CHAPTER 10
Fundamentals of Health Workflow Process Analysis and Redesign
J. Michael Kramer, Sheila Ochylski, Jane Brokel
In this chapter, you will learn how to
• Explain essential steps in design and development of a large electronic health record system and present an implementation method for large-scale process change
• Participate in the design of processes and information flows for clinical practice using engineering methods that accommodate evidence-based safety practices, quality improvement, and reporting
• Participate in developing within a healthcare system a sustainable plan for a revised and optimized clinical workflow that integrates professional practices and meaningful use of information technology
• Plan, analyze, and develop a process map for given clinical workflows within a complex healthcare system
• Critically analyze and document clinical and healthcare business processes by identifying gaps between current and desired states, areas of redundancy, delays, inefficiencies, work volume, task times, and elapsed times in order to redesign or optimize workflows
• Design, test, and implement information technology that supports effective teamwork, fosters open communications and care coordination, and enables shared decision making to achieve quality patient care
• Design and apply information technology and standardized practices that support documentation of compliance with applicable healthcare industry, regulatory, organizational safety, and quality standards
Implementing health information systems across an organization brings an unprecedented magnitude of change to that organization. This chapter reviews two major tools necessary to manage such change: process modeling and organization-wide change management. Before we discuss utilizing these tools, we will consider an important step in the life cycle of change. Traditional “project management,” discussed in Chapter 11, considers project closure as a phase of a change. At the project closure of a large-scale health information technology (HIT) implementation project, the team is often redeployed to other work, and the change is largely considered complete. However, the need to constantly apply new scientific evidence to clinical practice as well as frequent rapidly evolving healthcare accreditation, certification, and regulatory standards necessitates another approach. Sustained resources (certainly less than the large infusion of the many extra resources during the implementation project, but extra resources nonetheless) are necessary to sustain major HIT systems in an ongoing manner after the system has been implemented. Having the appropriate skills and teams to manage ongoing change is necessary to control the continuing work. Therefore, the concept of project closure per se is obsolete if organizations expect to leverage their newly implemented information systems to achieve higher levels of quality and safety.
Life Cycle of Major Information Technology Implementation and Organizational Change
To understand how health information technology can be managed, an appreciation for the larger context of change is necessary. As the United States implements electronic health records (EHRs) in every hospital and medical practice, EHRs become central to each organizations’ operations.1, 2, 3 Therefore, the responsibility and need to sustain systems in a practice or hospital does not end with the initial implementation. Each organization will choose how to support and maintain its systems differently with varying leadership models, teams, and reporting structures. See Chapter 18 for a more detailed discussion on governance.
No matter the model of support, we have observed a very clear life cycle in implementing EHRs across our combined experience in 35 hospitals and several large ambulatory practices. The phases of large-scale HIT change can be described as planning with analysis, implementation, stabilization, optimization, and transformation. This is depicted in the first row of Figure 10-1. Planning and implementation require a great deal of thorough analysis and traditional project management, which is clear to most organizations. The time it takes post-implementation to reset to new normal and stabilized operations, with productivity and other new EHR/transformation gains realized, is not always appreciated. In our experience, the movement from implementation to transformation varies across organizations. The characteristics, risks, benefits, and the HIT professional role with each phase are listed and further described in Table 10-1. Despite rigorous planning and thoughtful and careful implementation, there is still the risk of end-user workarounds and suboptimal benefits realization.
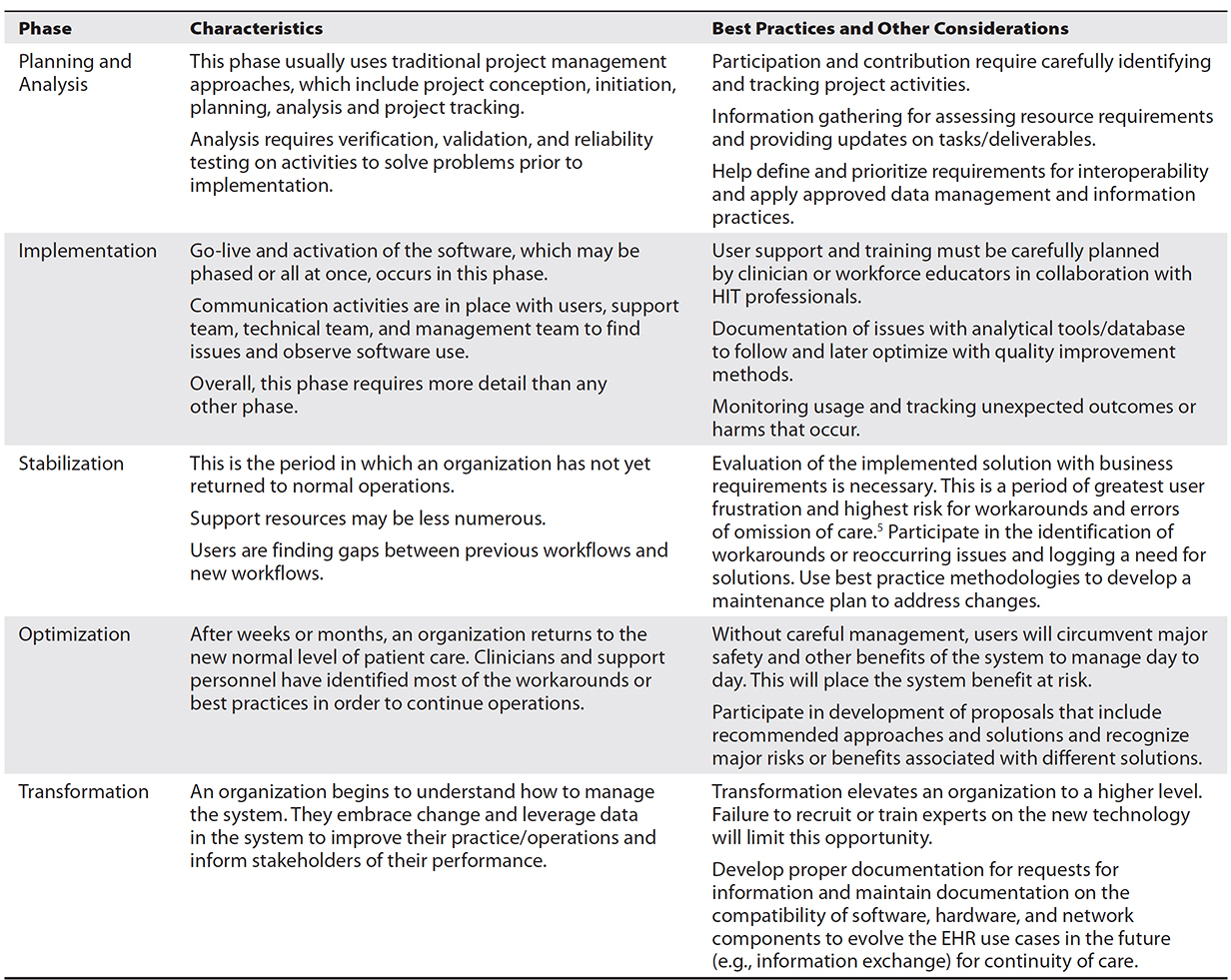
Table 10-1 Summary of the Life Cycle of Large-Scale HIT Change and HIT Role

TIP A workaround is a way to use the system in a fashion that was not designed or intended. Workarounds result in unplanned and unexpected outcomes.4 A physician might not find a lab test so instead enters an electronic order to the nurse with a typed comment to order the blood test. This workaround results in a delay in the lab completing the test because of the extra steps required for the nurse to clarify the order for completing the test.
In addition to the stages of implementation described in Table 10-1, Figure 10-1 introduces three additional organizational approaches to managing large-scale change that are illustrated in the second through fourth layers of the diagram: Layer 2: The Heart of Change—8 Steps to Successful Change, Layer 3: Continuous Activities, and Layer 4: Cycles of Communication. Large-scale organizational change management planning can reduce provider dissatisfaction, a prolonged stabilization phase, and a number of workarounds. Organizational change management is discussed further later in this chapter. Layer 2 is credited to Kotter and Cohen and provides a framework to develop four core activities that will help manage large-scale organizational change.6 Layer 3 with its four long arrows within the life cycle of change display how organizations must develop approaches to ongoing evolution and change in the system. These activities include maintaining the system knowledge base. Chapter 20 addresses the importance of maintaining and updating the system’s content (e.g., order sets, rules, and workflows) to stay current with advances in medical science, health regulation, and quality measures. Finally, with each change, organizations must maintain multiple cycles and methods of communication with all stakeholders. This is represented by the cogs in Layer 4 of Figure 10-1.6 Effective communication increases the awareness of the need to change, the understanding of the processes, the commitment to change, and the actions to achieve the desired changes and outcomes. These concepts are part of a theoretical model of change that is very helpful in creating a sequence of communications around major change.
