CHAPTER 19
Non-EHR HIT: From Architecture to Operations
Alistair Erskine, Bipin Karunakaran
In this chapter, you will learn how to
• Understand overall HIT department organizational structure
• Describe HIT roles in healthcare organizations
• Understand the technology environment for non-EHR systems
• Identify clinical and nonclinical systems that are critical to every healthcare organization
• Identify commonalities in design and operation between the various non-EHR systems
• Understand interoperability between critical clinical and nonclinical systems
As discussed in detail throughout this book, one of the major clinical HIT systems is the electronic health record (EHR) system, which helps clinicians with important clinical functions such as viewing patient charts, preparing clinical notes, and ordering medications for both acute and ambulatory settings. This chapter, while acknowledging the central importance of EHR systems in today’s healthcare organizations, focuses on the other major information systems and information technologies that complement EHR systems and, together with EHR systems, support healthcare operations. We describe major clinical and nonclinical “non-EHR” HIT systems and applications. This coverage is not meant to be exhaustive, as the incredible diversity of HIT systems and applications used in healthcare today is huge and would preclude such coverage here. Rather we provide a framework to allow the reader to understand the main divisions within HIT and some important examples within each of the divisions and subdivisions. To begin, we’ll discuss how the HIT functions in healthcare organizations are organized, including HIT department governance and roles and how key functions are operationalized.
The Healthcare IT Organization: Challenges, Structures, and Roles
The common goals of healthcare information technology (HIT) departments in healthcare organizations are to improve quality of patient care, increase provider efficiency for care delivery, and support the administrative and revenue cycle IT needs of the organization. Attaining these goals is challenging in healthcare delivery systems that are often fragmented, where most patients receive care from disparate providers. Even large, resource-rich integrated health systems encounter challenges in coordinating multiple centers of excellence and campuses.1 Healthcare information technologies and HIT departments benefit from being organized to enable the smooth flow of information between clinicians, technologists, nonclinicians, and technology systems. A clear understanding of organizational strategy, the current state of services, and future technical, clinical, and business directions is needed both by HIT department leaders and managers as well as key HIT department stakeholders. A common standard practice for delivery of technology services is essential for a HIT organization to be successful.
Most medium- to large-size healthcare organizations have a central HIT team supporting diverse specialty practices, medical centers, and campuses. The HIT team is often led by a physician, a nurse informaticist, or a technology administrator partnered with a physician. The head of the HIT team is a C-level executive, often with the title chief information officer (CIO), with various HIT department heads reporting to the CIO. Especially when a healthcare organization has a technologist CIO, as opposed to a licensed clinical professional CIO, a chief medical information officer (CMIO) may be part of the HIT team leadership. The CMIO is often a physician, but increasingly nurses and other clinicians are assuming these roles. Typically, major clinical systems such as radiology, lab, and pharmacy and nonclinical systems such as supply chain, finance/revenue cycle management and patient relationship management are organized as separate subdepartments under the CIO. These systems are described in depth in the next section.
Medium- to large-size healthcare organizations usually organize basic IT infrastructure functions such as networks, phone switches, computer servers, and data-center operations within the HIT department to be performed by a single centralized core infrastructure team. Similarly, user-facing phone systems, PCs, laptops, tablets, and helpdesk support are handled via a central user support team.
For HIT organizations to be successful, there is a need for close alignment and interaction with various departments/service lines of the health system. For example, the radiology department needs close alignment and interactions with the technology department working on radiology systems. This close alignment and interaction enables effective communication between the radiologists and the technologists. For example, this enables the radiology team (composed of select radiology department business and clinical staff) to quickly communicate needed business changes to the tech team, and enables the tech team to communicate to the radiology team changes in the technology landscape that may provide new clinical or business opportunities to the radiology team.
Even though HIT is a central organization under the CIO, the close alignment between the tech teams and the health system departments is essential for the best service experience. To enable effective collaboration, efficiency, and alignment, major health system departments often have one or more dedicated tech personnel enhancing and maintaining specific department systems. This arrangement of having a few dedicated technologists in major departments/service lines working closely with the IT department is becoming more common, creating a hub-and-spoke model of service. A business relationship manager (BRM) assigned to one or more health system departments plays a critical role as a conduit between the health system department(s) and the HIT department. In their role, a BRM is seen as the person representing the needs of the department(s) to the HIT department. The BRM often works with individual department heads, their representatives, or the tech teams embedded in the department to create a business case for modifications to existing software systems or the purchase or build of new software systems. The BRM works closely with the HIT governance committee to present business case proposals with the intent of gaining approvals. The BRM also communicates status of various departments or enterprise-level project status to the department heads and representatives.
Figure 19-1 shows an example of a HIT team’s organization. The goal of centralizing systems under one umbrella is to enable economies of scale for technology management and uniformity in practice for providing the best patient care using technology as an enabler. Figure 19-1 represents a very general organizational structure due to the large variability of how healthcare HIT functions and departments are organized—therefore there is no one best organizational structure for HIT. We encourage you to view Figure 19-1 in relation to the “Healthcare IT Workforce Roles” section of Appendix D (see Appendix C for how to access this content), which lists several dozen of the HIT workforce roles active in healthcare organizations today, and then mix and match your own HIT subdepartment dream teams. For example, the EHR team members in a large organization may include a computer and information systems manager (reporting directly to the CIO), two project managers, two business relationship managers, four system analysts, four application specialists, and two nurse informatics (who work closely with the CMIO). The infrastructure team may have one computer and information systems manager (reporting directly to the CIO), one project manager, three computer hardware engineers, two computer network architects, two computer programmers, one information security analyst, two network and computer systems administrators, one software developer, and two electrical engineering technicians. The enterprise-wide computer help desk may also be part of the infrastructure and have a dozen or more help desk support technicians.
