FDA regulations for drug manufacturing
B. The insistence of the U.S. population on identity management and quality
C. The financial incentives in the HITECH Act
D. The inability of paper-based charts to accommodate the volume of healthcare information
2. What is the Bureau of Labor Statistics estimated growth in the number of healthcare IT workers through 2018?
A. The growth is expected to increase by 20 percent through 2018.
B. There is no growth expectations for healthcare IT workers.
C. The growth is expected to increase by 50 percent through 2018.
D. A decrease is expected because there is currently a surplus of healthcare IT workers.
3. In recent years, what has added to the complexity in understanding healthcare information technology?
A. The challenge of maintaining privacy, confidentiality, and security in the widely expanding complex architecture
B. Greater access to healthcare data from multiple groups, including patients
C. The increase in mobile computing and the use of clouds for storage
D. All of the above
4. What innovations are driving new roadmaps, workflows, and algorithms in the delivery of healthcare?
A. Mobile health alone
B. Mobile devices, genetics, genomics, telehealth
C. Ever-increasing delivery of services via the Internet, including EHRs as hosted services
D. None of the above
5. Which U.S. government agency provides the regulatory framework for device manufacturers and importers?
A. NIST
B. FDA
C. AHRQ
D. NIH
6. What aspect of HIPAA security risk analysis covers cybersecurity for medical devices?
A. HIPAA currently does not include security risk analysis that covers PHI cybersecurity in medical devices.
B. HIPAA covers cybersecurity in the FDA regulations for medical devices.
C. The FTC covers the HIPAA regulations for cybersecurity for medical devices.
D. HHS covers cybersecurity for medical devices in its OCR regulations.
7. In what year did cybersecurity become a priority concern for healthcare organizations?
A. Cybersecurity has not become an issue for information technology for healthcare organizations.
B. Cybersecurity became a priority concern for healthcare organizations in 2011.
C. Cybersecurity became a priority concern for healthcare organizations in 2009.
D. Cybersecurity became a priority concern for healthcare organizations in 2015.
8. What event has led to the surge in cybersecurity threats to healthcare organizations?
A. The HITECH Act of 2009
B. The passage of HIPAA
C. The coordination of regulations from the FDA
D. The FTC changes in telehealth
Answers
1. C. The financial incentives in the HITECH Act have incentivized the uptake of healthcare information technology in the United States.
2. A. Employment of healthcare IT professionals is expected to increase by 20 percent through 2018, according to the Bureau of Labor Statistics.
3. D. Understanding healthcare IT has become more complex in recent years because of the challenge of maintaining privacy, confidentiality, and security in the widely expanding complex architecture; healthcare data has become more accessible to multiple groups, including patients; and mobile computing and the use of clouds for storage have increased.
4. B. Mobile devices, genetics, genomics, and telehealth are driving new roadmaps, workflows, and algorithms in the delivery of care.
5. B. The FDA is the U.S. government agency that provides the regulatory framework for device manufacturers and importers.
6. A. HIPAA currently does not include security risk analysis that covers PHI cybersecurity in medical devices. However, many devices include personal health information.
7. C. Cybersecurity became a priority concern for healthcare organization in 2009 with passage of the HITECH Act.
8. A. The HITECH Act of 2009 is the event that has led to the surge in cybersecurity threats to healthcare organizations.
References
1. Donaldson, S. E., Siegel, S. G., Williams, C. K., & Aslam, A. (2015). Enterprise cybersecurity: How to build a successful cyberdefense program against advanced threats. Apress.
2. Collins F. S., & Varmus, H. (2015). A new initiative on precision medicine. New England Journal of Medicine, 372(9), 793–795.
3. National Institutes of Health. (2017). All of Us Research Program: Precision Medicine Initiative. Accessed on January 24, 2017, from https://www.nih.gov/research-training/allofus-research-program.
4. Savage, N. (2014). Bioinformatics: Big data versus the big C. Nature, 509(7502), S66–S67.
5. McCormick, K. A., & Calzone, K. A. (2015). Big data initiatives: Genomics and information technology for personalized health. In V. K. Saba & K. A. McCormick (Eds.), Essentials of nursing informatics, sixth edition (pp. 707–725). McGraw-Hill.
6. Relling, M. V., & Evans, W. E. (2015). Pharmacogenomics in the clinic. Nature, 526(7573), 343–350.
7. Hoffman, J. M., Haidar, C. E., Wilkinson, M. R., Crew, K. R., Baker, D. K., Kornegay, N. M., & Relling, M. V. (2014). PG4KDS: A model for the clinical implementation of pre-emptive pharmacogenetics. American Journal of Medical Genetics Part C: Seminars in Medical Genetics, 166C(1), 4555.
