CHAPTER 23
Big Data and Data Analytics
John E. Mattison
In this chapter, you will learn how to
• Identify some of the best opportunities for innovation
• Define a taxonomy of exponential technologies and data sources in the multiplatform ecosystem, or Plecosystem™, that enable accelerated innovation
• Describe the likely impact of several powerful new innovations on the healthcare system
• Understand how harnessing and converging multiple exponential technologies and data sources across different platforms captures big opportunities for innovation
• Examine how current gaps in healthcare represent the best opportunities for the creative reconstruction of healthcare through innovation
Some of the best opportunities for the creative reconstruction of healthcare through innovation are described in this chapter. It is often useful to look through the lens of “where is there friction?” and “what frustrates you in your work?” from the perspective of both those who give and those who receive healthcare. A useful mantra is to “convert frustration into innovation.”
In this chapter, emerging technologies in the context of their respective roles in creating sustainable solutions for big data and analytics will be discussed. It is increasingly true that combining or converging different technologies or disparate data plays a key role in crafting new solutions. It is also apparent that we are experiencing exponential growth of many technologies and data sources across many platforms and that we can benefit by a deliberate consideration of the resulting multiplatform ecosystem, or “plecosystem.” The concept and taxonomy for the plecosystem continues to evolve and constitutes a useful way to create more comprehensive solutions to novel problems. As many of these exponential technologies have leveraged open application programming interfaces (APIs), more usable interfaces, and open source code bases, they have become much more accessible to people with little or no software programming experience. The implications for the future of the human experience, let alone the future of healthcare information technology (HIT), are profoundly and increasingly disruptive.
This chapter will also explore a variety of opportunities and technologies, but suffice it to say that three of the more important game-changing platforms for the next five years will be artificial intelligence (AI), robotics, and virtual reality/augmented reality (VR/AR). In 2008, the first “app store” was created and now “there’s an app for everything.” In 2016, virtual reality became a commoditized reality that creates an opportunity to create “a VR for everything.”
It would be negligent to begin a chapter on innovation in healthcare without first highlighting the central role that virtual reality will play in the immediate future. After paying homage to that currently emerging disruptive platform of today, VR/AR, this chapter will describe a taxonomy for innovation and then define some of the opportunities and disruptive innovations. Chapter 24 will then provide further examples of specific innovations in healthcare that require a multisystem platform such as genetics/genomics, mobile applications, and telehealth.
Innovation in Healthcare IT: The Creative Reconstruction of Health and Wellness
Nearly anyone alive today has the prospect of having a global impact.
–Steven Kotler, 2016
Despite abundant literature on innovation, much confusion remains about the systematic structure and process of innovation. The most prevalent problem is that simple ideation is often mistaken for innovation. True innovation usually requires the full life cycle from ideation, human-centered design, iterative evolution of usability, operationalization, commercialization of a minimum viable product (MVP), scale with widespread adoption, and then continuous improvement through iteration and expanded scope of services with each new version.
While an occasional “breakthrough” emerges out of the concentrated focus and interdisciplinary participation in a conventional “hackathon,” many factors often conspire to frustrate the successful transition from ideation to implementable innovation, including each of the following: the complexity of the human experience, the journey through health and disease, the cross-disciplinary solution sets required, and a highly regulated and litigious environment where fault tolerance is minimal. In addition, innovation often requires different approaches within small tech startups versus larger tech companies, although both generally benefit from collaboration with strategic partners or potential clients. Similarly, innovation within healthcare institutions often requires strategic partnering with multiple tech companies, arrayed across the plecosystem.
There are many pitfalls to healthcare institutional innovation programs for either products or services, and it is essential to consider strategies to minimize those risks. These pitfalls and mitigation strategies have been discussed elsewhere.1
One of the critical elements of impactful innovation is to first identify an important problem to solve. Clever solutions to small problems that affect few individuals may be “cute,” but the same creative energy, applied to a more important problem, could generate much more benefit, and a substantial revenue stream (or cost savings or new services) to support a new round of innovation. The good news is that the “programming constraints” for many of the newest disruptive technologies have been falling rather than rising.
It is also instructive when forecasting the future to recall an innovation truism and admonition known as Amara’s law (coined by Roy Amara): “We tend to overestimate the effect of a technology in the short run and underestimate the effect in the long run.”
Which Technologies Are Creating Big Opportunities for Innovation?
The list of technologies contributing to innovation continues to grow. Social, mobile, analytics, and cloud constitute a powerful quadriad of tools. However, they do not inherently address the real opportunity of the human-machine interface. While the predominant high-capacity input to the human brain is visual, we cannot neglect any of the other senses which also play reinforcing roles. The “killer technology” for that interface must leverage the foundational input/output (I/O) capabilities of the human experience (not just the I/O of the brain, but the emotional, social, psychological, and spiritual receptiveness of each individual to the I/O mediated through the brain, recognizing that there is variable volatility in each of these dimensions of human interaction). The single concept that most closely captures this I/O capability is the use of multiple n-dimensional avatars. We need provider avatars that represent sources of coaching, mentoring, and motivating individuals that resonate with the receptiveness of each individual at any moment in time. It is critical to realize that the receptiveness of an individual varies throughout the course of the day and the course of their life and is shaped by the emotional tone, social milieu, recent experience, and evolving sociocultural, community, family, and household norms. Personal avatars (for both providers and individual persons and their inevitable social network of avatars) must negotiate that complex context for each individual on a dynamic basis.
Further, we need tools that help us understand what communication modality and communication style and content are most effective to motivate an individual for a specific task toward a specific objective. We need deep learning to constantly mine the digital exhaust of the interaction between provider avatars and patients to continuously refine the approach and the context-sensitivity of the interaction. We need to instrument and implement real-time adjustments to how our provider avatars extend the reach of the care-delivery system to each individual person, while advancing the situational awareness of evidence-based information (how/when/what/how often/what medium/what sequence/what frequency/what time of day/what current emotional tone/what current social context) as the various motivational tools (“motivicons™” and a “motivational formulary™”) are applied as a sequence and as an ensemble. These provider or health mentor avatars will be more effective to the extent that they are coherent with emerging community and cultural behavioral cues toward better health.
Ultimately, the convergence of evolving community and social health elements with those of personal contextual health coach avatar activities will create what may be termed the “behavioral symphonies of wellness, empathy, and resilience™” which help maintain and reinforce healthy behaviors. There are many ways to achieve these goals, and there are decades of innovative discovery and implementation ahead about who responds best to the avatar mentor of their mother or daughter versus a cartoon character dog or cat versus a celebrity from sports or other celebrity arenas. There is a need for a strategy for how we match which avatar to which task in which individual and maintain an avatar milieu that conforms to the constraints of human cognitive and emotional capacity. We also need to recognize and manage to both the individual temporal and the inter-individual variability of that human cognitive and emotional capacity. It is quite likely that different people will benefit most from goal-specific avatars; for example, an avatar of a granddaughter might be the best way to motivate a grandmother to quit smoking, while an avatar of a senior Olympics sports celebrity might be the best way to help her become more active. This same principle of contextual personalization applies to how different social networks will be more or less effective for different objectives in different people; for example, a social group that helps support smoking cessation will often be different than a group that helps with exercise or weight loss. Increasingly and as a direct consequence of liberated communication and travel in the digital world, we all belong to a complex intersecting array of communities, each of which contributes significantly to the attitudes, behaviors, actions, and outcomes of each one of us, within our personal array of communities.
There are also personal avatar(s) that represents each one of us in our whole life experience, including aspects that reflect health, disease, and resilience. Amazon’s Echo open source platform is but the first primitive step toward a commoditized consumer avatar. The designers of Siri will soon release the next generation of extended capabilities, and every large consumer tech company is aware that these services will be a critical conduit for marketing and ad revenue, so investment and competition will increasingly intensify. Google home is another version of this type of service/product. A recent consortium of these groups was formed to collaboratively address the ethical issues and best practices, and deserves very close oversight for full social transparency.2
Ultimately, much of the contextualization and dynamism of how health provider avatars interact with individual people will be brokered by “dynamic digital handshakes” between the provider avatars and the personal avatars to render the most appropriate output in support of that individual’s implicit/explicit goals in ways and at times that find that individual most receptive to that motivational influence. For example, motivating someone to perform a difficult task should be withheld temporarily until after that individual recovers from an acutely traumatic emotional experience. These are not distant eventualities but are emerging today, and there are many projects in stealth mode that will begin to replicate the digital “second life” experience in real time and pervasively throughout our life experiences to the extent that we find them useful and convenient.