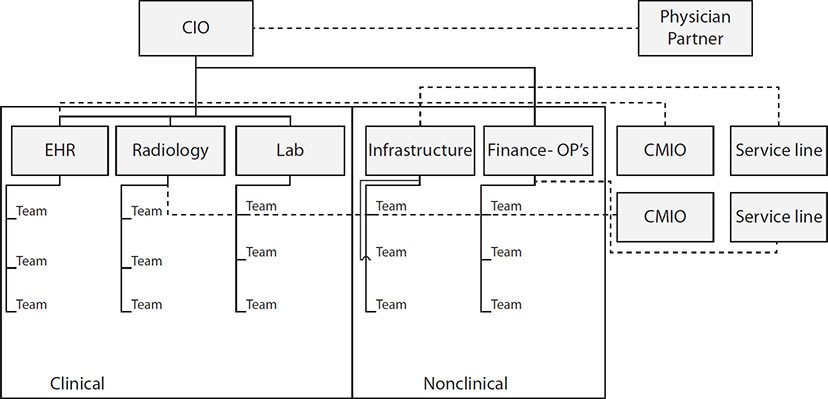
Figure 19-1 Typical HIT team organization
HIT Major Non-EHR HIT Systems and Applications
All of the major systems and applications in the non-EHR space fall into two major categories: clinical systems and nonclinical systems. One or more application data interchange systems integrate clinical and nonclinical systems data. Figure 19-2 depicts these major non-EHR systems and applications. For some vendors, these “ancillary” components are part of the core EHR system. For others, interfaces are used to connect to separate “best of breed” systems. For example, subsystems such as admission/discharge/transfer (ADT) and operating room management are tightly integrated with the EHR system, while other systems, like PACS and supply chain systems, have a more detached relationship.
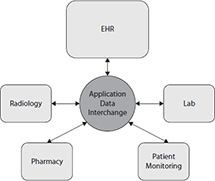
Figure 19-2 A model of select HIT clinical systems
Major clinical ancillary departments and the clinical systems that can stand alone and be integrated with an EHR system or a subsystem/module of an EHR system include:
• Radiology Picture archiving and communication system (PACS), radiology information system (RIS), speech recognition system
• Pharmacy Pharmacy management system, pharmacy workflow system, pharmacy dispensing system
• Clinical laboratory Laboratory management system, automated cellular imaging system, microbiology blood culture system, blood bank system
• Patient monitoring Electronic intensive care unit (EICU) monitoring system, operating room (OR) monitoring system
Major nonclinical systems include
• Supply chain Enterprise resource planning (ERP)/business process management systems
• Revenue cycle Billing, accounting, finance, and contract management systems
• Patient relationship management Similar to customer relationship management (CRM) software in other industries, a relatively new concept in healthcare
The application data interchange (ADI) is the application data and message interchange system for both internal system-to-system interchange and external interoperability across entities.
Working with Enterprise HIT Systems
Major HIT systems satisfy various needs of the clinical and nonclinical staff and assist in providing the best care for patients. Every health system has a core technology infrastructure that typically interfaces with other important systems. The core infrastructure consists of computer networks, phone systems, data centers with server farms, and various network switches directing network traffic internally as well as externally. Security systems such as firewalls prevent unauthorized network traffic from entering the internal network. Running on top of the core infrastructure are all systems and applications, both clinical and nonclinical.2
As patients enter the healthcare system, one of their first touch points is an online patient portal or a patient contact center. Increasingly, patients schedule appointments via the contact center or the online portal and are then seen in an ambulatory setting. Sometimes, due to the nature of the illness, patients are moved from an ambulatory setting to an acute care setting. In a few cases patients enter the system directly through the emergency department (ED). From the entry point to discharge and all throughout their care in an ambulatory or acute care facility, technology and technology systems play an important role in the care of the patient.
A patient can register online for an online account to schedule their first visit. Once an online patient account is created, subsequent visits can be scheduled online using the same account. Using the online portal, a patient can view their lab results, e-mail their provider, view and pay their bills, and so on. The online portal is one of the many systems that the HIT team builds and maintains. As the patient is scheduled for different appointments, a patient schedule management system maintained by the HIT team is used for matching patient appointments with provider availability. The schedule management system provides workflow support and reminders for patient coordinators, nurses, and providers.
As care is delivered to a patient in either an inpatient or outpatient setting, a variety of other HIT systems are used to deliver optimal patient care. A radiologist uses the PACS to store and read radiology images. A microbiologist uses the blood culture system to find an infection. To ensure the safety of donated blood, all donated blood must be tested in the lab. Blood banks are unique to the health system and one of the few functions that require FDA certification. Patient monitoring systems are used by the ICU physicians to closely monitor patient progress and their response to care. Pharmacy systems receive patient medication information as prescribed by the physician either electronically or in paper form. Pharmacy systems track medications for patients—dosage, refills, and so on. Pharmacy management software in many health systems is now part of the core EHR system.