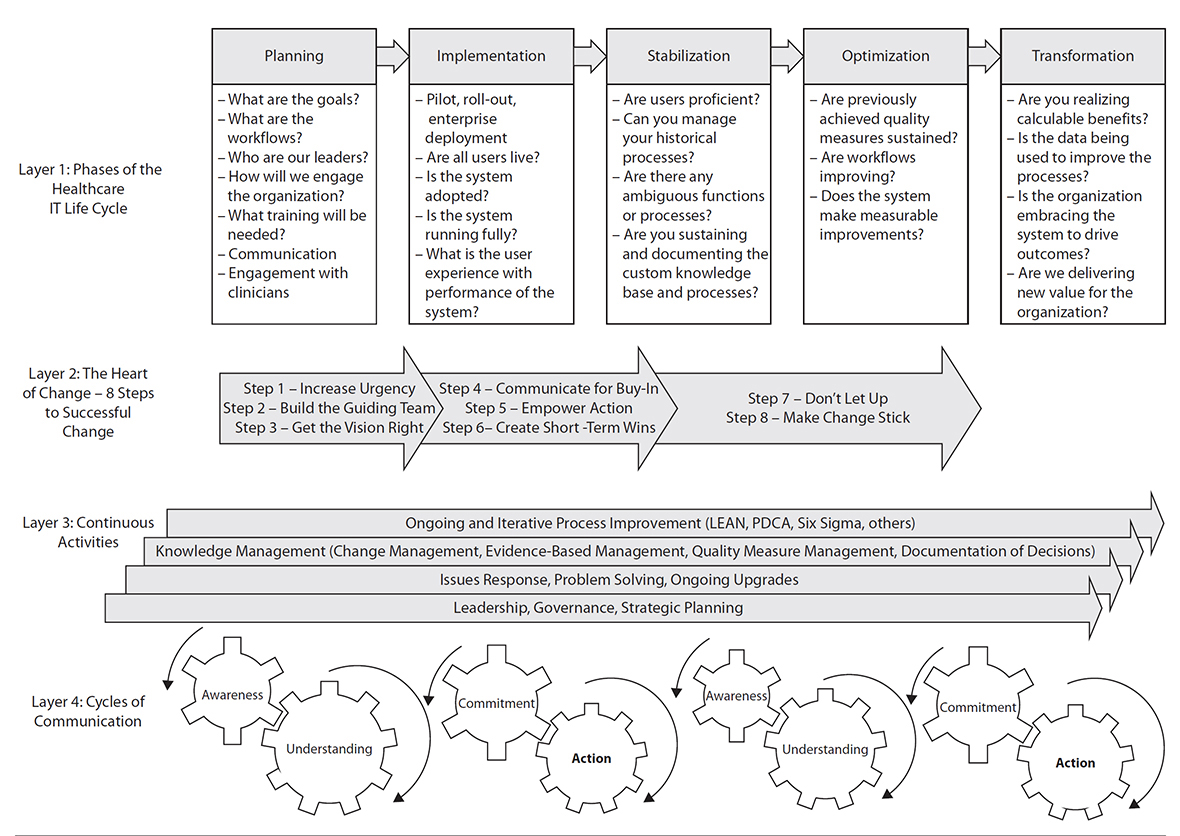
Figure 10-1 Activities across the life of a major healthcare IT implementation
Process Management and Process Improvement
When mapping processes for healthcare services, the opportunity exists to continuously improve patient care delivery by using safety and quality practices and reporting methods that are the best available based on scientific evidence. In this section we describe a process hierarchy for workflow analysis that HIT professionals can use to support stakeholders who are planning and implementing changes. A central theme to workflow analysis and redesign of care is keeping the patient and their information centered in the approach. This section discusses five levels of process mapping (see Table 10-2) that guide designers to consider the scope and standards of practice for key healthcare professionals, the accreditation and regulatory requirements, the Centers for Medicare and Medicaid Services (CMS) EHR meaningful use incentive program requirements, quality and patient safety goals, and new legislative requirements such as the Medicare Access and CHIP Reauthorization Act (MACRA).
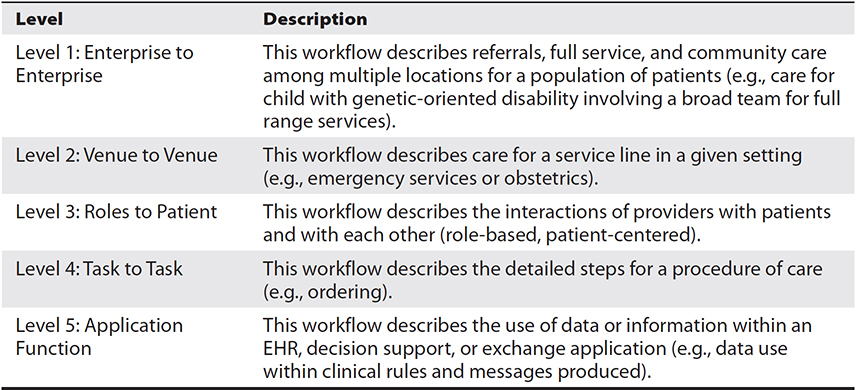
Table 10-2 Descriptions for Levels of Mapping Processes
Process Hierarchy: Levels of Mapping Processes
A process hierarchy for workflow analysis and design can be an effective approach to meet stakeholder needs in planning and implementing initial and ongoing changes. Stakeholders in this context include administrators, clinicians, department staff, and individuals who have specific tasks and functions.
Level 1: Enterprise to Enterprise
The first level is used by senior leaders who organize care among multiple settings for a population that will need full-service healthcare through community and referral providers. This first level is described as enterprise-to-enterprise mapping with a patient-centric viewpoint. This viewpoint ensures there are services available and that region-wide health information exchange of standard documents such as continuity of care documents—which include a patient’s problem list, medication profile, allergies, immunizations, and care plan—can enable sharing and movement of data between entities to accommodate the patient’s needs for holistic healthcare. This first level will capture the patient’s broad experience of moving in and out of provider venues and processes that support the clinical practice and patient needs, financial compensation and accounting, and public health obligations (e.g., immunizations, disease surveillance). Figure 10-2 illustrates what the patient may experience using healthcare services starting with the call for help and ending with a return home to self-manage their health.
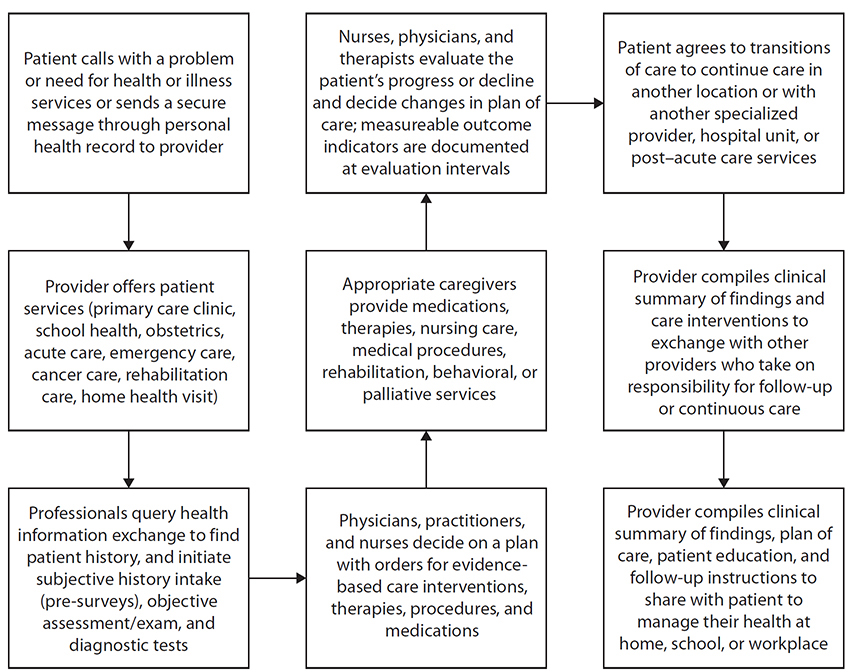
Figure 10-2 Enterprise-level processes for data, information, and knowledge use
Level 2: Venue to Venue
While patients perceive their care as being across visits and encounters with the healthcare system, many providers focus on care within one site such as a hospital or clinic. The second level in the leveled process mapping approach, venue to venue, consists of major service lines such as emergency, surgical, or oncology services. The service line director and clinical team are stakeholders who understand care delivery. This level proceeds from the first level by explaining the clinical processes the patient and family are involved in. Reuse of common processes reduces variation in the healthcare professional’s workflow, such as medication management that applies to most venues and all service lines of care. This standardization of process activities supports safety and quality across the service lines of care so that the process steps for medication ordering, medication databases with allergy or drug-drug interaction alerting (some medications interact with each other in patients such that the combination can be dangerous; drug-drug interaction alerting at the time of medication ordering is a HIT safety feature), medication dispensing, medication administration, and medication evaluation with documentation of therapeutic or side effects and adverse events are consistent and harmonized across the services.