How Do We Optimize the Human-Machine Interface?
The previous section characterized the role of avatars as digital abstractions of individuals, providers, and social networks, and explored their potential opportunities for improving each individual’s health journey. In a world where information overload is pervasive, and where individuals find solace in unconsciously constructing “digital echo chambers” where they preselect only what they want to hear and from whom they want to hear it, there is a fundamental challenge of overcoming both the ambient noise level and the implicit/explicit filters that individuals have constructed as very blunt instruments to screen out all but what they think they want/need to hear. Our overriding design goals in the human-machine interface must recognize the criticality of contextualizing the interaction to the individual in ways that do not appear as “more noise” and don’t get whacked by the blunt filters constructed by that individual. The best model for how to do that and for how to “get inside people’s heads” historically has been the elicitation of empathy through characters in novels and movies, and now includes more sophisticated digital gaming and VR. The avatar interactions between providers and individuals must exploit the science and art of entertainment to create compelling messaging that penetrates the conscious and unconscious filters for each individual.
While visual and audio media are most pervasive, we will increasingly witness the evolution of robotic devices that can deliver motivational emotional tone and sensory inputs beyond sight and sound. The Stanford University Virtual Human Interaction Lab has developed a science and products that allow individuals to experience “physical transfer,” where they can observe themselves real-time as a “third person” in their VR visual field.3 Early findings suggest that modifying the image of that physical transfer can also result in the person maintaining a strong identity with their virtual representation, even as that representation morphs. The potential to overcome implicit biases by recognizing one’s self as being that “other” entity which evokes the implicit bias are profound.
“Augmented empathy” through physical transfer of virtual reality scenarios is an incredibly exciting opportunity for growing the capacity of individuals and communities to break down bias and more broadly accept and support their communities. One of the remaining large challenges in AI and AR is referred to as “collaborative robotics” or designing robots to safely and effectively interact with humans, who are so unpredictable. Machine learning will allow robots to better anticipate human behavior, and similarly generate “social learning” between robots, and perhaps even between multiple AI personas within individual robots. The invention of Baxter is beginning to show promise for safer human-robotic interactions. Baxter is replacing many of the manual functions in industry.4
How Do We Accelerate Continuous Learning and Innovation?
New technologies and new business models will continue to disrupt every business vertical. It is widely accepted that education and healthcare are the two industries most ripe for such disruptions. The productivity of a population depends critically on the health of its citizens, and our ability to create and sustain advances in health outcomes relies heavily on better educational methods and outcomes. Our current educational systems have increasingly declined on both absolute and relative benchmarking scales. It is disturbing to note that concomitant with the decline in education (and the rise of individual debt from education), many metrics of innovation show a steady decline over the past several decades, with a range of speculation as to underlying causes. Most people find that decline to be counterintuitive with the obviously great innovations resulting in Google, Facebook, Twitter, Lyft, Airbnb, and so forth. However, those are the conspicuous exceptions to what otherwise appears to be a steady decline in the number of people directly participating in the innovation economy. One metric of that decline is the rise in social inequity in advanced economies like that of the United States. There is an emerging literature on how to address the decline in innovation through disrupting our educational systems with technology and restructuring of curricula.5
Two of the more critical disruptive technologies to accelerate learning in healthcare (and in general) will be virtual reality and augmented reality. The ability for individuals to practice various tasks, techniques, and approaches repeatedly and feel the result of their actions (through advanced haptics) will revolutionize training, certification, credentialing, privileging, and ultimately health outcomes. VR and AR allow for this training at far lower cost than physical alternatives. VR and AR will hopefully generate more meaningful jobs than the low-skilled jobs increasingly replaced by AI/robotics. A global rise in disintermediation of people performing simple tasks otherwise threatens economic and political stability through underemployment, unemployment, and the associated consequences of social inequity and unrest.
Much of the human experience is based on learning. Learning involves transfer of new knowledge from short-term to long-term memory. There are five chemicals in the brain known to affect the efficiency of that transfer: oxytocin, dopamine, endorphins, anandamide, and serotonin. It is now known that a virtual reality experience can stimulate each of these. The VR industry is aggressively studying how to optimize the levels of all five of them in a VR experience to optimize not only the pace of learning but the experience of pleasure during learning, since each of these naturally active neurochemicals induces a pleasurable state.
The Department of Defense (DoD) has already demonstrated that various training programs using VR can accelerate learning 2.4 times over any pre-existing method.6 The implications for these recent discoveries is that we are on the cusp of transforming learning and education across all fields, and healthcare is perhaps more in need of better learning paradigms than any other.
A Simple Taxonomy for Innovation
There are many published taxonomies for innovation.7,8 A simple approach includes four types of innovation, as described in the following sections.
Disruption and disintermediation of old tools, jobs, and processes with new ideas, tools, and business models
This is the least common type of innovation, but when successful can generate the most dramatic progress. Augmented reality is perhaps the next successor in this disruptive series.
Incremental optimization of people, process, and technology
This type of innovation is the most pervasive and critical element of “blocking and tackling” after the introduction of a new technology. The vast majority of benefits from the introduction of electronic health records (EHRs) derives from this continuous, laborious, and collaborative form of optimization of both workflow and usability.9,10 The same can be said of many of the IT innovations in healthcare.
Identify and spread local successes
This type of innovation, which includes methods such as identifying positive deviance11,12 and hotspotting, is the most widely neglected. Numerous superb innovations remain trapped within a local context until identified as useful, and then packaged, productized, and diffused with implementation guides and effective change management. Some form of commercialization is often required, and indeed many companies have emerged from the local imagination, innovation, and implementation by the founder(s) of that company.
Cultural transformation
Cultural transformation is the most difficult of the four types of innovation and requires leadership with maturity and wisdom for how to change attitudes, values, and behavior at scale. The clearest example of cultural transformation in healthcare is the accountable-care organization (ACO) movement. Historically, Kaiser Permanente was founded on an ethos and culture of integration and value optimization across the continuum of care, which has been continuously improved and extended over many decades and generations of leadership.13 In contrast, the migration from a fee-for-service culture to one of maximizing value, rather than widgets of reimbursed work, is a critical requirement for success in the current value-based ACO movement. There has been a failure to appreciate the primacy of powerful and wise leadership to drive this cultural transformation. It is difficult enough to integrate previously isolated services and venues of care or to provide digital integration of those sites. However, the cultural transformation necessary to succeed in that transition to value-based care dwarfs the organizational and technical challenges. That transformation can only be executed effectively by leaders who know how to translate the values and motivate change through localized narratives adapted to each affected community engaged in the new synthesis. The creative reconstruction of healthcare represented by ACOs has faltered largely for lack of the exceptional leadership required. Failure to meet this requirement is the “silent killer” of many ACO initiatives.
The Different Communities Engaged in Healthcare Delivery
There are three different communities that are engaged in healthcare delivery leading to innovations:
• Individual persons within their communities and cultures
• Professional caregivers, oftentimes working in teams
• Personal caregiver networks
Person-Centric Communities
First, it is important to recognize that traditional Western healthcare, while consuming massive resources, only addresses 10–20 percent of the factors that contribute to leading a long, healthy life.14 Epidemiologic research reveals that communities with exceptionally long, healthy lives have four features in common: healthy diet, exercise, sufficient sleep, and social interaction. These finding emerge from the study of five communities with long healthspans and lifespans and are called “Blue Zones.”15 We have understood the benefits of healthy diet, exercise, and sleep for many years, and over the past decade the evidence supporting the social impact on health has dramatically increased.16
Traditional healthcare IT innovation has made huge strides in treating disease. The larger opportunities for creative reconstruction of health and wellness reside in our ability to apply innovative design and new technologies to help reverse the habits that collectively create disorders of lifestyle, which in turn are driving the epidemics of obesity, diabetes, and the directly associated rise in cardiovascular disease, cerebrovascular disease, cancer, and most forms of dementia, including Alzheimer’s disease.
HIT experts have a key role to play in addressing the behavioral economics, early childhood experiences, and social determinants of health from a collaborative community perspective where healthcare and HIT professionals participate, catalyze, and at times lead these efforts.17 There is indeed a role for technology to play and abundant opportunities for innovation, but we must truly embrace the broader root causes of disease or we will neglect the larger opportunity to build health and resilience into our communities and reduce the prevalence of disease. We are beginning to witness a concerted focus on ensuring healthier and safer early childhood experiences and a collaborative leadership of community resources to address the many aspects that can positively impact the social determinants of health.18 While these are largely sociocultural, political, and even generational issues, there are critical opportunities for the use of technology to support and reinforce those positive cultural vectors.