An example of a nonclinical system is the supply chain system, which track supplies, inventory levels, and cost of supplies. Storage and movement of supplies across the health system are also tracked within a supply chain system. The supply chain system automatically orders drugs based on inventory levels, delivery timelines, and pricing. Other examples include billing systems, which are used by the revenue cycle team to create accurate billing statements for patients, and business intelligence (BI) and data systems, which are used by clinicians, operations personnel, and nonclinicians to analyze trends and future opportunities using data and analytics.
Systems that are not part of the core EHR system typically interoperate with each other via an application data interchange system. These systems facilitate exchange of data between multiple systems with guaranteed delivery mechanisms built in. For example, lab orders entered in the EHR system are sent to the lab management system via the application interchange; results from the lab management system are sent back to the EHR system also via the application interchange. This enables the labs to get information on the orders and match up the samples with the orders. The physicians see the lab results back in the EHR in a timely manner.
Vendor-Specific Systems: Acquisition, Installation, and Maintenance of HIT Systems
Healthcare information technology systems are a mix of purchased vendor software systems, usually making up the majority of systems, and internally developed custom software systems. Keeping track of the multiple enterprise-wide and more focused vendor software systems requires vendor management, which includes financial and contract management, software patching, and upgrades.
Most HIT departments have an annual budget, with a portion allocated to capital expenditures (CAPEX) and another portion allocated to operational expenses (OPEX). Dollars in the CAPEX budget are used to build or purchase new software systems, while OPEX budget dollars are used to maintain existing software system assets. Most HIT organizations have an annual budget-planning process. As part of the planning process, and based on the organization strategy and financial strength, funds are allocated to both capital and operational budgets. The budgets are managed closely by the HIT management team so that actual expenses meet the planned budget.
New software systems are purchased and implemented after a thorough vetting process, starting with a requirements analysis that includes assessing whether existing HIT within the organization meets new needs. This is followed by the researching of new solutions, which then leads to a Request for Proposal (RFP) and often involves a vendor proof of concept (PoC) implementation, as shown in Figure 19-3. A common decision point for most organizations is whether to purchase the non-core EHR components from their primary EHR vendor or to rely on stand-alone suppliers. Usually two or more vendors are vetted through the entire process before a final choice is made. The decision to select a particular vendor software system is usually based on the following four major criteria:
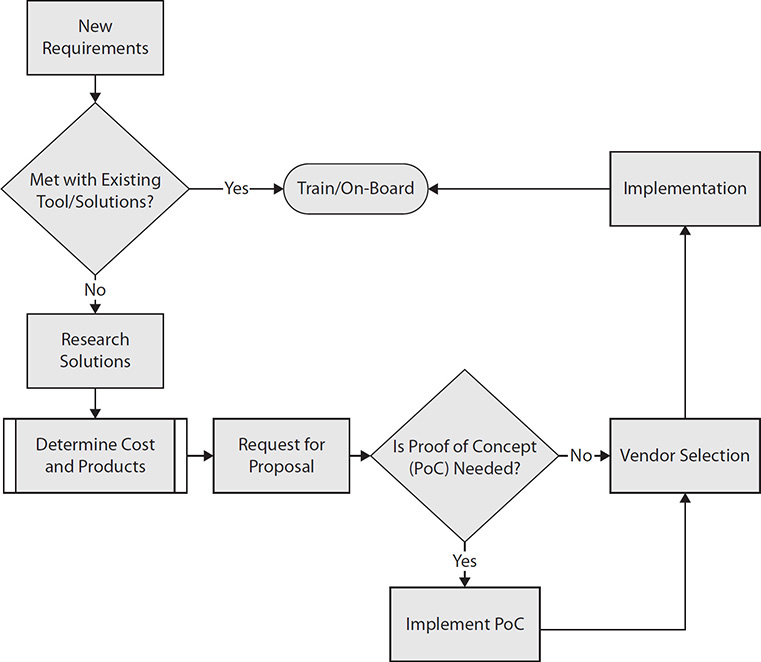
Figure 19-3 Model of a HIT vendor selection process
• System features meeting the needs of the organization
• Cost
• Vendor technical and financial strength
• Maturity of the core-EHR vendor’s solution and risks/benefits of relying on an interface to third-party applications and systems
Radiology Systems
Radiology departments use three major technology systems: picture archiving and communication system (PACS), radiology information system (RIS), and speech recognition system.
PACS
The picture archiving and communication system is used to store and display radiologic images. The standard digital format for PACS data is Digital Imaging and Communications in Medicine (DICOM).3 Radiology departments employ a variety of modalities, each designed for a particular focus. Some examples include
• General X-ray or digital radiography (DR)
• Computed tomography (CT)
• Ultrasound (US)
• Magnetic resonance imaging (MRI)
• Nuclear medicine (NM)
• Positron emission tomography (PET)
• Mammography (MG)
Originally, all radiographic images were printed on film. PACS eliminates the need for film. Additional benefits of PACS are
• The ability to store and retrieve images digitally, thus eliminating the need for film librarians to process a request, find the films, deliver them, and hang them onto a lightbox for interpretation by the radiologist.
• The ability to access the images from any location. This allows any radiologists in one hospital or clinic to read images from another hospital or clinic. It also allows for “nighthawk” coverage, where, for example, radiologists in Australia can easily cover the night shift for hospitals in the United States (since our night is their day).
• Allows for integration and interfacing with other digital hospital systems, such as the radiology information system (RIS) and EHR system.