TIP For a patient undergoing surgery, typical processes include registration, pre-admission testing activities, surgical and anesthesia preparations, intraoperative procedures with pathology examination for specimens, postoperative care, shift change or handoff activities, daily care coordination, transfer and/or discharge, quality monitoring and reporting, as well as hospitalist consultation, diagnostic radiology, laboratory, and pharmaceutical services. Viewing the delivery of care as a modular activity allows reuse of defined processes within multiple venues and across multiple scenarios.
Level 3: Roles to Patient
The third level involves engineering role-based workflows within the clinical processes identified at the second level. “Roles to patient” reflects the reality that in many healthcare delivery processes, even modestly complex ones, there are many different types of healthcare professionals and healthcare workforce members that interact interdependently with patients to throughput patients through the system while striving for optimal outcomes for patients. This level will assist healthcare workforce members, professionals, and managers/leaders to emphasize interactions with the patient while specifying multiple process and documentation requirements established by federal agencies and states who license physicians, nurses, pharmacists, therapists, and technicians. The HIT professional evaluates these processes as implemented to identify problems and changes needed by interacting regularly with the clinical professionals. The HIT professional may be asked to present plans for potential process change to these clinicians to optimize clinical practice to meet new demands for services related to evidence-based research or regulatory updates.
Continuing our example of the medication management process at the third level, this process is viewed in more specific detail as a person-to-person workflow where three or more professional roles interact to use patient data, information, and evidence-based knowledge for clinical decisions. One decision may include a physician’s order/prescription of a beta blocker for a specific patient’s diagnoses and whether the nurse is to administer the medication when the patient’s current vital sign assessments for blood pressure and heart rate are unstable (i.e., low). Does the existing technology used by the nurse allow visualization of current assessments in the medication administration record to support a decision to administer or not administer the medication at the scheduled time? Medications have therapeutic effects, side effects, and adverse effects that a nurse evaluates and documents before and after administering the medicine. Will the technology support or add extra steps for the nurse to ensure the medication can be given safely and according to evidence-based practices? As you will see depicted later in the chapter in the section “Role-Based Swim-Lane Workflow,” the third level is a patient-centered workflow with the patient’s role in the center of the swim-lane rows using a cross-functional flowchart.7 This workflow defines the steps in each role where the communication of data, information, and knowledge within professional practices flows seamlessly to ensure proper handoffs across shifts or on a daily basis to safeguard care continuously for a patient.

TIP Level 3 focuses on clinician interactions with patients within the workflow and addresses the following question: Does the clinician have access to the right information at the right time when performing functions such as medication administration, clinical treatments, or respiratory therapies?
Role-based workflows—such as those for physicians or nurses or pharmacists—identify the timely collection and documentation of patient information, providing access to the data for subsequent clinical decisions. In analyzing the workflow, HIT professionals need to account for each delay in getting information, potential gaps, areas of redundancy, manual work on the part of clinicians, work volume added to the clinician, task time to accomplish a process using the technology, and elapsed time between clinician process steps. Each of these could add to safety concerns, duplications in documentation of care or orders, or quality of care errors. Role-based workflows provide a framework for how EHRs are designed to manage information for decision makers and those coordinating care with other providers or departments. The availability of patient data and evidence-based knowledge resources (e.g., drug and disease databases, nurse procedure/intervention databases, cancer protocols) is necessary in the workflow to support clinical decisions and appropriate treatment steps. HIT professionals should focus on processes that are necessary in the clinicians’ roles when providing care and monitor for unintended consequences of change with an EHR when a clinician’s practice is not fully supported. An example of a gap is when a care practice to document the risk for aspiration and planned interventions is not possible within the EHR system and the care is forgotten or omitted. Solutions to avoid errors of omission include adding risks to the problem list, reminders, dashboards, templates, or other types of clinical decision support.5 Person-to-person and patient-centered service-line workflows minimize the stress and better coordinate the complex activities of implementations.8

TIP Standardizing the care process into modules and the various workflows (role-based person-to-person, task, and functional) is useful to transfer process knowledge from one setting to the next.
Communication of information can be accomplished via electronic methods, direct conversation, or paper methods. These person-to-person handoffs identify the professional’s scope of practice to care for patients, which includes their use of trended and aggregated information to evaluate patient status over time. The role-based (person-to-person) workflows use action verbs in the process steps (rectangles) to describe the activities each healthcare professional performs in a given venue (e.g., admission, clinic visit, surgery) (see Figure 10-3 later in this chapter). This workflow displays questions to describe which physician or nurse decisions (diamonds) have to be made (e.g., medication management, transfer, discharge). In the analysis of process mapping, action steps, decisions, and movement of information are identified and documented. This process is enhanced when healthcare professionals and workforce members participate in actively informing the workflow diagrams as they are created and revised. One technique often employed by HIT professionals is to ask many questions of healthcare professionals and workforce members about the process being depicted. Another technique is to “demo” (demonstrate) system functionality that could potentially support the clinical process being depicted in a more effective or efficient way. The interaction between healthcare professionals and workforce members and HIT professionals by these and other techniques can strengthen the quality of the workflow diagrams created and the eventual HIT functionality that the diagrams inform. Besides these level 3 diagrams’ primary use for designing/redesigning processes and workflows, the diagrams created at this level are used for training healthcare professionals and support personnel so they understand what the technology can and cannot do before any implementation. The workflow can avoid workarounds because the caregivers know how the technology is used or not used in the workflow to accomplish care activities.
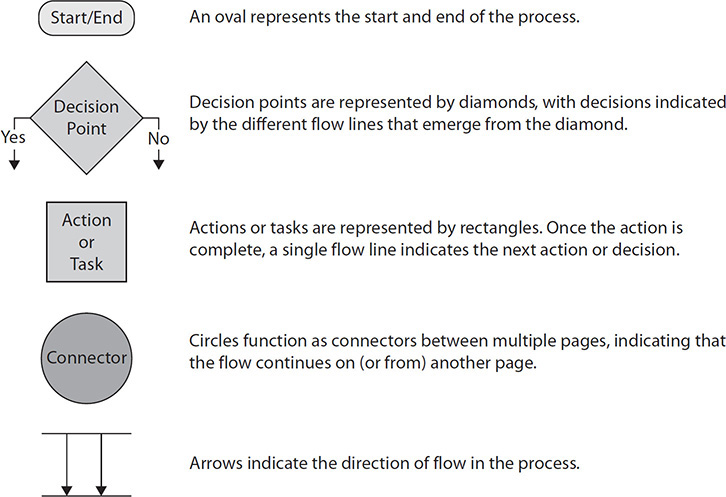
Figure 10-3 Graphic representation of workflow mapping
As an example, the nurse will see the nursing process steps displayed within the workflow and can relate nursing practice steps in their use of the EHR system. Randell et al. found that nurses are more likely to change their actions when they are involved and understand why the nursing process is better when using the EHR system.9 Physicians respond similarly when they know why a given step is important.3 This level of patient-centered cross-functional workflow provides a far better illustration of the steps for each role when working with patients.3, 7, 9
Level 4: Task to Task
The fourth level is task to task. At this level, the detailed use of a function is described. To illustrate, how does a physician order a radiologic test that requires pretest preparations and the holding of a medication prior to and 24 hours after the test? These workflows are modular in that they are specific to a task being completed by someone. This computerized ordering step can vary from other ordering processes, and therefore a task-oriented workflow provides the orientation to the additional steps necessary. These unique tasks are limited to a few professionals or support personnel to complete, while most others don’t require this level of detail.