While these simple steps are somewhat obvious, it is remarkable how many local initiatives neglect key elements that are necessary for success. More importantly, there are many opportunities for innovative technologies to support each and every step of this process during planning, execution, and building sustainability. These evidence-based steps must also be iterative as each community evolves and learns, and as the palette of available technologies and resources evolves.
Professional Care-Delivery Teams
A growing chorus of voices laments the problems of usability in electronic health records and the growing work associated with the digital in-basket, even to the point of slogans like “It’s the in-basket, stupid.” Unfortunately, the in-basket workload is just a symptom of a deeper disease in digital healthcare. Just as in treating symptoms of disease, treating usability of EHRs and in-baskets will only address a small portion of the underlying problem afflicting physicians, which is fundamentally an increase in transparency into care gaps generated by the rise of digital data while disorders of lifestyle continue to wreak havoc on our communities. We have created an exponential growth both in the science of health and disease and in our ability to quantify health and disease in every individual. While both sets of information are valuable, we have not yet delivered commensurate services to transform the collision of those two large, complex sets of information into simplified actionable knowledge.
Rather than simplifying care, the barrage of data has mostly shined a spotlight on previously unseen care gaps without a corresponding increase in our ability to address those gaps. This problem is amplified by a legitimate emphasis on focusing on “value-based care” where measurable care outcomes are increasingly incentivized. Every director of quality has a mission to raise the bar on the practice of medicine and thereby compounds this growing chasm between the transparency of problems versus the constraints upon efficiently resolving those problems. It should not be such a mystery that many physicians are experiencing burnout at historic levels. This is especially true when our toolkit for healthcare is focused on disease care, whereas the root causes reside much deeper in our behaviors as individuals and in our social fabric. Setting aside the sociocultural issues for a moment, we clearly need a sophisticated set of tools that simplifies and facilitates each of the following tasks:
• Simplify the reconciliation between each individual’s digital health footprint with the exponentially growing science of medicine and behavior. These personal digital footprints have been referred to as either “the quantified self” or “N of 1.” These terms have acquired a large footprint themselves.
• Deploy “deep learning on the fly” with global searches of “practice-based evidence” to match individuals with a cohort that most closely resembles each individual to learn which approaches to intervention are most appropriate for that individual based on the outcomes of different treatment options previously applied to a cohort of similar individuals.
• Efficiently identify the values and objectives of the individual within their individual, sociocultural, familial, and household contexts. We need better survey instruments to more effectively elicit and elucidate both implicit and explicit values and objectives that represent the soil into which we can plant and fertilize the behavioral changes that are appropriate and realistic for that individual to pursue. “Noncompliance” is a physician-centric construct that often disguises a failure to create solutions that are practical and sustainable within a broader sociocultural and value-based context. When a person with diabetes is “noncompliant” with their behavioral or medical prescriptions because they have undiagnosed or untreated depression, this is not a failure of compliance by the patient, it is a failure of the caring profession to identify, understand, and address the comorbidity of depression. Further, the depression may result from the fact that the person has a husband in jail and a teenage daughter who is pregnant. Treating her diabetes is not at the top of her priorities, and treating her depression requires social services in concert perhaps with an antidepressant.
• Effectively use visualization tools to array the alternative approaches to closing those gaps while exposing the differences between options in ways that reflect the values and objectives of each individual. Simple facets of that array can include each of the following:
• Potential benefits
• Potential risks
• Behavioral and environmental changes required to support that option
• Opportunities to leverage support networks within their social milieu
• Level of effort required for behavioral change and ability of and support for the individual to commit
These visualizations must elucidate alternative options in ways that are readily accessible to each individual in the context of their basic literacy, health literacy, and ability and willingness to own and participate in their own health outcomes. Underlying those visualization tools must be access to the underlying knowledge sets, personal data, and the algorithms that connect those big data with little data. Individuals with different levels of literacy need to be able to drill down through the supportive data to understand their options to the extent they are capable of understanding (within their basic literacy and health literacy), within both sets of data (their personal health data and the larger knowledge base of health sciences).
• Leverage effective metrics and remote monitoring for progress against goals. There is a well-known element of “wearable monitoring fatigue” where digital nannies like Fitbit have a high attrition rate. We have observed for many years that the notion of a digital nanny is doomed and that we need to substitute a different behavioral model whereby we use digital monitoring for three objectives:
• Initiate desired behavioral changes
• Sustain motivation
• Calibrate progress against goals periodically
Products such as MUSE and from companies such as HeartMath have adopted this philosophy and approach.
One method for shifting from the model of a digital nanny to one of mindfulness is to progressively increase the time period between checking the data (e.g., steps taken) to reinforce the internal motivations toward health, while using the digital technology for calibration of those efforts toward more mindfulness. Other behavioral tools including gamification, personal health avatar coaches, and so on will assume increasingly powerful roles as motivation toward positive change. These tools need to be applied in a personalized, evidence-based approach that is subject to continuous machine learning and adaptation.
The coordination of care across the continuum of care and the “warm handoffs” required between services have been elaborated extensively as the foundation of ACOs. The best example of how this can and does accelerate improvement in health outcomes has been provided by the few truly integrated delivery networks who were early adopters of integrated health record technology, such as Kaiser Permanente, Geisinger, Intermountain Healthcare, Group Health Cooperative, and others. These are largely issues of clinical operations and organizational structure and culture and will not be elaborated further in this chapter.
Personal Caregiver Networks
Some individuals will remain isolated in the context of managing their own health for personal health goals. Web communities such as PatientsLikeMe and Smart Patients are specifically designed to create self-assembled groups of people with similar issues to help support each other toward better health outcomes. There is a bit of a legal conundrum about how care professionals can actively moderate these micro-communities without incurring undue risk, but many entrepreneurs are tackling that issue in novel ways. These social support technologies can be placed into three categories:
• Unmonitored
• Monitored
• Active intervention
Increasingly, human-centered design reveals how critical it is to embed any form of support, including social, within native workflows and experiences. As a result, dominant social networks (Facebook, Snapchat, WeChat, etc.) will increasingly become the preferred platforms for these social support technologies. There are inherent conflicts incurred by the naturally monopolistic nature of these networks with the sensitive tradeoffs of access, privacy, and security.1
What Can the Impact of Innovations Be on the Future Technologies?
Any physician who can be replaced by a computer should be.
–Warner Slack19
Just how far can we go with new technology in healthcare? Several respected futurists have raised the existential and philosophical question of how the future of AI and robotics could fundamentally threaten the role and/or existence of the human species.20 While the existential threat is debated, the threat to optimal levels of human employment is recognized worldwide as robotics continues to displace tens of millions of jobs.
While we discover how often machines can replace many routine and complex tasks, we simultaneously e-discover the essence of healing, where a focus on the compassion and empathy of caring can be mimicked and leveraged by the machine, but not replaced. We must use modern technology to restore ancient wisdom and compassion. This simple maxim will help define the human roles in our increasingly technologic future.21 Even chatbots and health robots can model empathy and stimulate reciprocal feelings of trust when specific human characteristics are embedded in language, tone, and facial expressions of robots.
Key Gaps and How Technology Can Help Close Them
There are 14 gaps between where we are today and where we can go with better technologic support. If we close those gaps with innovative applications of technology, such as a plecosystem, there will be new opportunities in innovation to solve healthcare problems. The most important gap to close is the empathy gap, which I will discuss first.
The Empathy Gap Is the Most Important Gap to Close
For the secret of the care of the patient is in caring for the patient.
–Francis W. Peabody, MD, October 21, 1925
This simple assertion that empathy is a requirement for healing is both the most critical and the most challenging gap to close in all of humanity today, with healthcare representing a central opportunity. Great leaders such as Dr. Peabody have inspired generations of compassionate physicians. However, many factors conspire to inhibit or even rob the caring professions of their true potential for empathy. The rigors of qualifying for a competitive spot in medical school (or any of the healing arts) results in a pre-selection bias against the most empathic candidates who might not get the same grades and scores because their empathy leads them to be less self-indulgent in their own career paths. The intense training, often with sleep deprivation, delayed gratification, debt accumulation, constant time pressure, and an unspoken (and sometimes spoken) sense of futility in treating people who are not motivated to do their part to engage in a healthy lifestyle all contribute to a drain on empathy. Further, healers are not immune from the implicit bias that contributes to social disparities in health outcomes. The “empathy gap” is the most critical and first for discussion because it is truly at the core of “why” someone should be motivated to enter and practice the healing arts, and yet technology itself has, if anything, increased the distance between the healer and that empathic ethos.