PACS allows for more efficient image interpretation. Instead of looking at images in a linear fashion (reviewing 150 MRI images laid out over a series of lightboxes), PACS allows the radiologist to sit at a high-resolution workstation and zoom through the images on the Z-axis, much like watching a movie. This has distinct clinical advantages over film radiographic images.4
RIS
Whereas a PACS is designed to optimize the viewing of radiology images for clinical purposes, a radiology information system (RIS) is an information management system specifically designed for tracking radiology operations. A RIS manages patient identification and flow, including scheduling and tracking the patient and storing the results of their radiology test, as dictated by the radiologist.
The RIS is a database designed to track functions such as
• Scheduling and defining the exam (the provider determines the tests and evaluates the conditions of a particular patient) to be performed
• Ordering the exam
• Tracking the patient while in the radiology department
• Storing the radiologist’s result of the interpretation of the images of the exam
• Billing for the exam
The RIS most often interfaces with other hospital systems, notably the EHR system and likely a speech recognition system that is used to interpret the radiologist’s dictation into text. Often, the RIS interfaces with the EHR system via an interface engine that passes electronic messages among various hospital systems such as the EHR system, lab, and radiology systems. The protocol used for this interface is typically Health Level 7 (HL7) versions 2.xx, 3, or Fast Healthcare Interoperability Resources (FHIR). See Chapter 8 for more details about the HL7 standards.
Speech Recognition System
Much of a radiologist’s responsibilities lie with two functions:
• Interpreting the image(s)
• Documenting their findings related to the image(s)
In most instances, when a radiology exam is ordered, the ordering physician (primary care doctor or specialist) is interested in having the images interpreted by the radiologist as quickly as possible so that the physician can provide the next step of care based on the results of the exam. A typical radiologist’s workflow for documenting their findings involves reviewing and interpreting the image while simultaneously dictating into a dictation microphone or telephone dictation system. The radiologist’s voice recording is stored in an analog dictation repository. Later, a transcriptionist listens to the recording and keyboards the report into the RIS. When the draft report is available, the radiologist accesses the report via the RIS, reads the transcribed report, and, if there are no errors, approves it.
With a speech recognition system, the radiologist typically views the images on a PACS workstation and simultaneously inputs his or her findings by speaking through a microphone headset. The speech recognition system converts the speech to text in real time, so that once the radiologist has completed dictation, he or she can immediately review the text, correct any errors, and electronically sign the report. The report is immediately sent to the RIS and/or the EHR system. This technology has allowed for significantly improved efficiencies in the generation of radiology reporting.
Pharmacy Systems
Typically, a pharmacy system has the following major modules:
• Drug information system A drug information system is an online, Internet-based reference tool used by pharmacists to obtain information about drugs.
• Order-filling system A robot-based order-filling system is used to fill prescriptions. The system interfaces with the EHR computerized provider order entry (CPOE) module to receive medication orders directly and then, once a pharmacist has approved them as valid, fill them via a robot installed in an inpatient pharmacy. There are regularly scheduled “cart-fill” processing runs as well as ad hoc filling of “first-dose” orders in the system. The system is usually server based and has several workstations located in a central location for access and operation of the order-filling process. Generally, the order-filling system vendor maintains a 24/7 support structure including proactive monitoring of vital system functions.
• TPN compounder system A total parenteral nutrition (TPN) compounder system is usually two separate applications that are used together to accomplish mixing custom TPN solutions. A compounder application is used by pharmacists to create formulas of TPN compounds for patients. This is a server-based, client/server application that references a database containing information about various elements and proper proportions for mixtures. The compounder is used to create custom mixtures for patients; its primary output is a text file for each formula that is stored on the server. A separate application (or separate module of a combined TPN compounder system) reads the formula files created by the compounder and then, via its interface with a specialized pump, combines up to 24 different elements to create an intravenous (IV) solution based on the pharmacist’s formula for administration to a specific patient.
• Prescription workflow solution In many inpatient settings, unit doses are required. The U.S. Food and Drug Administration (FDA) defines a unit dose as “The delivery of a single dose of a drug to the patient at the time of administration for institutional use, e.g., hospitals.”5 A prescription workflow solution includes software and hardware designed to provide a complete pharmacy workflow solution, including unit dose packaging. As such, the workflow solution fulfills the inventory management and drug distribution needs of the central pharmacy by providing barcode verification of dispensed drugs from the pharmacy to the patient’s bedside. The hardware side consists of two core products: a carousel and a packager. Some customers may purchase only one or the other, as these products can work independently. A software package usually controls the devices to automate the retrieval, inventory management, and packaging.
• Pharmacy management system A pharmacy management system is composed of the following functions: e-prescribing, inventory management, barcode and Universal Product Code (UPC) scanning, workflow management, integrated voice response (IVR) system, drug maintenance updates, fax, long-term care functionality, reporting packages, and a web portal for patients to refill prescriptions.
• Pharmacy workflow system As a key entry point into pharmacy automation, a pharmacy workflow system delivers comprehensive workflow management, in-depth quality control, and real-time prescription tracking. To ensure filling accuracy, workstations establish quality checkpoints by employing barcode scanning, digital imagery of medications and original paper prescriptions, and high-quality software protocols at every stage of the prescription fulfillment process. To achieve continuous improvement, the information management tools provide full visibility into the pharmacy’s daily activity, enabling informed decision-making and best practices, which lead to increased profitability.