Level 5: Application Function
The last and fifth level of workflow is described as application function. These workflows generally are modular and depict the functioning of the application itself, or HIT system, with little human or user involvement. For example, the EHR’s problem list may be used in several summary views, such as screen displays within the care planning function for nurses or ordering by physicians who need to link medications or interventions to conditions on the problem list. The application function workflow for this example would be very detailed and reference many modules and sub-modules of the application such as the care planning module and decision support module.

TIP The flow of information in an EHR application, such as clinical decision support applications (covered in more detail in Chapter 20), is typically more automated than paper-based systems and often requires less human interaction.
Workflow for a functional application has a very limited focus, such as clinical decision support or documenting allergies or supporting a specific decision. Although this workflow level lacks the perspective of care delivery, it is essential for achieving safety, avoiding errors, and meeting quality measures or regulatory requirements to share data.

TIP The person-to-person development of workflows displays time-oriented interaction and steps taken for all the interdisciplinary team’s processes occurring with patients.
Methodologies for Understanding Processes
There are several methods for understanding processes:
• Observation of current daily workflow
• Modeling workflow based on the formal scope of professional practice standards
• Simulation of the proposed workflow steps
• Quality-based deployment strategies such as Lean and Six Sigma
• Continuous workflow improvement with functional technology advances
Most organizations use business process management and modeling tools such as Microsoft Visio or others. Benefits and limitations for each method are described in the following pages. This discussion of methodologies for understanding processes is designed to help you critically analyze the workflow processes in a selected clinical setting, taking into account potential gaps, areas of redundancy, delays, inefficiencies, work volume, task time, elapsed time, and other factors.
Observation
Observation provides an opportunity to view settings and see various patient scenarios within each setting. This method is very good for understanding the task time, manual work, delays, and multiple variations that exist within care processes for a discipline. Observation is beneficial to highlight the typical time it takes to complete a task and to identify variations in practice among professionals. While there may be a good reason for variation, a common result is unnecessary cost and inefficiency. The Lean principle of Gemba is a tool to observe workflow. “Gemba” is a Japanese word that refers to the location where value is created. The principle behind “going to Gemba” (meaning the “place where the work is being done”) is commonly used by Lean experts. The foundation of this principle is to observe the actual process to get the facts and data.10
Modeling Workflows for Scope of Professional Practice Standards
A second method for understanding processes is modeling that is informed by the scope of healthcare professional practice. Data, information, and evidence-based knowledge are used to analyze clinical decision-making requirements.
Professional practice standards are sources to identify who, what, when, how, and where information is needed. Information technology professionals may not understand or appreciate the differences, unique responsibilities, and accountabilities for each of the healthcare disciplines that are central to patient services. The processes followed by each clinical discipline or role (such as medical assistant, nurse, or physician) are equally important to the patient’s care and treatment. As an example, the professional practice standards for pediatric nurses would be found in Pediatric Nursing: Scope and Standards of Practice, Second Edition,11 which outlines the practice for nursing assessment, diagnosis, outcomes identification, planning care, implementation of care, coordination of care, health teaching and health promotion, consultation, and evaluation in all settings and inclusive of the role of parents and family with pediatric care.

TIP Spending time with clinicians (or, “going to the Gemba”) as they provide care can help IT professionals appreciate the time and other resource constraints caregivers encounter and identify and take into account potential functionality or other gaps of the EHR .
Physicians examine, diagnose, and order medications and therapies to treat diseases and injuries or perform noninvasive or invasive procedures to improve a disease process or medical condition over time. Physicians can be specialized by the age groups they treat or in primary-care practice for all ages, while many more physicians focus on a specific body system such as cardiovascular, orthopedics, or psychiatry. (You can find more detail on care within and across venues and various medical roles and specialties roles in the appendix about healthcare professional and workforce roles. See Appendix C for how to access this content.) EHRs aggregate patient information and historical information along with drug and disease databases, laboratory, radiology, and other diagnostic references, and evidence-based guidelines to support physician decisions on diagnoses, plan for care, referrals, consultations, treatment, and follow-up. Table 10-3 describes processes and decisions for different healthcare professionals. When the EHR system lacks the ability to organize and aggregate pertinent data for a clinician or specialized practice, the professional frequently finds workaround alternatives to accomplish the same function and come up with a treatment plan individualized to the patient’s condition.

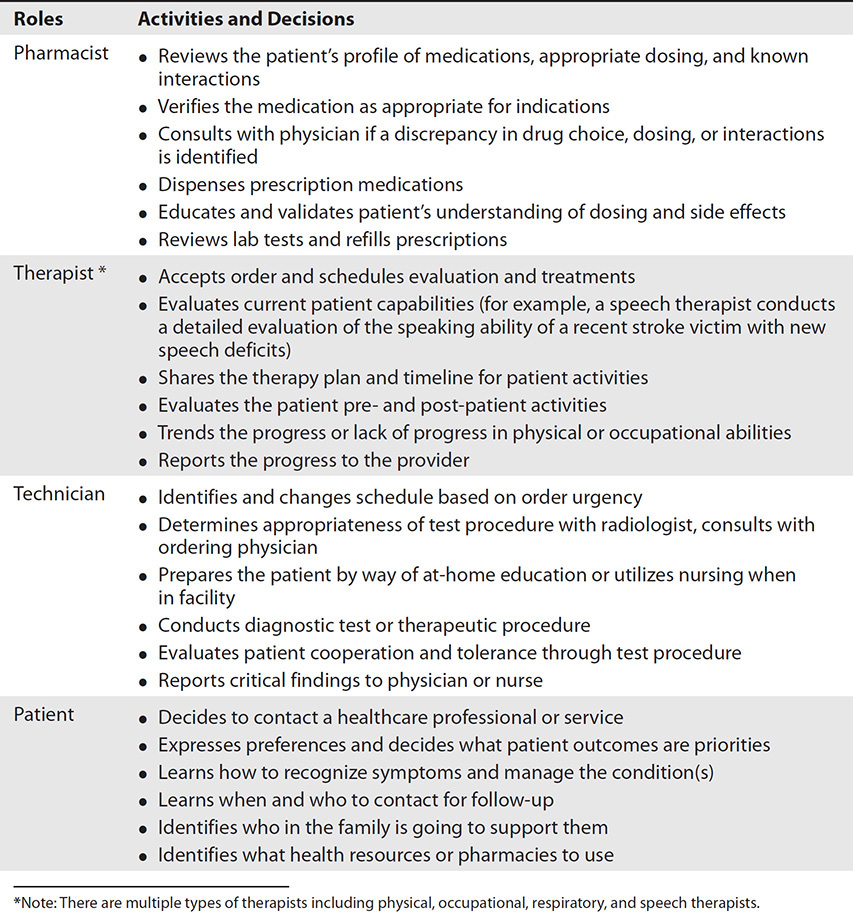
Table 10-3 Processes and Decisions in Scope of Healthcare Professional Practices and Patient Care
Nurses—the largest group of healthcare professionals in acute-care and other healthcare facilities—are often the main users of EHR systems, providing around-the-clock coverage for patients in a number of venues. Table 10-3 highlights the major activities of the nursing process and decisions for the patient. While physicians are usually responsible for the overall management of a given disease, the nurses typically carry out the recommendations made by the physician and also address a number of patient responses including fear, agitation, confusion, nausea, acute or chronic pain, impaired skin integrity (which can lead to pressure ulcers), impaired mobility (a risk for accidental falls), and a lack of knowledge about their condition. In addition, they watch for patients who might become suicidal or aspirate (accidental entry of food or stomach contents in the airway). Nurses develop and are responsible for implementing a plan of care with evidence-based interventions to prevent problems, avoid risks, and promote healthy lifestyle changes; they use evidence-based information for nursing decisions about care that is usually different from information that guides physicians. Finally, given the amount of time they spend with the patient, they tend to have a more holistic view of the patient’s care and observe/document the changes in patients.
Patients and their families have an important role in workflows because most information from assessments and ultimately the patient’s outcome is gathered from them. Table 10-3 highlights the patient’s role in learning about diagnostic results and changes in treatment activities. Any workflow that doesn’t include the patient is missing the most important stakeholder in patient care. Given the time they spend with the patient and their training and skills in collecting detailed assessments, nurses frequently obtain the information to evaluate the patient to detect positive and negative outcomes of a given treatment and communicate the changes to others.