8. DIGITizE: Displaying and integrating genetic information through the EHR. Accessed on October 14, 2016, from www.nationalacademies.org/hmd/Activities/Research/GenomicBasedResearch/Innovation-Collaboratives/EHR.aspx.
9. Robert Wood Johnson Foundation, Mathematica Policy Research, Harvard School of Public Health. (2012). Health Information technology in the United States: Driving toward delivery systems change. Accessed on January 25, 2017, from www.rwjf.org/content/dam/farm/reports/reports/2012/rwjf72707.
10. Henry, J., Pylypchuk, Y., Searcy, T., & Patel, V. (2016). Adoption of electronic health record systems among U.S. non-federal acute care hospitals: 2008–2015. ONC Data Brief 35. Accessed on January 24, 2017, from https://dashboard.healthit.gov/evaluations/data-briefs/non-federal-acute-care-hospital-ehr-adoption-2008-2015.php.
11. Office of the National Coordinator for Health Information Technology. (2016). Office-based physician electronic health record adoption. Accessed on January 25, 2017, from https://dashboard.healthit.gov/quickstats/pages/physician-ehr-adoption-trends.php.
12. U.S. House of Representatives Committee on Energy and Commerce. (2016). The 21st Century Cures Act fact sheet. Accessed on January 26, 2017, from https://energycommerce.house.gov/sites/republicans.energycommerce.house.gov/files/documents/114/analysis/20161128%20Cures%20Fact%20Sheet.pdf.
13. Accenture. (2016). Conceptualizing a data infrastructure for the capture, use, and sharing of patient-generated health data in care delivery and research through 2024. Accessed on January 25, 2017, from https://www.healthit.gov/sites/default/files/Draft_White_Paper_PGHD_Policy_Framework.pdf.
14. McCormick, K. A., Gugerty., B, & Sensmeier, J. (2017). A comparison of professional informatics-related competencies and certifications. Online Journal of Nursing Informatics, 21(1). Available at www.himss.org/library/online-journal-nursing-informatics-volume-21-winter-2017.
15. Perlin, J. B., Baker, D. B., Brailer, D. J., Fridsma, D. B., Frisse, M. E., Halamka, J. D., … Tang, P. C. (2016). Information technology interoperability and use for better care and evidence. Vital Directions for Health and Health Care Series. Discussion Paper, National Academy of Medicine. Accessed on October 12, 2016, from https://nam.edu/wp-content/uploads/2016/09/Information-Technology-Interoperability-and-Use-for-Better-Care-and-Evidence.pdf.
16. Office of the National Coordinator for Health Information Technology. (2011–2015). Federal health information technology strategic plan. Accessed on December 21, 2016, from https://www.healthit.gov/sites/default/files/utility/final-federal-health-it-strategic-plan-0911.pdf.
17. Bureau of Labor Statistics, U.S. Department of Labor. (2015). Medical records and health information technician. Occupational outlook handbook, 2015. Accessed on June 14, 2016, from www.bls.gov/ooh/Healthcare/Medical-records-and-health-information-technicians.htm.
18. Bureau of Labor Statistics, U.S. Department of Labor. (2015). Computer and information technology occupations. Occupational outlook handbook, 2015. Accessed on June 15, 2016, from www.bls.gov/ooh/computer-and-information-technology/home.htm.
19. Bureau of Labor Statistics, U.S. Department of Labor. (2015). Computer and information systems managers. Occupational outlook handbook, 2015. Accessed on June 15, 2016, from www.bls.gov/ooh/management/computer-and-information-systems-managers.htm.
20. HIMSS. (2016). 27th annual HIMSS leadership survey. Accessed on January 26, 2017, from www.himss.org/27th-annual-leadership-survey/full-report.
21. HIMSS. (2014). Nursing informatics workforce survey salary resource guide. Accessed on June 15, 2016, from www.himss.org/2014-nursing-informatics-workforce-survey-salary-resource-guide.
22. CompTIA®. CompTIA Healthcare IT Technician retirement. Accessed on June 15, 2016, from https://certification.comptia.org/certifications/healthcare-it-technician.
23. HIMSS CAHIMS certification. Accessed on June 15, 2016, from www.himss.org/health-it-certification/cahims.
24. AHIMA certification exam portal. Accessed on January 23, 2017, from https://my.ahima.org/certification/getcertified.