• Infusion system An infusion system or module of a broader pharmacy system allows for viewing real-time infusion data, drug library management, drug library uploading, and clinical reporting. This system includes large-volume IV pumps that use real-time communications with a server across a wireless local area network (WLAN) connection. While the pumps actually operate completely independent of the server, the connectivity is used to allow pump infusion libraries to be centrally maintained and selectively pushed out to the pumps as well as to allow pumps to transmit metrics back to the server to report on their operation.
• Drug verification/inspection system This system includes patient safety and process improvement software solutions for difficult-to-manage processes of a hospital pharmacy. Software uses the medication barcode as a control measure for the prevention of medication restocking errors, including those stemming from look-alike or sound-alike items. The system also continually monitors all locations for medications that are near expiration to allow for timely removal prior to use. The system has different audible sound alerts at the time of medication scanning to indicate whether the medication scanned is equivalent to the one assigned. This system saves the pharmacy staff time during the restocking process and serves as an important patient safety check. The planning tool provides pharmacy leadership an easy way to plan, schedule, and monitor inspections of everywhere that medications are stored throughout the hospital. It can provide customizable e-mail alerts when inspections are overdue, provide quality assurance and compliance reports, and provide documentation for all medications removed from stock due to expiration date.
• Automated medication dispensing cabinets Each automated medication dispensing cabinet consists of a computer that is touch-screen accessible as well as accessible via an integral keyboard and touchpad. The computer is used to control access to the various medications that are stored in the cabinet. The cabinets have a wide variety of physical configurations available to accommodate the storage and dispensing for various medications in various containers and forms. Each cabinet is custom designed to best suit the particular location of operation. A provider, most typically a nurse, logs into the cabinet using a personal identification. Each cabinet has screens showing the patients that are currently in that area along with medication profile information regarding the drugs that they are currently prescribed. This information is kept current via data interface feeds from various hospital systems. A specialized cabinet is typically used to store controlled substances; the backend database for this cabinet stores inventory and creates detailed tracking and reporting for each transaction.
• Refill mobile app This is an application for mobile telephone devices that allows the user to refill prescriptions through the outpatient and mail-order pharmacies from their iPhone or Android mobile device. The app talks to the interactive voice response (IVR) server, which then sends the prescription information to the pharmacy software for refill.
Lab Systems
A clinical laboratory—often divided into an anatomic pathology lab and a clinical pathology lab—is where tests are done on clinical patient specimens in order to obtain information pertaining to the diagnosis, treatment, and prevention of disease.6 An anatomic pathology lab, sometimes known as the tissue lab, includes histopathology and cytopathology among its divisions. A clinical pathology lab—sometimes known as the test tube lab—includes microbiology, chemistry, hematology, and genetics among its subdivisions.
Following are the major technology/information systems for clinical laboratories:
• Laboratory management system This system includes microbiology, blood bank lab processing, and a specimen tracking module.
• Laboratory test results system for anatomic and clinical pathology This provides physician clients with disease-oriented pathology reports that convert laboratory data on various tests into information and knowledge applicable at the patient’s bedside. This system correlates the patient’s status with the collective experience of the world’s literature and ensures greater patient safety.
• Laboratory information system (LIS) This system automates and drives workflow for the clinical pathology lab. This system interfaces with software applications and instruments in the lab to create a powerful integrated lab workflow system. It streamlines lab processes to decrease specimen handling time, increase productivity, and improve turnaround time. As an example, a patient’s blood test result can be automatically reported to an EHR.7
• Quality management system Because high quality of results in a lab is critical, this system tracks and reports on various quality issues in registration, accessioning, histology, and transcription. Issues like block labeling are critical as the tests have to be repeated for the patient. Block labeling occurs when a pathologist slices a ”tissue block” removed from a patient by a surgeon into very thin layers and places them on a glass slide for examination under a microscope. Each slide has to be labeled carefully in reference to the tissue block and patient. Block labeling issues are tracked very closely and remediation steps and controls monitored and adjusted to meet thresholds of quality.8
• A system for Internet access to lab orders and results This web-based system is directly interfaced to several other lab and non-lab systems.
The laboratory’s systems are also interfaced to the billing system for inpatient admissions, discharges, and transfers (ADT) and outpatient registration and all billing functions. Usually, an order-entry and results-reporting interface is available in the EHR clinical repository and web-based laboratory system via an application interface engine.
The laboratory takes advantage of all the advanced features of these systems including, but not limited to, bar-coded sample and patient identification, bidirectional instrument interfacing, distributed patient report printing, image processing, rules processing, and Internet-based access.
In addition to meeting the care needs of the patients, these systems enable the health system to market the medical lab as a referral laboratory, develop partnerships with other organizations, and support substantial enhancements in overall productivity. In addition, they allow effective and seamless integration among separate facilities and interface with existing and future corporate and clinical information systems.
Technical support is provided by a central IT team or a lab information support team.
Patient Monitoring Systems
Patient monitoring systems are almost universally present in the intensive care units (ICU) and operating rooms (OR) of inpatient settings, but they are also found in “step-down” units that transition patients from ICUs and ORs to less acute care units prior to their discharge. A new setting for patient monitoring systems is the home where clinicians use mobile health technology solutions to connect patient monitors worn by patients continually or intermittently in their homes with clinicians who evaluate the patient monitoring data remotely. Two of these applications of patient monitoring systems are further explored here.