If this empathy gap and related implicit bias are so critical to healing and healthcare, and if technology so far has not helped, how can the use of technology close this gap? One relatively simple approach is to use validated survey tools to quickly understand how each individual approaches their life in terms of values, attitudes, and receptiveness to different types of behavioral support and motivational tools. A variety of innovations are moving in this direction. Ultimately, we can create a palette of tools that quickly helps assess how best to communicate with and motivate each individual, with a motivational formulary adapted to them, and motivicons that resonate with their receptiveness and aspirations. The social aspects of each individual’s learning style and their available personal social network support system (e.g., PatientsLikeMe or Smart Patients) augmentation of social support structures will play an increasingly important role.
As previously described, the VR-based “physical transfer” may utterly transform our ability to teach, motivate, and sustain empathy and overcome implicit bias. This single aspect of the rapidly maturing technology of VR is perhaps the most hopeful prospect for how technology can begin to directly shape the human experience in a concerted way toward a more empathic and compassionate future. It is not coincidental that the teams developing VR programs for increasing empathy and reducing implicit bias in healthcare have also targeted the most proximate existential threat to the human species, global warming, by using VR technology to create a “field trip” for the world to give large audiences the “experience” of how ocean acidification is unequivocally threatening our planet and our species. The recent unveiling of that technology will hopefully represent a milestone in our awareness and commitment to address climate change.
We are already experiencing many of the health effects of global warming, such as the epidemic spread of previously restricted mosquito-borne viruses including Zika virus, Dengue, and Chikungunya. These rising epidemics, while already serious health threats, pale in comparison to the health and social consequences of the human dislocations and associated access to clean drinking water caused by rising sea levels. Any technology can be used for good or evil purposes, and VR is no exception. There is already an association made of how “shoot-em-up” video games like Grand Theft Auto can desensitize game players to their impact on others and correlate with antisocial behaviors. So the biggest opportunity with VR is how we as a society and culture embrace its applications for the benefit of our societies and our planet. Facebook’s acquisition of Oculus for $2.3 billion is in no small part motivated by CEO Mark Zuckerberg’s personal commitment to use this technology for humanistic and philanthropic good.
Gap Between Evidence and Behavior for Disorders of Lifestyle
The future is already here—it’s just not very evenly distributed.
–William Gibson, sci-fi author
Gibson’s prescient assertion can be updated as follows to embrace the opportunity afforded by the exponential advances across many parallel and synergistic technologies:
The future is already here—it’s just not very evenly distributed across populations, converged across technologies, and democratized for the benefit of all.
Since traditional healthcare delivery only addresses about 10–20 percent of the root causes affecting the health of our communities,14 we must first imagine how to more effectively get at the root causes of disease. How do we create higher levels of health and resilience for individuals and their communities?
The epidemiologic evidence paints a fairly clear picture of what leads to longer and healthier lives. Despite that evidence, sedentary lifestyles, fast-food diets, epidemic sleep disorders, and, for many, the loss of a sense of real social community have all conspired to raise the disease burden of our population. These factors combined have contributed not only to the historically high levels of obesity and diabetes, but also to the rise in prevalence of cardiovascular and cerebrovascular disease, cancer, and many forms of dementia, including Alzheimer’s disease. The abundant epidemiologic evidence and detailed molecular and genetic evidence clearly indicate that the Blue Zone findings generalize to every individual, although there is some genetically based variation in susceptibility to each of the factors affecting healthspan and lifespan.15
However, the ability of the healthcare delivery system to address these issues by itself is clearly constrained. Several healthcare organizations, including Kaiser Permanente, have initiated aggressive campaigns to address these issues. The following projects are among many that Kaiser Permanente has sponsored:
• The “Thrive” campaign, which includes educational programs for all ages, such as “Every Body Walk” and “Exercise as a Vital Sign”
• The documentary series “Weight of a Nation”
• Increased availability of farmers’ markets in “nutritional deserts” in the inner cities
• Support for the creation of safe areas for walks and recreation through collaboration with communities and policy makers
Political/social efforts to address childhood obesity represent another key example of how social policy and advocacy can make a difference. While much progress has been made and some fast-food restaurants have recently revamped their menu offerings to include healthier choices, there is still a long way to go. In concert with these political, social, and community efforts, innovative technology can offer many solutions to help initiate, motivate, and calibrate individuals toward their goals for healthier lifestyles. As described earlier, wearable sensors in combination with motivational tools that are personalized to the individual, using avatars and behavioral economics, offer huge opportunities to close this central gap for driving unhealthy outcomes, reducing the cost of healthcare, and restoring the confidence of the healthcare communities that they can indeed succeed in thwarting the current epidemic in diseases of lifestyle.
Collectively, all of these changes create a “behavioral symphony of wellness.” In order to go forward, the careful integration of multiple technologies with social policies and collaborative community efforts is required. A simple example of the innovative opportunity is using new consumer-grade technologies that can quickly and reliably assess the “health value” of a particular food item, beyond what might be listed on a package label or restaurant menu.
Regular and sufficient sleep is critically important to overall health. Disruption of our circadian rhythm has pervasive consequences for health, and healthy patterns of sleep are critical for clearing the beta-amyloid (highly associated with Alzheimer’s disease) from our brains.22
Sleep disorders are far more prevalent now as a direct consequence of both the epidemic of obesity-associated sleep apnea and the high levels of anxiety associated with the time pressures of modern life. While many innovative wearable technologies have advanced our ability to monitor our sleep, we still struggle to effectively address the root causes of sleep disorders. Aside from sleep apnea, many sleep disorders reflect the cumulative impact of unhealthy lifestyle choices and exposures during the day. The previous discussion concerning the other aspects of healthy living will likely contribute to a final common pathway of healthier sleep habits and patterns, which hopefully will initiate a virtuous cycle of healthier wakeful behavior leading to healthier sleep habits leading to healthier wakeful behavior, ad infinitum.
In addition to better support healthy habits in children with respect to all these factors, we need better methods for early screening and detection of many morbidities deriving from lifestyle disorders. Earlier detection of metabolic manifestations will both enable earlier intervention and provide better metrics for gauging progress against goals. The introduction of “mindfulness as a vital sign” would systematize the capture of this information. This is similar to what has already been done with “exercise as a vital sign” or “BMI as a vital sign.” In addition, the science behind the mindfulness of many ancient healing arts, including transcendental medicine, is beginning to be elucidated at the genetic and molecular levels with evidence that brain architecture is favorably altered as well. Wearable technologies, including MUSE and HeartMath, are directly targeted at helping initiate and sustain a more peaceful, meditative, and mindful state. As we use big data analytics to better appreciate the benefits of these ancient wisdoms, we can more successfully infuse them not only into more widespread practice of integrative medicine but also into early childhood education to shape healthy habits earlier in the lifecycle where they can yield huge lifelong benefits. Effective educational programs including the use of VR for parents to help them experience the benefits of better parenting may well become a profoundly useful use case for VR globally in early parenting experiences and practices.
Environmental Disruption Gap (Chemical, Thermal, Microbial)
Our food, air, and water are contaminated with industrial toxins and carcinogens.23 We know that both automobile particulate exhaust and synthetic carpets are highly associated with the rise in reactive airway disease (RAD). Our food is riddled with antibiotics that disrupt our microbiome that normally maintains a healthy immune system, which in turn maintains a healthy brain.24 A pervasive herbicide impairs our natural enzymes that detoxify dietary antibiotics and disrupts the ancient evolutionary balance of bacterial ecosystems in our gut that are so essential to a healthy immune system.24 The global pervasiveness of these modern intrusions into our environment by over 80,000 novel manmade chemicals has made it extremely difficult to identify cause and effect. The Toxic Substances Control Act of 197625 was nothing less than a capitulation to the industrial chemical giants that has frustrated research about the impact of new chemicals before, during, and after their introduction into our environment.