Pharmacists are educated in helping physicians find the best medication options for patients and are responsible for verifying the safety of medications that patients will take. In some healthcare settings they directly communicate with patients about medications, while in other settings they indirectly communicate through others, such as nurses. Data are important to pharmacists because the age, gender, height, weight, pregnancy status, allergy presence or absence, genetic variants (e.g., P450 CYP2C9, resulting in slow metabolism of many medications), and patient’s condition(s) (e.g., problem list) are all relevant to safe medication dosing. Pharmacists and physicians rely heavily on laboratory results (e.g., creatinine and GFR for any kidney impairment; liver enzymes for liver impairment), vital signs, and other clinicians’ observations of signs and symptoms. Table 10-3 provides some scope of practice considerations for pharmacists.
Another broad category critical to the care of patients consists of the assorted therapies: dietitians, social workers, respiratory, physical, occupational, speech pathology, behavioral, and recreational professionals. Clinical professionals in these groups normally focus on a specific aspect of the patient’s care and, while normally autonomous, are typically involved and directed by physicians. Examples include treatments aimed at increasing a patient’s mobility; optimizing their diet; and respiratory function support with ventilators. Table 10-3 provides some scope of practice considerations for therapists.
Technicians within laboratory, radiology, neurological testing, cardiovascular diagnostics, and other areas need information to prepare patients for a test or diagnostic exam and to ensure safe transport to perform the tests. A key responsibility of these healthcare workforce members is prompt reporting of the results and timely notification to nurses and physicians when the findings are critical because these findings can dramatically alter the course of care and treatment for the patient. Medications will influence how and when a test is conducted, so many technicians need to know what medications the patient is taking.
Simulation
HIT technology simulation can provide a safe testing environment that allows practitioners to test new clinical processes using simulation of the technology before implementing with patients. Many simulation applications involve artificial “patients” and “providers” that can test tasks and functions to simulate care and treatment, like flight simulators used by pilots.12 The simulation environment provides a real-life opportunity to evaluate clinical and management information systems such as EHRs, secure messaging, and interactions with health information exchange networks in a realistic environment within the safety confines of a controlled artificial environment. Research using simulation approaches helps inform the design and development of electronic systems. The HIT professionals can facilitate testing opportunities using EHR simulation applications collaboratively with clinicians to view and further optimize healthcare processes prior to implementation.
Lean Strategy
Lean/Six Sigma principles and methods have been used extensively in manufacturing and production lines to identify the most efficient production practices using less costly resources and fewer tasks while still achieving optimal value for customers. Since 2005, the Lean strategy has been widely adopted in U.S. healthcare. Good examples of this work have been published by Toussaint and Gerard, including significantly decreasing “door-to-balloon” time (“door” referring to emergency room door and “balloon” referring to balloon angioplasty, a common treatment for heart attacks) for heart attack patients at two hospitals from 90 minutes to 37 minutes.13 The goal when using the Lean approach is to eliminate waste or redundancies in practices while providing the best possible patient outcomes.14 Examples of waste in healthcare include waiting, overproduction, overprocessing, defects, needless motion, excessive inventory, inefficient transport, and underutilization of healthcare workforce member skills.
The Lean methodology is also very useful to engage clinicians in increasing their sense of ownership of important changes.15 Often clinicians cannot see how broken their processes are until a methodology like Lean is applied. Such a methodology can break down resistance to change when facilitated properly. In general, that usually means the safest care at the lowest cost with the shortest stay and no complications (i.e., eliminating unnecessary tests and complications, hospital-acquired infections, pressure sores, injuries from falls, etc.). When Lean strategies are fully leveraged, the result is optimal outcome for the patient with less work volume and minimal to no redundancy in care. Most quality improvement professionals and clinical informaticians have advance training in one or more of these techniques and tools.

TIP When workflow is optimized, human interactions with the technology increase efficiency, decrease waste, and rely on scientific methods to decide which data are relevant rather than accepting prior methods, often based on paper or that were unique to an individual clinician.
The Lean approach poses critical questions to subject matter experts in a process undergoing improvement. These questions are helpful in identifying what matters most and avoiding the distraction of variation and waste. These who, what, where, how, and why questions highlight gaps, variations, unnecessary tasks, and redundancy in current practice and allow the clinical team to decide the safest and quickest ways to get to equivalent or better patient outcomes.
Business Process Management
Business process management (BPM) uses select engineering principles and practices to represent processes for the healthcare enterprise. BPM in healthcare settings often involves clinical informaticians and service-line leaders working with HIT professionals and business process managers or quality managers to analyze and improve current processes. Process improvements are part of everyday activities in healthcare and are useful to achieve meaningful use of HIT. HIT professionals should identify and work closely with business analysts and quality improvement staff members who are involved with improving practices for accreditation and certification. When planning to revise and optimize clinical workflow within the healthcare organization, EHR systems and HIT allow combining data analytical techniques yielding actionable insights on the organization’s clinical and business data with evidence-based research from outside the organization that can result in significantly improved processes.
Healthcare organizations and clinics should designate someone who is accountable for managing a central database of process maps/workflows. Management of workflows facilitates decision making regarding when and where workflows apply, allows for the reuse of standardization workflows across service lines, and allows for the continuous optimizing of healthcare processes (workflows).
Workflow Mapping Tools
A structured approach enabled by standard visualization artifacts and understandable diagrams can aid efficient and effective problem solving and decision making. Figure 10-3 is an example of the basic tools associated with process mapping. Specific shapes correspond to different types of activities performed to visually represent workflow. The shapes are quite straightforward given the simple explanations in Figure 10-3. The diamond shape, as it can be used in different ways, needs a bit more explanation to understand how it is typically used in workflow diagraming. Diamonds signify a decision-making process, usually resulting in two possible workflow directions. Most diamonds reflect a yes or no decision that has to be made; if the decision is yes, the workflow continues on the intended route, but if the answer is no, the workflow may have to go through another route to solve the problem.
Swim-lane diagrams, discussed in an upcoming section, often reduce the need for mapping roles and tasks.
Workflow Diagram Example
A workflow diagram, or map, is a graphic depiction of a course of action showing the steps in a process to accomplish a goal. Many work processes can be complex, so it is important to visually represent in detail how tasks are being completed to improve understanding and efficiency. Depending on the purpose of the map, it can be high level (abstract) or detailed. Figure 10-4 is an example of an enterprise high-level clinic visit workflow diagram to represent steps to obtain historical information on medications/allergies from the health information exchange for the patient and the patient’s flow through the clinic.

Figure 10-4 Clinic visit workflow
Role-Based Swim-Lane Workflow
Figure 10-5 is an example of a mid-level role-based swim-lane workflow. Role-based swim lanes describe who is responsible for each stage, what documentation is needed, and the relationship to resources at each stage. Knowing employee roles and resource requirements allows management to easily determine weaknesses and alleviate bottlenecks. A bottleneck represents any aspect of the workflow that impedes overall cycle time of the process.