EICU Monitoring Systems
A bedside physiologic monitor monitors patient vitals in an inpatient setting. An EICU system consists of a monitor in each room, tying back to a central server for processing of the monitored data. The unvalidated output of the monitors is transmitted through an interface engine to a care application (part of the monitoring software) for review by the care manager. The monitoring hardware and software are maintained by a combination of the clinical engineering department, the HIT department, and the vendors.
There is a second feed sourced from the EHR system containing validated monitoring data from specific vital-sign flowsheet records. The specific monitor-sourced, EICU-processed entries (e.g., temperature, heart rate, blood pressure) into the patient’s record within the EHR system can—if all the parts are working together effectively—give a valid representation of the patient’s status.
In addition, other datasets such as lab results and medications are interfaced to the EICU care application interface. The care application system uses algorithms from the various vitals, labs, and meds (all interfaced to the EHR system) to determine the patient’s status; it alerts the staff when a defined threshold is met.
OR Monitoring Systems
This group of monitoring systems includes not only the systems dedicated to hospital ORs but also the systems present in any procedure rooms with anesthesia capability, such as endoscopy, interventional radiology, cardiac catheterization, and MRI. Data capture software is used to interface the monitored data into the EHR system. To start the process, an anesthesiologist manually connects the data capture device to the EHR system. The data flows from the OR monitoring hardware to the EHR system. Most EHR systems have an anesthesia module to store data collected from monitoring systems as part of the medical record. All patient vital data from an anesthesia machine are recorded and transferred to the EHR system. This is unvalidated data that flow unfiltered to the EHR system for temporary storage. A nurse typically reviews the whole dataset and selects the appropriate vital signs for permanent submission into the EHR system. After 72 hours, all unvalidated data are purged from the EHR system.
Supply Chain Systems
The supply chain function of a healthcare organization typically consists of centrally managed core operations and strategically placed decentralized operations. A supply chain services division of a healthcare organization provides oversight management for contract support and all capital and related service acquisitions. Clinical integration for all product and equipment decisions occurs through the application of the Clinical Use Evaluation (CUE) or similar process. This process is a system-wide, structured, interdisciplinary process to review all aspects of product utilization, product selection, new products, and product formulary development and cost effectiveness. It facilitates review of product data and outlines product evaluations for recommendations and discussion leading to the formulation of an action plan to implement and measure the impact of change in the supply chain.
The following are the main CUE objectives:
• Aid in the cost-effective delivery of high-quality patient care through clinically driven product selection and utilization management
• Educate and involve staff in the process
• Develop a product formulary
By using the CUE process, members of supply chain services staff are able to review all products and equipment used throughout the organization. This process allows avoidance of duplication, reduction of inventory, and reduced costs. To help achieve these goals, the main system used in the supply chain department is an ERP software system, described next.
ERP Software Systems
An enterprise resource planning (ERP) software system is typically used by organizations to organize and maintain a set of integrated applications and associated data for operations. ERP systems support key operational functions like manufacturing, distribution, purchasing, accounting, and inventory management. Supply chain departments use ERP software because of the integrated nature of the applications in the ERP software, enabling the department to track products, utilization, and purchasing in a central place. This eliminates the need to use multiple applications and move data from one application to another.
Finance and Operations Systems
Patients in a hospital must be registered and tracked from location to location as they progress through different care areas. The services, treatments, medicines, and equipment they use must likewise be tracked and accounted for. Similar requirements exist in ambulatory settings. “Billing systems,” used for tracking patient expenses and billing them or their insurers, were some of the first HIT systems to be used in hospitals. They were started as simple systems in the 1960s and ’70s but over the years became more sophisticated as healthcare organizations became more complex. As this evolution occurred, the term “revenue cycle management” was coined to identify the increasingly complex functions in healthcare financial systems. At first this took the form of simply more robust billing systems, but over time these systems became more common and multifaceted. They are now either part of or interfaced with EHR systems and serve to automate financial and operational functions in healthcare.
Basic revenue cycle management systems contain the subsystems or modules in Table 19-1. It is important to note that as this is written, revenue cycle systems are changing to adapt to an increasingly consumer-directed healthcare environment and new forms of healthcare delivery such as retail health.9
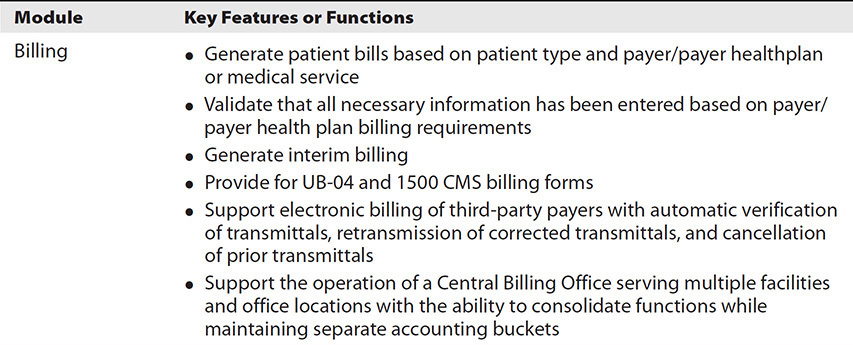
Table 19-1 Revenue Cycle Management System Modules and Key Features/Functions
Clinical Decision Support (CDS)
The Office of the National Coordinator of Health Information Technology (ONC) broadly defines CDS as follows:
Clinical decision support (CDS) provides clinicians, staff, patients or other individuals with knowledge and person-specific information, intelligently filtered or presented at appropriate times, to enhance health and health care. CDS encompasses a variety of tools to enhance decision-making in the clinical workflow. These tools include computerized alerts and reminders to care providers and patients; clinical guidelines; condition-specific order sets; focused patient data reports and summaries; documentation templates; diagnostic support, and contextually relevant reference information, among other tools.11
Lobach et al. found evidence showing that CDS has significant impact on clinical process outcomes such as the ordering of preventive, clinical, and treatment services, as well as the enhancement of clinician’s knowledge pertaining to a medical condition.12 This study and the ONC point to CDS broadly and importantly impacting increased quality of care, enhanced health outcomes, avoidance of errors and adverse events, and improved cost outcomes.