Careful toxicology of human serum and body tissues shows that even in remote parts of the world native residents have measurable levels of manmade toxins that have become globally pervasive in our food, air, and water. While we desperately need responsible social policy that funds research, and legislation that bans the biggest offenders for commercial use and release into our environment, there is once again a key role for technology and technologists to play in untangling this complex morass of toxins that now has universally contaminated every one of our bodies. The advent of big data analytics and deep learning should help us identify sources and causal relationships between specific pollutants, serum and tissue levels, impacts on our microbiomes, and specific health outcomes to help eradicate much of the unintended consequences of the otherwise salutary industrial revolution.
The dense sensor network developed by UCSD’s California Institute for Telecommunications and Information Technology (Calit2) and the deep analytics behind it and similar initiatives elsewhere will help us identify and eliminate more of the toxins from our air and water as we better understand which ones pose the more serious threats and at what levels or thresholds.26 There is a critical quadriad of technology that will dramatically enhance our ability to address this issue:
• Polyfunctional sensors (fixed and mobile)
• Pervasive testing of serum levels of toxic substances
• Identification of genetic variation in susceptibility, detoxification enzymes, and processes
• Big data analytics and visualization to suggest correlations, then validate causations
That quadriad of technologies when converged should help us identify each of the following:
• Which people are at risk of exposure to which chemicals?
• Which chemicals should be removed from commercial production?
• Which chemicals require decontamination of the environment?
• Which classes of chemicals should raise the bar for approval of any new species in that chemical class into commercial production?
Without the quadriad of technologies and innovative convergence of those tools focused on complex problems such as chemical exposure, we will continue to be creating environmental threats to the health of our global communities.
Learning/Education/Communication Gap
While better education is relevant to each of the three gaps described thus far, there is a pervasive need to provide more context-specific, validated, actionable information to individuals, communities, professionals, and policy makers. As previously discussed, VR and AR are extremely disruptive opportunities to accelerate learning. Avatars can increasingly broker personal and context-specific motivational material (including motivicons and motivational formularies). An example of matching motivational methods with individual motivational profiles is Framehealth.com. The matching occurs both at the reference level with avatar chatbots, as well as at the social level in social avatar networks and moderated escalations from both chatbot failures and avatar network failures.
In addition to the exponential rise of AI, VR, AR, and avatars as instruments of education, there is another exponential source of new and real-time information emerging from the Internet of things (IOT) that will challenge our ability to transform massive contextual information into actionable knowledge. Innovation in this space will be characterized by both the network topology and the “accordion model of learning,” explained next.
IOT Data Filtering and Analytics Designed for Continuous Learning
Rather than assume that we should stream all data from all sensors into an enormous centralized or federated cloud database as a substrate for all analytics, we can appreciate the necessity of some intelligent sorting of signal from noise. As a simple example, if we’re monitoring exercise, do we really need to know the GPS location of an individual at every pico-second? Clearly not, yet the technology could deliver that volume of data. So how do we decide what level of filtering of inbound information is appropriate for a specific use case or for future unknown use cases? We simply don’t yet know which data abstraction is appropriate for every existing and future possible use case. However, an iterative process embedded in a network topology by design can accommodate Continuous Learning as a Service (CLaaS™).
Specifically, in the example of monitoring exercise, the total translational motion can be abstracted from the accelerometer and GPS data to effectively determine distance moved, altitude changes, and a composite score for energy consumed. Only those abstracted data relevant for the use case need be transmitted to the analytic cloud, whereas the analytics that abstract that information can reside within the wearable device itself, within a body sensor network aggregator, or in edge analytics. These filtered data could be staged for transmission with topologic buffers so that no resource in the network is unnecessarily overwhelmed. In the reverse direction from the analytic and decision-support sources, the intelligent feedback/advice to the user (e.g., “slow down, you’re above ideal maximal heart rate”) can be staged on the efferent loop back to the individual. As a simple example, there may be dietary advice intended for a person who has just received emotionally distressing news unrelated to their diet. We need machine learning to help determine “when” to deliver motivicons within a personal motivational formulary to an individual based on emotional and other context for that individual. Does this person respond better to the advice of “don’t eat that unhealthy comfort food (donut)” when they are at peak emotional reactivity, or are they more likely to be receptive after their galvanic skin response (GSR) sensor, HeartMath, or Afectiva (www.affectiva.com) data indicate that they’ve partially/fully recovered from the stressor? Augmented reality sensors and displays will also play a role in informing individual decisions. Simply put, timing of the message may be as important as what the message communicates or what communication medium is used (e.g., text vs. video motivicon vs. humorous cartoon). There is an enormous goldmine of innovation to begin to instrument the data relevant to these questions, develop the behavioral science around the answers to these questions, “read” the emotional tone with tools like Afectiva, and use a network topology, edge analytics, temporal buffers that operate on appropriate inbound data and outbound alerts or deeper data interrogations, and the accordion model of learning (see below) to support both continuous and periodic learning.
The Accordion Model of Learning
The second component of this approach to continuous learning is “the accordion model of learning.™”
This refers to the fact that we may initially filter out “extraneous noise” in a data set before transmitting to a body sensor network aggregator, edge server, or a central server, but later we might subsequently learn that this “noise” has previously unrecognized signal in it. We need to elucidate and elaborate the triggers that warrant “opening that accordion” to reevaluate the filtered “noise.” Those triggers consist of newer technologies for analytics, new contextual information that might influence the value of those data, or better knowledge about what is relevant to which person under what situation of health or disease—that is, advances in the global knowledge base relevant to this specific subset of data. The periodicity of opening and closing of this accordion for filtering data will vary by data type and velocity of change in both the sensing and the analytics spaces, especially in the context of big data, wherein mashup of previously isolated types of data is overcome and visualization tools help recognize relevant correlations and potential causative relationships heretofore unknown. The network topology, storage topology, and localization of analytics will need to be structured in such a way that analytics can be moved as close as possible to the self-contained dataset but no closer, and data will be moved as far out as the analytics engine relevant to that datatype in context, and no farther.
Buffers for Staging Information Inbound and Outbound Between People, Devices, and Analytics Environments
The heuristic architecture previously described can function with or without temporal buffers, but there are two types of buffers that would assist overall performance and effectiveness:
• Inbound (to central services) data buffers Temporal staging for load-balancing resources (network/analytic/storage/CPU) with compromised headroom
• Outbound (to devices or individuals) alert/advice or data interrogation buffers Temporal staging to ensure that the device or individual is “ready” to most effectively respond to that alert/advice or interrogation
Failure and outlier detection in these contexts is a rich opportunity for innovation in AI and big data analytics and visualization. Failures of both process and outcome will become increasingly transparent and subject to both continuous and machine learning and will increasingly reinforce the paired questions “Who owns your avatar?” and “Who owns your black box?,” which refer to the human oversight of the values and objectives used both directly and heuristically to guide the libraries of algorithms that drive avatars and decision-support black boxes (e.g., Amazon’s Alexa as first-generation commodity). Clearly, the world of AI poses risks to the ability of any human or group of humans to truly retain control over which values and objectives are prioritized and how those values and objectives are delivered or motivated by various avatars and black boxes. Alternatively, these explicit and transparent values and objectives may be subjugated by other priorities in a variety of opaque methods.
The term “dyadarity™” as opposed to “singularity” is useful to capture this dilemma. In a dyadarity, the introduction of any new advance in AI could be deployed strictly under human direction to ask, and hopefully address, the following four questions within the existing AI infrastructure, avatars, and black boxes:
• Are the desired values and objectives both explicit and transparent?
• Are those values and objectives effectively governed by appropriately represented humans with a diversity of views?
• Are those values and objectives effectively implemented?
• Who decides who is included in any automation of the arbitration between conflicting values, and what are the limits of “auction design” in adjudicating those decisions?
David Brin’s book The Transparent Society is a primer for considering social policy goals in the context of the digital age.5 The emergence of powerful AI since the publication of that book in 1998 only highlights the necessity of a larger public exposure to the technologic risks and innovative opportunities.
AI/Robotics Robotics Gap
There are many lengthy treatments of the benefits and risks of the emerging AI/robotics infrastructure to the extreme of their representation as an existential threat to humans. Robots are predictable by design, whereas humans are much less so. Programming robots to be adaptive enough to anticipate the full range of human behavior is a significant challenge and hence a critical opportunity. Many of the remaining challenges for the self-driving car or truck relate to the interaction of such vehicles with either pedestrians or other vehicles driven by humans. Even intuitive heuristics from superior engineers fail to anticipate every permutation of unpredictable and/or dysfunctional behavior from individual humans.