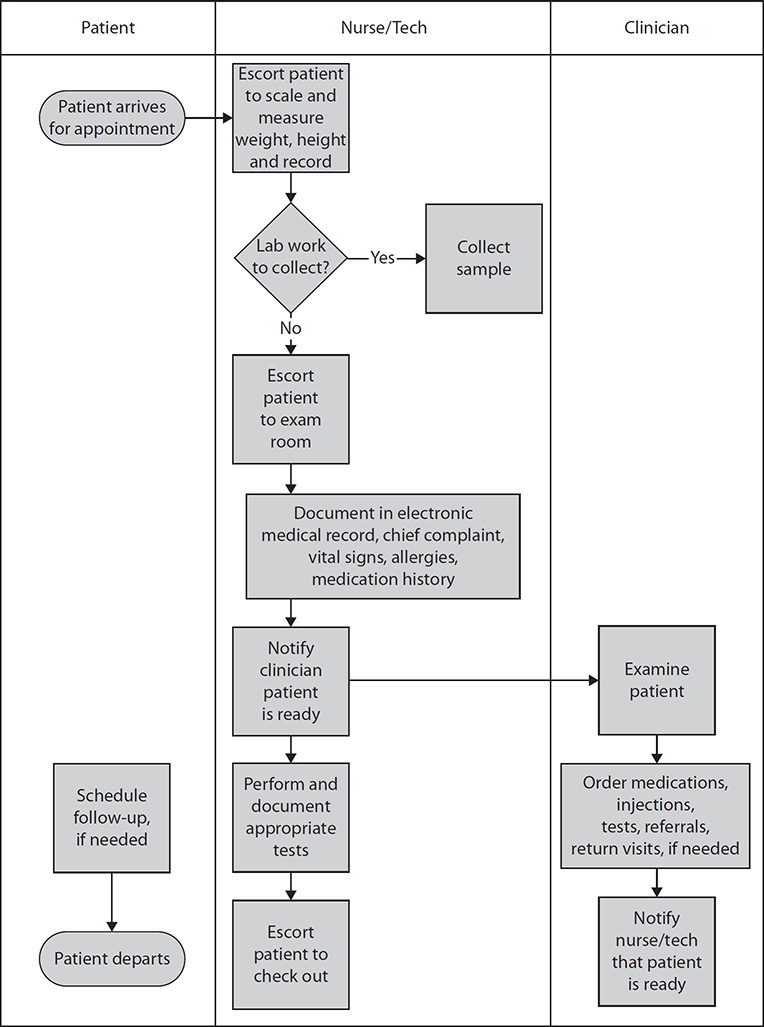
Figure 10-5 Clinic visit role-based swim-lane workflow
Value Stream Mapping
Figure 10-6 shows a value stream map. Value stream mapping is a type of process mapping or flowcharting of the value stream, which includes all of the steps (both the value-added and the non-value-added steps) in producing and delivering a service. A value stream map shows workflow from a systems perspective and can help in determining how to measure and improve the system or process of interest. Without a view of the entire stream, it is possible that individual aspects of the system will be optimized according to the needs of those parts, but the resulting total system will be suboptimal. Value stream mapping in healthcare is typically done from the perspective of the patient, where the goal is to optimize the patient’s journey through the system. Information, materials, and patient flows are captured in the value stream map. The key question to ask when determining whether an activity is value added is if the customer would be willing to pay for it. If the answer is no, the activity is not value added. In healthcare, an example of a non-value-added activity is waiting time. Value stream mapping is a recognized Six Sigma methodology.10
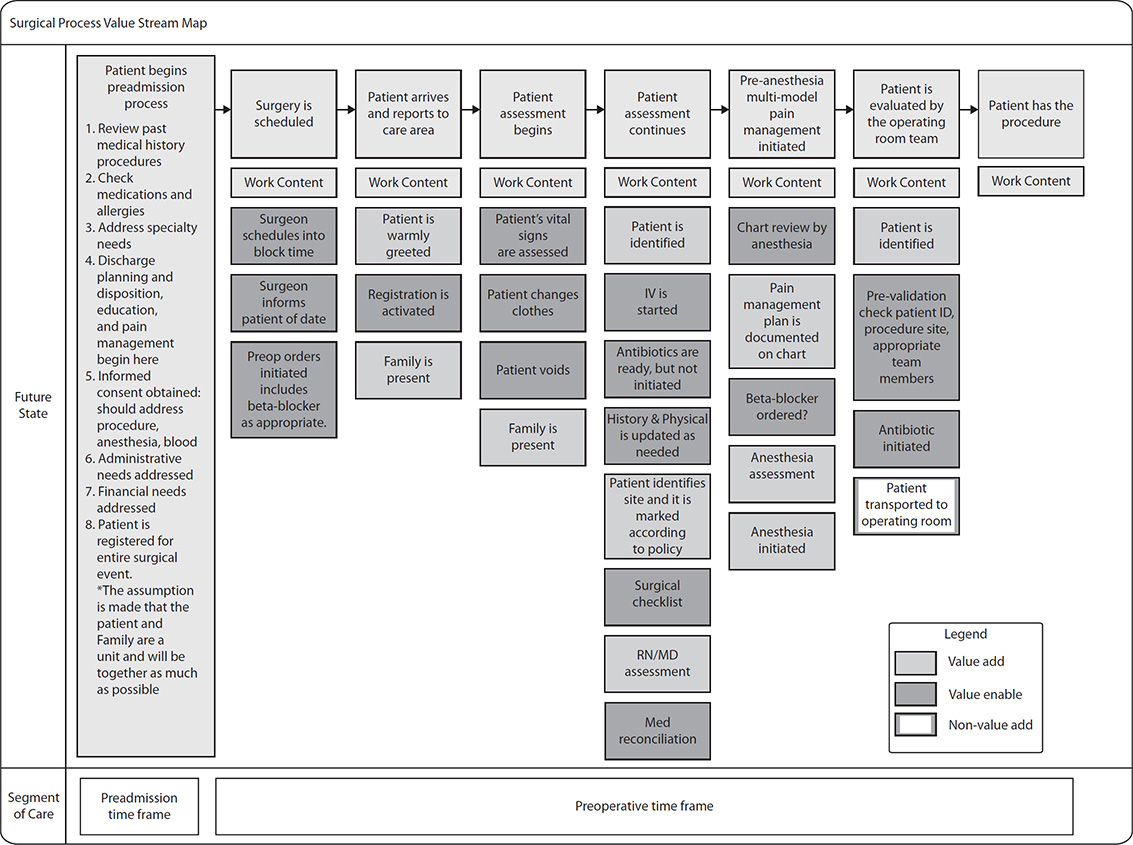
Figure 10-6 Value stream mapping
Success Factors for Implementing Clinical Process Change
Designing and applying information technology using standardized practices can be an extensive, time-consuming process. When possible, leverage the vendor’s standardized tools and process descriptions. When these are not suitable, incomplete, or need to be extended, you must assemble a process change team with the right skill sets, as well as subject-matter experts. A moderate-sized hospital may have 200 to 300 third-level process flows. A typical ambulatory clinic may have 50 to 75 process flows. It is useful to name each of the processes and assign a priority to map these processes explicitly. One question to ask is: Is this process well defined? If not, it may require a higher priority to determine a possible future state. Complex and ambiguous processes typically create a great deal of confusion, concern, and even risk to the patient during implementation of a new or substantially changed information system or EHR. The ideal implementation has no ambiguous processes at go-live. A knowledge manager assigned to track and manage these processes can minimize the risk. These individuals may also be experts in identifying potential gaps and facilitating problem-solving events or in managing gaps within the vendor-supplied content or by other means without existing technology support.

TIP Use the SIPOC (suppliers, inputs, process, outputs, customers) Six Sigma tool shown in Figure 10-7 to simplify problem solving or to plan a large process change event. A SIPOC form identifies all aspects of a process, including the beginning, the end, and all high-level steps in between. Outside of the core process, you should also identify suppliers and customers. This high-level description can be used before a more detailed process improvement activity is used.
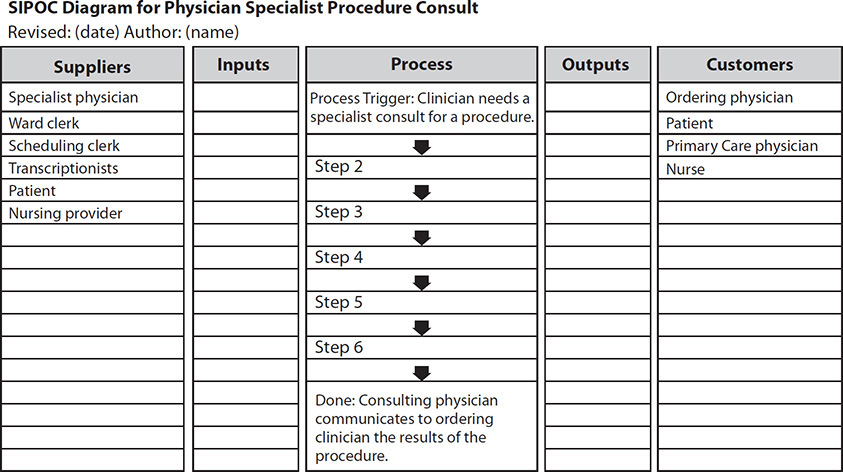
Figure 10-7 SIPOC chart for planning workflow mapping or problem-solving event
The implementation of the actual new steps represented in a workflow diagram is the hardest aspect of process change. Organizations often do not realize the importance of understanding processes and mistakenly rely instead on technology to resolve problems. With paper-based records, many organizations had thousands of individual order sets, many unique to specific physicians and frequently outdated. With computerized physician order entry (CPOE), most organizations appreciate the need for standardization in workflow and reducing variation among physicians. Organization-wide recognition of process improvement is imperative, and leadership support, understanding, and communication of the reason why change is necessary are key;3, 9 simply posting a workflow diagram on a nursing unit won’t significantly impact day-to-day activities. Most workflow diagrams should include a workflow improvement strategy such as Lean, Six Sigma, or Total Quality Management as well as clear instructions on how to follow them and practice the steps.