CDS is manifest in HIT in many ways. It is integral to many modules of an EHR system; for instance, a CPOE module of an EHR system relies on CDS to issue drug interaction alerts. CDS is also integral to applications that support “hot links” to clinical practice guidelines available to a clinician as he or she is treating a patient or documenting care, whether as a stand-alone app or embedded within an EHR clinical documentation module. A well-known and highly regarded resource for those who would like to learn more about this very important field within HIT and informatics is Improving Outcomes with Clinical Decision Support: An Implementer’s Guide, Second Edition, by Osheroff et al.13
Patient Relationship Management Systems
Patient relationship management is a relatively new concept that is being adopted in the healthcare industry. A patient relationship management software system maintains a list of all patients and their important personal preferences and attributes, such as preferred appointment times, the last contact via phone or e-mail the patient had with the contact center, and the length of time the patient has been associated with a particular health system. The patient relationship management system stores these and many more of their personal preferences and attributes and makes them easily accessible to contact center users. The goal of the patient relationship management software is to provide the best quality care and a personalized experience for patients. The patient relationship management system meets both these goals by providing tools and data in a single system.
Application Data Interchange Systems
Application data interchange systems are typically used to provide reliable connectivity within hospitals, information exchanges, and public health organizations. The application data interchange is one of the key systems helping in the delivery of consistent, efficient, quality patient care.14
An application data interchange system encompasses three main functional areas and two management console options:
• The interface engine is the main messaging service that implements communication, inter-format mapping, persistent message delivery, and message routing.11
• An integrated development environment (IDE) has an easy-to-learn graphical user interface to configure the functionality of the application data interchange system.
• The management console is usually a web-based application that displays system status and performance monitoring. It also allows the sorting, viewing, editing, and resending of messages and real-time monitoring of system logs and error conditions. It has two optional components:
• A mobile app that provides the basic monitoring capability of the management console on a smartphone or tablet.
• A web-based dashboard application that displays the notifications and system health of multiple application interface engines in a single monitoring-centric view.
Chapter Review
Healthcare information technology (HIT) systems play a critical role in improving patient care and enabling healthcare organizations to operate more effectively and efficiently. EHR and non-EHR systems enable better patient care through the use of technology. The HIT function in a healthcare organization, just like the IT function in companies or institutions, is led by a CIO in most cases. Many healthcare organizations also have a CMIO, which is a prominent position within or alongside the CIO’s department that is usually held by a physician or other clinician trained in informatics. These HIT leaders oversee a wide array of application specialists, system analysts, programmers, support technicians, project managers, and many other roles if the organization is large. The structure of HIT departments within healthcare organizations varies, but it often involves divisions or subdepartments with managers overseeing the EHR system. These “ancillary” systems include lab, pharmacy, and radiology; revenue cycle or other nonclinical systems; infrastructure (such as hardware and networks); and user support such as the help desk function.
In this “age of the EHR,” other systems crucial to the functioning of a healthcare enterprise are often overlooked. Clinical and operational systems in the lab, radiology, and pharmacy (either as part of the EHR system or otherwise) are critical for tracking patient workflow, recording results, providing quick access to records for both patients and providers, and storing digital information for long periods. These clinical systems also improve the quality of care by automating various functions, catching and alerting on errors in workflow. These systems integrate data into the EHR system via the central interface engine, making all information about the patient available in one place for providers to make better and faster decisions.
Nonclinical systems such as supply chain, finance, billing, and data interchange services provide the core support services that keep health systems in operation and financially viable. Supply chain systems provide ordering, tracking, and efficient movement of supplies through the health system.
Many technologies, information systems, and people work together to deliver clinical and operational support in today’s modern healthcare enterprises.
Questions
To test your comprehension of this chapter, answer the following questions by selecting the best available choice and then check your answers against the list of correct answers at the end of the chapter.
1. Due to the increase in use and importance of the electronic health record (EHR) in healthcare organizations, _________________.
A. non-EHR systems are no longer needed
B. non-EHR systems usually interface or integrate with the EHR system
C. non-EHR systems have been entirely replaced by EHR modules
D. non-EHR systems have not proliferated
2. Which of the following is a major clinical system, whether a stand-alone system interfaced with the EHR system or a module of the EHR system?
A. Supply chain system
B. Patient relationship management system
C. Clinical laboratory system
D. Revenue cycle system
3. A(n) ___________ is usually part of the vetting process when a healthcare organization is acquiring a new software system.