Gap in Seamless and Reliable Human Data Entry
Integration of conventional input devices (keyboard, mouse, trackpad, joystick, etc.) with more natural inputs such as full haptics-based data capture, video capture combined with video analytics (e.g., for monitoring progress with neurologic disorders), and natural voice capture with natural language understanding (NLU) with real-time natural language processing (NLP) will advance in ways that simplify, augment, and streamline the data-capture process. Innovation in this arena will significantly relieve the current conundrum around usability of electronic health records.
Gap in Evidence-Based Virtual Care
While some have predicted that 80 percent of doctors will be rendered unnecessary by automation, that assertion assumes that the role of the human will remain static as machines replace various human tasks. The “human aspect” of care can be simulated, but it is unlikely that genuine empathy will ever be fully entrusted to devices. The evolution of commoditized “tricorder-like” diagnostic devices will raise the opportunity for virtual care, whether by e-mail, text, phone, video, app-based autonomous avatars, or other medium. One of the biggest innovation opportunities in virtual care is how to reconcile two intersecting data sets. The first is the evidence basis for what level of communication or care is appropriate for which clinical situation. The second is the evidence basis for what individual people prefer as a communication and/or motivational modality. We have already observed that sometimes individuals will demand care over the phone for what can only safely be evaluated and treated in person. The challenge will be to reconcile the evidence base for effectiveness with the evidence base for personal preference so that overall we can achieve the highest balance of access, clinical outcomes, and patient satisfaction. Where those goals are in conflict, we need to put patient safety as the top priority, but within that frame there is an opportunity for innovative intelligent routing of problems through various modalities from simple text messaging at one extreme to face-to-face encounters at the other extreme, and everything in between.
The Science vs. the Application of –omics (Genomics, Microbiomics, Proteomes, etc.) Gap
In no area of healthcare is the science of health so disrupted as in the areas of genomics and microbiomics. It is increasingly clear that the genome, microbiome, immunome, and neurome are intimately interrelated and interdependent. Collectively these areas are called the “omics.” Simple examples include the fact that excessive exposure to antibiotics in children under age 5 is associated with disruption of the gut bacteria (dysbiosis), and by age 15 those children have maldistribution of gray matter in the brain, closely resembling the typical pattern for people suffering from depression and anxiety. There are huge opportunities for big data analytics and visualization to begin to disambiguate the complexity of these interactions. In genomics alone, the big opportunities currently reside in four main areas:
• Diagnosing and treating cancer
• Diagnosing and treating over 500 known inborn errors of metabolism
• Pharmacogenomics decision support (selecting drug and dosing based on pharmacogenomics profiles)
• Early diagnosis and appropriate treatment of infectious diseases (where antibiotic resistance can be detected with initial sequencing)
Many other benefits of genomic sequencing will emerge, but these appear to be among the most promising to have impact in the immediate future. It won’t be long before personalized health maintenance and preventive medicine schedules are routinely informed by the genome of each individual.
The Cancer Genome Trust (CGT) concept pioneered by David Haussler at UC Santa Cruz as part of the Global Alliance for Genomic Health (GA4GH) is based on blockchain technology that promises to revolutionize our ability to do global research across many inputs to human health, including all of the conventional “omics” data, and extended to socialomics and exposomics.27
Each of these areas affords opportunities to integrate traditional medicine, lifestyle interventions, and integrative medicine. Traditional evidence-based medicine reflects the use of approaches for entire populations of patients. We are moving to much more personalized medicine when we use analytical tools to identify patients with like conditions to help guide care for an individual. When we can identify small cohorts of individuals who more closely resemble the individual patient under consideration, we can apply practice-based evidence in a more context specific method to each individual. This approach is at the core of both “personalized medicine” and “practice-based evidence,” while not abandoning the traditional “evidence-based practice” of medicine embodied in clinical practice guidelines targeted less precisely on a population of individuals.
While CRISPR/Cas9 genetic editing technology is very promising for correcting many germ-cell line genetic disorders, there have been a variety of other genetic editing technologies discovered since CRISPR was first reported. Other related technologies such as “gene drive” offer profound opportunities for eliminating certain infectious diseases, but also carry huge concerns about unintended consequences. Both of the technologies will rely on extensive use of big data analytics and AI to model for potential unintended consequences and balance of benefits and risk.
Gap in Drones and Healthcare
In many medical emergencies such as heart attacks, strokes, narcotic overdoses, or traumatic injuries such as ruptured spleens, minimizing the time elapsed between the event and the medical/surgical response can be life-saving. First-responder drones will likely become ubiquitous so that within minutes of a 911 emergency call, a drone or multiple drones could arrive at the scene and deliver life-saving advice and care, such as cardioversion to restore normal heart rhythm or bystander-administered Narcan in the case of a verified narcotic overdose. There are many opportunities for innovation in how we design and operationalize the deployment of these drones and how we coordinate medical oversight with direct-care delivered by untrained bystanders and first responders.
In less acute situations, highly contagious diseases will be diagnosable through commoditized home/field diagnosis of infectious agents and antibiotic sensitivity so that appropriate antibiotics can be delivered quickly and efficiently to a patient anywhere in the world without the risk of exposing others to that infectious agent. Solar-powered drone-charging stations that support drones capable of delivering emergency drugs have already been field-tested in Haiti and are on the verge of widespread deployment in remote corners of Africa. This drone delivery network will become an integrated component of virtual care and remote monitoring.
Gap in 3D Printing
Simply put, the ability of 3D printers to print nearly any physical product from a rapidly growing array of materials has already led to printed functioning organelles and larger organs such as human esophagus for implant post-esophagectomy for cancer, in conjunction with stem cell therapy. Soon to follow will be autologous kidneys created from one’s own stem cells, as well as other organs. There are almost limitless possibilities for how 3D printing will transform health and reverse local organ aging. There are already over 300 materials that can be used for printing, and China has already printed five single-family houses in two days as well as a five-story apartment building. What was previously unimaginable and cost-prohibitive because of complex design is becoming affordable because there is no material wastage in 3D printing, no matter how complex the design.
Gap in Chatbots, AI, Trust, and Health
An “AI psychiatrist” developed by the Department of Defense (DoD) has proved to be more trusted by users than human psychiatrists, because it is perceived as nonjudgmental as opposed to human psychiatrists.28 This is a simple extension of the finding 30 years ago that patients were more candid with computer surveys of their illicit drug use for the same reason. The implications for scalability and bringing more relief to more sufferers of mental illness are profound. IBM has put Watson in the cloud, open-sourced the API, and put up millions of dollars to encourage use of Watson in the cloud. The possibilities are extraordinary for discovering new useful knowledge and applying it.
Gap in Transcranial Magnetic Stimulation and Health
Weak magnetic pulses to specific brain regions have created experiences including out-of-body experiences and mystical experiences resembling those of people with near-death experiences. The use of high-resolution imaging of the brain and deep-learning analytics and visualization tools will provide new probes into how the brain functions and have already provided examples of how we can begin to treat serious neuropsychiatric disorders through increasingly less invasive brain stimulation.
Gap in New Psychopharmacology Research and Previously Refractory Psychiatric States
Use of low doses of MDMA (ecstasy) in conjunction with talk therapy have created sustained recovery from severe post-traumatic stress disorder (PTSD) for up to four years.29 Again, the use of high-resolution dynamic brain imaging and big data analytics and visualization will help guide research and treatment for an expanding array of mental illnesses, including common disorders of anxiety and depression.
Gap in Harnessing Exponential Technology
When considering the vast array of technologies that are expanding in scope and impact at an exponential pace, it is useful to cluster these exponentials into a simple taxonomy. Table 23-1 provides a brief and partial taxonomy.