Exercise 10-1: Create a Simple Process Model Using the SIPOC Tool
In this exercise, review Use Case 10-1, and develop a process model and overview.
1. Describe the steps in the process, including trigger and completion.
2. Identify inputs into the process.
3. Identify desired outcomes.
4. Develop a plan to engage customers and suppliers in the future state process design.
5. Advanced: After completing a process map, enhance the map by utilizing role-based swim lanes or a value stream approach.
6. Advanced: What measurement could you use to determine that the new process is being used and not a workaround?
Use Case 10-1: Physician Consult for Specialty Procedure
Mrs. Hurst is a 35-year-old woman who presented to her primary-care physician with early-onset high blood pressure. In the office she was found to have signifi-cant high blood pressure without a strong family history or other explanation. On examination, she had evidence of an abdominal bruit (an abnormal sound heard with a stethoscope over the abdomen and a sign of a narrowed renal artery). The primary-care physician treated the patient with blood pressure medications and ordered an abdominal ultrasound that identified a condition called renal artery stenosis. Since her blood pressure did not respond to multiple medications, the primary-care physician consults a specialist vascular surgeon who could enlarge the renal artery using balloon angioplasty.
The doctor recently started using an EHR and is unsure how to order for this patient situation and how to share the continuity of care document (CCD) with the consulting specialist through the health information exchange network. Is this an “order” like one might write for an X-ray, or is it a consult for the specialist to see the patient and then determine the appropriate course of action? Previously, the physi-cian would communicate the intent to the nurse or office manager who would man-age the details of such a workflow. Unfortunately, the physician and office manager do not know how to order the same consult or potential resulting procedure using the new EHR. After calling the supervisor superuser (an individual with additional training) and the EHR implementation team, everyone involved realizes that they had not developed a process to manage this type of problem. The implementation team needs to develop this process and communicate it to all involved quickly. While the team works on defining and implementing an electronic version of the paper process, the office returns to the previous method of handwriting the order and faxing it and the physician’s visit notes to the specialist office. In addition, as the patient is at risk of losing a kidney, the office manager, following the direction of the physician who anticipates the vascular surgeon will agree with the need for renal angioplasty, calls the hospital surgical scheduling clerk, who enters the request into the surgical scheduling system.
Additional Techniques
When workflow processes are viewed in isolation, they often appear quite logical and efficient enough to accomplish the end goal. When viewed more broadly across multiple disciplines, complexities arise. Frequently missed are conflicts in the priorities of different roles in an organization (e.g., tasks that nursing is accountable for versus the pharmacy).
The suggested steps for creating a process map or workflow are as follows:
1. Assemble a stakeholder planning team. The team should consist of individuals from all clinical areas and all levels with the goal of ensuring the true process is captured.
2. Determine the level of detail desired, the methodology you will employ, and the participants needed (e.g., value stream mapping, role based, SIPOC, or simple diagramming). The level of detail will depend on the problem the team is addressing and the number of handoffs between disciplines.
3. Schedule the mapping event for the team with HIT professional support and obtain the appropriate supplies.
4. Begin the event by giving the team sufficient background on the approach you will be using. Provide initial training in the weeks before or at the start of the event.
5. Complete the mapping event. Identify the activities in your current and future state. List them and arrange them in order.
6. Create a formal chart with standard symbols for process mapping using Microsoft Visio and Excel to track questions to follow up on with the EHR technology capabilities and gaps.
7. Create an accurate picture, and check for accuracy.
8. Identify problem areas and gaps between the current and future state.
9. Prioritize projects that will address the gaps.
Identification and Prioritization of Targets for Workflow Improvement
Information technology should be designed to support effective teamwork, foster open communication, and enable shared decision making to achieve optimal, quality patient care. Once the process is mapped, gaps between the current process and best practices will become apparent. Members of the team with the most detailed understanding of the best practices can recognize gaps and highlight them for the team. A simple approach to ranking gaps using two dimensions includes “ease of implementation” and “value to the organization.” Value should be defined early in the life cycle of the program. Three common primary objectives for many organizations are safety, quality, and overall patient experience, with financial and provider experience as secondary benefits.
Change Management
Change management describes a structured approach to transition individuals, teams, and organizations from a current state to a desired future state. Considered an organization imperative, change management helps employees cope with and adapt to the numerous changes every industry faces. One reason change initiatives fail is because they rely on data gathering, analysis, report writing, and presentations while not adequately factoring in human motivation, evidence-based research, political, and symbolic elements.
John Kotter, a leading thinker and author on organizational change management, describes an eight-stage model for understanding and managing change.6 Kotter defines change management as the utilization of basic structures and tools to control any organizational change effort. Change management refers to a set of basic tools or structures intended to keep the change effort under control. Ultimately, the goal is to minimize the impact on workers and avoid distractions.
Change Management Principles
Four principles for change management are as follows:
• Elicit support from people within the system (system = environment processes, culture, relationships, and behaviors, both personal and organizational).
• Understand the current state of the organization.
• Understand where you want to be, when, why, and what the measures will be.
• Communicate, involve, enable, and facilitate involvement from people, as early, openly, and completely as possible.
Kotter’s Eight Steps to Successful Change
Kotter’s eight-stage approach to realizing significant change includes the following:
1. Establish a sense of urgency Inspire people to move, and make objectives real and relevant. Build a compelling case for change, and assess change readiness of stakeholders.
2. Build the guiding coalition Put the right people in place with the right emotional commitment and the right mix of skills. Engage sponsors in change leadership and team development to build competence and trust.
3. Develop a vision and strategy Create a team to establish a simple vision and strategy and focus on emotional and creative aspects necessary to direct the change effort.
4. Communicate the change vision for buy-in Involve as many people as possible, communicate the essentials simply, and respond to people’s needs. Declutter communications; make technology work for you rather than against you.
5. Empower action Remove obstacles, and enable constructive feedback and support from leaders. Reward and recognize progress and achievements, and encourage risk taking.
6. Generate short-term wins Set aims that are easy to achieve. Recognize and reward people who made the wins possible. Finish current stages before starting new ones.
7. Don’t let up Foster and encourage determination and persistence, and encourage new projects, themes, and change agents.
8. Make change stick Reinforce the value of successful change via recruitment and promotion, and develop new change leaders. Weave change into the culture.
Chapter Review
Ignoring or inadequately understanding workflows can lead to a decline in use of the EHR over time and the development of workaround steps. Workarounds can include both those within and outside an automated process. Analyzing workflows can help discover key factors to success: underuse and misuse of the EHR, workarounds clinicians find to collect or use patient information, and the need for aggregated information or reports to be available for decision making and sharing beyond the organization (often via health information exchange [HIE]). Working together, HIT professionals as members of an interdisciplinary team must review existing clinical workflows when technology upgrades or the clinical evidence advances to make necessary adjustments. Creating a culture focused on process and change management and understanding workflow will help guide organizations through new technology implementations and inevitable upgrades.7, 8
Questions
To test your comprehension of the chapter, answer the following questions and then check your answers against the list of correct answers at the end of the chapter.
1. Which of the following describes a way of using health information systems in a manner not originally designed, resulting in unplanned and unexpected outcomes?
A. Workflows
B. Workarounds
C. Tracking issues
D. Flowcharts
2. Which of the following are life-cycle phases of large-scale health information technology changes?
A. Workflows with workarounds and testing the technology with users
B. Planning, implementation, quality monitoring, and improvement
C. Planning, training, testing, implementation, and closure
D. Planning, implementation, stabilization, optimization, and transformation
3. Healthcare services are organized by many service lines of care such as surgical or obstetrical (i.e., maternal-child) services. Within each service, processes are organized such that they can be replicated across many services. Which of the following does not describe the healthcare general processes within venues of healthcare services?