A. Request for Proposal (RFP)
B. Proof of Perquisites (PoP)
C. Exit Plan (EP)
D. Federal Government Audit (FGA)
4. Which of the following best describes a business relationship manager (BRM) in a healthcare IT department?
A. The information systems department manager who handles human relations issues
B. A quality improvement professional
C. The person representing the needs of the clinical and nonclinical departments to the HIT department
D. The person representing the needs of the vendors to the HIT department
5. A radiologist uses speech recognition software to accomplish which of the following?
A. Automatically classify images
B. More easily document findings related to images
C. Interpret communication from patients and staff members who speak other languages
D. Keep track of tasks
6. A laboratory information system can interface to a(n) _________________.
A. laboratory instrument and instantly report a result of a patient’s blood chemistry test to an EHR
B. pharmacy system and direct a nurse to administer a unit of blood
C. radiology system, resulting in an automatic order for an X-ray
D. EHR system by route of a cybersecurity module of the healthcare organization interface engine
7. Finance and operations systems are used for which of the following?
A. Clinical decision support
B. Clinical case management
C. Priority management
D. Billing
8. Which one of the functional areas of an application data interchange is not considered a main functional area?
A. The interface engine
B. The integrated development environment (IDE)
C. The management console
D. Mobile smartphone-mediated management
Answers
1. B. Due to the increase in use and importance of the EHR in healthcare organizations, non-EHR systems usually interface or integrate with the EHR system.
2. C. The clinical laboratory is a major clinical system, whether it is a stand-alone system interfaced with the EHR or a module of the EHR system.
3. A. The Request for Proposal (RFP) is usually part of the vetting process when a healthcare organization is acquiring a new software system.
4. C. The business relationship manager (BRM) is usually the person representing the needs of the clinical and nonclinical departments to the HIT department.
5. B. A radiologist uses speech recognition software to more easily document his or her findings related to the images.
6. A. A laboratory information system can interface to a laboratory instrument and instantly report a result of a patient’s blood chemistry test to an EHR system.
7. D. Finance and operations systems are used for billing.
8. D. The interface engine, integrated development environment (IDE), and management console are considered the three main functional areas of an application data interchange. A mobile app that supports smartphone-mediated management may be an option. Another management console option that is not listed in the choices is a web-based dashboard.
References
1. Medicare Payment Advisory Commission. (2016, June). Report to Congress: Medicare and the healthcare delivery system. Accessed on August 15, 2016, from www.medpac.gov/docs/default-source/reports/june-2016-report-to-the-congress-medicare-and-the-health-care-delivery-system.pdf?sfvrsn=0?.
2. Vitalari, N. P. (n.d.). A prospective analysis of the future of the U.S. healthcare industry. Accessed on August 20, 2016, from http://merage.uci.edu/ResearchAndCenters/CDT/Resources/Documents/N%20Vitalari%20A%20Prospective%20Analysis%20of%20the%20Healthcare%20Industry.pdf.
3. PACS History web site. Accessed on August 1, 2016, from www.pacshistory.org/documents/index.html.
4. Forsberg, D., Rosipko, B., & Sunshine, J. L. (2016). Factors affecting radiologist’s PACS usage. Journal of Digital Imaging, 29(6), 670–676.
5. U.S. Food and Drug Administration. (2015). Unit dose labeling for solid and liquid oral dosage forms (section 430.100). In Compliance policy guides. Accessed on November 28, 2016, from www.fda.gov/ICECI/ComplianceManuals/CompliancePolicyGuidanceManual/ucm074377.htm.
6. Farr, M., & Shatkin, L. (2004). Best jobs for the 21st century (p. 460). JIST Works.
7. Futrell, K. (2013). The value of the laboratory in the new healthcare model. Accessed on July 29, 2016, from www.orchardsoft.com/files/white_paper_value_lab.pdf.
8. MUSC Laboratory Information Services Team. (2014). Cerner CoPath. Documentation: Histology section. Accessed on November 28, 2016, from https://www.musc.edu/pathology/website/labservices/anatomic/CoPath/index.html?introduction.htm.
9. HIMSS Revenue Cycle Improvement Task Force. (2015). Rethinking revenue cycle management. Accessed on April 6, 2017, from www.himss.org (membership login required).
10. HIMSS. (2010). Revenue cycle management vendor requirements checklist. Accessed on April 6, 2017, from http://www.himss.org/revenue-cycle-management.
11. Office of the National Coordinator of Health Information Technology. (2014). Clinical decision support (CDS). Accessed on November 19, 2015, from https://www.healthit.gov/policy-researchers-implementers/clinical-decision-support-cds.
12. Lobach, D., Sanders, G. D., Bright, T. J., Wong, A., Dhurjati, R., Bristow, E., … Kendrick, A. (2012, April). Enabling health care decisionmaking through clinical decision support and knowledge management. Evidence Report / Technology Assessments, No. 203. Agency for Healthcare Research and Quality.
13. Osheroff, J. A., Teich, J. M., Levick, D., Saldana, L., Velasco, F. T., Sittig, D. F., … Jenders, R. A. (2012). Improving outcomes with clinical decision support: An implementer’s guide, second edition. HIMSS.
14. Office of the National Coordinator of Health Information Technology. (2016). A 10-year vision to achieve an interoperable health IT infrastructure. Accessed on July 22, 2016, from https://www.healthit.gov/sites/default/files/ONC10yearInteroperabilityConceptPaper.pdf.