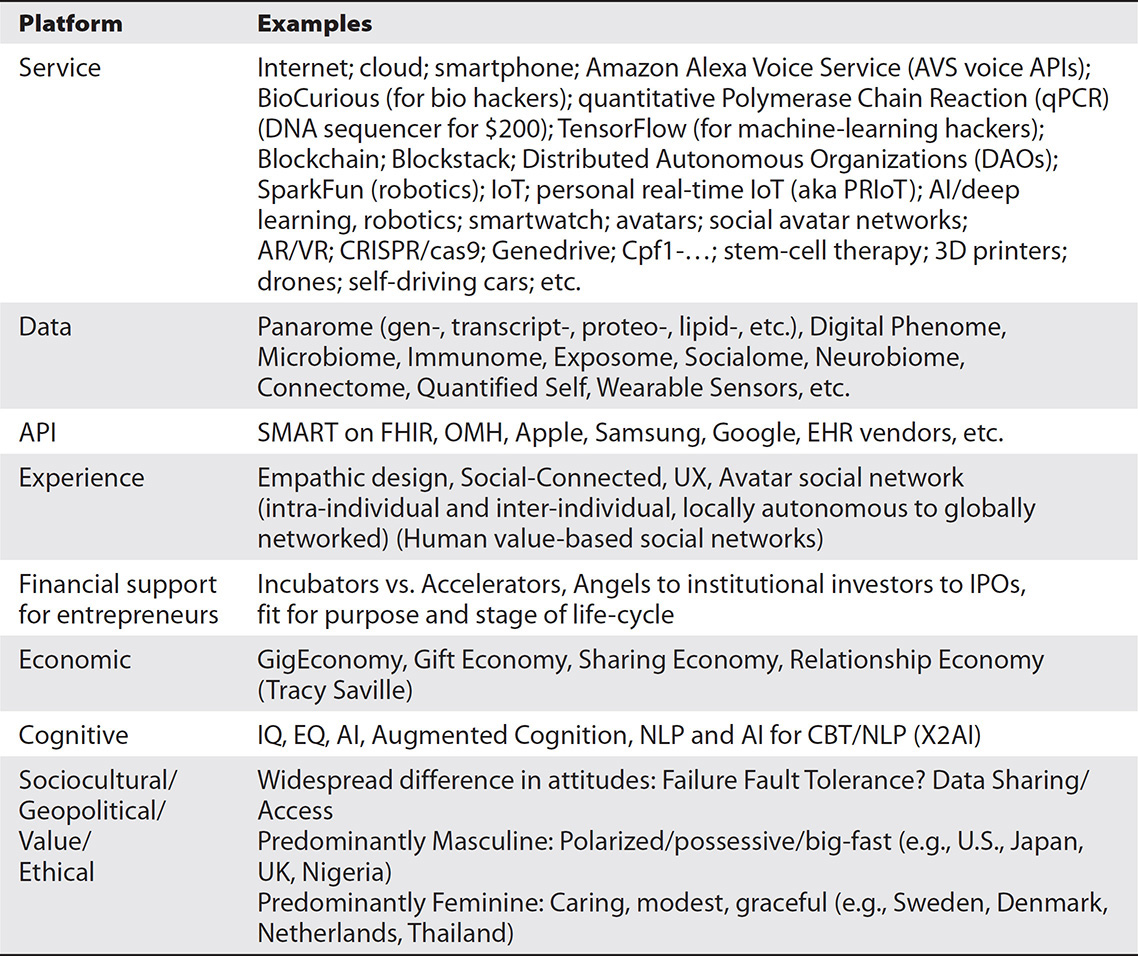
Table 23-1 Eight-Platform Dimensional Taxonomy of a Plecosystem
There are five principles that characterize members of this taxonomy:
• Exponential growth As an example, it took only ten years from the introduction of the first smartphone to reach 1 billion phones; a similar exponential pattern exists for many platforms.
• Synergy and convergence Value rises exponentially with the number of nodes accessible, the number of data types accessible, and the number of platforms converged within any solution set.
• Data liquidity Amplified by federation of data, respecting local privacy values/policy. Blockchain may be a game-changer here (CGT of GA4GH as a model).
• Person-centricity (e.g., Matticalfe’s law) The number of data types linked to a single person raises the value of each individual data type linked to that individual.
• Open source acceleration of value Open source communities accelerate innovation through “interoperability by design.”
I reserved this final gap, “harnessing the plecosystem,” for last because understanding the potential convergences of each of these dimensions of the multiplatform exponential world we now live in has given rise to what can be described as “The Sci-Fi Generation.” If you can imagine it, you can create it in your own lifetime.
Chapter Review
This chapter covered several concepts of innovation. It offered a frame of reference for the big opportunities to innovate in healthcare using healthcare IT as one of the integrated components within the broader framework of communities, social determinants of health, and behavioral and motivational frameworks. This chapter provided an understanding of how critical it is to restore empathy throughout every aspect of health and wellness and some of the emerging technologies that can help develop and reinforce empathy, alongside tools that help us personalize our behavioral and motivational tools to each individual as a major component of personalized medicine. It also examined the emerging roles of various new technologies to help accelerate both learning and the acquisition of healthier behaviors to combat the epidemics of diseases of lifestyle disorders. The chapter presented how the plecosystem can help inform healthcare IT work to exploit emerging cross-platform technologies and services to create synergy through convergence. Finally, the chapter described the principles that help accelerate innovation across the plecosystem.
Questions
To test your comprehension of the chapter, answer the following questions and then check your answers against the list of correct answers that follows the questions.
1. Which of the following are distinct types of innovation?
A. Disruption and disintegration of old tools, jobs, and processes with new ideas, tools, and business models
B. Incremental optimization of how a technology is operationalized and advanced
C. Identify, scale, and spread local successes (hotspotting, positive deviance)
D. Cultural transformation
E. All of the above
2. How can the gap between science and action be closed to address the crippling disorders of lifestyle?
A. There are no innovative tools that can close the gap between science and action to address the crippling disorders of lifestyle.
B. Start in early life to develop healthy habits of sleeping, eating, exercise, and social health and use modern motivational tools and techniques to personalize the behavioral program for each individual and create a digitally enhanced “behavioral symphony of wellness.”
C. Develop new empathy tools for patients.
D. None of the above.
3. How can you reverse the unhealthy impacts of environmental disruption?
A. Polyfunctional sensors (fixed and mobile), pervasive testing of serum levels of toxic substances, identification of genetic variation in susceptibility, detoxification enzymes, and processes, and big data analytics and visualization methods to suggest correlations.
B. Big data analytics and validation of causes alone.
C. Wearable sensors alone.
D. Big data analytics and visualization of genetic variation alone.
4. How do we architect an infrastructure for continuous learning?
A. Feedback from sensors and avatars.
B. Bring analytics as close to the source data as practical.
C. Accordion model of learning, filter noise out close to the source, bring analytics close to the source, identify triggers, and leverage evidence-based practice.
D. None of the above.
5. What approaches enhance data capture and usability?
A. Enhanced sensor data only
B. Enhanced video capture only
C. Enhanced capture and analytics of genomic data only
D. Enhanced voice capture with real-time NLP and NLU, enhanced video capture with real-time video analytics, and enhanced capture and analytics of haptics-based data as well as the increasing array of noninvasive sensor data
6. What evidence-based approaches will guide how we implement virtual care?
A. Individual patient’s preference for communication tools alone will be the best approach.
B. Explicit methods for balancing between NLP and NLU voice capture.
C. There are no ways that evidence-based approaches guide virtual care.
D. Evidence basis of which form of care is most effective for an individual at a point in time, based on their complete health history as well as their current problem, patient’s preferences for communication tools, and explicit methods for balancing between the evidence and the patient preference when they are in conflict.
7. What are some of the near-term wins for the role of genomics in healthcare?
A. Diagnosing and treating cancer, diagnosing and treating over 500 known inborn errors of metabolism, pharmacogenomics decision support (selecting drug and dosing based on pharmacogenomics profiles), and early diagnosis and appropriate treatment of infectious diseases (where antibiotic resistance can be detected with initial sequencing).
B. It is too early to determine the role of genomics in healthcare.
C. The results of the Precision Medicine Initiative will determine the near-term wins for the role of genomics in healthcare.
D. The only win will be in pharmacogenomics in selecting drug and dosing based on pharmacogenomics profiles.
8. Name five of the platform types in the plecosystem?
A. Data, API, financial support, Internet, consumer service
B. Data, economic, Internet, consumer, and API
C. API, data, economic, Internet, and consumer
D. Experience, financial support for entrepreneurs, economic platforms, cognitive platforms, and sociocultural/geopolitical/value/ethical platforms
9. What are the five principles of the plecosystem?
A. Exponential growth of platforms, synergy through convergence across platforms, data liquidity, person-centricity of data, and acceleration through open source communities and components.
B. There is only one principle of a plecosystem: it can accept sensor data.
C. Person-centered data is the sole principle of a plecosystem.
D. None of the above.
Answers
1. E. The four distinct types of innovations are (1) disruption and displacement of old tools, jobs, and processes with new ideas, tools, and business models, (2) incremental optimization of how a technology is operationalized and advanced, (3) identify, scale, and spread local successes (e.g., hotspotting, positive deviance); and (4) cultural transformation.