A. Registration, admission, daily care coordination, shift change, discharge
B. Surgical preoperative visit, surgery, postoperative, same-day discharge
C. Registration, dining, coding, billing, reporting
D. Check-in, laboratory testing, radiology test, chemotherapy infusion visit, depart
E. Emergency triage, registration, assessment, examination, education, discharge
4. The role-based (person-to-person) workflow describes processes by which of the following?
A. Using swim lanes to show the roles
B. Describing steps in the process (rectangles) with action verbs
C. Organizing into venues for care (e.g., admission, clinic visit, surgery)
D. Displaying physician or nurse decisions (diamonds)
E. All of the above
5. Which workflow best describes the clinical scenario of a nurse sending a secure message using the health information exchange network to a home-care provider on research protocols which involve medication administration at very specific times for three days in the patient’s home setting?
A. Functional or application workflow
B. Role-based workflow
C. Enterprise-to-enterprise workflow
D. Venue-to-venue workflow
E. Task-to-task workflow
6. Which is a method to articulate the tasks, time, manual work, delays, and multiple variations that exist within care processes for a discipline or with a reporting process associated with many departments?
A. Modeling workflow based on scope of professional practice standards
B. Simulation
C. Observation of daily activities
D. Lean strategy, Six Sigma, and continuous improvement
E. Business process management and modeling tools
7. The HIT professional is involved in the analysis of workflow processes. Which of the following is not a list of roles, responsibilities, and tools of the HIT professional to accomplish this analysis to avoid workarounds and to find solutions?
A. Provide updates on tasks/deliverables; document issues within analytical tools/database to follow; monitor usage and track unexpected outcomes of harms.
B. Define and prioritize healthcare requirements and standards for care within the workflow; provide strategies to best use technology to efficiently retrieve and document clinical processes; know the healthcare standards for safety and quality requirements for clinical practice.
C. Evaluate implemented solution with business requirements for interoperability; develop documentation requests for information and maintain documentation on the compatibility of software, hardware, and network components to evolve the EHR use cases in the future (i.e., information exchange) for continuity of care; apply approved data management and information practices.
D. Identify and track project activities; participate in development of proposed recommended approaches and solutions; recognize major risks or benefits associated with different solutions.
8. Kotter provides steps to help achieve successful organizational change. Clinicians are generally accustomed to making evidence-based practice change when new research advances practice on how to detect and diagnose, to test for problems or risks, or to initiate with new interventions or procedures. The change associated with electronic health records must mirror the level of constant change to ensure evidence-based practices are implemented sooner rather than later. Which one of the following least describes this level of systematic change?
A. Quality improvement strategies: identify the focus, plan the solution, do the change, study the change through measurement, take action to implement the solution, and reinforce the value of successful change via recruitment and promotion.
B. Establish a sense of urgency, build a team with the right people, develop a vision and plan, communicate this, reward and recognize ideas and risk taking, set aims to easily achieve, encourage new projects with change agents, and reinforce the change.
C. Build a compelling case for change, identify a team with mix of skills to create direction, share the direction and listen for feedback, remove obstacles, generate short-term wins, encourage determination and persistence, and use change agents to weave change into the culture with successful change.
D. Assess change readiness of stakeholders, engage sponsors, develop team competence and plan a clear direction, declutter communications, empower action, recognize wins and don’t let up with new project work, and make change stick with change leaders.
Answers
1. B. A workaround is a way to use the electronic health records, other information system, or paper-based alternatives in an unintentional way. A common example is the use of nursing communication orders in place of actual departmental orders to communicate the need for a specific test. A delay occurs while the nurse contacts the physician to determine and place the correct order, with the continued risk of miscommunication. The department misreads the test and completes the test incorrectly, resulting in invalid results, and the patient needs a repeat test for diagnostic accuracy.
2. D. In summary, with large-scale HIT change, the stakeholders are involved from project conception with planning; implementation; feeling a sense of normalcy within the clinic or hospital (stabilization); optimizing practices; and embracing the change and fully using the data to determine performance to advance practice with transformation.
3. C. Processes within most venues have a well-defined start and endpoint and include a number of service lines during the episode of care. This option does not include any processes for care delivery, whereas the others depict general processes to consider where patient data and information are being collected from the patient and used to plan and deliver care.
4. E. All four answers describe how workflow is designed to display the steps and decisions within a process for those with a role in taking care of patients.
5. E. Task-to-task workflows provide additional detailed steps for less frequent activities that might occur during care delivery (e.g., a patient involved in a research study). In this scenario, the task-to-task workflow represents a process step beyond the hospital setting to ensure an intervention is coordinated between the physician, nurse, and home-care provider. When the health information exchange network is utilized to share information, the enterprise-to-enterprise workflow will work to share the patient’s plan of care through a continuity of care document, but the uniqueness of a research study makes this a task-to-task workflow.
6. C. Observation of workflow will help identify some gaps, the time involved, and delays, but this method alone will not help clinicians and IT professionals in discerning all potential interactions and gaps in practice workflows.
7. B. Central to the role of clinicians (not HIT professionals) is to define and prioritize healthcare requirements and standards for practice within the workflow; provide strategies to best use technology to efficiently retrieve and document clinical processes; and know the healthcare standards, safety, and quality requirements for clinical practice. Each healthcare professional must ethically and legally provide care according to their state’s or country’s (if outside of the US) professional practice act and their scope and standards of practice for their specialty practices. HIT professionals would not be expected to fully understand the scope of practice for each clinical discipline or their respective specialties.
8. A. Often, systematic and cultural change requires more than quality improvement strategies because the change needs to be at an organizational level and systematic. The consequences of one change can impact the practices of others and therefore a team approach with multiple skill sets is needed to plan, measure, and implement changes.
References
1. Blumenthal, D. (2009). Launching HITECH. New England Journal of Medicine, 362, 382–385.
2. American Recovery and Reinvestment Act of 2009 (ARRA). (2009). Accessed on June 17, 2010, from http://frwebgate.access.gpo.gov/cgi-bin/getdoc.cgi?dbname=111_cong_bills&docid=f:h1enr.pdf.
3. Sittig, D. F., Longhurst, C. A., Russo, E., & Singh, H. (2015). Electronic health record features, functions, and privileges that clinicians need to provide safe and effective care for adults and children. In C. A. Weaver, M. J. Ball, G. R. Kim, & J. M. Kiel (Eds.), Healthcare information management systems: Cases, strategies, and solutions, fourth edition. Switzerland: Springer International.
4. Halbesleben, J. R., Wakefield, D. S., & Wakefield, B. J. (2008). Work-arounds in health care settings: Literature review and research agenda. Health Care Management Review, 33, 2–12.
5. Piscotty, R. J., Kalisch, B., & Gracey-Thomas, A. (2015). Impact of healthcare information technology on nursing practice. Journal of Nursing Scholarship, 47(4), 287–293.
6. Kotter, J. P., & Cohen, D. S. (2002). The heart of change: Real life stories of how people change their organizations. Harvard Business School Press.
7. Brokel, J. M., & Harrison, M. I. (2009). Redesigning care processes using an electronic health record: A system’s experience. Joint Commission Journal of Patient Safety and Quality, 35, 82–92.
8. Brokel, J. M., Ochylski, S., & Kramer, J. M. (2011). Re-engineering workflows: Changing the life cycle of an electronic health record system. Journal of Healthcare Engineering, 2, 303–320.
9. Randell, R., Mitchell, N., Thompson, C., McCaughan, D., & Dowding, D. (2009). Supporting nurse decision making in primary care: Exploring use of and attitude to decision tools. Health Informatics Journal, 15, 5–16.
10. Wheeler, D. J. (2004). The Six Sigma practitioner’s guide to data analysis. SPC Press.
11. American Nurses Association, National Association of Pediatric Nurse Practitioners, and Society of Pediatric Nurses. (2015). Pediatric nursing: Scope and standards of practice, second edition. Nursesbooks.org.
12. Agency for Healthcare Research and Quality (AHRQ). (2012). Improving patient safety through simulation research. Accessed on June 19, 2012, from www.ahrq.gov/qual/simulproj.htm.
13. Toussaint, J., & Gerard, R. (2010). On the mend: Revolutionizing healthcare to save lives and transform the industry. Lean Enterprise Institute.
14. Lawal, A. K., Rotter, T., Kinsman, L., Sari, N., Harrison, L., Jeffery, C., …Flynn, R. (2014). Lean management in health care: Definition, concepts, methodology and effects reported—Systematic review protocol. Systematic Reviews, 3, 103.
15. Rother, M., & Shook, J. (2003). Learning to see: Value stream mapping to add value and eliminate muda. Lean Enterprise Institute.