2. B. We close the gap between science and action to address the crippling disorders of lifestyle by starting in early life to develop healthy habits of sleeping, eating, exercise, and social health and use modern motivational tools and techniques to personalize the behavioral program for each individual and create a digitally enhanced “behavioral symphony of wellness.”
3. A. You can reverse the unhealthy impacts of environmental disruption with polyfunctional sensors (fixed and mobile), pervasive testing of serum levels of toxic substances, identification of genetic variation in susceptibility, detoxification enzymes, and processes, and big data analytics and visualization methods to suggest correlations.
4. C. We architect an infrastructure for continuous learning by the accordion model of learning, filter noise out close to the source, bring analytics as close to the source data as practical, identify triggers that allow the accordion to reopen to “old noise” and discover a new “signal” within it as new knowledge and technologies emerge, and leverage a virtuous cycle of evidence-based practice and practice-based evidence.
5. D. The approaches to enhancing data capture and usability are through enhanced voice capture with real-time NLP and NLU, enhanced video capture with real-time video analytics, and enhanced capture and analytics of haptics-based data as well as the increasing array of noninvasive sensor data.
6. D. Evidence-based approaches that will guide how we implement virtual care include using an evidence basis of which form of care is most effective for an individual at a point in time, based on their complete health history as well as their current problem, the individual patient’s preference for communication tools, and explicit methods for balancing between the evidence basis of effectiveness and the individual patient preference, when they are in conflict.
7. A. The near-term wins for the role of genomics in healthcare are diagnosing and treating cancer, diagnosing and treating over 500 known inborn errors of metabolism, pharmacogenomics decision support (selecting drug and dosing based on pharmacogenomics profiles), and early diagnosis and appropriate treatment of infectious diseases (where antibiotic resistance can be detected with initial sequencing).
8. D. Five of the platform types in the plecosystem are experience, financial support for entrepreneurs, economic platforms, cognitive platforms, and sociocultural/geopolitical/value/ethical platforms. Service, data, and APIs are also platform types, but not sole platform types.
9. A. The five principles of the plecosystem are exponential growth of platforms, synergy through convergence across platforms, data liquidity, person-centricity of data, and acceleration through open source communities and components.
References
1. Mattison, J. E. (2015). Managing risk in institutional innovation programs. Accessed on October 6, 2016, from http://medtechevents.blogspot.in/2015/10/managing-risk-in-institutional.html.
2. Weitzner, D. (2004). The transparency paradox: Privacy design strategies for open information networks. Accessed on October 6, 2016, from https://www.w3.org/2004/05/loc-priv-transparency-extab.html.
3. Stanford University Virtual Human Interaction Lab. (2016). Accessed on October 6, 2016, from https://vhil.stanford.edu/.
4. RethinkRobotics.com. (2017). Baxter. Accessed on February 27, 2017, from www.rethinkrobotics.com/baxter/.
5. Brin, D. (1999). The transparent society: Will technology force us to choose between privacy and freedom? Basic Books.
6. Kotler, S. (2014). Legal heroin: Is virtual reality our next hard drug? Accessed on October 6, 2016, from http://singularityhub.com/2014/02/24/legal-heroin-is-virtual-reality-our-next-hard-drug/.
7. Christensen, C. M. (2013). The innovator’s dilemma: When new technologies cause great firms to fail. Harvard Business Review Press.
8. Keeler, L., Walters, H., Pikkel, R., & Quinn, B. (2013). Ten types of innovation: The discipline of building breakthroughs. John Wiley & Sons.
9. American Medical Association (AMA). (2014). Improving care: Priorities to improve electronic health record usability. Accessed on October 6, 2016, from www.aace.com/files/ehr-priorities.pdf.
10. Payne, T. H., Corley, S., Cullen, T. A., Gandhi, T. K., Harrington, L., Kuperman, G. J., … Zaroukian, M. H. (2015). Report of the AMIA EHR 2020 task force on the status and future direction of EHRs. Accessed on October 6, 2016, from http://jamia.oxfordjournals.org/content/early/2015/05/22/jamia.ocv066.
11. Sternin, J., & Choo, R. (2000). The power of positive deviancy. Harvard Business Review, January–February 2000, 14–15. Accessed on February 15, 2017, from https://hbr.org/2000/01/the-power-of-positive-deviancy.
12. Zanetti, C., & Bhatt, J. (2014, June 28). Big data with a personal touch: The convergence of predictive analytics and positive deviance. Huffington Post. Accessed on February 27, 2017, from www.huffingtonpost.com/cole-zanetti-do/big-data-with-a-personal-_b_5206219.html.
13. O’Brien, A., & Mattison, J. E. (2015). Emerging roles in health and healthcare. In C. Weaver, M. Ball, M. Kim, & J. Kiel (Eds.), Healthcare information management systems: Cases, strategies, and solutions (pp. 199–217). Springer-Verlag.
14. Heiman, H., & Artiga, S. (2015). Beyond health care: The role of social determinants in promoting health and health equity. Accessed on October 6, 2016, from http://kff.org/disparities-policy/issue-brief/beyond-health-care-the-role-of-social-determinants-in-promising-health-and-health-equity.
15. Buettner, D. (2008). The Blue Zones: Lessons for living longer from the people who’ve lived the longest. National Geographic Society. See also Harvard Business Review (January–February 2012) and Time Magazine (July 1, 2016), both dedicated to happiness metrics and literature.
16. Christakis, N. A., & Fowler, J. H. (2009). Connected: The surprising power of our social networks. Little Brown.
17. Kaiser Family Foundation. (2016, Aug. 2). U.S. government and global non-communicable disease efforts. Accessed on October 6, 2016, from http://kff.org/global-health-policy/fact-sheet/the-u-s-government-and-global-non-communicable-diseases/.
18. Council of Economic Advisers, Executive Office of the President of the United States. (2015). The economics of early childhood investments. Accessed on October 6, 2016, from https://obamawhitehouse.archives.gov/sites/default/files/docs/early_childhood_report_update_final_non-embargo.pdf.
19. Oldenburg, J., & Grieskowisz, M. (2017). Participatory healthcare: A person-centered approach to healthcare transformation. CRC Press for HIMSS.
20. Zolfagharifard, E. (2015). Don’t let AI take our jobs (or kill us): Stephen Hawking and Elon Musk sign open letter warning of a robot uprising. DailyMail.org, January 12. Accessed on October 6, 2016, from www.dailymail.co.uk/sciencetech/article-2907069/Don-t-let-AI-jobs-kill-Stephen-Hawking-Elon-Musk-sign-open-letter-warning-robot-uprising.html.
21. Human Resources for Health (HRH). (2012). Integrated health and post modern medicine. Journal of the Royal Society of Medicine, 105(12), 496–498.
22. National Institutes of Health, NIH Research Matters. (2013, Oct. 28). How sleep clears the brain. Accessed on February 27, 2017, from https://www.nih.gov/news-events/nih-research-matters/how-sleep-clears-brain.
23. Baselt, R. C. (2014). Disposition of toxic drugs and chemicals in man, tenth edition. Biomedical Publications.
24. Lundberg, G. (2016). Is Roundup slowly killing us? Medscape News, August 8. Accessed on October 6, 2016, from www.medscape.com/viewarticle/866710?nlid=108743_3243&src=WNL_mdplsfeat_160809_mscpedit_imed&uac=126057HX&spon=18&impID=1175750&faf=1.
25. Toxic Substances Control Act of 1976. Accessed on October 6, 2016, from https://en.wikipedia.org/wiki/Toxic_Substances_Control_Act_of_1976.
26. California Institute for Telecommunications and Information Technology (Calit2). (n.d.). Sensor network testbed proposed. Accessed on October 6, 2016, from www.calit2.net/newsroom/article.php?id=28.
27. Global Alliance for Genomic Health (GA4GH). Accessed on October 6, 2016, from http://ga4gh.org.
28. Darcy, A. M., Louie, A. K., & Roberts, L. W. (2016, Feb. 9). Machine learning and the profession of medicine. JAMA 315(6), 551–552.
29. Mithoefer, M. C., Wagner, M. T., Mithoefer, A. T., Jerome, L., Martin, S. F., Yazar-Klosinski, B., ... Doblin, R. (2011). Durability of improvement in post-traumatic stress disorder symptoms and absence of harmful effects of drug dependency after 3,4 methylenedioxymethamphetamine-assisted psychotherapy: A prospective long-term follow-up study. Journal of Psychopharmacology 27(1), 28–39.
